- 1Department of Pediatrics, Seoul St. Mary’s Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 3Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Republic of Korea
- 4Medical Library, The Catholic University of Korea, Seoul, Republic of Korea
- 5Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
Background: Centrally inserted central catheterization (CICC) is a critical procedure in pediatric care. However, CICC in children poses greater challenges compared to adults due to anatomical and physiological differences, leading to higher complication rates. Ultrasound-guided approaches have been developed to enhance the safety and effectiveness of CICC, but the comparative efficacy of different axis approaches remains unclear.
Methods: A systematic review and meta-analysis of randomized controlled trials comparing different axis approaches for ultrasound-guided CICC in children was conducted. Searches were carried out in databases up to June 10, 2024. Six studies were included in the systematic review and three studies were included in the meta-analysis. Primary outcomes included first-attempt success rate, overall success rate, and cannulation time. Secondary outcomes were complications such as hematoma and posterior wall puncture.
Results: Data from 547 children were analyzed. The long-axis in-plane approach significantly reduced cannulation time (MD −27.48 s, 95% CI, −33.99 to −20.97) and overall complications OR 0.21, 95% CI, 0.1–0.48) compared to short-axis out-of-plane approach. No significant differences were found in first-attempt or overall success rates between the long-axis and short-axis approaches.
Conclusion: The long-axis approach for ultrasound-guided CICC in children offers significant advantages in reducing cannulation time and complications. While dynamic needle tip positioning method may serve as an alternative to in-plane methods, further studies are needed to validate its clinical efficacy. Further research is needed to refine these techniques and explore their application in diverse clinical settings.
1 Introduction
Central catheter placement is crucial for critically ill patients requiring hemodynamic monitoring, and vasoactive drug administration (1, 2). However, centrally inserted central catheterization (CICC) in children presents more challenges and higher complication rates compared to adults (3, 4). The success and risk of complications also depend on the patient's condition, anatomy, and the operator's skill (4–6). Therefore, it is essential to identify a safe and effective method for CICC in children.
In pediatric patients, CICC is generally performed through the internal jugular, subclavian, or femoral vein (7). Traditionally, this procedure used anatomical landmarks and techniques such as the Seldinger technique (8, 9). With the advent of ultrasound (US) in intensive care settings, US-guided approaches have gained prevalence (10). Compared to anatomical approaches, US-guided CICCs have shown higher success rates, fewer puncture attempts, and reduced complication rates (11–14).
The US probe for central venous access can be oriented to provide either a “short-axis” (cross-sectional view) or a “long-axis” (longitudinal view) image of the vessel (15, 16). Needle insertions are classified as in-plane or out-of-plane based on their visibility in the US image (15). A combined technique begins with a short-axis view and then rotates the probe to a long-axis view (17). The modified dynamic needle tip positioning (DNTP) is a modified short-axis out-of-plane technique designed to improve needle tip tracking (18). Unlike the traditional static short-axis out-of-plane approach, where the transducer remains fixed and the needle is advanced blindly, DNTP involves dynamic transducer movement to intermittently relocate the needle tip.
The comparative effectiveness and safety of the short-axis out-of-plane vs. long-axis in-plane approaches have not been conclusively established in adult patients (19–21). This study evaluates the effectiveness and complications associated with the short-axis out-of-plane, long-axis in-plane, DNTP methods for US-guided CICC in children through a systematic review and meta-analysis.
2 Methods
2.1 Study design
A systematic review of RCTs comparing different axis approaches for ultrasound-guided CICC in children was conducted, accompanied by a meta-analysis to evaluate the effectiveness and safety of these CICC approaches. The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (22).
2.2 Database and search strategy
A comprehensive and peer-reviewed search strategy was developed by a medical librarian (NJK). Searches were carried out in PubMed, Embase, and The Cochrane Library from inception to June 10, 2024, employing terms related to US, CICC, and pediatric age. The detailed search strategy is outlined in Supplementary 1.
2.3 Data collection and analysis
Two independent reviewers (IKL and KHL) screened titles and abstracts to identify potentially eligible trials. They then evaluated the full texts of the selected studies for eligibility. Any discrepancies between the reviewers were resolved through discussion, and if necessary, a third reviewer was consulted to reach a consensus.
2.4 Inclusion criteria
Included were trials that: (1) involved studies with children; (2) were RCT; and (3) compared different axis approaches for US-guided CICC.
2.5 Exclusion criteria
Excluded were trials that: (1) were observational studies, case reports, letters, editorials, or were not peer -reviewed; (2) included duplicate samples; (3) involved only adult participants; (4) did not utilize US for CICC; or (5) involved studies with peripherally inserted central catheters.
2.6 Outcomes
The primary outcome focused on catheterization success rates and cannulation time. Secondary outcomes included complications such as overall complication, hematoma, and posterior wall puncture.
