
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 15 March 2024
Sec. Neurosurgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1386887
This article is part of the Research TopicTraining and Education in Neurosurgery: Strategies and Challenges for the Next Ten Years, volume IIView all 11 articles
 Camilla de Laurentis1,2
Camilla de Laurentis1,2 David Pirillo2
David Pirillo2 Andrea Di Cristofori1,2
Andrea Di Cristofori1,2 Alessandro Versace2
Alessandro Versace2 Tommaso Calloni1,3
Tommaso Calloni1,3 Andrea Trezza2
Andrea Trezza2 Valentina Villa4
Valentina Villa4 Lucia Alberti4
Lucia Alberti4 Angelo Baldo1,2
Angelo Baldo1,2 Federico Nicolosi1
Federico Nicolosi1 Giorgio Carrabba1,2
Giorgio Carrabba1,2 Carlo Giussani1,2*
Carlo Giussani1,2*
Background: Recently, non-technical skills (NTS) and teamwork in particular have been demonstrated to be essential in many jobs, in business as well as in medical specialties, including plastic, orthopedic, and general surgery. However, NTS and teamwork in neurosurgery have not yet been fully studied. We reviewed the relevant literature and designed a mock surgery to be used as a team-building activity specifically designed for scrub nurses and neurosurgeons.
Methods: We conducted a systematic review by searching PubMed (Medline) and CINAHL, including relevant articles in English published until 15 July 2023. Then, we proposed a pilot study consisting of a single-session, hands-on, and cadaver-free activity, based on role play. Scrub nurses were administered the SPLINTS (Scrub Practitioners’ List of Intraoperative Non-Technical Skills) rating form as a self-evaluation at baseline and 20–30 days after the simulation. During the experiment, surgeons and scrub nurses role-played as each other, doing exercises including a simulated glioma resection surgery performed on an advanced model of a cerebral tumor (Tumor Box, UpSurgeOn®) under an exoscope. At the end, every participant completed an evaluation questionnaire.
Results: A limited number of articles are available on the topic. This study reports one of the first neurosurgical team-building activities in the literature. All the participating scrub nurses and neurosurgeons positively evaluated the simulation developed on a roleplay. The use of a physical simulator seems an added value, as the tactile feedback given by the model further helps to understand the actual surgical job, more than only observing and assisting. The SPLINTS showed a statistically significant improvement not only in “Communication and Teamwork” (p = 0.048) but also in “Situation Awareness” (p = 0.031).
Conclusion: Our study suggests that team-building activities may play a role in improving interprofessional teamwork and other NTS in neurosurgery.
In recent years, non-technical skills (NTS) have been shown to play a pivotal role in every type of job. Not only should workers have and train in specific technical skills, they should also demonstrate and refine their interpersonal skills, such as efficient communication, leadership, and collaboration and teamwork, as well as their cognitive skills, represented by flexibility and coping attitudes, awareness of the situation, and decision-making (1–4). NTS can help in improving the quality and safety of work, on the one hand, and in allowing a reduction of stress, anxiety, and workload for the whole team, on the other hand—a beneficial effect on everyone's mental health.
One of the most important NTSs is teamwork, the ability to collaborate with colleagues toward a common aim, listening to them and helping if needed, allowing one to speed up processes while providing a high level of safety and also a calm, friendly environment for every team member.
NTS and teamwork, in particular, appear to be as important as technical skills (TS) to obtain high-quality results of jobs, both in the environment of business and companies (3, 4), in aviation (5), as well as in healthcare (6, 7). In surgical specialties, teamwork is mandatory, for example, in the operating room (OR) where errors could be fatal, and a collaborative environment is needed for the wellbeing of OR personnel. A safe and relaxed climate ultimately facilitates a smooth process and contributes to patient safety during the whole perioperative period (8, 9). Teamwork has been reported for example as a mainstay of general surgery, orthopedics, and plastic surgery (10–12), carrying positive consequences both on safety attitudes and results, and on the climate and personnel's wellbeing.
The theme of NTS in neurosurgery has not been explored much yet, and teamwork in neurosurgery is even more obscure in the literature. In particular, few publications have evaluated interprofessional teamwork in the neurosurgical OR and interventions intended as “team-building activities”.
The aims of our study were two: first, reviewing the literature about teamwork at the neurosurgical OR table; second, propose a simulation project as a team-building activity, specifically studied for scrub nurses working in neurosurgery and neurosurgeons.
First, we conducted a systematic review of the existing literature on the topic “teamwork at the neurosurgical table” by searching the main medical and nursing databases, i.e., PubMed (Medline) and CINAHL, from the creation of the databases themselves until 15 July 2023. We included articles without restrictions about their publication status (fully published articles, online-ahead-of-print articles), in the English language, that could study the topic from surgeons’, trainees’, and scrub nurses’ points of view. Articles about perceptions or evaluation of the teamwork in the neurosurgical OR, or multi-specialty studies involving at least a neurosurgeon were eligible. Studies concerning interventions to improve teamwork were included when they dealt specifically with neurosurgery/neurosurgical procedures.
We excluded articles only describing multi-disciplinary surgeries (without evaluation of the value of teamwork), studies limited to other surgical domains or studying teamwork among anesthesiologists and neurosurgeons, publications about teamwork outside the OR (in the ward, in the whole healthcare system, in the rehabilitation process, and for emergent fire events). Publications that only mentioned scrub nurses working in “a wide range of specialties” or “in every specialty,” without further specification, were also excluded. We also excluded non-English articles, editorials, literature reviews, commentaries/perspectives/opinions, newspaper articles, proceedings or abstracts, and dissertations.
The systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement 2020 (13) (Data Sheet 1 in the supplementary material).
We searched on PubMed for each of the following words: “teamwork”, “team building”, “team working”, and “non-technical skills”, combined with each of the following other words: “neurosurgery”, “surgery”, and “operating room”. We repeated the same procedure on CINAHL. We eliminated duplicates and then screened all titles and abstracts of the uniquely obtained articles. The publications assessed for eligibility were analyzed through reading of the full-texts and the relevant articles were finally included.
Afterward, we reviewed the references of the relevant studies as additional sources of eligible articles.
Data of the eligible works were obtained through careful analysis of full text by one author and checked by another. If a shared choice could not be reached between the two authors, a third surgeon was called to evaluate the most suitable solution.
The second part of our article focuses on a pilot, explorative study carried out at our Institution (Fondazione IRCCS San Gerardo dei Tintori) to test the utility, appreciation, and value in boosting teamwork between scrub nurses and neurosurgeons of a simulation experience (Figure 1). This experience was a single-session, hands-on, and cadaver-free activity, based on role play, and it was specifically organized for scrub nurses working in neurosurgery (dedicated neurosurgical scrub nurses and scrub nurses taking part in emergent procedures including neurosurgical ones). An organizational meeting was held 10 days before the beginning of the simulation sessions, explaining the project step by step and how to use the self-evaluation questionnaire.
