- 1Service de Chirurgie Orthopédique et Traumatology de L’appareil Locomoteur, Hopitaux Universitaires de Genève, Genève, Switzerland
- 2Unité d’orthopédie et Traumatology Pédiatrique, Hopitaux Universitaires de Genève, Genève, Switzerland
- 3Servizio di Chirurgia e Ortopedia Pediatrica, Bellinzona, Switzerland
The shear fractures of the capitellum are rare fractures in the pediatric population. Their diagnosis is challenging because of the high cartilaginous component of the growing elbow, requiring a high level of clinical suspicion especially in the case of small osteochondral or chondral fragments. The literature on capitellar shear fractures is mainly represented by case reports, which provides a patchy view of the topic. For this reason, we aimed to draw a narrative review presenting the available management strategies and their outcomes, and present two cases treated in our institution.
1 Introduction
The shear fractures of the capitellum are rare fractures both in children and adult patients. Due to the anatomical features of the elbow, their diagnosis can be often missed or delayed. For this reason, in the pediatric literature, these fractures have been grouped among the so-called TRASH injuries, an acronym that stands for “The Radiographic Appearance Seemed Harmless”, including also osteochondral fractures of the radial head and lateral condyle, incarcerated medial epicondylar and unossified medial condylar fractures, transphyseal separations of the distal humerus, and Monteggia lesions (1). The anatomy of the pediatric elbow is characterized by six ossification centers, merged in radio-transparent physes, which fuse during adolescence in a sequential order, beginning from the capitellum, trochlea and olecranon around the age of 14 (2). Consequently, any injury before the fusion of the ossification centres can cause chondral or osteochondral fragments that can be missed on radiographs, especially if small in size.
Capitellar shear fractures account for less than 1% of elbow fractures in both pediatric and adult patients (3–7). In children, they usually affect adolescents around the age of 14, just before the fusion of the ossification centre (8, 9). These fractures are generated by an axial load towards the humeral paddle with an elbow in extension or semiflexion, as in a fall on the outstretched arm (10–12). Depending on the flexion or extension of the elbow at injury, the fracture fragment can be anterior or posterior. These fractures can also be generated by a posterolateral elbow dislocation or subluxation, due to the impact of the radial head and coronoid against the capitellum (10–12). Even though in many cases they are isolated, the capitellar shear fractures can be associated with other injuries of the lateral column, such as radial head or neck fractures, lateral condyle fractures, lateral collateral ligament complex avulsion, but also medial condyle and olecranon fractures (13).
There are two main classifications of capitellar shear fractures in use for children and adults, the modified Bryan-Morrey and Dubberley (4, 14). The Bryan-Morrey classification distinguishes these injuries into three types, mainly depending on the fracture size of the fragment (4). Type 1, also called Hahn-Steinthal fracture, is an isolated fracture of the capitellum, characterized by a single fracture fragment including both the chondral and subchondral component of the capitellum, eventually extended to the lateral trochlear ridge. Type 2, the Kocher-Lorenz fracture, is a thin articular cartilage fragment of the capitellum. Type 3, also called Broberg-Morrey fracture, has the same extension as Type 1 but is comminuted. McKee added a fourth type to the Bryan-Morrey classification, that extends up to the trochlear groove (4).
Dubberley classified capitellar fractures into three types, differentiated by the extension in the trochlea, each one distinguished in type A and B, according to a more anterior or posterior involvement of the capitellum on the sagittal plane (14). In this classification, Type 1 is like a Hahn-Stenthal fracture, involving the lateral trochlear ridge, Type 2 describes a capitellar fragment that extends in the trochlear groove, and Type 3 is comminuted, with at least a capitellar and a trochlear fragment.
Due to the anatomy and the timing for the ossification of the pediatric elbow, the capitellar shear fracture diagnosis can be missed or delayed. In clinical practice, distinguishing these patterns of injuries requires not only a radiological diagnosis but also high clinical suspicion. The reason stands in the high cartilaginous component of the pediatric elbow, making impossible a direct radiographic diagnosis of small chondral fragments. Radiographs rather show a double contour sign, when the fracture involves the subchondral bone or just a fat pad sign in the case of a small chondral fragment (11). What leads clinicians to further investigate the injured elbow is the clinical appearance of a swollen and tender elbow, eventually accompanied by hematoma. The limitation of motion is not only related to pain but also to a mechanical blockage of the elbow amplitude related to the interposition of the fragment. In these cases, investigations are usually pursued with a computed tomography scan (CT) or magnetic resonance imaging (MRI) of the elbow, to characterize the fracture pattern and plan the surgery. The surgical approach and osteosynthesis or fragment excision are planned based on the imaging, leaving margins for the intraoperative adaptation of the strategy. Since there is no consensus on the best management, we aimed to describe two cases treated in our institution and provide a narrative review of available pediatric literature.
