- Department of Orthopaedic Hand Surgery, Texas Tech University Health Sciences Center, Lubbock, TX, United States
Background: Tendon repairs often result in adhesion formation which can cause persisting functional deficits. Close proximity of healing tissues increases friction during tendon excursion, often leading to tendon tethering postoperatively. Despite continued improvements in techniques for tendon repairs, there is currently no consensus on the most effective modality to reduce adhesion formation. The VersaWrap Tendon Protector is a bioresorbable hydrogel that is FDA-cleared for use in tendon repair by separating healing tendons from surrounding tissues and improving tendon gliding. We conducted a study to assess the efficacy of VersaWrap in improving clinical outcomes related to adhesions and tethering in tendon repairs involving the hand.
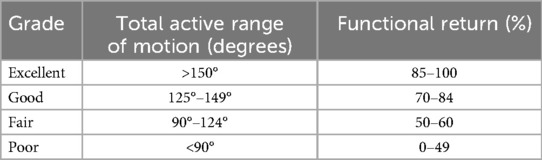
Materials & methods: Age, sex, injury type, mechanism of injury, visual analogue scale (VAS) pain scores, active and passive range of motion (ROM), percent return to normal function, and patient-reported outcomes forms (QuickDASH) were collected at baseline and routine follow up visits. Functional outcomes were classified according to Strickland and Glogovac grading system.
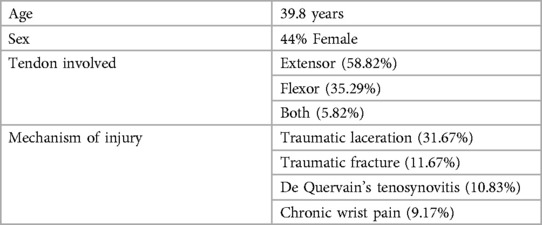
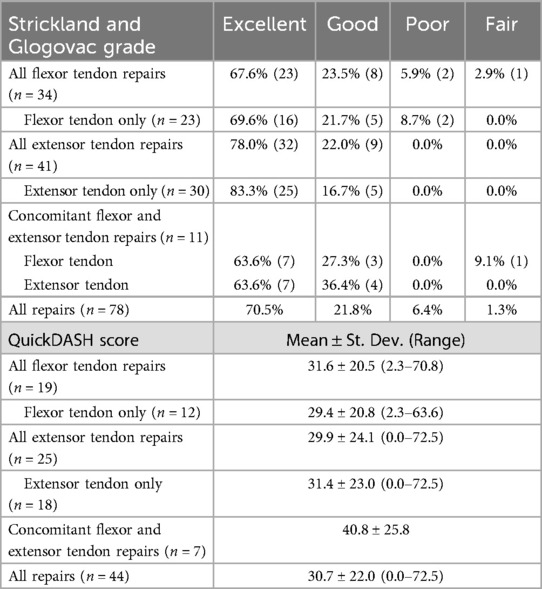
Results: 90 patients were included, with an average age of 39.8 years and a 44% female gender. The most common mechanism of injury was sharp laceration, and the majority of repairs involved the extensor mechanism (58.8% extensor, 35.3% flexor, 5.8% both). At a mean follow-up of 4.6 months, the mean active and passive ROM was 88.8% and 94.3%, respectively. Mean percent return of function was 87.7%. Good or Excellent functional outcomes were achieved in 92.3% of patients – 70.5% Excellent, 21.8% Good, 6.4% Fair, 1.3% Poor. The average QuickDASH score was 30.7, and the average final VAS pain score was 1.3.
Conclusions: Tendon repairs and tenolysis procedures often result in reduced functionality due to impeded tendon gliding, and there is currently no consensus on optimal treatment to prevent tethering to surrounding tissues. The VersaWrap Tendon Protector creates a gelatinous layer between the tendon and surrounding soft tissue to improve gliding resistance, thereby limiting tendon sheath adhesions. Our data suggests that VersaWrap may be a useful adjunct in preventing tendon tethering adhesion post-repair.
