- 1U.O. Chirurgia Generale e d’Urgenza, Ospedale Montebelluna, Montebelluna, Italy
- 2Unit of Epidemiology and Medical Statistics, Department of Diagnostics & Public Health, University of Verona, Verona, Italy
- 3General Surgery, ASST Spedali Civili di Brescia, Montichiari, Italy
- 4UOC Chirurgia Generale 2, ASST Spedali Civili di Brescia, Brescia, Italy
- 5U.O. Chirurgia Generale, Ospedale Civile Santa Maria del Carmine, Rovereto, Italy
- 6U.O. Chirurgia Generale e Mininvasiva, Ospedale San Camillo, Trento, Italy
Purpose: Diastasis of rectus abdominis (DRA) refers to a separation of the rectus abdominis from the linea alba, which is common in the female population during pregnancy and in the postpartum period. The present study aimed at investigating DRA severity, risk factors and associated disorders.
Methods: In the present cross-sectional study, a web-based questionnaire was addressed to the 23,000 members of the Women's Diastasis Association. The questionnaire comprised three parts, dedicated respectively to diastasis characteristics, possible risk factors, and related disorders. Faecal and urinary incontinences were assessed using the Wexner and ICIQ-SF score, respectively. Risk factors for diastasis severity (<3, 3–5, >5 cm) were evaluated by a multinomial regression model.
Results: Four thousand six hundred twenty-nine women with a mean age (SD) of 39.8 (6.5) years and a median BMI of 23.7 kg/m2 (range 16.0–40.0) responded to the questionnaire. Proportion of DRA >5 cm increased from 22.8% in norm weight women to 44.0% in severely obese women, and from 10.0% in nulliparous women to 39.3% in women with >3 pregnancies. These associations were confirmed in multivariable analysis. DRA severity was associated with the risk of abdominal hernia and pelvic prolapse, whose prevalence more than doubled from women with DRA <3 cm (31.6% and 9.7%, respectively) to women with DRA >5 cm (68.2% and 20.2%). In addition, most patients reported postural pain and urinary incontinence, whose frequency increased with DRA severity.
Conclusion: The present study confirmed that DRA severity increases with increasing BMI and number of pregnancies. Larger separation between rectal muscles was associated with increased risk of pain/discomfort, urinary incontinence, abdominal hernia and pelvic prolapse. Prospective studies are needed to better evaluate risk factors.
Introduction
Diastasis of rectus abdominis (DRA) refers to a separation of the rectus abdominis from the linea alba, which often affects multipara women (1). There is no universal definition of the minimum distance to diagnose DRA, although two papers in the literature agree on a minimum inter-recti distance of 20 mm supraumbilical regardless of patient age (2–4).
Although the whole population can be affected, DRA has a marked prevalence in women, especially after multiple births. Indeed, pregnancy changes the abdominal conformation due to the space occupied by the uterus and increases the physiological lumbar lordosis. This changes the levels of elongation of the abdominal muscles by modifying the angles of origin and insertion, leading, among other effects, to flaccidity of the linea alba with a consequent increase in the space between the muscle's bellies of the rectus (5–7). This effect may persist from 24% to 70% of cases during postpartum in different regions of the linea alba. The remodelling time typically lasts 6–8 weeks, although this parameter may vary individually with continuous decreases up to 6–12 months postpartum (6, 8, 9). The prevalence of this pathological condition of the abdominal wall is very variable, ranging from 39% to 52% in post-pregnancy women. In addition to pregnancy, obesity is a major risk factor for the onset of this condition (10).
An increase in the distance between the anterior borders of the rectus muscles influences the strength of the abdominal wall musculature and does not usually cause pain at rest. During physical activities, however, the characteristic bulging of the abdominal wall may appear, due to an increase of the intra-abdominal pressure. Therefore, DRA may be associated with epigastric and umbilical hernias. Pregnancy may cause herniation or render a pre-existing one apparent, because of progressively raised intra-abdominal pressure (11–13). The presence of diastasis of the rectus muscles is not only an “aesthetic” fact but is associated with the development over time, if not corrected properly, of uterine prolapse, faecal and urinary incontinence. Considering the role of abdominal muscles in maintaining posture and their engagement in various physical activities one may suspect that the presence of DRA may have an impact on the trunk and pelvic stabilization, thus leading to poor posture, limitations during physical activity, as well as lumbo-pelvic pain and hip pain (13).
There is a scant knowledge on the prevalence, risk factors, prevention, or management of the abovementioned condition. For many years, abdominal diastasis of the rectus was considered an exclusively aesthetic problem by surgeons, and treatment was entrusted exclusively to plastic surgeons. Over the last few years, surgeons' attention to this anatomical, pathological condition has progressively increased. The association of DRA with the presence of a midline hernia has led surgeons to develop some minimally invasive surgical techniques to treat this pathology.
The aims of the present study are:
(1) To investigate possible determinants of the severity of DRA, including maternal conditions, comorbidities/treatments, previous pregnancies, childbirth characteristics.
(2) To study the association between DRA severity and post-partum disorders, such as pain/discomfort, urinary/faecal incontinence.