1.1 Case report
After approval by the local ethics committee, we retrospectively reviewed the charts of patients who accessed the Pediatric Emergency Service from January 2010 to December 2023 for traumas of the upper limbs. The age limit for admission to pediatric care in Switzerland is 16 years. Two patients with a capitellar shear fracture of the elbow were retrieved and are here described.
1.2 Case 1
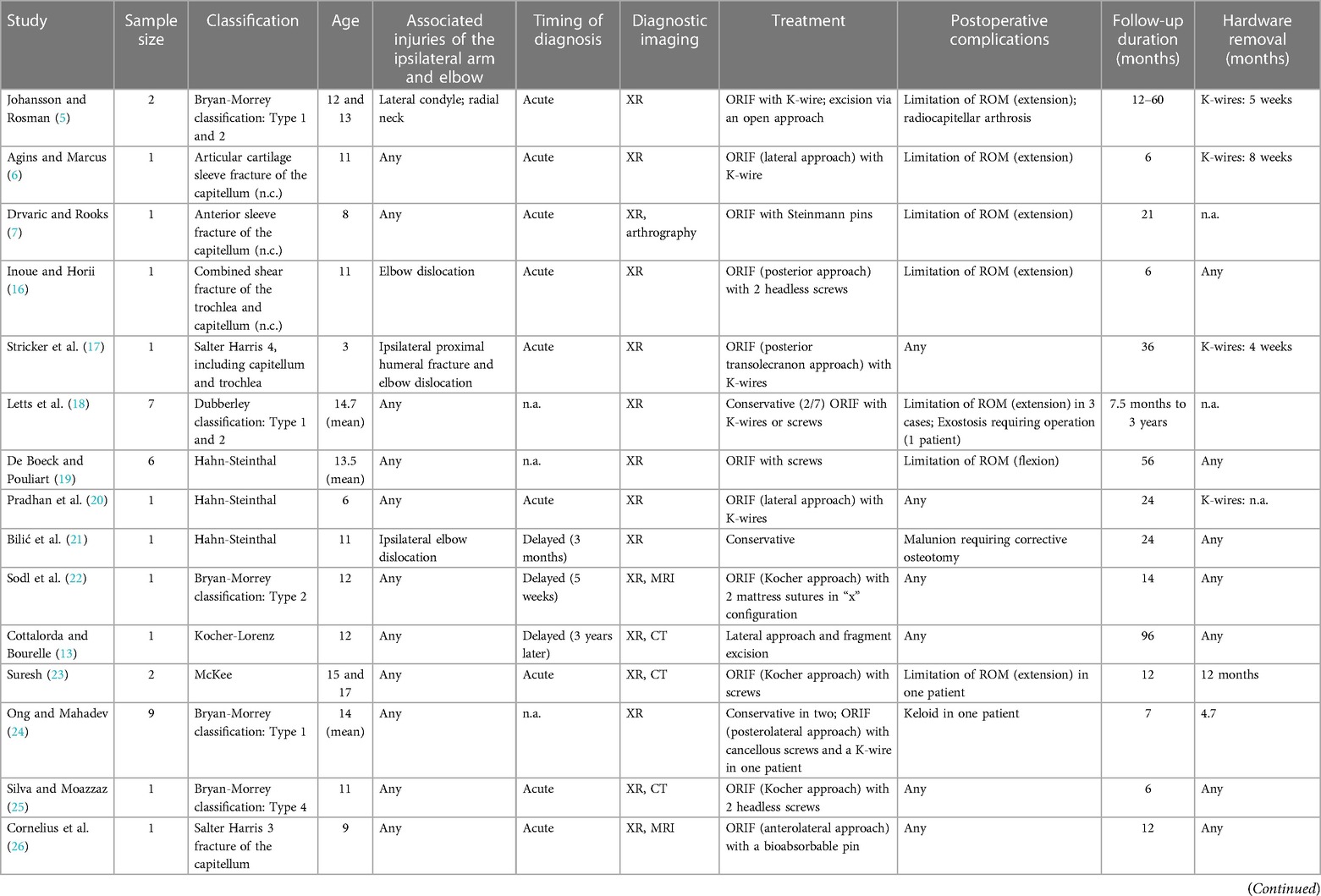
An 11-year-old female fell from the horse, with a trauma to her left upper limb and abdomen. The patient complained of pain in her left elbow and renal lodge. At the emergency department, the radiographs of the left elbow showed a double contour sign and a bone age of 12.5 years according to the Sauvegrain method (15). The elbow was then temporarily immobilized in a soft splint and a CT scan was scheduled. The blood and urinary test as well as an abdominal ultrasound allowed to exclude any renal or visceral injury. The CT scan of the elbow showed a shear fracture of the capitellum involving the lateral trochlear ridge, a Hahn-Steinthal fracture, with proximal and medial displacement. The surgery was scheduled for the following day. Through an anterolateral approach with distal anterior extension, through a deep plane between the brachioradialis and pronator teres, the fracture was exposed and prepared. The fracture was reduced and fixed by two K-wires, that guided the insertion of two headless cortical screws taking care to bury their anterior extremity. The intraoperative radioscopic check showed an adequate reduction and correct screw length, also confirmed by the postoperative radiographs. The elbow was immobilized in a brachioantebrachial (BAB) cast for 10 days. The postoperative follow-up lasted one year. The recovery occurred without complications, with a gradual improvement of the range of motion, requiring physiotherapy, and evidence of bone union at 2 postoperative months. At the final follow-up, the range of motion of the left elbow was identical to the right one (Figure 1).