1 Introduction
The hands are frequently involved in traumatic and/or chronic injuries, representing up to 30% of presentations to urgent or emergency care centers (1). Tendon injuries are the second most common injury of the hand and can result in long-term disability if not treated appropriately (2, 3). These injuries are thought to be caused by either mechanical (excess loading on tendon) or vascular (loss of blood supply leading to ischemic damage) processes, with athletes and individuals in high-risk occupations such as construction being at a higher risk (4, 5). These injuries can manifest in various forms, such as tendinopathies, tendinosis, and tendinitis, and as such, various treatment methods have been developed to restore patient function (6, 7). The initial approach to treating tendon injuries is typically conservative and includes rest, physical therapy, and medication (2). However, even non-steroidal anti-inflammatory drugs (NSAIDS) and steroids, which are commonly used to relieve pain and inflammation, have shown negative effects on tendon healing in the long term, and are typically used as last resort conservative treatments (4, 8, 9). Alternative treatments, such as transdermal nitric oxide patches, shock wave therapy, and eccentric loading exercises, have also shown promise in treating tendon injuries in which there is not complete rupture or transection (4, 10, 11). In cases where conservative treatment is unsuccessful and in more severe traumatic injuries, surgical intervention is often indicated.
Surgical approaches vary depending on the severity and location of the injury (2). The primary goal of surgery is to achieve intrinsic tendon healing and limit extrinsic scarring, with the ultimate goal of maximizing patient functional outcomes (12). Operative interventions, while often successful, can lead to a high rate of reoperations, with one report showing a 11.4% reoperation rate following flexor tendon repair (12, 13). Surgical procedures may also present with a risk of complications post operation, such as tendon rupture, joint stiffness, poor tendon gliding, and adhesion formation (14, 15).
Adhesion formation and excess scarring are of particular concern, as impairments to gliding and anatomic motion can progress to permanent deficits or the need for reoperation (12, 13). Adhesions can arise from a variety of tissues surrounding the repair, such as dense adhesions arising from the bony floor, loose adhesions arising from subcutaneous tissues, or moderate adhesions arising from the synovial sheath or pulleys (15, 16). It is estimated that adhesions develop in 30% of tendon repairs, and while modified suture techniques such as the Kessler repair method and early mobilization have improved adhesion-related functional deficits to some degree, outcomes of flexor and extensor tendon repairs of the hand remain suboptimal (3, 17, 18).
Recently, novel uses of tissue barriers and pharmacologic agents (both alone and in combination) have been explored as potential adjuncts to adhesions in tendon repair, including hyaluronic acid (HA) preparations, lubricin (also known as proteoglycan 4), di-palmitoyl phosphatidylcholine, 5-flourouracil, celoxumib sheets, and acellular dermal matrix products (19, 20). While some of these have shown potential for reducing adhesions and scarring, the majority of studies have been performed on animal models or in vitro, and their clinical utility in the context of tendon repair has yet to be established (19).
The VersaWrap tendon protector (Alafair BioSciences, Austin, TX, USA) is a plant-based (non-tissue, non-collagenous) bioresorbable hydrogel sheet that was developed to protect tendons, ligaments, skeletal muscle, and peripheral nerve. VersaWrap provides an interface between tissues that reduces friction and prevents tethering (21). In the context of tendon repairs in the hand, we postulated that this product may be a useful adjunct to prevent adhesion formation and scarring in healing tendons, with the ultimate goal of improved tendon gliding. Given the promising early data of VersaWrap as a tendon protector, we designed a study to evaluate the clinical efficacy of VersaWrap in tendon repairs of the hand. Given the unique function of this device in reducing adhesion formation and friction, we hypothesized that tendon repairs utilizing this novel tissue barrier would result in improved functional outcomes.