(3) To address the association between rectal muscle separation and other consequences of increased intra-abdominal pressure, such as hernia, prolapse.
Materials and methods
In the present observational cross-sectional study, approximately 23,000 Italian women, belonging to the voluntary organisation Diastasi Donna® ODV (https://www.diastasidonna.it/diastasi-donna-odv/), were invited to anonymously answer an online questionnaire by Google form. The questionnaire was filled in by 4,629 women (about 20.1%) aged 39.8 ± 6.5 years (mean ± SD; range 22–74) with a median BMI of 23.7 kg⁄m2 (range 16.0–40.0), who had had a median of 2 pregnancies (range 0–5). While filling-in the anonymous questionnaire, women were also asked to release informed consent for anonymous data publication.
The questionnaire comprised three parts, dedicated respectively to diastasis characteristics, possible risk factors, and related disorders (Table 1; Supplementary Table S1). Faecal incontinence was assessed by Wexner score, and urinary incontinence by ICIQ-SF score (14, 15).
Rectal muscle separation was measured during Valsalva maneuver by ultrasounds and/or computed tomography. In detail, 3,742 women (80.8%), reported to have undergone ultrasounds, 434 (9.4%) abdominal magnetic resonance imaging, and 453 (9.8%) abdominal CT-scan. According to the classifications proposed by Ranney, the severity of DRA was defined by the distance between rectal muscles (mild DRA >3, moderate DRA 3–5, severe DRA >5 cm) and the extension of DRA (supra-umbilical, sub-umbilical, both) (16). Of note, severe diastasis >5 cm is considered as an indication for surgical treatment (13).
Statistical analyses
The endpoint of the study was separation of rectus abdominis muscles. Significance of the association between DRA severity and potential determinants was evaluated by Fisher's exact test or chi-squared test for categorical variables, and Kruskal–Wallis test for quantitative variables.
In multivariable analysis determinants of DRA severity (≥3, 3–5, >5 cm) were investigated by a multinomial logistic regression model, where BMI, number of pregnancies, Kristeller's manoeuvre and episiotomy were the potential determinants, and age at interview, smoking habits, gestational diabetes, hypothyroidism, use of steroids during gestation the possible confounders.
The association between DRA severity and related disorders (postural pain/discomfort, urinary or faecal incontinence, abdominal hernia, pelvic prolapse) was investigated by Fisher's exact test or chi-squared test. These associations were further investigated by multivariable logistic models, where abdominal hernia (0 = no, 1 = yes), pelvic prolapse (0 = no, 1 = yes) or urinary incontinence (0 = no, 1 = yes) was the response variable, DRA severity was the main determinant, and BMI, number of pregnancies, Kristeller's manoeuvre, episiotomy, age at interview, smoking habits, gestational diabetes, hypothyroidism, use of steroids during gestation were potential confounders.
Results
Determinants of severity of rectus abdominis diastasis