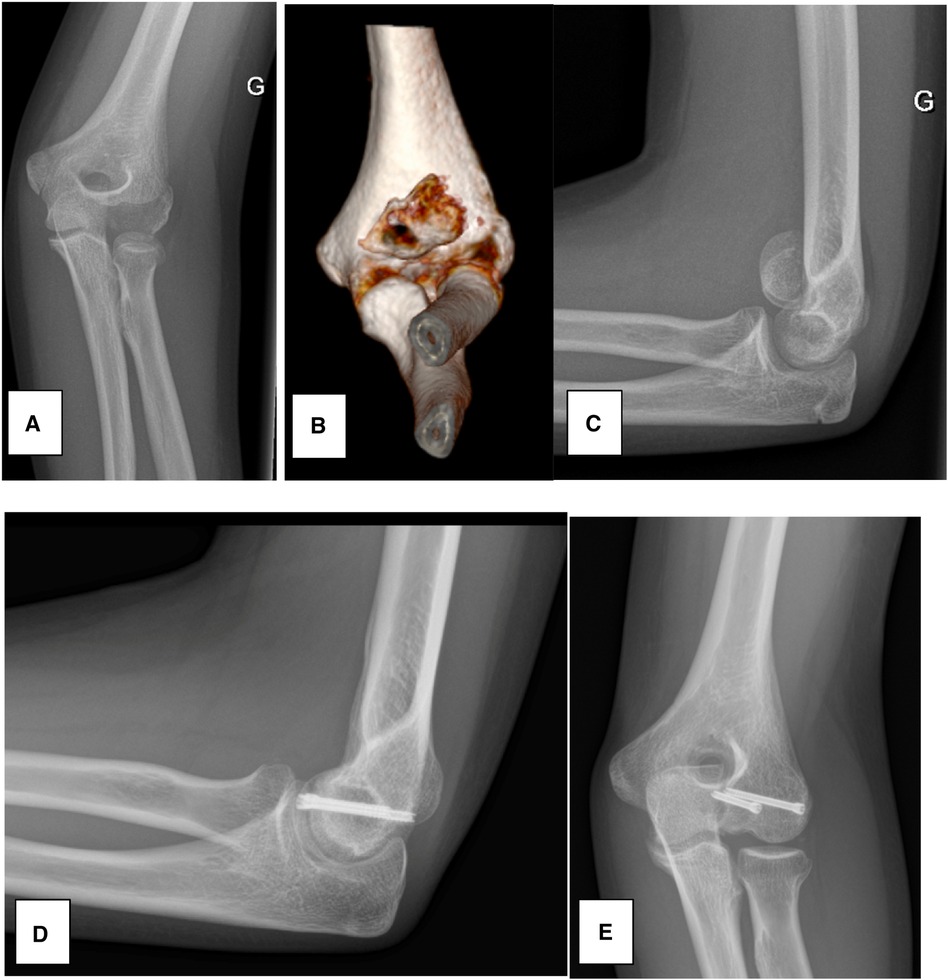
Figure 1 Case 1. (A) AP radiograph at admission. (B) 3D CT-scan showing the capitellar shear fracture, displaced towards proximal and medial. (C) Lateral radiograph at admission, showing the displaced capitellar shear fracture. (D,E) AP and lateral of the 1-year follow-up.
1.3 Case 2
This is the case of an 11-year-old female who fell from monkey bars at school, with a trauma of her right upper limb. As she arrived at the emergency, she complained of pain in her right elbow, which appeared swollen and tender, and showed a reduced range of motion. The radiographs showed a double contour sign and a 12.5-year bone age according to the Sauvegrain method (15). The CT scan showed a McKee fracture extending up to the trochlear groove, with proximal and lateral displacement. The patient was hospitalized and surgery was scheduled for the following day. The fracture was approached by an anterolateral approach, reduced and fixed by two K-wires, whose extremities were kept subcutaneously at the closure. The elbow was immobilized in a BAB cast for 4 weeks when the K-wires were removed. At 10 postoperative weeks, the patient achieved a full range of motion and was allowed to gradually begin sportive activities. The radiographs showed the union of the fracture. The follow-up is still ongoing, with a planned consultation and 6 and 12 postoperative months (Figure 2).