On the day of the simulation, first, scrub nurse participants were asked to complete the SPLINTS (Scrub Practitioners’ List of Intraoperative Non-Technical Skills) rating form as a self-evaluation at baseline (14–17). SPLINTS is a behavioral rating system, developed by psychologists and OR teams, that was originally designed to observe and rate scrub nurses in the OR. It comprises three main categories (situation awareness, communication and teamwork, and task management), each one further developed into three more specific subcategories, as explained in the User Manual (16). It is a rating system specifically developed for scrub nurses, in the same way as NOTECHS (18), ANTS (19), and NOTSS (20) were created for pilots, anesthesiologists, and surgeons, respectively.
A briefing about the neurosurgical oncological technique and the use and working of Exoscope was then offered to the participants. For the actual simulated surgery, a role switch was performed: the scrub nurse played the role of the surgeon, while the surgeon acted like a neurosurgical scrub nurse. Then, the session was developed into three exercises, executed with an exoscopic microsurgical technique. First, the scrub nurse had to make a surgical knot with forceps and a needle holder, looking at the monitor of the Exoscope. Second, they had to perform a cerebral tumor removal onto a model of intrinsic cerebral neoplasm (Tumor Box, UpSurgeOn®), with the support of the neurosurgeon who had prepared the surgical table and is now passing instruments. They also could try and understand the use of BLUE 400 filter for 5-aminolevulinic acid (5-ALA) vision, having the model a fluorescent tracer simulating 5-ALA. Third, the simulation was further developed with the support of a second scrub nurse impersonating the assistant surgeon (Figure 2). An observer noted every relevant comment or evaluation expressed during the whole session.
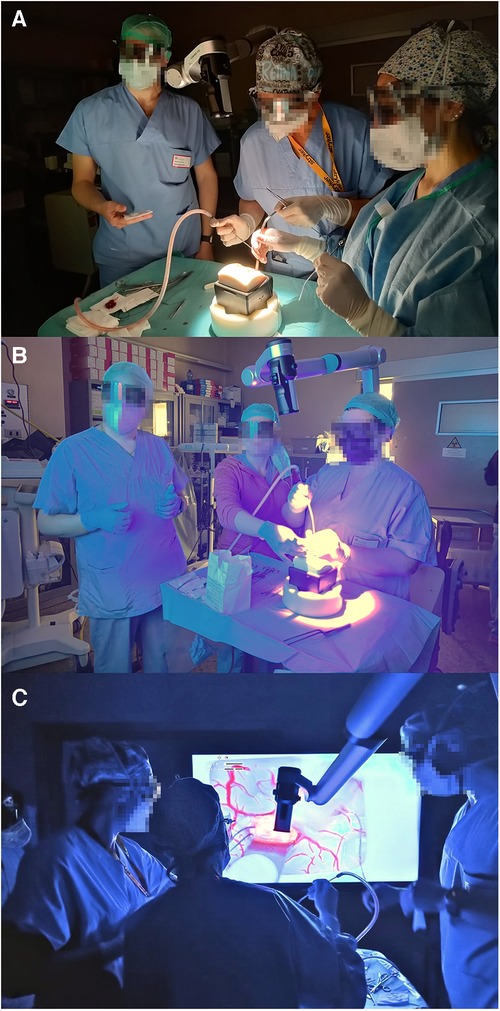
Figure 2. Pictures taken during some of the simulation sessions. (A) A scrub nurse is playing the first surgeon, a second scrub nurse is playing the assistant surgeon, and the neurosurgeon cares for the operating table. (B,C) Exercise made with the help of the blue filter for 5-ALA. In (B), the position of the participants in front of the exoscope screen is shown; in (C), all participants are seen looking at the exoscope screen.
At the end of the simulation, a debriefing took place, underlining the acquired skills, stressing the understanding of the other's role, and giving the participants the chance to ask questions. Every participant—scrub nurses as well as neurosurgeons—was finally asked to complete an evaluation questionnaire with seven questions with a five-point Likert scale for answers, with the possibility to freely add comments. The questionnaire was adapted from a previous article by Shapiro (21) that had proposed a similar team-building experience in another domain of medicine.
The SPLINTS rating form was re-administered as a self-evaluation after three to four weeks after the experience. Every involved scrub nurse took part in at least three neurosurgical procedures in the intervening period, to better evaluate the practical value of the experience in improving their NTS in neurosurgery. The questionnaire results were collected anonymously. Supplementary Image 1 shows the evaluation questionnaire; the SPLINTS rating form can be found at the end of the user manual (16).
An online open-source software, jamovi® (www.jamovi.org) (22), was used for statistical analyses. The sample was described by means of the usual descriptive statistics. To compare independent discrete variables, we applied the Student's t-test. A threshold of p < 0.05 was set for statistical significance.
As mentioned previously, we searched first on PubMed, and then on CINAHL. We obtained a total of 6,415 articles (4,145 from PubMed, 2,270 from CINAHL), of which 2,066 were duplicated. At this point, all titles and abstracts of the unique 4,349 articles were screened. A total of 292 studies were selected, but 47 of them were not retrievable. We finally assessed 245 articles for eligibility, analyzing full-texts, and excluded 211 of them for the following reasons: 88 because they specifically involved specialties other than neurosurgery; 51 because they did not specify involved surgical specialties; 57 because they were types of articles to be excluded; 15 treated irrelevant themes; and 3 were not in English.
From the references of the relevant studies, we further evaluated 11 eligible articles, and 3 were included.
The publications finally included in the study amounted to 34 (Figure 3).