2.7 Quality assessment
The risk of bias in included trials was assessed by two reviewers (IKL and KHL) using a modified version of the Cochrane risk of bias tool (23). Each trial was examined for bias across various domains, with each domain assessed as having low, unclear, or high risk. The classification of the overall risk of bias for each trial was as follows: classified as low if the risk of bias was low or possibly low in all domains, classified as unclear if there was an unclear risk of bias in at least one domain with no domain having a high risk of bias, and classified as high if there was a high or possibly high risk of bias in any domain. Any discrepancies were resolved through discussion and consensus.
2.8 Statistical analysis
The meta-analysis employed R version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria) to analyze different axis approaches of CICC. For continuous outcome data, the mean difference served as the primary measure, with estimates aggregated using the inverse variance method. The Mantel-Haenszel method pooled estimates for binary outcome data, using odds ratio and risk ratio as primary metrics. The choice between a common or a random effects model was based on heterogeneity levels, indicated by I2 exceeding 50%, favoring a random effects model at that point.
3 Results
3.1 Study selection and characteristics
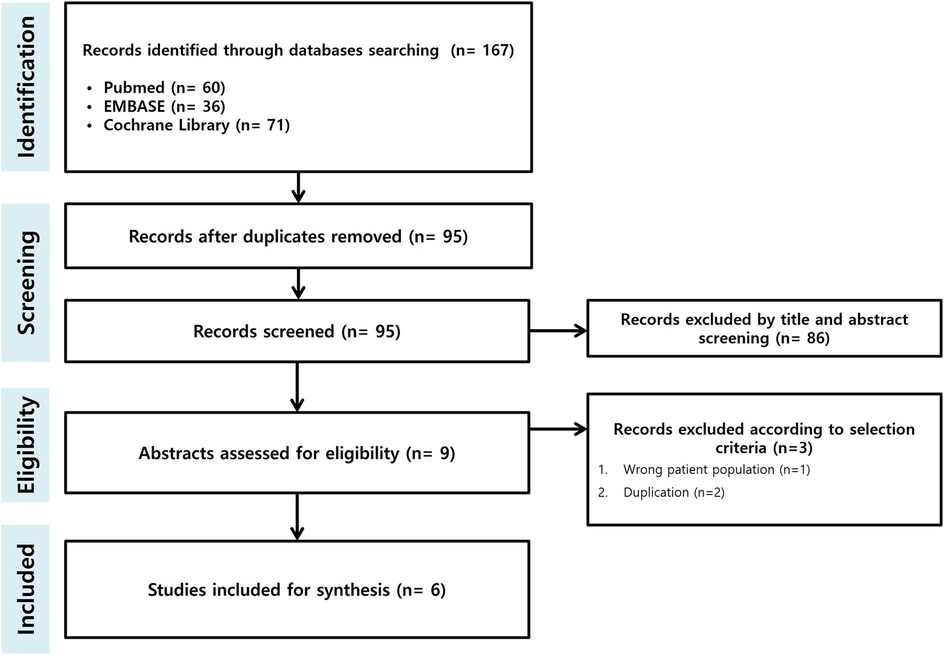
The search identified a total of 167 records. After screening and assessing for eligibility, six studies were included in the systematic review, and three studies were included in the meta-analysis (24–29) (Figure 1).
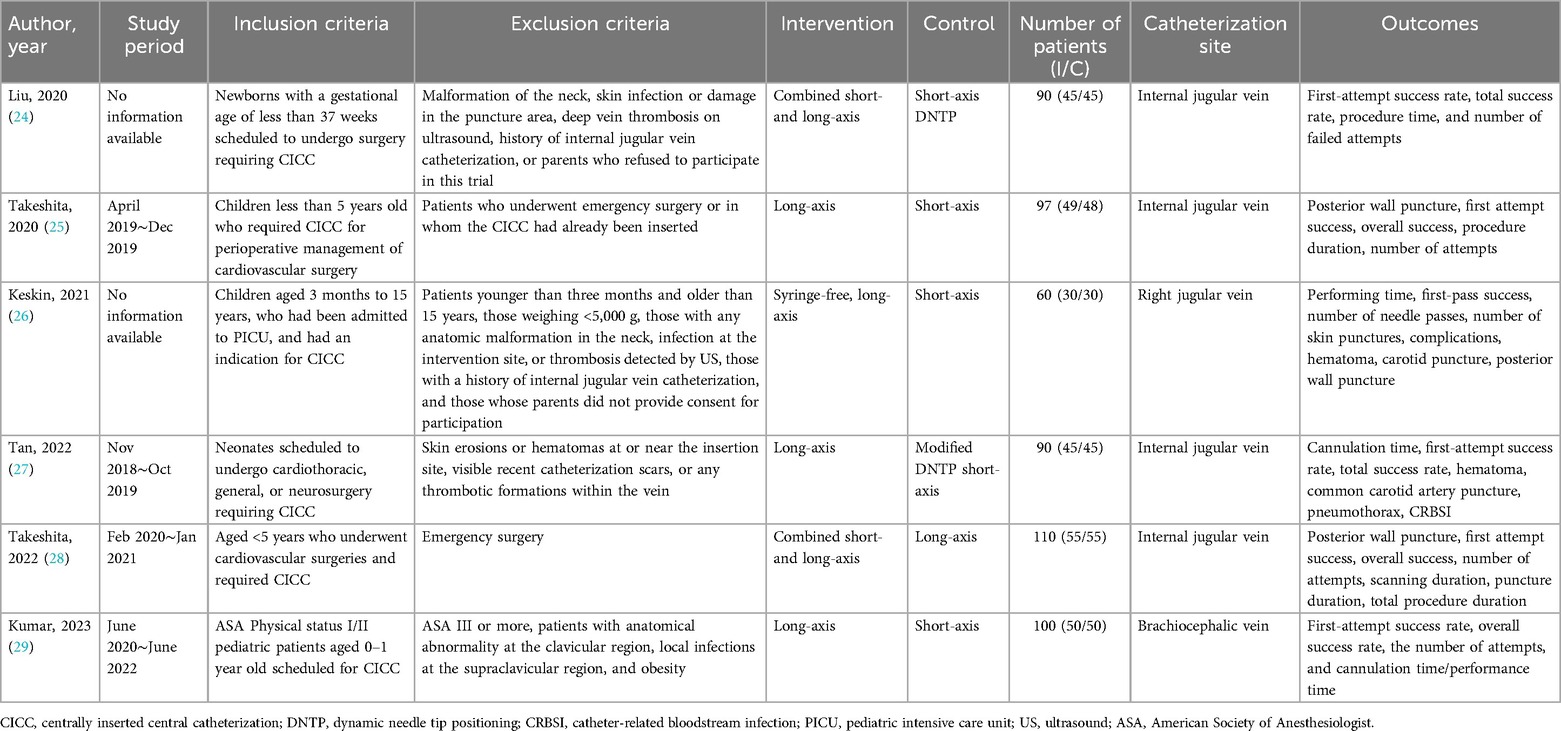
Among these, two studies focused on neonates, and four studies included participants scheduled for surgery. Three studies compared the long-axis and short-axis approaches, while two studies compared the DNTP approach to conventional approaches, such as the long-axis or combined short- and long-axis approaches (Table 1). However, studies including DNTP approaches were not included in the meta-analysis due to heterogenous comparison groups.
3.2 Risk of bias
The risk of bias within the included studies is illustrated in Figure 2.
3.3 Outcomes
3.3.1 Catheterization success rates and cannulation time
Data from three studies were integrated into the meta-analysis for catheterization success rates and cannulation time. No significant differences were observed in first-attempt success rates (OR 2.16, 95% CI, 0.81–5.75, Figure 3A) or