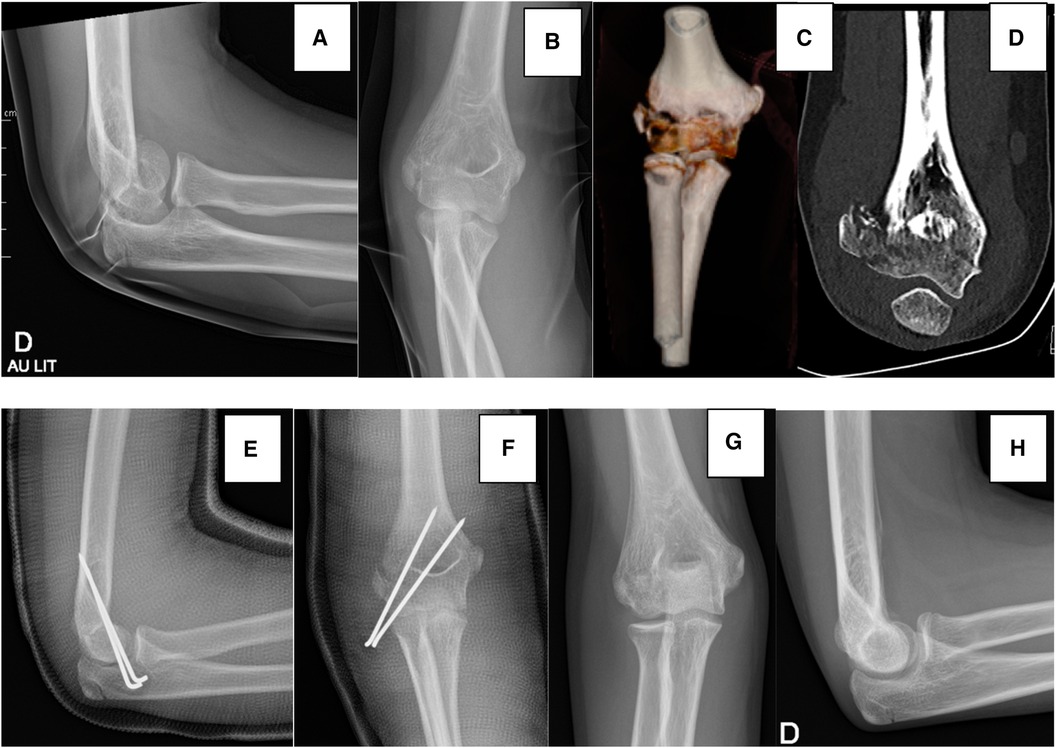
Figure 2 Case 2. (A) Lateral radiograph at admission, showing the double contour sign, (B) AP radiograph at admission. (C) 3D CT-scan showing the extension of the fracture towards the trochlear groove. (D) Coronal slice of the CT-scan showing the lateral displacement of the fragment. (E,F) Postoperative radiographs. (G,H) 2-month follow-up radiographs.
2 Discussion
We carried out a narrative review of the pediatric literature for capitellar shear fractures (shown in Table 1). Most of the literature consists of case reports (5–8, 13, 16, 17, 20–23, 25–27, 29–31, 33, 38), followed by a smaller number of retrospective case series (9, 18, 19, 24, 28, 32, 34–37). The retrieved literature showed a bimodal distribution of these fractures, with a first peak in childhood (<10 years) (7, 17, 20, 31) and a second one, the most representative, in pre-adolescents and adolescents (5–9, 13, 16, 18, 19, 21–25, 27–30, 32–38). The most frequent associated injury was the ipsilateral elbow dislocation, followed by the involvement of the medial or lateral condyle, or an olecranon or radial head fracture (5, 16, 17, 21, 31, 37, 38).
The radiographs are the baseline exam for diagnosis, accompanied by a clinical suspicion. Before the advent of CT and MRI, arthrography was perioperatively used in selected cases or oblique radiographs were carried out to better visualize the fragments (7, 20). The use of CT and MRI has improved the diagnosis of capitellar shear fractures, allowing us to visualize them early and plan the treatment. According to the time elapsed between the accident and the management, it is possible to distinguish between fractures that are diagnosed early in the acute post-traumatic period or whose diagnosis is delayed. The availability of CT and MRI, within the first weeks from the injury, allowed setting a threshold of two weeks between the acute and delayed diagnosis (36). In fact, in most of the studies on the delayed finding of capitellar shear fractures, the diagnosis was stated between five post-traumatic weeks up to three years, with most of the cases between 3 and 6 months from the accident (8, 13, 21, 22, 30, 37).