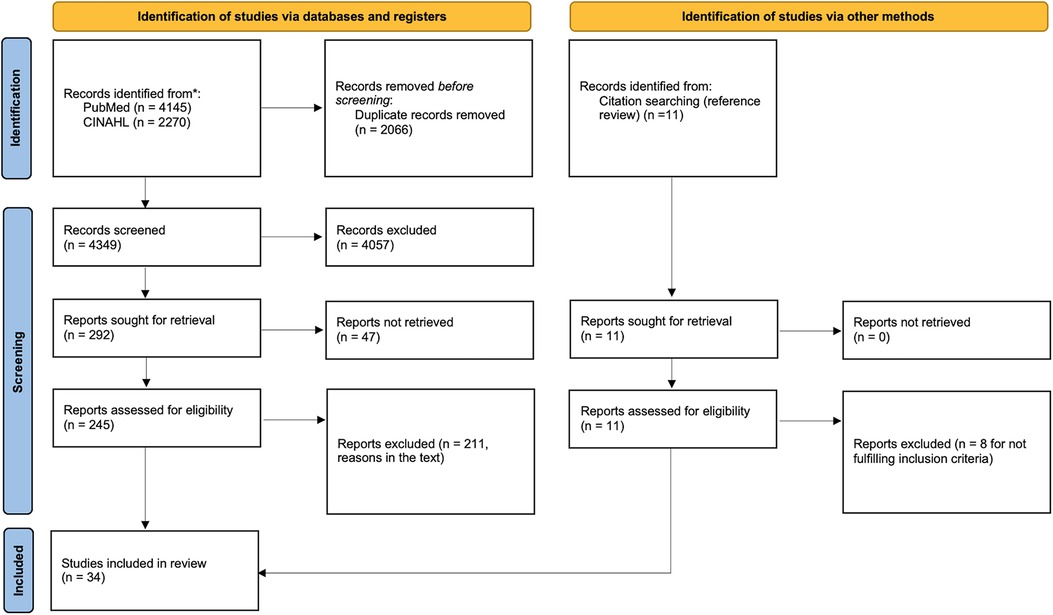
Figure 3. PRISMA 2020 flow diagram for new systematic reviews that included searches of databases, registers, and other sources. The flow chart of the inclusion process based on the “PRISMA 2020 flow diagram” [(see (13)].
We divided the included studies into two groups: the ones dealing with our theme exclusively in neurosurgery in Table 1 (23–36), and the ones studying teamwork and possible other NTS in many specialties, neurosurgery included, in Table 2 (8, 9, 37–54).
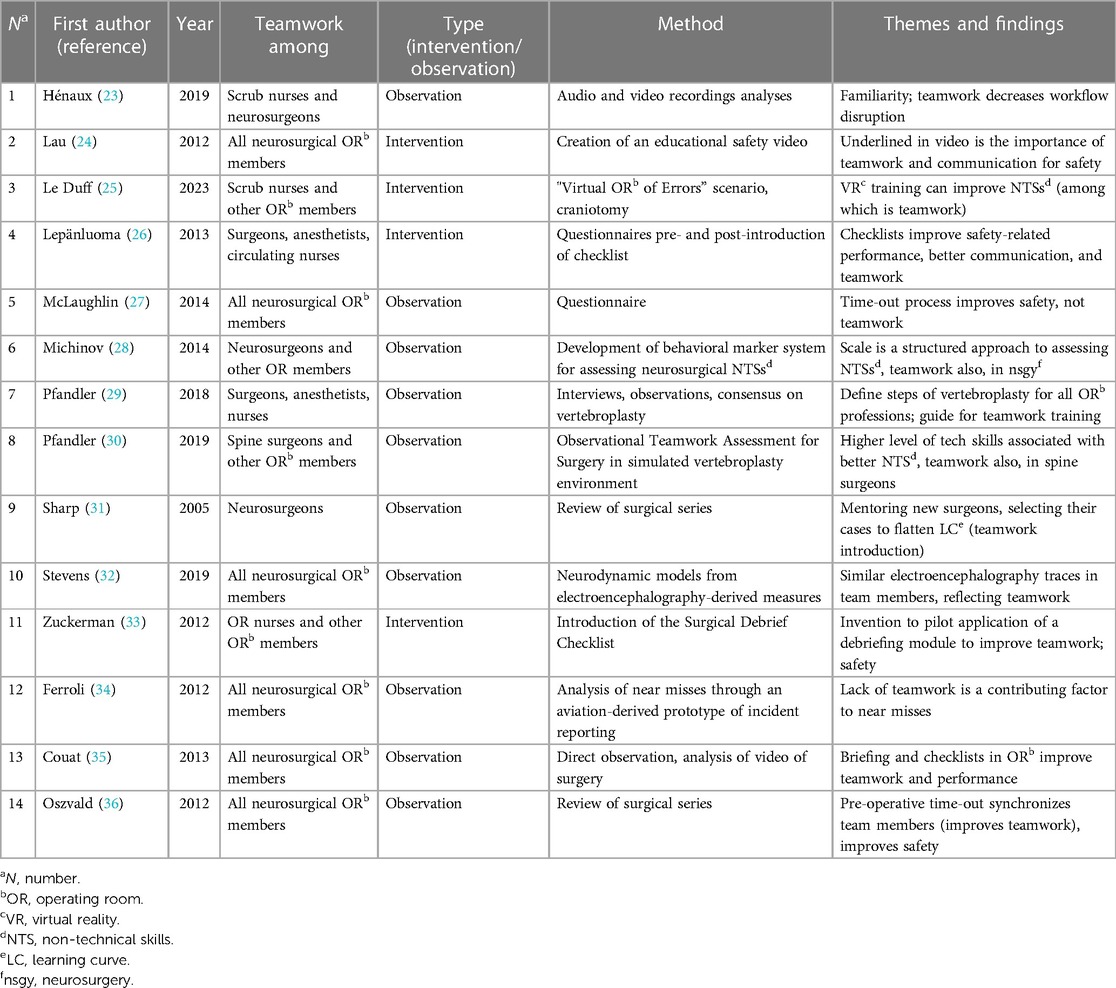
Table 1. Studies included in the systematic review, dealing with our theme exclusively in neurosurgery.