2 Methods
We performed a retrospective study of patients who underwent surgeries using the VersaWrap tendon protector over a period of 2 years. In all cases, a 2 × 2 inch sheet preparation of VersaWrap (VTP 2201) was cut to the appropriate length and wrapped around the affected zone circumferentially immediately following repair. No adjustments in repair technique were made to facilitate the use of VersaWrap. All procedures were performed by two fellowship trained hand surgeons, each with over 10 years of experience.
Demographic information, injury characteristics, and functional measures were collected, including: age, sex, tendons injured, mechanism of injury, pain scores, disability scores, range of motion, and percent return to normal function. These variables were assessed at baseline and at routine follow-up visits until patients had reached maximal recovery or were lost to follow up. Functional outcomes were further categorized using the Strickland and Glogovac grading system, and disability scores were calculated at final follow up using the Shortened Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire when possible (Tables 1–4) (2, 22). Descriptive statistics were used to evaluate clinical endpoints.
3 Results
In the specified time frame, 120 patients had tenolysis and/or tendon reconstruction with the use of a VersaWrap tendon protector. Patients with follow up <1 month were excluded from analysis. A total of 90 patients were included in the analysis, with an average age of 39.8 years and a 44% female gender. The most common mechanism of injury was sharp laceration, and the majority of repairs involved the extensor mechanism (58.8% extensor, 35.3% flexor, 5.8% both flexor and extensor repairs) (Table 2).
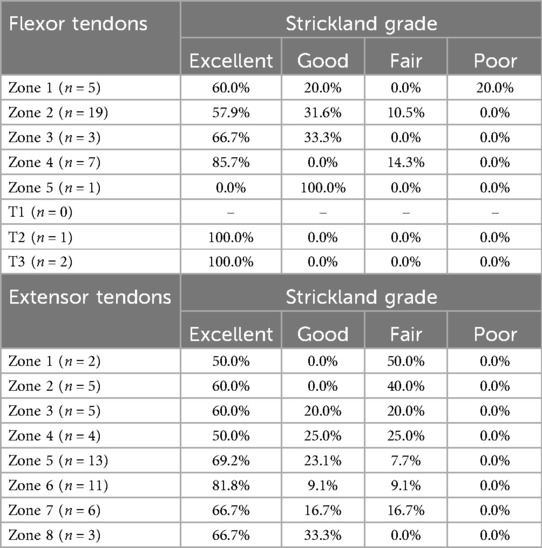
At most recent follow-up (mean: 4.6 months, range: 1.0–19.3), the mean active and passive ROM were 88.8% (n = 66, range: 40%–100%) and 94.3% (n = 53, range: 50%–100%), respectively. The average percent return of function was 87.7% (n = 59, range: 30%–100%). Classification using Strickland and Glogovac criteria showed 92.3% of patients had Good or Excellent functional outcomes (70.5% Excellent, 21.8% Good, 6.4% Fair, 1.3% Poor) (Table 3). The average QuickDASH score was 30.7 (n = 44, range: 0–72.5), and the average pain score on the visual analogue scale (VAS) was 1.3/10 (n = 90, range: 0–8) (Table 3). Outcomes of flexor and extensor tendon repairs classified by zone of involvement can be found in Table 4.
4 Discussion
After tendon injury and/or repair, healing is achieved via extrinsic and intrinsic processes. Extrinsic healing involves a distinctive inflammatory response followed by proliferation and remodeling, in which fibroblasts of the paratenon facilitate migration and may result in adhesion formation, particularly with prolonged immobilization. The intrinsic process is supported by tendon movement and is carried out by “fibroblast-like tenocytes” which produce collagenous tissue and drive remodeling (1). Minimizing the inflammatory response is critical to preventing adhesions and/or excessive scarring surrounding the tendon repair, and early motion is critical to healing and remodeling of the tendon itself. Close proximity of hand tendons to surrounding structures creates an environment favorable for adhesions during the inflammatory stage of healing (1). These adhesions can lead to restricted tendon movement, and once tendon adhesion has developed, it is unlikely that the patient will achieve excellent range of motion.