In almost two-thirds of the participants (2,983/4,629 = 64.4%) diastasis affected both the supra- and sub-umbilical areas. Diastasis width was moderate (3–5 cm) in 54.9% of cases, and severe (>5 cm) in 27.6%.
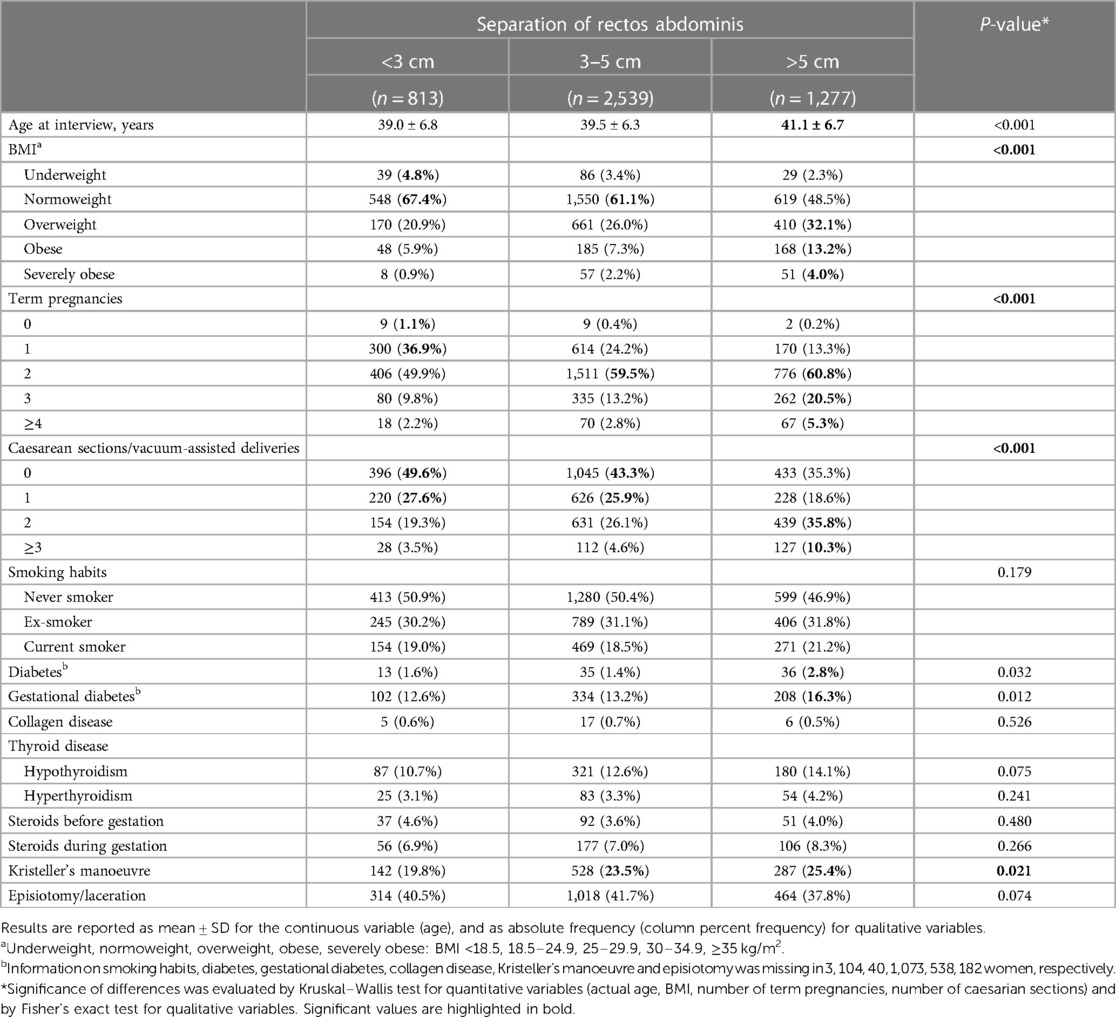
The separation between rectal muscles increased with age at interview, BMI, and number of term pregnancies (p < 0.001). Separation >5 cm was recorded in 18.8%, 22.8%, 33.0%, 41.9%, 44.0% of underweight, norm weight, overweight, obese, severely obese women, respectively (Table 1). As regards number of term pregnancies, separation >5 cm was observed in 10.0% of nulliparous women, 27.1% of women with 1–3 term pregnancies and 43.2% of women with 4 or more term pregnancies. This trend became even steeper when considering caesarean sections or otherwise assisted deliveries, as the proportion of separation >5 cm increased from 23.1% in women never undergoing caesarean delivery to 47.6% in women undergoing 3 or more caesarean deliveries. The proportion of diabetes increased from 1.6% in women with separation <3 cm to 2.8% in women with separation >5 cm (p = 0.032); likewise, the proportion of gestational diabetes increased from 12.6% to 16.3% (p = 0.012). Among delivery characteristics, Kristeller's manoeuvre was associated with larger separation between Rectus Abdominis: the manoeuvre was reported by 19.8% of women with separation <3 cm and by 25.4% of those with separation >5 cm (p = 0.021). On the contrary, a negative trend was observed between diastasis severity and episiotomy/laceration from delivery, although the association did not achieve statistical significance (p = 0.074). Severity of rectal muscle separation was not significantly affected by smoking habits, collagen or thyroid disease, steroid treatment whether administered before or during pregnancy (Table 1).
The risk profile was substantially confirmed by multivariable analysis: in the multinomial logistic regression model, when considering separation >5 cm vs. <3 cm (reference), the relative risk ratios (RRRs) for overweight, obese, severely obese with respect to normoweight were respectively 1.92 (95% CI 1.51–2.45), 2.57 (95% CI 1.74–3.79), 5.15 (95% CI 2.26–11.77). Rectal muscle separation increased with increasing number of pregnancies: with respect to one pregnancy, the RRRs of 2, 3, ≥4 pregnancies were 3.74 (95% CI 2.91–4.79), 5.64 (95% CI 3.94–8.06), 6.15 (95% CI 3.37–11.23) respectively (Figure 1, lower panel). Kristeller's manoeuvre, which increases intra-abdominal pressure during delivery, was associated with larger separation (RRR of presence vs. absence of previous Kristeller's manoeuvre = 1.51, 95% CI 1.15–1.98), while an inverse relation was observed for episiotomy, which facilitates delivery (RRR of presence vs. absence of previous episiotomy = 0.60, 95% CI 0.48–0.76) (Figure 1, lower panel). Rectal muscle separation significantly increased with increasing age at interview: when considering separation >5 cm vs. <3 cm, the RRR for 10-year increase in age was 1.34 (1.14–1.58). Severity of rectal muscle separation was not significantly affected by either smoking habits, gestational diabetes, hypothyroidism, or corticosteroids treatment during pregnancy (Figure 1).