overall success rates (OR 2.38, 95% CI, 0.71–7.97, Figure 3B) between the long-axis and short-axis approaches. However, the cannulation time was significantly shorter with the long-axis approach compared to the short-axis approach (MD −27.48 s, 95% CI, −33.99 to −20.97, Figure 3C).
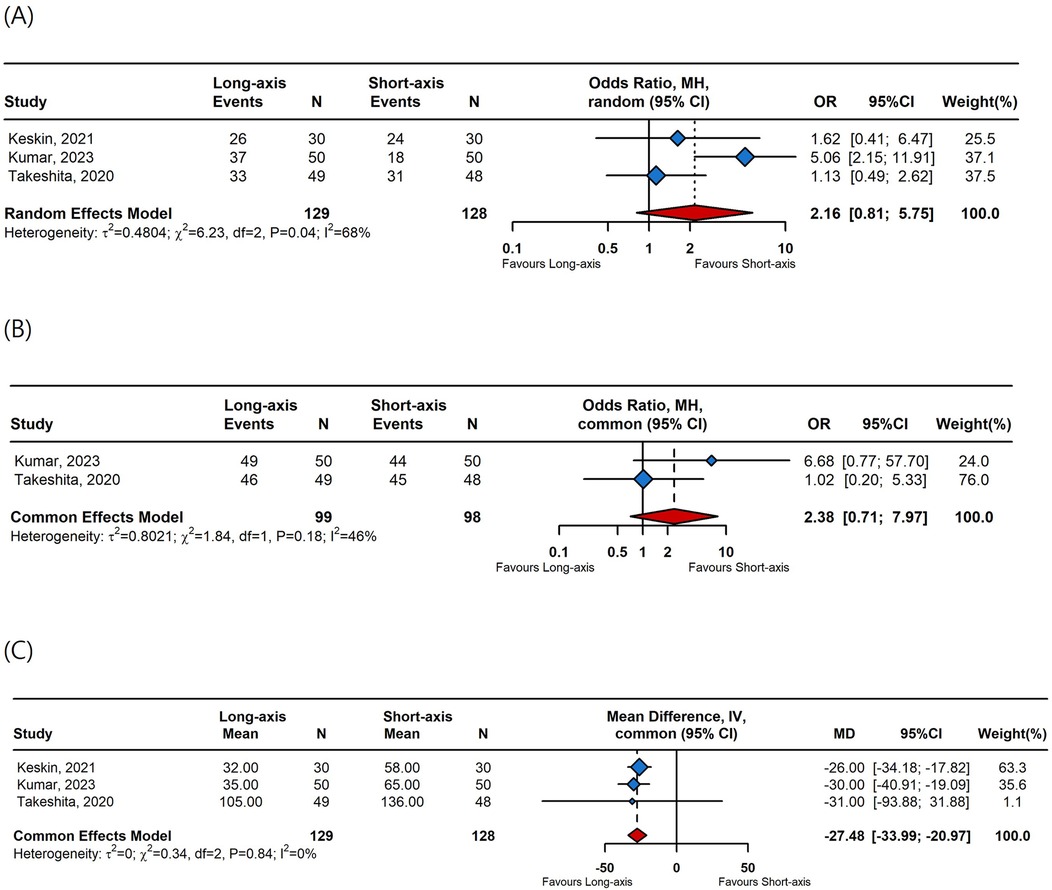
Figure 3. A forest plot comparing (A) first-attempt success rates, (B) overall success rates, and (C) cannulation time between long-axis and short-axis. OR, odds ratio; CI, confidence interval; MD, mean difference.
3.3.2 Catheterization complications
Data from three studies were included in the meta-analysis for complications. The long-axis approach significantly reduced overall complications (OR 0.21, 95% CI, 0.1–0.48, Figure 4A) and posterior wall punctures (OR 0.14, 95% CI, 0.05–0.43, Figure 4C) compared to the short-axis approach. However, there was no difference in hematoma incidences between the long-axis and short-axis approaches (OR 0.42, 95% CI, 0.12–1.42, Figure 4B).
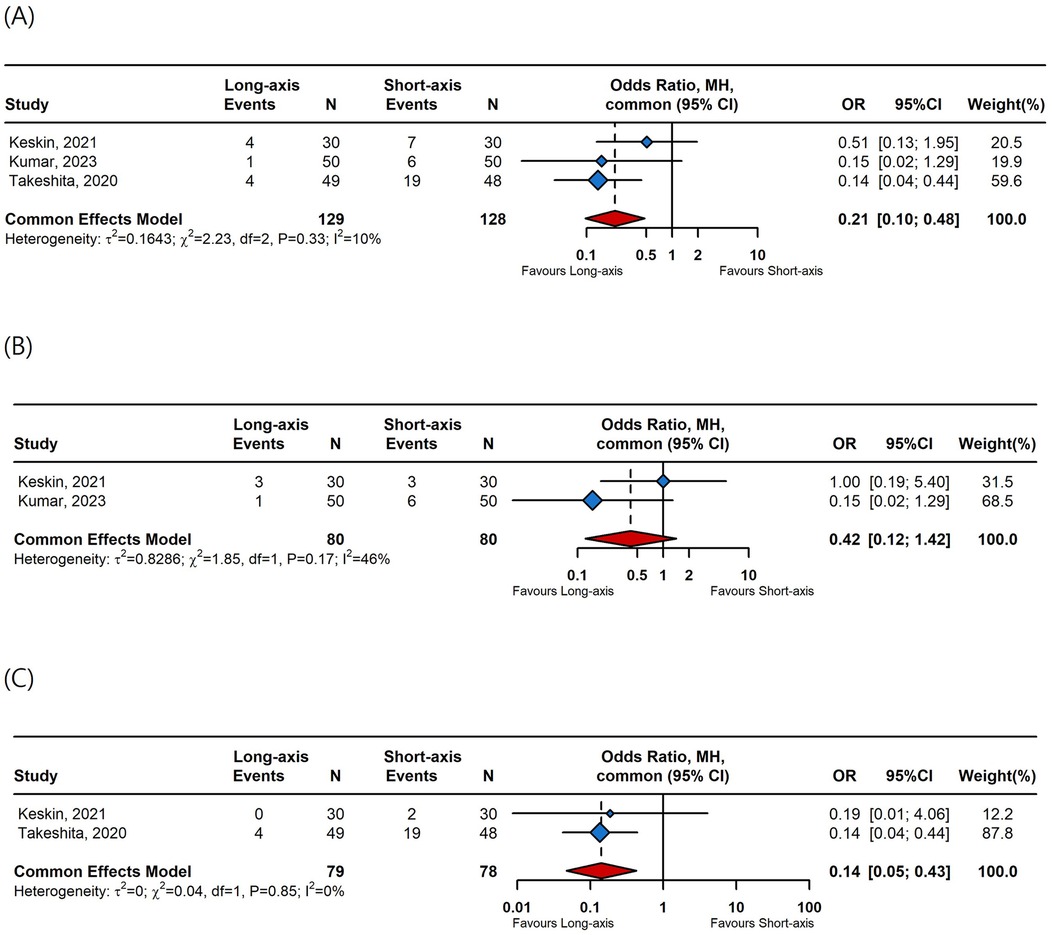
Figure 4. A forest plot comparing (A) overall complication rates, (B) hematoma rates, and (C) posterior wall puncture rates between long-axis and short-axis. OR, odds ratio; CI, confidence interval.