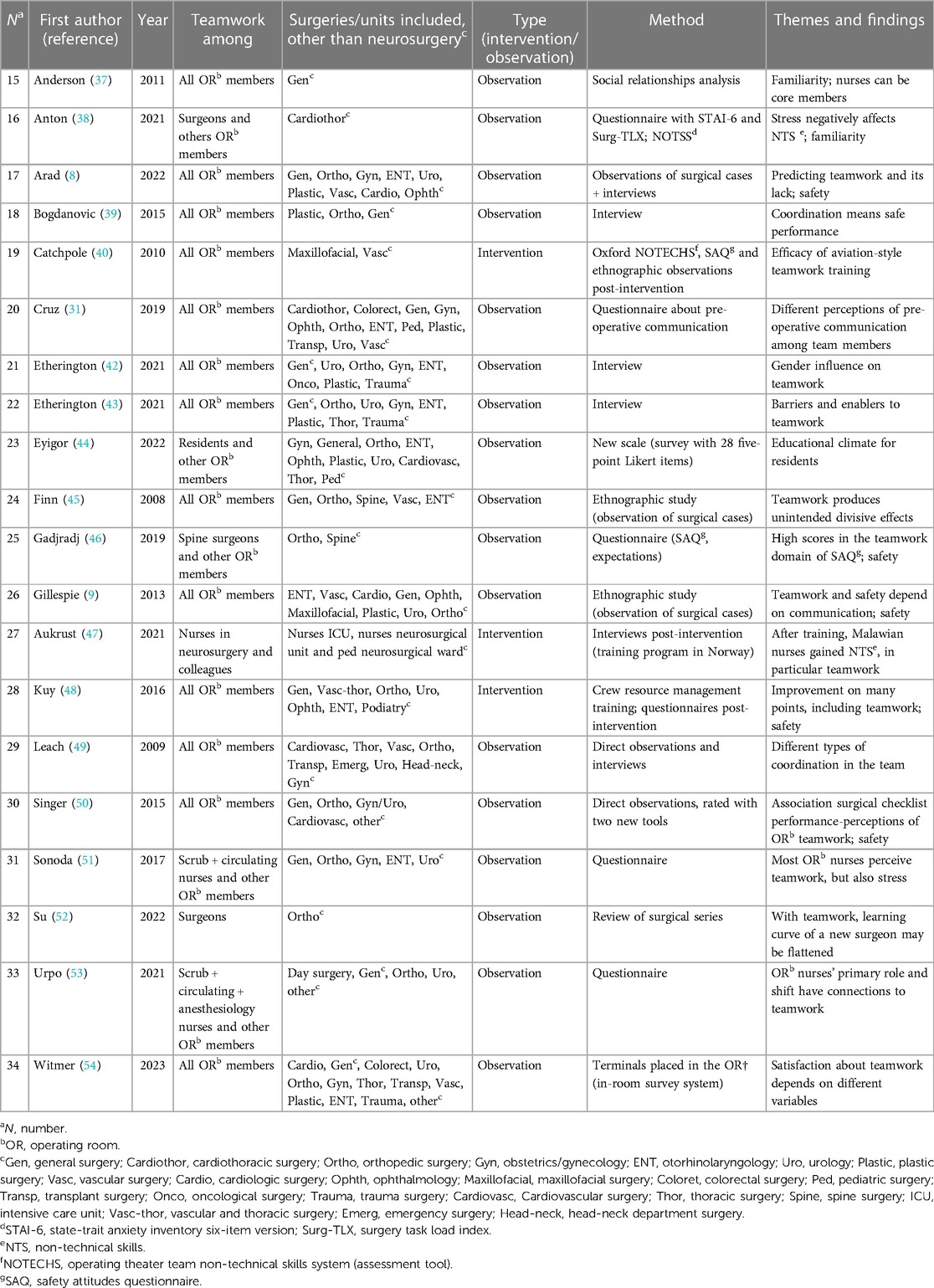
Table 2. Studies included in the systematic review, dealing with our theme in many specialties, neurosurgery included.
Table 1 shows that only one studied the specific relationship among scrub nurses and neurosurgeons at the table (23), while the others globally looked at teamwork in the whole neurosurgical OR environment (24, 26, 27, 29, 32, 34–36), focusing on neurosurgeons (28, 30, 31), or studied exclusively nurses’ tasks or points of view (25, 33).
Similarly, only 4 out of 14 studies tried an intervention to improve teamwork (24–26, 33). The interventions included (1) the production of a video, (2) a virtual reality simulation in which nurses had to find errors in the preparation of a craniotomy, and (3) and (4) the introduction of a checklist.
Very interestingly, the work by McLaughlin et al. concluded that the time-out process may improve safety, but not teamwork—the only “negative” report about teamwork in this group of articles (27).
In Table 2, it is evident that similarly to exclusively neurosurgical reports, the majority of publications (13 out of 20) globally looked at teamwork among the whole staff; 3 focused primarily on surgeons (38, 46, 52), 3 on nurses (47, 51, 53), and 1 on residents (44). The interventional activities are also limited: 3/20, including aviation-style teamwork training (40), a training program in Norway for Malawian nurses (47), and crew resource management training (48).
In all the articles, the theme of safety is often stressed: teamwork and NTS, in general, are considered above all as tools to improve safety in the OR.
A total of 10 scrub nurses and 5 neurosurgeons participated in the simulation experience. Six of the nurses worked exclusively in neurosurgery, four were part of the emergency staff and were involved also in emergent neurosurgical cases. Nine were women and one, man. Every nurse had at least 2 years of experience in the OR. The five neurosurgeons included four attending surgeons and one final-year resident.
The results of the comparison between the pre- and post-experience self-evaluations are provided in Table 3. Very interestingly, the rating scrub nurses gave themselves in the macro-categories “Situation Awareness” and “Communication and Teamwork” showed a statistically significant improvement from the pre- to the post-evaluation. The overall score also improved significantly (A in Table 3).
When looking at the rating scrub nurses wrote in every single item, three showed statistically significant improvement (“Recognizing and understanding information”, “Anticipating”, “Exchanging information”) and all showed improvement tending toward statistical significance (B in Table 3).
Among the items in the evaluation questionnaire, the last four questions specifically concerned teamwork training [4. The quality of the final debriefing for my understanding of the surgeon's work was high, 5. The experience was useful to understand the surgeon's point of view, 6. The experience helped improve my teamwork skills, 7. I would redo the activity to further improve my teamwork skills].
The results of the questionnaire administered to scrub nurses are shown in Figure 4, whereas the surgeons’ evaluations are represented in Figure 5.
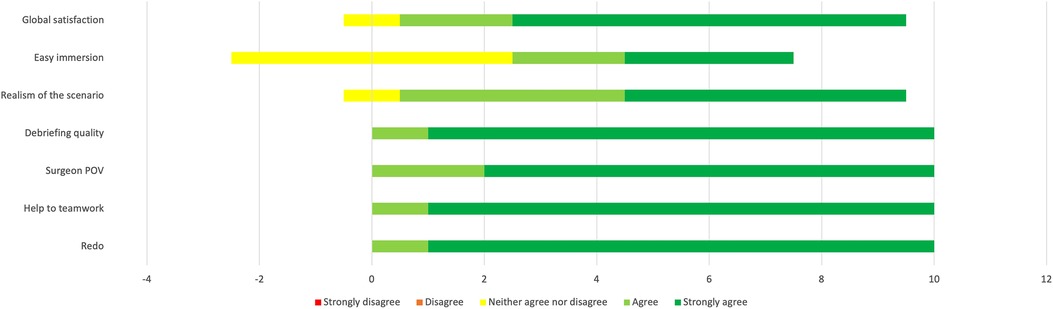
Figure 4. Results of the evaluation questionnaire administered to scrub nurses (n = 10). Answers are expressed on a five-point Likert scale.