Recent clinical studies on 315 primary flexor tendon repairs reported that 28% of flexor tendon repairs had only a fair to poor functional recovery, likely as a result of adhesion formation (23). One meta-analysis consolidated 20 major reports over the course of 15 years to track outcomes of flexor tendon repairs in the hand. In this report, Tang et al. found that 4%–10% of repairs ruptured, and 10% developed restrictive adhesion leading to tenolysis or secondary grafting (15).
In a study of 225 primary flexor tendon repairs, “Excellent” or “Good” function was achieved by only 30% of patients at 8 weeks and 48% of patients at final follow-up (minimum 3 months). A systematic review of flexor tendon repairs found rates of “Excellent” or “Good” functional recovery varied from 61%–82% in adult patients (24, 25). In our cohort, 87% of patients achieved “Excellent” or “Good” functional status after flexor tendon repair with the VersaWrap tendon protector (Table 3).
Extensor tendon repairs are often analyzed separately from flexor tendons due to differences in anatomy and their potential effects on prognosis (1). One study reported only 31% improvement in total active motion from tenolysis performed after extensor tendon repair (26). In a study of 101 extensor tendon injuries, Newport et al. reported “Excellent” or “Good” results in 50% of repairs in zones 1–4 and 63%–83% of repairs in zones 5–8 (27). A more recent study of 72 extensor tendon repairs showed “Excellent” or “Good” outcomes in 75% of patients (42% Excellent, 33% Good, 13% Fair, 13% Poor) (28). While attempts have been made to establish prognosis by zone of injury involved, the current literature is conflicted with regard to which zones are likely to have better or worse outcomes (29). In our cohort, 91% of patients achieved “Excellent” or “Good” functional status after extensor tendon repair with the VersaWrap tendon protector (Table 3).
The majority of studies evaluating both flexor and extensor tendon repairs have excluded patients with concomitant injuries such as fractures, complex skin injuries, or revascularisations (23–25, 27–29). Despite including all patients with adequate follow-up, regardless of concomitant injuries or complex reconstruction, our results compare favorably to the historical outcomes of both flexor and extensor tendons of the hand. These findings indicate that the VersaWrap tendon protector may be a valuable adjunct in tendon repairs resulting from a wide variety of injuries.
The present study is not without limitations. Injuries in our cohort varied in terms of mechanism and chronicity of injury. While aggregate outcomes are promising in our cohort, comparative analysis between zones of injury is limited by sample size (Tables 3, 4). Further, there was no control group to provide definitive comparison of VersaWrap vs. non-VersaWrap repairs. Despite these limitations, our study provides valuable data regarding the efficacy of this novel product in improving gliding and preventing complications related to scarring and/or adhesions.
5 Conclusion
Tendon injuries and tendinopathies are a prevalent issue that affects individuals of all ages and backgrounds and can greatly impact a patient's functionality. Functional recovery is often dependent on the degree of scarring and adhesions post-repair. The gelatinous layer provided by VersaWrap between the tendon and surrounding soft tissue reduces friction and improves gliding, thereby limiting the formation of tendon sheath adhesions. Our data suggests that the VersaWrap Tendon Protector may be a useful adjunct in preventing tendon adhesion and excessive scarring, ultimately leading to improved outcomes in patients undergoing tendon repairs of the hand.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The Ethics Committee/Institutional Review Board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this study is a retrospective chart review of treatments that have already been performed. Obtaining individual consent at this point would have been impractical and could have potentially exposed the participants to greater privacy risks. Many patients may no longer have been reachable due to outdated contact information or could be deceased. Additionally, requiring written consent would create a document linking participants to the study, increasing their privacy risk. Therefore, the waiver minimized these risks and allowed the study to proceed without compromising participant privacy.