As far as the classification is concerned, the most used one was the Bryan-Morrey, followed by the Dubberley. A few studies published in the 80ies and 90ies were rather descriptive in the definition of the fracture or used the Salter-Harris classification (6, 7, 16, 17). An orthopedic surgery team from Harvard provided their classification, based on the sagittal appearance of the capitellar shear fractures (9). By reversing the perspective provided by Dubberley, they proposed a classification distinguishing between anterior (Type 1) and posterior (Type 2) osteochondral fractures of the capitellum and chondral fractures (Type 3) (9). The perspectives offered by the mentioned classifications open the discussion for surgical planning. One of the most important elements for the planification of the surgical approach is a coronal extension of the fracture and any associated injury requiring surgical management (13, 18). The available literature shows that the most used approach is the lateral, especially through the Kocher interval between the anconeus and extensor carpi ulnaris (also called the posterolateral approach) (39). This allows a good exposure of both posterior and anterior fractures of the capitellum. For most anterior fractures, the options are the lateral approach through the Kaplan interval, between extensor carpi radialis brevis and extensor digitorum communis, but in rare cases also the anterior and anterolateral approach, especially for large fragments anteriorly displaced and with medial extension or in case of associated injuries to the lateral column (13, 18). To a lesser extent, also bilateral approaches or the posterior (eventually transolecranon) approach have been used (16, 17, 32, 36, 37).
The most used devices for osteosynthesis are screws and Kirschner wires. The latter were usually percutaneously fixed, allowing the removal between three to eight postoperative weeks (5, 6, 17, 20, 33). The headless screws, put on the sagittal plane of the fractures, have taken the place of the cancellous screws, not requiring another surgery for hardware removal, and being well tolerated in most of the cases. Some authors have also used osteosuture (22) or bioabsorbable pins (26, 35, 37). In the case of small fragments generating a mechanical blockage in the joint, whose size does not allow any fixation, these fractures are accessible for excision by an open or even arthroscopic approach (9). Finally, capitellar shear fractures can also be accessible to the conservative treatment for non-displaced fractures (9, 18, 21, 24, 30). In brief, the surgical indication lies in a symptomatic displaced fracture of the capitellum, where the most relevant determinant for surgical management is a mechanical blockage to the elbow range of motion.
When considering the timing of diagnosis, most of the cases with a prompt diagnosis were managed with open reduction and internal fixation. This was probably related to the fact that the fractures characterized by a remarkable displacement were promptly diagnosed on conventional radiographs. The fractures whose diagnosis was delayed were susceptible to all treatment strategies, from a conservative attitude when the clinical status allowed, rather than fragment excision or fixation (8, 13, 21, 22, 30).
In many cases, the treatment allows good and uneventful clinical and radiological outcomes. Among the postoperative complications, we can distinguish between the clinical manifestations with limitation of function, especially extension, persistent pain and even blockage. On one hand, the limitations to the elbow amplitudes can be related to soft tissue contractures, eligible for arthrolysis when the functional arc of motion is affected. On the other, pain and blockage can be the epiphenomenon of radiocapitellar osteoarthritis, capitellar necrosis and, in rare cases, loose fragments or cartilage defects, requiring surgical management (5, 9, 21, 30, 32, 36, 37). When distinguishing between the early and delayed diagnosis, the available literature showed that there was not a propensity for radiocapitellar osteoarthritis and capitellar necrosis in delayed cases, but these seemed to be equally distributed. One case of malunion requiring a corrective osteotomy was also described in the literature (21).
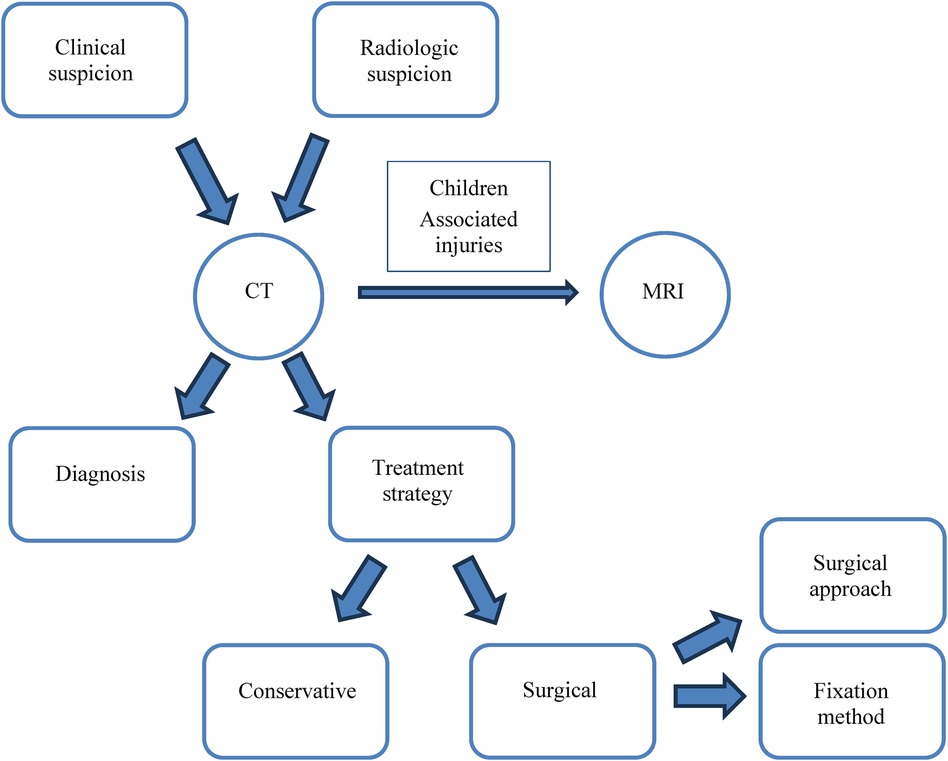