4 Discussion
This systematic review and meta-analysis, which included 547 children undergoing CICC, demonstrates that the long-axis approach significantly reduces cannulation time and catheterization complications compared to the short-axis approach. However, it did not demonstrate significant effects on success rates.
Depending on the US probe's position relative to the vessel, US-guided CICC can be categorized into short-axis and long-axis views. Needle insertions are classified as in-plane or out-of-plane based on their visibility in the US image. The short-axis out-of-plane view provides a cross-sectional image of the vessel, enhances visualization of arterial and venous structures, reduces the risk of arterial puncture, and is simpler for less experienced physicians to learn (15, 30). However, this traditional technique lacks consistent needle tip visualization, which can lead to higher complication rates, longer cannulation times, and an increased risk of posterior wall puncture. In contrast, the long-axis in-plane view offers a longitudinal image and improves needle tip visualization (15, 16, 31). A combined technique begins with a short-axis view and rotates the probe to a long-axis (17), and has been shown to have a lower incidence of posterior wall puncture in adult patients (32).
More recently, the DNTP technique has emerged as a modification of the short-axis out-of-plane approach, aiming to improve needle tip tracking while retaining the cross-sectional vessel view. DNTP starts with a short-axis view, moves the probe away, and advances the needle until the tip is visible in the vessel lumen (18). This modification has largely replaced the traditional static out-of-plane approach in clinical practice, as it improves needle tip guidance while maintaining the benefits of short-axis imaging. As a result, the main clinical debate now lies in the choice between DNTP and in-plane approaches, as both methods provide comparable success rates while differing in operator preference and training (33, 34).
Central catheterization in children is more challenging than in adults, primarily due to distinct anatomical and physiological differences. Pediatric patients generally possess thinner, more delicate veins requiring careful needle handling and placement (35). The smaller vessel size not only complicates vein access but also increases the likelihood of complications such as puncturing the posterior wall or causing vessel trauma. Moreover, younger children with increased adiposity may experience obscured vascular lanmarks during CICC placement. Another challenge in children is their lower intravascular pressure, which can lead to vessel collapse under the weight of ultrasound transducer. Additionally, pediatric patients present unique challenges because they rarely lie still during the procedure, particularly if they are non-intubated or awake. Comfort measures, sedation, or child-friendly distraction techniques are often necessary to ensure procedural success and patient cooperation. These factors underscore the importance of selecting the most suitable and safe CICC method for pediatric patients.
Previous meta-analyses on different axis approaches of CICC primarily focused on adults (19, 20). The most recent meta-analysis in adults indicated that the short-axis approach might offer advantages such as higher first needle pass success rates, potentially reducing cannulation attempts and access time (36). However, our study demonstrated that the long-axis approach offers shorter cannulation times and fewer complications in pediatric patients. This difference could be attributed to the unique anatomical and physiological characteristics of children, which may influence the outcomes of different CICC approaches. To our knowledge, this is the first systematic review and meta-analysis in pediatrics comparing different axis approaches for US-guided CICC.
Our analysis revealed no significant difference in first-attempt or overall success rates between the long-axis and short-axis approaches, suggesting that both methods are equally effective for pediatric CICC. However, the long-axis approach significantly reduced the duration of cannulation compared to the short-axis approach. This efficiency may be attributed to the continuous visualization of the needle tip provided by the long-axis view, facilitating more accurate needle placement.
Furthermore, the long-axis approach significantly decreased overall complications and posterior wall punctures compared to the short-axis approach, making it a safer option for pediatric CICC. Continuous visualization of the needle tip during insertion likely contributes to the reduced complication rates, as it allows for more precise needle guidance and reduces the risk of accidental puncture. However, there was no significant difference in hematoma rates between the two approaches, and carotid artery puncture rates could not be analyzed due to limited results.