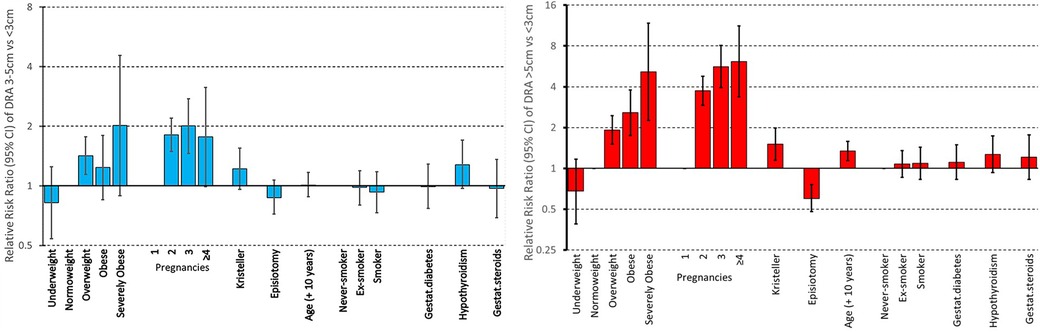
Figure 1. Multivariable analysis of determinants of severity of rectal muscle separation. Relative Risk Ratios (RRR) and p-values were computed by a multinomial model, controlling for all other variables. Nulliparous women (n = 20) were excluded from the analysis.
Association between severity of rectus muscle diastasis and post-partum disorders: urinary and faecal incontinence, postural pain/dicomfort
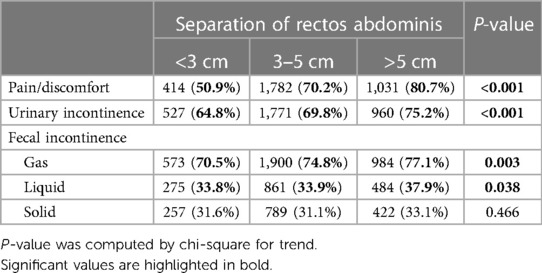
The prevalence of post-delivery disorders significantly increased with increasing separation of rectal muscles. The prevalence of pain/discomfort, urinary incontinence, incontinence for gas, incontinence for liquid stools was 50.9%, 64.8%, 70.5%, 33.8% respectively in the group with separation <3 cm and rose to 80.7%, 75.2%, 77.1% and 37.9% in the group with separation >5 cm. At variance, incontinence for solid stools was not significantly affected by DRA severity (Table 2).
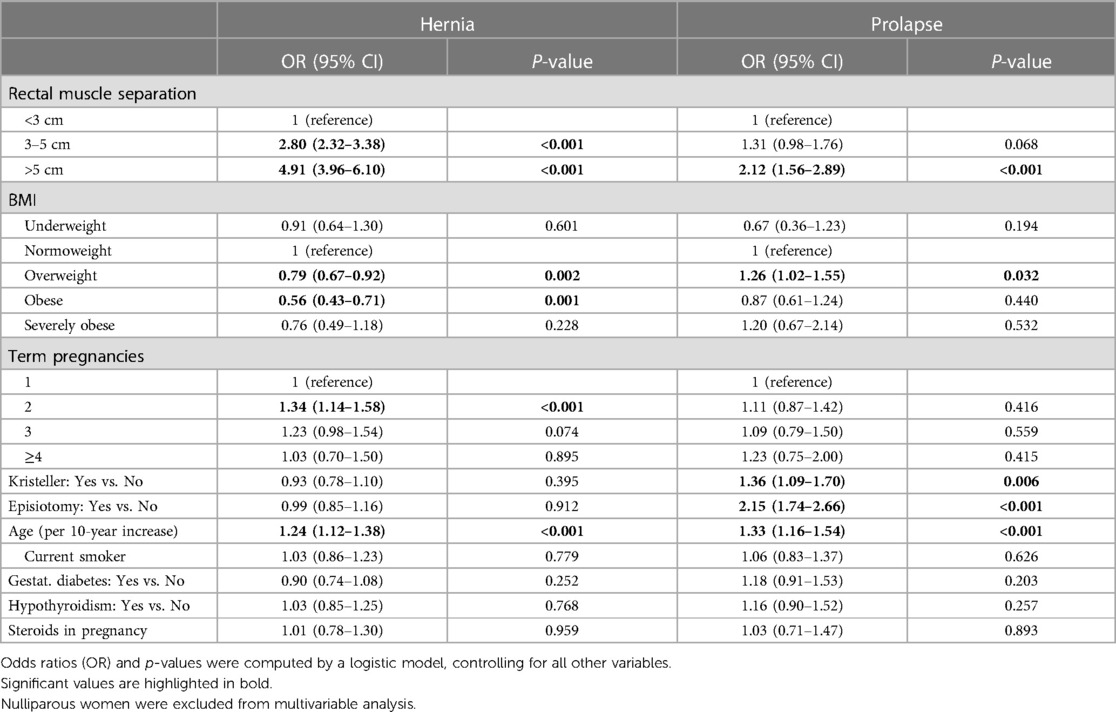
The effect of severe DRA on urinary incontinence persisted in multivariable analysis, although the association was stronger in univariable analysis (OR of severe vs. mild diastasis = 1.64, 95% CI 1.36–1.99) than in multivariable analysis (OR = 1.30, 1.04–1.62). Indeed, obesity and episiotomy were much stronger determinants of urinary incontinence than DRA severity. The risk of urinary incontinence was also increased in overweight, older women with several term pregnancies, current and ex-smokers, and women with hypothyroidism (Table 3).