Author contributions
YA: Writing – original draft, Writing – review & editing. JH: Writing – original draft, Writing – review & editing. CC: Writing – original draft, Writing – review & editing. GB: Writing – original draft, Writing – review & editing. EH: Writing – original draft, Writing – review & editing. BM: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Schöffl V, Heid A, Küpper T. Tendon injuries of the hand. World J Orthop. (2012) 3(6):62–9. doi: 10.5312/wjo.v3.i6.62
2. Rigo IZ, Rokkum M. Predictors of outcome after primary flexor tendon repair in zone 1, 2 and 3. J Hand Surg Eur Vol. (2016) 41(8):793–801. doi: 10.1177/1753193416657758
3. Campbell E, Pillai S, Vamadeva SV, Pahal GS. Hand tendon injuries. Br J Hosp Med (Lond). (2020) 81(11):1–14. doi: 10.12968/hmed.2020.0141
4. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford). (2006) 45(5):508–21. doi: 10.1093/rheumatology/kel046
5. Kane SF, Olewinski LH, Tamminga KS. Management of chronic tendon injuries. Am Fam Physician. (2019) 100(3):147–57.31361101
6. Fares MY, Khachfe HH, Salhab HA, Zbib J, Fares Y, Fares J. Achilles tendinopathy: exploring injury characteristics and current treatment modalities. Foot (Edinb). (2021) 46:101715. doi: 10.1016/j.foot.2020.101715
7. Aicale R, Bisaccia RD, Oliviero A, Oliva F, Maffulli N. Current pharmacological approaches to the treatment of tendinopathy. Expert Opin Pharmacother. (2020) 21(12):1467–77. doi: 10.1080/14656566.2020.1763306
8. Chan KM, Fu SC. Anti-inflammatory management for tendon injuries—friends or foes? Sports Med Arthrosc Rehabil Ther Technol. (2009) 1(1):23. doi: 10.1186/1758-2555-1-23
9. Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clin Orthop Relat Res. (2008) 466(7):1539–54. doi: 10.1007/s11999-008-0260-1
10. Rowe V, Hemmings S, Barton C, Malliaras P, Maffulli N, Morrissey D. Conservative management of midportion achilles tendinopathy: a mixed methods study, integrating systematic review and clinical reasoning. Sports Med. (2012) 42(11):941–67. doi: 10.1007/bf03262305
11. Murrell GA. Using nitric oxide to treat tendinopathy. Br J Sports Med. (2007) 41(4):227–31. doi: 10.1136/bjsm.2006.034447
12. Lilly SI, Messer TM. Complications after treatment of flexor tendon injuries. J Am Acad Orthop Surg. (2006) 14(7):387–96. doi: 10.5435/00124635-200607000-00001
13. Lalchandani GR, Halvorson RT, Zhang AL, Lattanza LL, Immerman I. Patient outcomes and costs after isolated flexor tendon repairs of the hand. J Hand Ther. (2022) 35(4):590–6. doi: 10.1016/j.jht.2021.04.015
14. Griffin M, Hindocha S, Jordan D, Saleh M, Khan W. An overview of the management of flexor tendon injuries. Open Orthop J. (2012) 6:28–35. doi: 10.2174/1874325001206010028
15. Tang JB. Clinical outcomes associated with flexor tendon repair. Hand Clin. (2005) 21(2):199–210. doi: 10.1016/j.hcl.2004.11.005
16. Colzani G, Tos P, Battiston B, Merolla G, Porcellini G, Artiaco S. Traumatic extensor tendon injuries to the hand: clinical anatomy, biomechanics, and surgical procedure review. J Hand Microsurg. (2016) 8(1):2–12. doi: 10.1055/s-0036-1572534
17. Howell JW, Peck F. Rehabilitation of flexor and extensor tendon injuries in the hand: current updates. Injury. (2013) 44(3):397–402. doi: 10.1016/j.injury.2013.01.022