Our case report showed the story of two adolescents with a capitellar shear fracture Type 1 and 4 according to Bryan-Morrey classification, surgically treated with open reduction and internal fixation by headless screws and K-wires, respectively, with complete recovery of function and radiological union at follow-up. According to our experience and the review of the literature, the diagnostic and therapeutic work-up of the pediatric shear fractures of the capitellum starts with a clinical and radiologic suspicion, based on the double contour sign or indirect signs of elbow injury (joint effusion, soft tissue edema) on standard radiographs. In pre-adolescents and adolescents, the diagnostics should be pursued to the CT, which not only allows the confirmation of the diagnosis, but also the choice of the treatment strategy, conservative or surgical. The CT scan also provides relevant information as the site where the fragment is displaced, which will guide the choice of the surgical approach, and its size, useful in the planning of the fixation method (Figure 3). The CT scanner is more widely available compared to MRI, that should be used for children due to the higher cartilaginous component, or in pre-adolescents and adolescent to clear associated injuries (ligamentous lesions, for instance).
The narrative review is limited by the impossibility of drawing statistical conclusions due to the predominance of case reports in the pediatric literature. The predominance of case reports has justified the performance of a narrative review rather than a systematic one. The description of complications and sequelae could be affected by the follow-up time of individual studies, varying between 4.5 months to 8 years. The limitation of retrospective case reports or case series are mainly represented by the recall and selection bias as well as the missing data related to the retrospective collection. To overcome these limitations, future research should rather aim to produce prospective studies, testing clinical guidelines and collecting predetermined clinical-radiologic variables and outcome measures, in the setting of multicenter studies. These data could aid to clearly define the diagnostic strategy that avoids the delayed diagnosis and treatment of these fractures, and standardize their management.
The interest in pediatric capitellar shear fractures lies not only in their challenging diagnosis and treatment but also in the sequelae that can develop and their further management. Future research should prospectively study these pediatric fractures, not only to draw decisional trees but also to find out the predictors of outcome, especially for the development of severe sequelae such as radiocapitellar osteoarthritis and osteonecrosis of the capitellum.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the minor’s legal guardians for the publication of any potentially identifiable images or data included in this article.
Author contributions
J-MP: Conceptualization, Writing – original draft, Writing – review & editing, Methodology. SV: Conceptualization, Writing – original draft, Writing – review & editing, Methodology. GD: Writing – review & editing, Supervision. OV: Writing – review & editing, Supervision. VD: Writing – review & editing, Supervision. MM: Writing – review & editing, Supervision. GD: Writing – review & editing, Supervision. RD: Conceptualization, Writing – original draft, Methodology, Writing – review & editing. DC: Conceptualization, Writing – original draft, Methodology, Writing – review & editing. CS: Conceptualization, Writing – original draft, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Open access funding by University of Geneva.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Waters PM, Beaty J, Kasser J. Elbow “tRASH” (the radiographic appearance seemed harmless) lesions. J Pediatr Orthop. (2010) 30(Suppl 2).
2. Jauregui JJ, Abzug JM. Anatomy and development of the pediatric elbow. In: Abzug JM, Herman MJ, Kozin S, editors. Pediatric Elbow Fractures. Cham, Switzerland: Springer International Publishing AG (2018). p. 3–12.
3. Ravishankar MR, Kumar MN, Raut R. Choice of surgical approach for capitellar fractures based on pathoanatomy of fractures: outcomes of surgical management. Eur J Orthop Surg Traumatol. (2017) 27(2). doi: 10.1007/s00590-016-1877-5
4. Bryan R, Morrey B. Fractures of the distal humerus. In: Morrey B, editor. The Elbow and its Disorders. Philadelphia: WB Saunders (1985). p. 325–33.