The DNTP approach, designed to improve needle tracking while maintaining a short-axis view, was excluded from meta-analysis due to heterogeneity of study designs but was included in the systematic review. DNTP, which is a modified short-axis approach first introduced by Clemmesen et al. for peripheral venous cannulation (37), suggests that while it may offer theoretical benefits such as improved needle tip visualization, its practical advantages in pediatric CICC over established techniques require further investigation. In adults, only a few studies have demonstrated the advantage of the DNTP method over the palpation technique in arterial cannulation (18, 38). Future studies should focus on larger sample sizes and standardized protocols to better assess the potential benefits of DNTP in pediatric CICC.
Moreover, US pre-assessment has emerged as a crucial component in central venous access procedures, offering numerous benefits for both clinicians and patients. Protocols like the Rapid Central Vein Assessment allow clinicians to evaluate vascular anatomy, vessel condition, and any anatomical variations before cannulation (39). As guidelines increasingly emphasize US guidance, integrating a standardized US pre-assessment protocol is now essential for improving clinical outcomes (40, 41).
There are also certain limitations in this study. Firstly, the number of included studies and patients was relatively small. Secondly, the heterogeneity among the included studies concerning patient populations, operator experience, and procedural protocols could affect the outcomes. Thirdly, we could not conduct meta-analysis of the combination of two approaches and the oblique approach due to limited data. Lastly, the variability in follow-up periods among studies may not adequately capture long-term complications associated with different CICC approaches. Future research should address these limitations by conducting larger, well-designed randomized controlled trials with standardized outcome measures and extended follow-up periods.
In conclusion, the long-axis approach for US-guided CICC in children significantly reduces cannulation time and catheterization complications compared to the short-axis approach. Despite the innovative nature of the DNTP technique, it did not demonstrate significant superiority in our analysis. These findings support the use of the long-axis approach in pediatric CICC procedures, although there were no differences in success rates. Further research is needed to refine these techniques and explore their application in diverse clinical settings.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the dataset used in this study is derived from previously published randomized controlled trials (RCTs) and is publicly available through the original publications. As such, the dataset is subject to the restrictions and limitations imposed by those original studies, including access to full datasets, specific study methodologies, and any proprietary or ethical restrictions placed by the original authors. The data extracted and analyzed in this meta-analysis are limited to what was reported in these published studies, and no additional or raw data were generated or accessed beyond the scope of these publications. Therefore, the dataset is not directly available through this article but can be accessed through the referenced studies. Requests to access these datasets should be directed toaW5reXVuZzkyMzNAaGFubWFpbC5uZXQ=.
Author contributions
IL: Conceptualization, Data curation, Formal Analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. KL: Conceptualization, Data curation, Formal Analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. H-jH: Conceptualization, Writing – original draft, Writing – review & editing. JC: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. NK: Data curation, Writing – original draft, Writing – review & editing. KK: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grant no. 09-2024-0001 from the SNUBH Research Fund.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1481975/full#supplementary-material
References
1. Jamshidi R. Central venous catheters: indications, techniques, and complications. Semin Pediatr Surg. (2019) 28(1):26–32. doi: 10.1053/j.sempedsurg.2019.01.005
2. Javeri Y, Jagathkar G, Dixit S, Chaudhary D, Zirpe KG, Mehta Y, et al. Indian society of critical care medicine position statement for central venous catheterization and management 2020. Indian J Crit Care Med. (2020) 24(Suppl 1):S6. doi: 10.5005/jp-journals-10071-G23183
3. Tercan F, Oguzkurt L, Ozkan U, Eker HE. Comparison of ultrasonography-guided central venous catheterization between adult and pediatric populations. Cardiovasc Intervent Radiol. (2008) 31:575–80. doi: 10.1007/s00270-008-9315-7