18. Dy CJ, Hernandez-Soria A, Ma Y, Roberts TR, Daluiski A. Complications after flexor tendon repair: a systematic review and meta-analysis. J Hand Surg Am. (2012) 37(3):543–51.e1. doi: 10.1016/j.jhsa.2011.11.006
19. Klifto CS, Capo JT, Sapienza A, Yang SS, Paksima N. Flexor tendon injuries. J Am Acad Orthop Surg. (2018) 26(2):e26–35. doi: 10.5435/jaaos-d-16-00316
20. Lee YJ, Ryoo HJ, Shim HS. Prevention of postoperative adhesions after flexor tendon repair with acellular dermal matrix in zones III, IV, and V of the hand: a randomized controlled (CONSORT-compliant) trial. Medicine (Baltimore). (2022) 101(3):e28630. doi: 10.1097/md.0000000000028630
21. McDermott ER, Bowers Z, Nuelle JA. The application of hyaluronic acid/alginate sheet to flexor pollicis Longus tendon repair to prevent adhesion formation: a second look. Cureus. (2022) 14(12):e33147. doi: 10.7759/cureus.33147
22. Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. (2006) 7:44. doi: 10.1186/1471-2474-7-44
23. Wong JKF, Lui YH, Kapacee Z, Kadler KE, Ferguson MWJ, McGrouther DA. The cellular biology of flexor tendon adhesion formation: an old problem in a new paradigm. Am J Pathol. (2009) 175(5):1938–51. doi: 10.2353/ajpath.2009.090380
24. Wu YF, Tang JB. Recent developments in flexor tendon repair techniques and factors influencing strength of the tendon repair. J Hand Surg Eur Vol. (2014) 39(1):6–19. doi: 10.1177/1753193413492914
25. Giesen T, Sirotakova M, Copsey AJ, Elliot D. Flexor pollicis longus primary repair: further experience with the tang technique and controlled active mobilization. J Hand Surg Eur Vol. (2009) 34(6):758–61. doi: 10.1177/1753193408096025
26. Creighton JJ Jr., Steichen JB. Complications in phalangeal and metacarpal fracture management. Results of extensor tenolysis. Hand Clin. (1994) 10(1):111–6. doi: 10.1016/S0749-0712(21)01038-6
27. Newport ML, Blair WF, Steyers CM. Long-term results of extensor tendon repair. J Hand Surg Am. (1990) 15(6):961–6. doi: 10.1016/0363-5023(90)90024-l
28. Mehdinasab SA, Pipelzadeh MR, Sarrafan N. Results of primary extensor tendon repair of the hand with respect to the zone of injury. Arch Trauma Res. (2012) 1(3):131–4. doi: 10.5812/atr.7859
Keywords: tendon, operative tendon repairs, tendon protector, bioresorbable hydrogel sheet, VersaWrap
Citation: Adu Y, Harder J, Cox C, Baum G, Hernandez EJ and MacKay BJ (2024) Evaluating the effect of VersaWrap tendon protector on functional outcomes in operative tendon repairs. Front. Surg. 11:1447515. doi: 10.3389/fsurg.2024.1447515
Received: 20 June 2024; Accepted: 18 November 2024;
Published: 16 December 2024.
Edited by:
Francesco De Francesco, Independent Researcher, Ancona, ItalyReviewed by:
Fatih Zor, Wake Forest University, United StatesMohammad El Khatib, University of Teramo, Italy
Copyright: © 2024 Adu, Harder, Cox, Baum, Hernandez and MacKay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brendan J. MacKay, YnJlbmRhbi5qLm1hY2theUB0dHVoc2MuZWR1
 Yaw Adu
Yaw Adu Justin Harder
Justin Harder Gracie Baum
Gracie Baum Evan J. Hernandez
Evan J. Hernandez Brendan J. MacKay
Brendan J. MacKay