5. Johansson J, Rosman M. Fracture of the capitulum humeri in children: a rare injury, often misdiagnosed. Clin Orthop Relat Res. (1980) 146:157–60. doi: 10.1097/00003086-198001000-00022
6. Agins HJ, Marcus NW. Articular cartilage sleeve fracture of the lateral humeral condyle capitellum: a previously undescribed entity. J Pediatr Orthop. (1984) 4(5):620–2. 6490888.6490888
7. Drvaric DM, Rooks MD. Anterior sleeve fracture of the capitellum. J Orthop Trauma. (1990) 4(2):188–92. doi: 10.1097/00005131-199004020-00016
8. Nagda TV, Vaidya SV, Pinto DA. Chondral shear fracture of the capitellum in adolescents—a report of two late diagnosed cases and a review of literature. Indian J Orthop. (2020) 54(Suppl 2):403–7. doi: 10.1007/s43465-020-00197-1
9. Murthy PG, Vuillermin C, Naqvi MN, Waters PM, Bae DS. Capitellar fractures in children and adolescents. J Bone Joint Surg Am. (2017) 99(15):1282–90. doi: 10.2106/JBJS.16.01393
10. Faber KJ. Coronal shear fractures of the distal humerus: the capitellum and trochlea. Hand Clin. (2004) 20(4):455–64. doi: 10.1016/j.hcl.2004.08.001
11. Lee JJ, Lawton JN. Coronal shear fractures of the distal humerus. J Hand Surg Am. (2012) 37(11):2412–7. doi: 10.1016/j.jhsa.2012.09.001
12. Fram BR, Seigerman DA, Ilyas AM. Coronal shear fractures of the distal humerus: a review of diagnosis, treatment, and outcomes. Hand. (2021) 16(5):577–85. doi: 10.1177/1558944719878817
13. Cottalorda J, Bourelle S. The often-missed Kocher-Lorenz elbow fracture. Orthop Traumatol Surg Res. (2009) 95(7):547–50. doi: 10.1016/j.otsr.2009.07.010
14. Dubberley JH, Faber KI, MacDermid JC, Patterson SD, King GJW. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am. (2006) 88(1):46–54. doi: 10.2106/JBJS.D.02954
15. Diméglio A, Charles YP, Daures JP, De Rosa V, Kaboré B. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am. (2005) 87(8):1689–96. doi: 10.2106/JBJS.D.02418
16. Inoue G, Horii E. Combined shear fractures of the trochlea and capitellum associated with anterior fracture-dislocation of the elbow. J Orthop Trauma. (1992) 6(3):373–5. doi: 10.1097/00005131-199209000-00018
17. Stricker SJ, Thomson JD, Kelly RA. Coronal-plane transcondylar fracture of the humerus in a child. Clin Orthop Relat Res. (1993) (294):308–11. 8358934.
18. Letts M, Rumball K, Bauermeister S, McIntyre W, D’Astous J. Fractures of the capitellum in adolescents. J Ped Orthop. (1997) 17(3):315–20. 9150018.
19. De Boeck H, Pouliart N. Fractures of the capitellum humeri in adolescents. Int Orthop. (2000) 24(5):246–8. doi: 10.1007/s002640000160
20. Pradhan BB, Bhasin D, Krom W. Capitellar fracture in a child: the value of an oblique radiograph. A case report. J Bone Joint Surg Am. (2005) 87(3):635–8. doi: 10.2106/JBJS.B.2887pp
21. Bilić R, Kolundžić R, Antičević D. Absorbable implants in surgical correction of a capitellar malunion in an 11-year-old: a case report. J Orthop Trauma. (2006) 20(1):66–9. doi: 10.1097/01.bot.0000161541.14103.67
22. Sodl JF, Ricchetti ET, Huffman GR. Acute osteochondral shear fracture of the capitellum in a twelve-year-old patient: a case report. J Bone Joint Surg Am. (2008) 90(3):629–33. doi: 10.2106/JBJS.G.00017
23. Suresh SS. Type 4 capitellum fractures: diagnosis and treatment strategies. Indian J Orthop. (2009) 43(3):286–91. doi: 10.4103/0019-5413.53460
24. Ong KL, Mahadev A. Cannulated cancellous screw fixation for capitellum fractures in adolescents. J Orthop Surg (Hong Kong). (2011) 19(3):346–9. doi: 10.1177/230949901101900317
25. Silva M, Moazzaz P. Coronal shear fracture of the distal humerus in an 11-year-old patient. J Ped Orthop B. (2011) 20(1):50–5. doi: 10.1097/BPB.0b013e32833cb784
26. Cornelius AL, Bowen TR, Mirenda WM. Anterolateral approach for an unusual pediatric capitellar fracture: a case report and review of the literature. Iowa Orthop J. (2012) 32:215–9. 23576943; 3565404.23576943
27. Gonçalves Pestana JA, MacEdo França AP, Cunha Freitas APT, Jales BT, Alves C, Ferreira F, et al. An unusual case of an isolated capitellar fracture of the right elbow in a child: a case report. J Med Case Rep. (2012) 6:57. doi: 10.1186/1752-1947-6-57