Severity of DRA was strongly associated with the frequency of postural disorders (Spearman's rho = 0.273; p < 0.001). Indeed, nearly one third (32.7%) of women with mild DRA <3 cm reported no postural problems and <10% had symptoms always or during the whole daytime. These percentages were reversed in women with severe DRA >5 cm, as only 12.8% reported no postural problems, and 36.7% had symptoms always or during the whole daytime (Figure 2).
Association between severity of rectus abdominis diastasis and abdominal hernia/pelvic prolapse
Hernia and prolapse were rather frequent disorders in the population under study, affecting 54.4% and 14.6% of women, respectively. Both were strongly correlated with the severity of rectus abdominis diastasis (p < 0.001). Indeed, the prevalence of hernia increased from 31.6% in women with separation <3 cm, to 54.8% in women with 3–5 cm separation, and further to 68.2% in women with separation >5 cm. Likewise, the prevalence of prolapse increased from 9.7% to 13.4% and 20.2% (Table 4). These results were confirmed in multivariable analyses, where the severity of rectal muscle separation emerged as the strongest determinant of hernia and prolapse (Table 5).
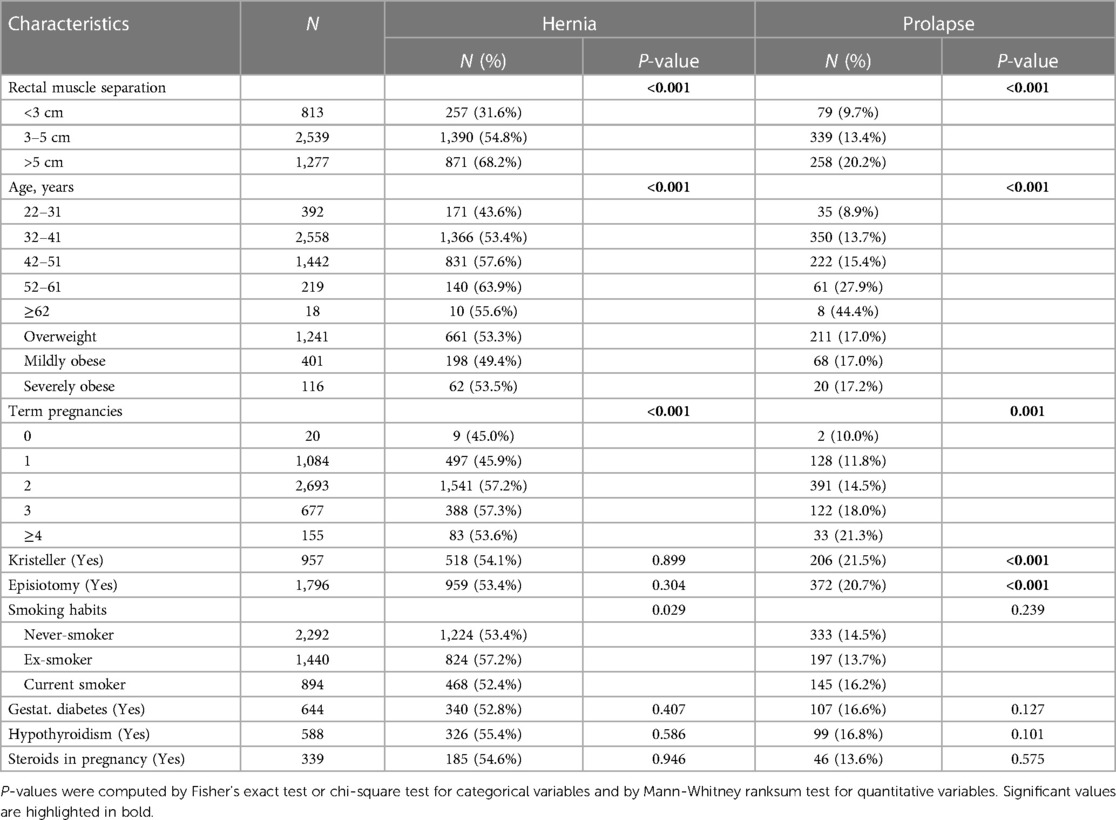
Table 4. Association between clinical characteristics, including rectal muscle separation, and hernia/prolapse.
Other important determinants of hernia were older age and a large number of pregnancies, both in univariable (Table 4) and multivariable analyses (Table 5). Obesity was negatively associated with herniation.
The risk of pelvic organ prolapse increased with advancing age, both in univariable and multivariable analyses. The effect of increasing number of pregnancies on prolapse was less pronounced than the effect on hernia, and it achieved significance only in univariable analysis. Prolapse was less common in underweight women and more prevalent in overweight ones. Both the interventions during delivery, i.e., Kristelller's manoeuvre and episiotomy, significantly increased the risk of prolapse (Table 5).