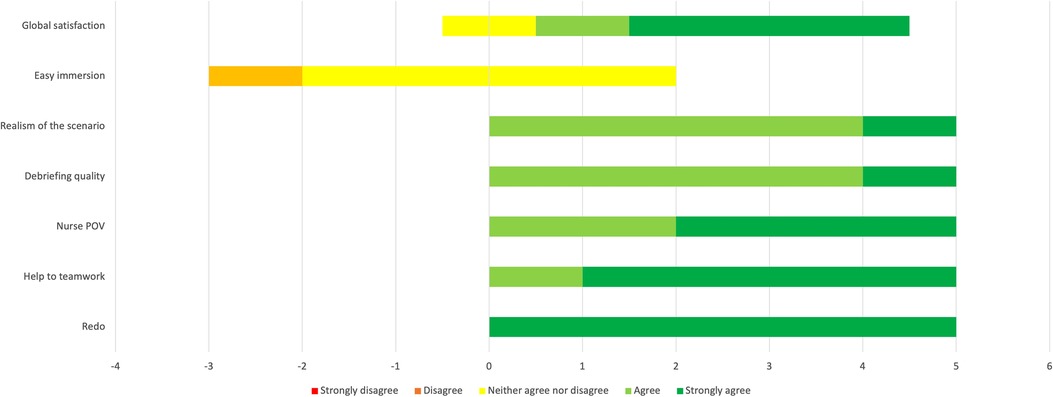
Figure 5. Results of the evaluation questionnaire administered to neurosurgeons (n = 5). Answers are expressed on a five-point Likert scale.
As shown by the graphs, the results of the four items about teamwork were all positive in both groups (agree and strongly agree). The nurses scored items 5, 6, and 7 even higher than the surgeons. The surgeons were globally not satisfied by the ease of immersion in the simulation (four neurosurgeons answered “neutral”; one answered “disagree”), whereas half of the scrub nurses were satisfied to some extent (five agreed or strongly agreed with the sentence).
Every relevant comment orally expressed by participants during the sessions and noted by an external observer was qualitatively analyzed, in the same way as every possible note written at the end of the final evaluation questionnaire (Table 4).
We grouped them into three main themes. The first group of comments was about repeating and improving the simulation experience. As already evident from the Likert items, five scrub nurses further underlined their desire to repeat the experience. Moreover, one suggested trying other boxes from UpSurgeOn® and exercises within neurosurgery, and another one mentioned the possible value of extending such an experience to other specialties. One nurse asked for a possible improvement in the realism of the global scenario and another suggested repeating the experience with all the surgeons, in particular the ones perceived as stricter and/or shyer, to try and strengthen a friendly and trusting relationship.
The second theme in free comments regarded the pleasure of participating in such a simulation, which was stressed by two participants. They felt they had agency and enjoyed the chance to ask questions, understand, and learn in a “safe,” tension-free setting.
The third group of comments was about the surgeons’ work. Two other nurses in particular commented on it: “I now understand how difficult it is to use the Exoscope”; “How many things do you surgeons have to think about, while operating!” Moreover, very interestingly, during each session, every single participant was light-heartedly mocking the other group's typical expressions and comments. For example, every nurse playing the surgeon exaggeratingly complained about the blockage of the aspirator, a typical complaint of the surgeon during everyday surgical cases.
NTS are becoming more and more relevant in every type of job. Any type of worker should be able not only to acquire specific technical abilities, but also work on their interpersonal skills, such as leadership, efficient communication, and collaboration and teamwork, as well as their cognitive abilities, represented by awareness of the situation, decision-making, and flexibility and coping attitudes (1–4). The importance of NTS depends on their demonstrated role in both contributing to the improvement of quality and safety of work and in allowing the construction of a calm, friendly work environment for the whole team—which is beneficial to everyone's mental health and to the safety in the workflow.
Teamwork is a fundamental NTS, and it is in fact the ability to focus as a team on a common aim, listening to colleagues and offering them help. Teamwork contributes to speeding up processes and workflows while maintaining a high level of safety at each step and also guaranteeing a healthier environment for team members.
Our literature review showed a limited number of articles about interprofessional teamwork among neurosurgeons and scrub nurses in the OR, mainly focusing on observing the existing situation (Tables 1, 2). Interestingly, the vast majority of articles did not focus on the specific relationship between scrub nurses and neurosurgeons but globally looked at teamwork among the whole staff, exclusively in neurosurgery or also in neurosurgery. We strongly believe that this relationship should be studied and taken care of on its own because it requires a set of shared skills, know-how, and knowledge that is never required in the whole OR environment. Another point that is worth stressing is that few interventions have been proposed to try and improve NTS and teamwork in particular (7 out of 34, 20.6%), while as mentioned the others generally reported measurements and observations about the status quo of teamwork in the OR. When analyzing these interventions, we can find three passive approaches—production of a video in one case (24), introduction of a checklist in two cases (26, 33)—and four active ones—a virtual reality simulation for nurses (25), a nurse-centered training program in a foreign country (47), and two training models borrowed from aviation (40) and crew resource management (48).
It seems clear that no activity, neither active nor passive, can be found in the literature reproducing the exclusive, real-life relationship among scrub nurses and neurosurgeons in the OR, and with the ultimate aim of trying to improve the quality of that working relationship.
Thus, we developed the project of our hands-on, cadaver-free simulation, which may therefore be considered one of the first experiences in the literature describing a neurosurgical team-building activity to boost interprofessional teamwork in the OR, specifically addressing scrub nurses.
Although missing in neurosurgery, a certain number of similar activities has already been proposed in other surgical specialties, for example, plastic surgery (12), emergency medicine (55), and gynecology (56), often based on concepts taken from aviation (5, 34, 40). The initial experiences of NTS in healthcare historically came from aviation, in which pilots are required not only to perfectly demonstrate their technical abilities but also to cultivate their interprofessional skills and cognitive skills to provide safety during their job activity. Our review reports some recalls to aviation (34, 40).
We believe it is important to underline that beneficial effects on teamwork could be seen on safety but also on the work environment (8). In fact, based on our review, the role of teamwork in a professional’s wellbeing appears to be quite overlooked. To us, this seems like a big omission. Teamwork is surely pivotal for safety in the OR, but safety for the patient improves through the reduction of stress, anxiety, and workload for the team members. Moreover, mental health is a right of every worker. Therefore, a friendly, familiar, and harmonious work environment surely gives benefits to everyone—the care team and patients.
Our simulation may suggest the role of team-building activities in teamwork improvement in neurosurgery (Table 3). For the sake of clarity, the reasons for choosing the SPLINTS rating form (14, 15, 17) were multiple and are now discussed. First, it is specifically aimed at scrub nurses, which was our primary criterion. Second, it is user-friendly and easy to understand, and we found it to be both very precise and non-redundant and thus efficient. A goal for us during the design of this study was not to hinder the professional activity or personal life of study participants by limiting the amount of time needed to take part. Third, as specified in the manual (16), although it was designed for evaluation by an external observer, it can also be used for self-evaluation. Finally, it also allows a global evaluation not only of teamwork but also of other NTS, giving clues about a more comprehensive value of our project.
The SPLINTS rating form items showed a statistically significant improvement from the pre- to the post-evaluation not only in the macro-category “Communication and Teamwork” but also in another NTS that is “Situation Awareness,” while the results were not significant for “Task management.” This seems straightforward, as the first two categories imply putting oneself in somebody else's shoes, that is exactly what is experienced in the role switch of our simulation. On the contrary, the proposed activity does not focus on the management of different tasks.