28. Kurtulmus T, Saglam N, Saka G, Avci CC, Kucukdurmaz F, Akpinar F. Posterior fixation of type IV humeral capitellum fractures with fully threaded screws in adolescents. Eur J Trauma Emerg Surg. (2014) 40(3):379–85. doi: 10.1007/s00068-013-0332-0
29. Dressler HB, de Paula RNB. Bryan and Morrey type IV intra-articular fracture of the distal extremity of the humerus treated surgically with anterior access: case report. Rev Bras Ortop. (2015) 50(3):352–5. doi: 10.1016/j.rboe.2015.04.008
30. Frank JM, Saltzman BM, Garbis N, Cohen MS. Articular shear injuries of the capitellum in adolescents. J Shoulder Elbow Surg. (2016) 25(9):1485–90. doi: 10.1016/j.jse.2016.03.013
31. Fuad M, Elmhiregh A, Motazedian A, Bakdach M. Capitellar fracture with bony avulsion of the lateral collateral ligament in a child: case report. Int J Surg Case Rep. (2017) 36:103–7. doi: 10.1016/j.ijscr.2017.04.026
32. Onay T, Gümüştaş SA, Baykan SE, Akgülle AH, Erol B, Irgit KS. Mid-term and long-term functional and radiographic results of 13 surgically treated adolescent capitellum fractures. J Ped Orthop. (2018) 38(8):e424–8. doi: 10.1097/BPO.0000000000001208
33. Papamerkouriou YM, Tsoumpos P, Tagaris G, Christodoulou G. Type IV capitellum fractures in children. BMJ Case Rep. (2019) 12(8):e229957. doi: 10.1136/bcr-2019-229957
34. Ju L, Jiang L, Zhang Y, Wu J, Li M, Liu X, et al. Therapeutic analysis of Herbert screw fixation for capitellar fractures via the anterior approach in adolescent patients. J Orthop Surg Res. (2021) 16(1):394. doi: 10.1186/s13018-021-02536-w
35. Wiktor Ł, Tomaszewski R. Humeral capitellum fractures in adolescents: a study of 6 cases treated by open reduction and internal fixation with bioabsorbable nails. Adv Orthop. (2022) 2022:4012125. doi: 10.1155/2022/4012125
36. Kraus R, Lieber J, Schwerk P, Rüther H, Tüshaus L, Karvouniaris N, et al. Incidence, treatment techniques, and results of distal humeral coronal shear fractures in children and adolescents-a multicenter study of the German section of pediatric traumatology (SKT). Eur J Trauma Emerg Surg. (2023). doi: 10.1007/s00068-023-02370-1 [Epub ahead of print]37815546
37. Simanovski N, Horowitz RS, Goldman V, Sharabati T, Lamdan R, Zaidman M. Capitellum and capitellar-trochlear shear injury in children. J Orthop Trauma. (2023) 37(2):e68–72. doi: 10.1097/BOT.0000000000002471
38. Cao C, Xing H, Cao F, Du Z, Wang G, Wang X. Three-dimensional printing designed customized plate in the treatment of coronal fracture of distal humerus in teenager: a case report. Medicine (United States). (2023) 102(2):e32507. doi: 10.1097/MD.0000000000032507
39. Kloen P, Ring D. Lateral Approach to the Proximal Forearm. Available online at: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-forearm/approach/lateral-approach (Accessed March 24, 2024).
Keywords: capitellum, fracture, pediatric, osteosynthesis, shear fracture
Citation: Pilotto J-M, Valisena S, De Marco G, Vazquez O, De Rosa V, Mendoza Sagaon M, De Coulon G, Dayer R, Ceroni D and Steiger C (2024) Shear fractures of the capitellum in children: a case report and narrative review. Front. Surg. 11:1407577. doi: 10.3389/fsurg.2024.1407577
Received: 26 March 2024; Accepted: 18 June 2024;
Published: 4 July 2024.
Edited by:
Yuan Zhang, Children’s Hospital of Chongqing Medical University, ChinaReviewed by:
Ignacio Sanpera, Hospital Universitario Son Espases, SpainDaniel Robert Schlatterer, WellStar Health System, United States
© 2024 Pilotto, Valisena, De Marco, Vazquez, De Rosa, Mendoza Sagaon, De Coulon, Dayer, Ceroni and Steiger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvia Valisena, c2lsdmlhLnZhbGlzZW5hQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Jean-Marc Pilotto
Jean-Marc Pilotto Silvia Valisena
Silvia Valisena Giacomo De Marco
Giacomo De Marco Oscar Vazquez
Oscar Vazquez Vincenzo De Rosa
Vincenzo De Rosa Mario Mendoza Sagaon
Mario Mendoza Sagaon Geraldo De Coulon
Geraldo De Coulon Romain Dayer2
Romain Dayer2 Dimitri Ceroni
Dimitri Ceroni Christina Steiger
Christina Steiger