4. Johnson EM, Saltzman DA, Suh G, Dahms RA, Leonard AS. Complications and risks of central venous catheter placement in children. Surgery. (1998) 124(5):911–6. doi: 10.1016/S0039-6060(98)70016-9
5. Whitney R, Langhan M. Vascular access in pediatric patients in the emergency department: types of access, indications, and complications. Pediatr Emerg Med Pract. (2017) 14(6):1–20.28562239
6. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. (2003) 348(12):1123–33. doi: 10.1056/NEJMra011883
7. Lau CS, Chamberlain RS. Ultrasound-guided central venous catheter placement increases success rates in pediatric patients: a meta-analysis. Pediatr Res. (2016) 80(2):178–84. doi: 10.1038/pr.2016.74
8. Higgs Z, Macafee D, Braithwaite B, Maxwell-Armstrong C. The Seldinger technique: 50 years on. Lancet. (2005) 366(9494):1407–9. doi: 10.1016/S0140-6736(05)66878-X
9. Hsu CCT, Kwan GN, Evans-Barns H, Rophael JA, van Driel ML. Venous cutdown versus the seldinger technique for placement of totally implantable venous access ports. Cochrane Database Syst Rev. (2016) 2016(8):CD008942. doi: 10.1002/14651858.CD008942.pub2
10. Biasucci DG, La Greca A, Scoppettuolo G, Pittiruti M. What’s really new in the field of vascular access? Towards a global use of ultrasound. Intensive Care Med. (2015) 41:731–3. doi: 10.1007/s00134-015-3728-y
11. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF, Emergency C, et al. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. (1996) 2018(12). doi: 10.1002/14651858.CD011447
12. Oulego-Erroz I, González-Cortes R, García-Soler P, Balaguer-Gargallo M, Frías-Pérez M, Mayordomo-Colunga J, et al. Ultrasound-guided or landmark techniques for central venous catheter placement in critically ill children. Intensive Care Med. (2018) 44:61–72. doi: 10.1007/s00134-017-4985-8
13. Shime N, Hosokawa K, MacLaren G. Ultrasound imaging reduces failure rates of percutaneous central venous catheterization in children. Pediatr Crit Care Med. (2015) 16(8):718–25. doi: 10.1097/PCC.0000000000000470
14. de Souza TH, Brandao MB, Nadal JAH, Nogueira RJN. Ultrasound guidance for pediatric central venous catheterization: a meta-analysis. Pediatrics. (2018) 142(5). doi: 10.1542/peds.2018-1719
15. Saugel B, Scheeren TW, Teboul J-L. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Critical Care. (2017) 21(1):225. doi: 10.1186/s13054-017-1814-y
16. Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American society of echocardiography and the society of cardiovascular anesthesiologists. Anesth Analg. (2012) 114(1):46–72. doi: 10.1213/ANE.0b013e3182407cd8
17. Takeshita J, Nishiyama K, Fukumoto A, Shime N. Comparing combined short-axis and long-axis ultrasound-guided central venous catheterization with conventional short-axis out-of-plane approaches. J Cardiothor Vasc An. (2019) 33(4):1029–34. doi: 10.1053/j.jvca.2018.08.005
18. Kiberenge RK, Ueda K, Rosauer B. Ultrasound-guided dynamic needle tip positioning technique versus palpation technique for radial arterial cannulation in adult surgical patients: a randomized controlled trial. Anesth Analg. (2018) 126(1):120–6. doi: 10.1213/ANE.0000000000002261
19. Chen J-Y, Wang L-K, Lin Y-T, Lan K-M, Loh E-W, Chen C-H, et al. Comparing short-, long-, and oblique-axis approaches to ultrasound-guided internal jugular venous catheterization: a meta-analysis of randomized controlled trials. J Trauma Acute Care Surg. (2019) 86(3):516–23. doi: 10.1097/TA.0000000000002158
20. Maitra S, Bhattacharjee S, Baidya DK. Comparison of long-, short-, and oblique-axis approaches for ultrasound-guided internal jugular vein cannulation: a network meta-analysis. J Vasc Access. (2020) 21(2):204–9. doi: 10.1177/1129729819868927
21. Gao Y-B, Yan J-H, Ma J-M, Liu X-N, Dong J-Y, Sun F, et al. Effects of long axis in-plane vs short axis out-of-plane techniques during ultrasound-guided vascular access. Am J Emerg Med. (2016) 34(5):778–83. doi: 10.1016/j.ajem.2015.12.092
22. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. (2009) 151(4):W-65–94. doi: 10.7326/0003-4819-151-4-200908180-00136
23. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343. doi: 10.1136/bmj.d5928
24. Liu W, Tu Z, Liu L, Tan Y. Combined short-and long-axis method for internal jugular vein catheterization in premature newborns: a randomized controlled trial. Acta Anaesth Scand. (2021) 65(3):420–7. doi: 10.1111/aas.13728
25. Takeshita J, Tachibana K, Nakajima Y, Nagai G, Fujiwara A, Hamaba H, et al. Long-axis in-plane approach versus short-axis out-of-plane approach for ultrasound-guided central venous catheterization in pediatric patients: a randomized controlled trial. Pediatr Crit Care Med. (2020) 21(11):e996–e1001. doi: 10.1097/PCC.0000000000002476