When looking at the single items, they tend to have statistical significance although this is less evident than in the macro-categories. We think this may be related to multiple factors. First, dividing single specific behaviors within a global category may be difficult for people not having a long, focused training on NTS evaluation. Second, the evaluation scale was a four-point one, which may contribute together with the number of participants in making the otherwise relevant chances not cross the statistical significance threshold. Third, self-evaluation also includes judgments about oneself and the mood of the day, being therefore more variable than an external evaluation.
All the participants, neurosurgeons as well as scrub nurses, globally rated the experience positively (Figures 4, 5). Scrub nurses in particular showed a high level of enthusiasm, suggesting repeating the experience and in some cases even opening it to other specialties. They felt more active than usual and perceived a tension-free environment in which learning was facilitated. In particular, they demonstrated a particular utility in understanding the neurosurgeon's point of view, difficulties, and challenges. The use of a physical simulator such as the Tumor Box from UpSurgeOn® seems an added value, as the tactile feedback given by the model further helps understand the actual surgical job, more than only observing and assisting.
Unexpectedly, in all sessions every participant mocked the other profession's typical expressions and comments, often causing a general laugh. This may suggest a role of team-building activities also in exorcizing their own fears and awe, in facing possible resentments and disagreements, and in helping the other professionals resize their exaggerated behaviors.
The realism of the situation and the general context, specifically in tasks related to preparation for surgery, patient positioning, and space management in the OR, was a less appreciated point, together with the ease of immersion in the simulation. In fact, the simulators used were designed to replicate the surgical field itself rather than the surrounding context (the surgical drapes, the patient, the spatial organization of the OR), which certainly diminished the perception of realism in terms of “faithful reproduction of all steps of a surgical session,” from patient arrival in the OR to drapes removal. This aspect could be further developed in future sessions. Moreover, it was suggested to repeat the simulation with all the neurosurgeons of the department, in particular those perceived as stricter and/or shyer ones, to try and strengthen a friendly and trusting relationship that could carry over to real—and often very challenging and stressful—scenarios.
Having a look at the whole of our results, we could imagine some possible practical research implications and evolutions of our pilot experience. With the introduction of cadaver-free simulation models, it is possible to assume that all dedicated neurosurgical scrub nurses may have the chance to simulate the role of the neurosurgeon in a safe scenario and to repeat these simulation sessions as needed, ideally arriving at the realization of a specific educational program. This may lead to a global reinforcement of all NTSs, in particular,
- increased perception of the neurosurgeon's needs in case of adverse intraoperative events (e.g., massive sudden bleedings);
- better step-by-step anticipation of the neurosurgeons’ needs, to speed up the surgical procedure and optimize the use of the operatory room time for each procedure;
- better help the neurosurgeon in surgeries performed in a single-surgeon setting, to make surgery more efficient;
- increase in awareness during surgery of complex cases, so as to have all the dedicated instruments available as soon as possible during surgery.
Furthermore, the establishment of such cadaver-free NTS programs for scrub nurses may be proposed for every specific setting. This might lead to the definition of specialized scrub nurses for each surgical specialty. Such an implementation of educational training of scrub nurses might be considered an evolution of the professional competencies of nurses as it happens in medical specialties or sub-specialties.
Our study shows some limitations, as already mentioned, and may suggest some future directions. First, the number of participants was extremely limited, given the voluntary recruitment and the nature of our research itself as a “pilot study.” This point limits, in fact, the impact of the statistical analysis and the generalizability of our findings. Ideally, the simulation should be repeated with as many scrub nurses working in neurosurgery as possible, and with all the neurosurgeons of the department, if not even in a multi-centric fashion. Second, self-evaluation allows a rapid, realistic evaluation of oneself, but includes one's own self-esteem, which is incredibly variable among people and even on different days. Thus, a similar session with a specifically trained external observation may overcome this limitation. Lastly, we did not evaluate the persistence of the improvements. In other words, we do not know if improvement in teamwork and situation awareness remains months after the simulation. Another evaluation could be administered at a certain time distance, as well as new “recall sessions” could be proposed. A pre-simulation theoretical meeting about teamwork and NTS could also be offered.
Our study represents one of the first experiences of a hands-on, cadaver-free neurosurgical simulation to boost teamwork in the neurosurgical OR. It was globally very well welcomed for its subjectively perceived utility. The present work may suggest that team-building activities could play a role in improving teamwork abilities and other NTS in neurosurgery. Future studies and sessions may support our findings and perhaps even further improve the efficacy of such interventions, also studying the possible sustainment of improvement.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
CdL: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization. DP: Writing – review & editing, Writing – original draft, Investigation, Data curation, Conceptualization. AD: Writing – review & editing, Writing – original draft, Investigation, Data curation. AV: Writing – review & editing, Writing – original draft, Investigation, Data curation. TC: Writing – review & editing, Writing – original draft. AT: Writing – review & editing, Writing – original draft. VV: Writing – review & editing, Writing – original draft, Investigation. LA: Writing – review & editing, Writing – original draft. AB: Writing – review & editing, Writing – original draft, Investigation, Formal Analysis. FN: Writing – review & editing, Writing – original draft, Validation, Supervision. GC: Writing – review & editing, Writing – original draft, Validation, Supervision. CG: Writing – review & editing, Writing – original draft, Validation, Supervision.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank A. Longoni for the support in digital art creation.
FN is founder and CEO of UpSurgeOn®.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The handling editor CZ declared a past co-authorship with the authors CG and FN.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2024.1386887/full#supplementary-material
1. Hénaux PL, Jannin P, Riffaud L. Nontechnical skills in neurosurgery: a systematic review of the literature. World Neurosurg. (2019) 130:e726–36. doi: 10.1016/j.wneu.2019.06.204
2. Yule S, Flin R, Paterson-Brown S, Maran N. Non-technical skills for surgeons in the operating room: a review of the literature. Surgery. (2006) 139(2):140–9. doi: 10.1016/j.surg.2005.06.017
3. Jackson D, Hancock P. Non-technical skills in undergraduate degrees in business: development and transfer. ERP. (2020) 37(1):52–84.
4. Nielsen K, Ng K, Guglielmi D, Lorente L, Pătraş L, Vignoli M. The importance of training transfer of non-technical skills safety training of construction workers. Int J Occup Saf Ergon JOSE. (2023) 29(1):444–52. doi: 10.1080/10803548.2022.2052624
5. Leedom DK, Simon R. Improving team coordination: a case for behavior-based training. Mil Psychol. (1995) 7(2):109–22. doi: 10.1207/s15327876mp0702_5
6. Prineas S, Mosier K, Mirko C, Guicciardi S. “Non-technical skills in healthcare”. In: Donaldson L, Ricciardi W, Sheridan S, Tartaglia R, editors. Textbook of Patient Safety and Clinical Risk Management. Cham: Springer (2021). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK585613/ (accessed September 3, 2023).
7. Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, et al. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol. (2018) 73(4):433–50. doi: 10.1037/amp0000298
8. Arad D, Finkelstein A, Rozenblum R, Magnezi R. Patient safety and staff psychological safety: a mixed methods study on aspects of teamwork in the operating room. Front Public Health. (2022) 10:1060473. doi: 10.3389/fpubh.2022.1060473
9. Gillespie BM, Gwinner K, Chaboyer W, Fairweather N. Team communications in surgery—creating a culture of safety. J Interprof Care. (2013) 27(5):387–93. doi: 10.3109/13561820.2013.784243
10. Stahel PF, Cobianchi L, Dal Mas F, Paterson-Brown S, Sakakushev BE, Nguyen C, et al. The role of teamwork and non-technical skills for improving emergency surgical outcomes: an international perspective. Patient Saf Surg. (2022) 16(1):8. doi: 10.1186/s13037-022-00317-w
11. Alzahrani KH, Abutalib RA, Elsheikh AM, Alzahrani LK, Khoshhal KI. The need for non-technical skills education in orthopedic surgery. BMC Med Educ. (2023) 23:262. doi: 10.1186/s12909-023-04196-2
12. Gowda S, Elsabra R, Lindero E, Mohan A. Improving interprofessional teamwork in plastic surgery: a novel approach to microsurgical skills training. Plast Aesthetic Nurs. (2021) 41(4):203. doi: 10.1097/PSN.0000000000000399
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
14. Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Evaluation of the scrub practitioners’ list of intraoperative non-technical skills (SPLINTS) system. Int J Nurs Stud. (2012) 49(2):201–11. doi: 10.1016/j.ijnurstu.2011.08.012
15. Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Development of a behavioural marker system for scrub practitioners’ non-technical skills (SPLINTS system). J Eval Clin Pract. (2013) 19(2):317–23. doi: 10.1111/j.1365-2753.2012.01825.x
16. Mitchell L. “Scrub practitioners’ list of intra-operative non-technical skills—SPLINTS”. In: Mitchell L, Flin R, editors. Safer Surgery, 1st ed. Aberdeen: Univerisity of Aberdeen (2017). p. 67–81. Available online at: https://www.taylorfrancis.com/books/9781317060048/chapters/10.1201/9781315607436-5 (accessed September 3, 2023).
17. Flin R, Mitchell L, McLeod B. Non-technical skills of the scrub practitioner: the SPLINTS system. ORNAC J. (2014) 32(3):33–8.25322533
18. van Avermaete JAG. NOTECHS: non-technical skill evaluation in JAR-FCL. Natl Lucht- Ruimtevaartlaboratorium—National Aerospace Laboratories NLR (1998).
19. Fletcher G, Flin R, McGeorge P, Glavin R, Maran N, Patey R. Anaesthetists’ non-technical skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth. (2003) 90(5):580–8. doi: 10.1093/bja/aeg112
20. The Royal College of Surgeons of Edinburgh. The Non-Technical Skills for Surgeons (NOTSS)—System Handbook v2.0. Aberdeen: Univerisity of Aberdeen (2019).
21. Shapiro MJ. Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum? Qual Saf Health Care. (2004) 13(6):417–21. doi: 10.1136/qshc.2003.005447
22. The jamovi project. jamovi (Version 1.6) [Computer Software]. (2021). Available online at: https://www.jamovi.org (accessed October 10, 2023).
23. Henaux PL, Michinov E, Rochat J, Hémon B, Jannin P, Riffaud L. Relationships between expertise, crew familiarity and surgical workflow disruptions: an observational study. World J Surg. (2019) 43(2):431–8. doi: 10.1007/s00268-018-4805-5
24. Lau CY, Greysen SR, Mistry RI, Han SJ, Mummaneni PV, Berger MS. Creating a culture of safety within operative neurosurgery: the design and implementation of a perioperative safety video. Neurosurg Focus. (2012) 33(5):E3. doi: 10.3171/2012.9.FOCUS12244
25. Le Duff M, Michinov E, Bracq MS, Mukae N, Eto M, Descamps J, et al. Virtual reality environments to train soft skills in medical and nursing education: a technical feasibility study between France and Japan. Int J Comput Assist Radiol Surg. (2023) 18(8):1355–62. doi: 10.1007/s11548-023-02834-0
26. Lepänluoma M, Takala R, Kotkansalo A, Rahi M, Ikonen TS. Surgical safety checklist is associated with improved operating room safety culture, reduced wound complications, and unplanned readmissions in a pilot study in neurosurgery. Scand J Surg. (2014) 103(1):66–72. doi: 10.1177/1457496913482255
27. McLaughlin N, Winograd D, Chung HR, Van De Wiele B, Martin NA. Impact of the time-out process on safety attitude in a tertiary neurosurgical department. World Neurosurg. (2014) 82(5):567–74. doi: 10.1016/j.wneu.2013.07.074
28. Michinov E, Jamet E, Dodeler V, Haegelen C, Jannin P. Assessing neurosurgical non-technical skills: an exploratory study of a new behavioural marker system: non-technical skills in neurosurgery. J Eval Clin Pract. (2014) 20(5):582–8. doi: 10.1111/jep.12152
29. Pfandler M, Stefan P, Wucherer P, Lazarovici M, Weigl M. Stepwise development of a simulation environment for operating room teams: the example of vertebroplasty. Adv Simul. (2018) 3(1):18. doi: 10.1186/s41077-018-0077-2
30. Pfandler M, Stefan P, Mehren C, Lazarovici M, Weigl M. Technical and nontechnical skills in surgery: a simulated operating room environment study. Spine. (2019) 44(23):E1396–400. doi: 10.1097/BRS.0000000000003154
31. Sharp M, MacFarlane R, Hardy D, Jones S, Baguley D, Moffat D. Team working to improve outcome in vestibular schwannoma surgery. Br J Neurosurg. (2005) 19(2):122–7. doi: 10.1080/02688690500145480
32. Stevens R, Galloway T, Willemsen-Dunlap A. Advancing our understandings of healthcare team dynamics from the simulation room to the operating room: a neurodynamic perspective. Front Psychol. (2019) 10:1660. doi: 10.3389/fpsyg.2019.01660
33. Zuckerman SL, France DJ, Green C, Leming-Lee S, Anders S, Mocco J. Surgical debriefing: a reliable roadmap to completing the patient safety cycle. Neurosurg Focus. (2012) 33(5):E4. doi: 10.3171/2012.8.FOCUS12248