Discussion
The main results of the present study are:
(1) DRA severity markedly increases with increasing age, BMI, and number of pregnancies. Moreover, gestational diabetes and Kristeller's manoeuvre during labour are positively associated the severity of DRA, while episiotomy is negatively associated.
(2) Larger separation between rectal muscles is associated with increased risk of pain/discomfort and incontinence for liquid but not solid stools. At variance with Fei et al. (1), the present study found that the severity of DRA is associated with increased risk of urinary incontinence.
(3) Severe DRA is associated with abdominal hernia and, to a lesser extent, pelvic prolapse. Additional risk factors for hernia and prolapse are older age and a large number of pregnancies. Overweight and obesity have opposite effects on the two disorders, as they decrease the risk of hernia and increase the risk of prolapse. Interventions during delivery, i.e., Kristeller's manoeuvre and episiotomy, are associated with a significant increase in the risk of pelvic prolapse but not abdominal hernia.
The role of women's age as a risk factor of DRA is unclear. Age is reported a risk factor by Spitznagle, and most recently by Kaufmann (10, 17). On the contrary, other authors have not confirmed this finding (8, 18). These different results could be explained by ethnic and methodological factors. The study by Sperstad considered a cohort of 300 primiparous women between 19 and 40 years of age, of European ethnicity (8). Wu et al. analyzed a cohort of 644 Chinese women from 18 to 90 in age (18). They used separate cutoff values for DRA in patients under 45 years and over 45 years and, to analyze age as a risk factor, they compared 116 elderly women ≥60 years (18% of the cohort) to young women <45 years (50% of the cohort).
Our results regarding high BMI and number of pregnancies as significant risk factors for DRA severity are consistent with the results of other studies. Both obesity and pregnancy increase abdominal pressure and volume. Moreover, multiple pregnancies, as well as other factors such as lack of exercise, may contribute to cumulative mechanical stress to the connective tissue of the abdominal wall contributing to the development of a DRA (10, 17–20).
Hernia affected 54.4% of the patients with DRA in the present study and the severity of DRA was its main risk factor. Hernias are very common in patients with DRA, and in a recent paper (21) abdominal hernia was over 20 times more frequent in patients affected by DRA compared to general population. Umbilical hernia was the most common type of hernia in women (38%) and presented the highest incidence in their reproductive years (21).
Application of fundal pressure during the second stage of labor (Kristeller's maneuver) is sometimes used to accelerate fetal head delivery. The maneuver is associated with a high risk of pelvic floor injury and consequent onset of prolapse of pelvic organs (22, 23). Given our results, we can assume that the maneuver also induces damage of the linea alba leading to a separation between the rectus abdominis.
Our work supports the view that not only DRA onset but also its severity are mainly affected by conditions leading to an increase in intra-abdominal pressure during gestation and childbirth. In particular, the number of pregnancies, maternal obesity, and the traumatic Kristeller maneuver were among the elements analyzed. These elements may link the severity of DRA with the mechanical effect of increased intra-abdominal pressure.
Pregnancy can lead to DRA through hormonally mediated and/or mechanical effects on the abdominal musculature. During the gestation period, increased levels of relaxin, progesterone, and estrogen soften the connective tissues and weaken the linea alba. This weakening, together with the mechanical strain of the anterior abdominal wall due to the enlarging uterus, can result in a separation of the two rectus abdominis muscle along the linea alba. Moreover, it has been hypothesized that multiple pregnancies may contribute to cumulative mechanical stress to the connective tissue of the abdominal wall contributing to the development of a DRA (3, 17, 24).
Blotta has reported a relationship between collagen types in linea alba specimens, collected both above and below the level of the umbilicus, and DRA. She found that in women with diastasis recti, type I and type III collagen were less abundant than in women without diastasis (25). Others studies found that smoking, which has detrimental effects on fibroblast biology, induces a weakness of the linea alba through a deficit of hydroxyproline, an early compound in the collagen synthesis pathway (26, 27). Despite diabetes can impair wound healing and contribute to develop incisional hernias, its potential role in DRA pathogenesis is not clear (28). In a study by Wu et al. 43.0% of diabetic women had DRA while only 25.5% of non-diabetic women had the abdominal wall disorder (18). In the present study diabetes and gestational diabetes showed a significant correlation with DRA severity, but only in univariable analysis not in multivariable analysis when controlling for BMI and age (data not shown). Among other factors traditionally associated with wall pathology, the present study did not highlight any statistically significant associations between DRA severity and smoking habits, collagen disease, steroid use, and thyroid disease. These findings could therefore frame DRA as a pathology with a predominantly “mechanical” genesis.
Severity of DRA was strongly associated with the frequency of postural disorders such as back pain. It has been reported that DRA adversely affects normal trunk function but the matter is still controversial. In a recent systematic review, a positive correlation between DRA and back pain was observed in only 38.5% of the included studies (29).
Another finding of the present study is that the greater the separation of the recta, the greater the risk of both urinary and fecal incontinence. As described above, physiological urination and defecation functions can be traced back to the correct contractility of the abdominal wall muscles, so their inefficiency is related to the onset of incontinence. Unfortunately, detailed information on this disorder, such as at rest or stress incontinence, are lacking, so little can be said about the underlying abdominal dynamics alteration.