26. Keskin H, Keskin F, Aydin P, Guler MA, Ahiskalioglu A. Syringe-free, long-axis in-plane versus short-axis classic out-of-plane approach for ultrasound-guided internal jugular vein catheter placement in critically ill children: a prospective randomized study. J Cardiothor Vasc An. (2021) 35(7):2094–9. doi: 10.1053/j.jvca.2021.03.029
27. Tan Y, Tu Z, Ye P, Xu Y, Ye M, Bai L, et al. Ultrasound guidance for internal jugular vein cannulation in neonates: modified dynamic needle tip positioning short-axis out-of-plane technique versus long-axis in-plane technique, a randomized controlled trial. J Vasc Access. (2022) 23(6):922–9. doi: 10.1177/11297298211015043
28. Takeshita J, Nakajima Y, Tachibana K, Hamaba H, Yamashita T, Shime N. Combined short-axis out-of-plane and long-axis in-plane approach versus long-axis in-plane approach for ultrasound-guided central venous catheterization in infants and small children: a randomized controlled trial. PLoS One. (2022) 17(9):e0275453. doi: 10.1371/journal.pone.0275453
29. Kumar A, Sinha C, Kumar A, Kumari P, Singh K, Sinha AK. Comparison between in-plane and out-of-plane techniques for ultrasound guided cannulation of the left brachiocephalic vein in pediatric population: a randomised controlled trial. Anaesth Crit Care Pain Med. (2023) 42(5):101247. doi: 10.1016/j.accpm.2023.101247
30. Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med. (2003) 10(12):1307–11. doi: 10.1111/j.1553-2712.2003.tb00002.x
31. Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach. Am J Emerg Med. (2010) 28(3):343–7. doi: 10.1016/j.ajem.2008.11.022
32. Takeshita J, Nishiyama K, Fukumoto A, Shime N. Combined approach versus 2 conventional approaches in ultrasound-guided central venous catheterization: a randomized controlled trial. J Cardiothor Vasc An. (2019) 33(11):2979–84. doi: 10.1053/j.jvca.2019.03.051
33. Baidya M, Sinha M, Kumar M, Agrawal N, Ramchandani S, Sandeep G, et al. A randomized study comparing ultrasound-guided internal jugular vein cannulation using two techniques: short-axis out-of-plane with dynamic needle tip positioning versus long-axis in-plane. Cureus. (2024) 16(6):e63004. doi: 10.7759/cureus.63004
34. Mesa BK, Sinha M, Kumar M, Ramchandani S, Dey C, Agrawal N, et al. Radial arterial cannulation by ultrasound-guided dynamic needle-tip positioning using the short-axis out-of-plane approach versus the long-axis in-plane approach: a randomized controlled study. Cureus. (2024) 16(2). doi: 10.7759/cureus.54183
35. Hanif I, Alsuwailem HS, Almazyad MM, Almadani LA, Alenezi RH. Overview on central venous access in pediatric patients; review article. Saudi Med Horizons J. (2023) 3(2):83–9. doi: 10.54293/smhj.v3i2.74
36. AlGhamdi F, AlJoaib N, Aldawood A, AlGhamdi M, AlMulhim A. Comparing short-axis versus long-axis ultrasound-guided techniques for internal jugular vein cannulation: a meta-analysis of clinical outcomes and safety. Australas J Ultrasound Med. (2024) 27(3):149–58. doi: 10.1002/ajum.12385
37. Clemmesen L, Knudsen L, Sloth E, Bendtsen T. Dynamic needle tip positioning–ultrasound guidance for peripheral vascular access. A randomized, controlled and blinded study in phantoms performed by ultrasound novices. Ultraschall Med. (2012) 33(07):E321–E5. doi: 10.1055/s-0032-1312824
38. Hansen M, Juhl-Olsen P, Thorn S, Frederiksen C, Sloth E. Ultrasonography-guided radial artery catheterization is superior compared with the traditional palpation technique: a prospective, randomized, blinded, crossover study. Acta Anaesth Scand. (2014) 58(4):446–52. doi: 10.1111/aas.12299
39. Spencer TR, Pittiruti M. Rapid central vein assessment (RaCeVA): a systematic, standardized approach for ultrasound assessment before central venous catheterization. J Vasc Access. (2019) 20(3):239–49. doi: 10.1177/1129729818804718
40. Brusciano V, Lecce M. Advantages of the use of ultrasound in newborn vascular access: a systematic review. J Ultrasound. (2024) 27(2):203–7. doi: 10.1007/s40477-023-00832-1
Keywords: central venous catheters, vascular access, ultrasonography, pediatrics, meta-analysis
Citation: Lee IK, Lee KH, Han H-j, Choi J, Kim NJ and Kim K (2025) Different axis approaches for ultrasound-guided centrally inserted central catheterization in children: a systematic review and meta-analysis of randomized controlled trials. Front. Surg. 12:1481975. doi: 10.3389/fsurg.2025.1481975
Received: 20 August 2024; Accepted: 10 February 2025;
Published: 24 February 2025.
Edited by:
Maurizio Pacilli, Monash University, AustraliaReviewed by:
Robin Van Der Lee, Radboud University Medical Centre, NetherlandsTimothy R. Spencer, Global Vascular Access, LLC, United States
Copyright: © 2025 Lee, Lee, Han, Choi, Kim and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kyunghoon Kim, am91cm5leTIzN0BzbnUuYWMua3I=
†These authors have contributed equally to this work and share first authorship
 In Kyung Lee
In Kyung Lee Kyeong Hun Lee1,†
Kyeong Hun Lee1,† Kyunghoon Kim
Kyunghoon Kim