34. Ferroli P, Caldiroli D, Acerbi F, Scholtze M, Piro A, Schiariti M, et al. Application of an aviation model of incident reporting and investigation to the neurosurgical scenario: method and preliminary data. Neurosurg Focus. (2012) 33(5):E7. doi: 10.3171/2012.9.FOCUS12252
35. Couat JF, Cegarra J, Rodsphon T, Geeraerts T, Lelardeux C, Sol JC, et al. A prospective video-based observational and analytical approach to evaluate management during brain tumour surgery at a university hospital. Neurochirurgie. (2013) 59(4–5):142–8. doi: 10.1016/j.neuchi.2013.05.001
36. Oszvald Á, Vatter H, Byhahn C, Seifert V, Güresir E. “Team time-out” and surgical safety—experiences in 12,390 neurosurgical patients. Neurosurg Focus. (2012) 33(5):E6. doi: 10.3171/2012.8.FOCUS12261
37. Anderson C, Talsma A. Characterizing the structure of operating room staffing using social network analysis. Nurs Res. (2011) 60(6):378–85. doi: 10.1097/NNR.0b013e3182337d97
38. Anton NE, Athanasiadis DI, Karipidis T, Keen AY, Karim A, Cha J, et al. Surgeon stress negatively affects their non-technical skills in the operating room. Am J Surg. (2021) 222(6):1154–7. doi: 10.1016/j.amjsurg.2021.01.035
39. Bogdanovic J, Perry J, Guggenheim M, Manser T. Adaptive coordination in surgical teams: an interview study. BMC Health Serv Res. (2015) 15(1):128. doi: 10.1186/s12913-015-0792-5
40. Catchpole KR, Dale TJ, Hirst DG, Smith JP, Giddings TAEB. A multicenter trial of aviation-style training for surgical teams. J Patient Saf. (2010) 6(3):180–6. doi: 10.1097/PTS.0b013e3181f100ea
41. Cruz SA, Idowu O, Ho A, Lee MJ, Shi LL. Differing perceptions of preoperative communication among surgical team members. Am J Surg. (2019) 217(1):1–6. doi: 10.1016/j.amjsurg.2018.06.001
42. Etherington C, Kitto S, Burns JK, Adams TL, Birze A, Britton M, et al. How gender shapes interprofessional teamwork in the operating room: a qualitative secondary analysis. BMC Health Serv Res. (2021) 21(1):1357. doi: 10.1186/s12913-021-07403-2
43. Etherington C, Burns JK, Kitto S, Brehaut JC, Britton M, Singh S, et al. Barriers and enablers to effective interprofessional teamwork in the operating room: a qualitative study using the theoretical domains framework. PLoS One. (2021) 16(4):e0249576. doi: 10.1371/journal.pone.0249576
44. Eyigor H, Kara CO, Sezik M, Gurpinar E. Operating room educational climate scale for surgical specialty residents: scale development and validation. Turk Neurosurg. (2020) 32(1):28–35. doi: 10.5137/1019-5149.JTN.30775-20.1
45. Finn R. The language of teamwork: reproducing professional divisions in the operating theatre. Hum Relat. (2008) 61(1):103–30. doi: 10.1177/0018726707085947
46. Gadjradj PS, Harhangi BS. Safety culture and attitudes among spine professionals: results of an international survey. Glob Spine J. (2019) 9(6):642–9. doi: 10.1177/2192568218825247
47. Aukrust CG, Kamalo PD, Prince RJ, Sundby J, Mula C, Manda-Taylor L. Improving competencies and skills across clinical contexts of care: a qualitative study on Malawian nurses’ experiences in an institutional health and training programme. Nurs Open. (2021) 8(6):3170–80. doi: 10.1002/nop2.1030
48. Kuy S, Romero RAL. Improving staff perception of a safety climate with crew resource management training. J Surg Res. (2017) 213:177–83. doi: 10.1016/j.jss.2016.04.013
49. Leach LS, Myrtle RC, Weaver FA, Dasu S. Assessing the performance of surgical teams. Health Care Manage Rev. (2009) 34(1):29–41. doi: 10.1097/01.HMR.0000342977.84307.64
50. Singer SJ, Molina G, Li Z, Jiang W, Nurudeen S, Kite JG, et al. Relationship between operating room teamwork, contextual factors, and safety checklist performance. J Am Coll Surg. (2016) 223(4):568–80.e2. doi: 10.1016/j.jamcollsurg.2016.07.006
51. Sonoda Y, Onozuka D, Hagihara A. Factors related to teamwork performance and stress of operating room nurses. J Nurs Manag. (2018) 26(1):66–73. doi: 10.1111/jonm.12522
52. Su YF, Tsai TH, Kuo KL, Wu CH, Tsai CY, Lu YM, et al. Potential roles of teamwork and unmet needs on surgical learning curves of spinal robotic screw placement. J Multidiscip Healthc. (2022) 15:1971–8. doi: 10.2147/JMDH.S380707
53. Urpo M, Eskola S, Suominen T, Roos M. Teamwork: a perspective of perioperative nurses. Cent Eur J Nurs Midwifery. (2021) 12(3):430–40. doi: 10.15452/cejnm.2021.12.0018
54. Witmer HDD, Morris-Levenson JA, Keçeli Ç, Godley FA, Dhiman A, Adelman D, et al. Novel application of a dynamic, in-room survey platform to measure surgical team satisfaction. Ann Surg. (2023) 279(1):71–6. doi: 10.1097/SLA.0000000000005993
55. Kiessling A, Amiri C, Arhammar J, Lundbäck M, Wallingstam C, Wikner J, et al. Interprofessional simulation-based team-training and self-efficacy in emergency medicine situations. J Interprof Care. (2022) 36(6):873–81. doi: 10.1080/13561820.2022.2038103
Keywords: education, interprofessional, non-technical skills, operating room, roleplay, simulation, teamwork
Citation: de Laurentis C, Pirillo D, Di Cristofori A, Versace A, Calloni T, Trezza A, Villa V, Alberti L, Baldo A, Nicolosi F, Carrabba G and Giussani C (2024) Boosting teamwork between scrub nurses and neurosurgeons: exploring the value of a role-played hands-on, cadaver-free simulation and systematic review of the literature. Front. Surg. 11:1386887. doi: 10.3389/fsurg.2024.1386887
Received: 16 February 2024; Accepted: 29 February 2024;
Published: 15 March 2024.
Edited by:
Cesare Zoia, San Matteo Hospital Foundation (IRCCS), ItalyReviewed by:
Naci Balak, Istanbul Medeniyet University Goztepe Education and Research Hospital, Türkiye© 2024 de Laurentis, Pirillo, Di Cristofori, Versace, Calloni, Trezza, Villa, Alberti, Baldo, Nicolosi, Carrabba and Giussani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlo Giussani Y2FybG8uZ2l1c3NhbmlAdW5pbWliLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.