A number of studies reported that the presence of DRA can predispose pelvic floor dysfunctions which include urinary as well as fecal incontinence, although their relationship is still debated (17, 30, 31). Factors such as age, pregnancy, childbirth, type of delivery, number of births, and BMI play a role in the etiology of pelvic floor dysfunctions but are also linked to the onset of DRA (32). As two possible risk factors of DRA are connective tissue weakness and increased intra-abdominal pressure, which are also risk factors for pelvic floor diseases, it can be reasonably assumed that there are common causes. However, a mild effect of DRA severity on urinary incontinence persisted as significant even when controlling for obesity, number of pregnancies, episiotomy. Anyway, further studies are needed to clarify the relationship between DRA and dysfunctions of the pelvic floor.
In recent years some studies have evaluated the effects of surgical treatment of DRA on symptoms such as postural disorders, back pain, and urinary incontinence. The results of these analyses support the role of DRA in determining these symptoms. Indeed, surgical reconstruction of the linea alba can restore the normal anatomy of the abdominal wall with an improvement of abdominal trunk function and urinary incontinence (33–35).
Abdominal hernia and pelvic prolapse were frequent comorbidities in this population of women were rather frequent disorders in the population under study, affecting 54.4% and 14.6% of women with pelvic prolapse. Indeed, DRA severity emerged as the strongest determinant of both abdominal hernia and pelvic prolapse.
Strengths and limitations
Our study has some limitations. First, the sample was not randomly drawn from the general population but rather originates from a pathology registry, so that it is not possible to estimate prevalence of DRA but only of DRA severity and its determinants. Moreover, participation in the survey was not large, reaching a response rate of about 20%.
In addition, this study did not consider the impact of DRA and associated symptoms on aesthetics and quality of life.
Conclusions
The prospects arising from our work confirm and possibly consolidate our knowledge on individual risk factors for the development of severe DRA and related disorders. Of course, the associations observed in this cross-sectional study should be confirmed in prospective cohort studies. A subsequent step could be to develop a risk score for predicting the development and/or worsening of DRA, which could allow the implementation of preventive pre-delivery measures.
Data availability statement
The datasets presented in this article are not readily available due to data protection regulation. Data are available from the corresponding author, on reasonable request. Requests to access the datasets should be directed to Giuseppe Verlato,Z2l1c2VwcGUudmVybGF0b0B1bml2ci5pdA==.
Ethics statement
The studies involving humans were approved by Ethics Committee of Treviso, Italy. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AS: Conceptualization, Investigation, Resources, Supervision, Writing – original draft, Writing – review & editing. AT: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing, Supervision. EB: Writing – original draft, Writing – review & editing. JA: Writing – original draft, Writing – review & editing. EL: Writing – original draft, Writing – review & editing. GC: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. GV: Data curation, Formal Analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. AD: Conceptualization, Investigation, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
The Article Processing Fee was paid by the University of Verona, Italy, special grant for open access publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2024.1360207/full#supplementary-material
References
1. Fei H, Liu Y, Li MX, He J, Liu XL, Li JH, et al. The relationship of severity in diastasis recti abdominis and pelvic floor dysfunction: a retrospective cohort study. BMC Women’s Health. (2021) 21:68. doi: 10.1186/s12905-021-01194-8
2. Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. The normal width of the linea alba in nulliparous women. Clin Anat. (2009) 22(6):706–11. doi: 10.1002/ca.20836
3. Chiarello C, Falzone L, McCaslin K, Patel M, Ulery KR. The effects of an exercise program on diastasis recti abdominis in pregnant women. J Womens Health Phys Ther. (2005) 29(1):11–6. doi: 10.1097/01274882-200529010-00003
4. Hernández-Granados P, Henriksen NA, Berrevoet F, Cuccurullo D, López-Cano M, Nienhuijs S, et al. European hernia society guidelines on management of rectus diastasis. Br J Surg. (2021) 108(10):1189–91. doi: 10.1093/bjs/znab128
5. Coldron Y, Stokes MJ, Newham D, Cook K. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. (2008) 13(2):112–21. doi: 10.1016/j.math.2006.10.001
6. Fernandes da Mota PG, Pascoal AG, Carita AI, Bo K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. (2015) 20(1):200–5. doi: 10.1016/j.math.2014.09.002
7. Gustavsson C, Eriksson-Crommert M. Physiotherapists' and midwives' views of increased inter recti abdominis distance and its management in women after childbirth. BMC Womens Health. (2020) 20(1):37. doi: 10.1186/s12905-020-00907-9
8. Sperstad JB, Tennfjord MK, Hilde G, Ellstrom-Engj M, Bo K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. (2016) 50(17):1092–6. doi: 10.1136/bjsports-2016-096065
9. Liaw LJ, Hsu MJ, Liao CF, Liu MF, Hsu AT. The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: a 6-month follow-up study. J Orthop Sports Phys Ther. (2011) 41(6):435-43. doi: 10.2519/jospt.2011.3507
10. Kaufmann RL, Reiner CS, Dietz UA, Clavien PA, Vonlanthen R, Käser SA. Normal width of the linea alba, prevalence, and risk factors for diastasis recti abdominis in adults, a cross-sectional study. Hernia. (2022) 26:609–18. doi: 10.1007/s10029-021-02493-7
11. Baumann DP, Butler CE. Diastasis recti and primary midline ventral hernia: the plastic surgery approach. Hernia. (2019) 23:1017-8. doi: 10.1007/s10029-019-02055-y
12. Mommers EHH, Ponten JEH, Al Olmar AK, Reilingh TSD, Bouvy ND, Nienhuijs SW. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. (2017) 31:4934–49. doi: 10.1007/s00464-017-5607-9
13. Carlstedt A, Bringman S, Egberth M, Emanuelsson P, Olsson A, Petersson U, et al. Management of diastasis of the rectus abdominis muscles: Recommendations for Swedish National Guidelines. Scand J Surg. (2021) 110(3):452-9. doi: 10.1177/1457496920961000
14. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. (1993) 36:77–97. doi: 10.1007/BF02050307
15. Hilton P, Robinson D. Defining cure. Neurourol Urodyn. (2011) 30(5):741–5. doi: 10.1002/nau.21098
16. Ranney B. Diastasis recti and umbilical hernia causes, recognition and repair. SDJ Med. (1990) 43(10):5–8.
17. Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct. (2007) 18:321–8. doi: 10.1007/s00192-006-0143-5
18. Wu L, Gu Y, Gu Y, Wang Y, Lu X, Zhu C, et al. Diastasis recti abdominis in adult women based on abdominal computed tomography imaging: prevalence, risk factors and its impact on life. J Clin Nurs. (2020) 30:518–27. doi: 10.1111/jocn.15568
19. Benjamin DR, van de Water ATM, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. (2014) 100(1):1–8. doi: 10.1016/j.physio.2013.08.005
20. Cavalli M, Aiolfi A, Bruni PG, Manfredini L, Lombardo F, Bonfanti MT, et al. Prevalence and risk factors for diastasis recti abdominis: a review and proposal of a new anatomical variation. Hernia. (2021) 25:883–90. doi: 10.1007/s10029-021-02468-8
21. Yuan S, Wang H, Zhou J. Prevalence and risk factors of hernia in patients with Rectus abdominis diastasis: a 10-year multicenter retrospective study. Front Surg. (2021) 8:730875. doi: 10.3389/fsurg.2021.730875
22. Sartore A, De Seta F, Maso G, Ricci G, Alberico S, Borelli M, et al. The effects of uterine fundal pressure (Kristeller maneuver) on pelvic floor function after vaginal delivery. Arch Gynecol Obstet. (2012) 286:1135–9. doi: 10.1007/s00404-012-2444-x
23. Youssef A, Salsi G, Cataneo I, Pacella G, Azzarone C, Paganotto MC, et al. Fundal pressure in second stage of labor (Kristeller maneuver) is associated with increased risk of levator ani muscle avulsion. Ultrasound Obstet Gynecol. (2019) 53:95–100. doi: 10.1002/uog.19085
24. Thabet AA, Alshehri MA. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. J Musculoskelet Neuronal Interact. (2019) 19(1):62–8.30839304
25. Blotta RM, Costa SDS, Trindade EN, Meurer L, Maciel-Trindade MR. Collagen I and III in women with diastasis recti. Clinics (Sao Paulo). (2018) 73:e319. doi: 10.6061/clinics/2018/e319
26. Jorgensen LN, Kallehave F, Christensen E, Siana JE, Gottrup F. Less collagen production in smokers. Surgery. (1998) 123(4):450–5. doi: 10.1016/S0039-6060(98)70167-9
27. McPhail I. Abdominal aortic aneurysm and diastasis recti. Angiology. (2008) 59:736–9. doi: 10.1177/0003319708319940
28. Reilly MJ, Larsen NK, Agrawal S, Thankam FG, Agrawal DK, Fitzgibbons RJ. Selected conditions associated with an increased incidence of incisional hernia: a review of molecular biology. Am J Surg. (2021) 221:942–9. doi: 10.1016/j.amjsurg.2020.09.004
29. Sokunbi G, Camino-Willhuber G, Paschal PK, Olufade O, Hussain FS, Shue J, et al. Is diastasis recti abdominis associated with low back pain? A systematic review. World Neurosurg. (2023) 174:119–25. doi: 10.1016/j.wneu.2023.03.014
30. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. (2001) 20(1):31-42. doi: 10.1002/1520-6777(2001)20:1 31::aid-nau5 3.0.co;2-p11135380
31. Wang Q, Yu X, Chen G, Sun X, Wang J. Does diastasis recti abdominis weaken pelvic floor function? A cross-sectional study. Int Urogynecol J. (2020) 31(2):277-83. doi: 10.1007/s00192-019-04005-9
32. Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. (2014) 123(1):141–8. doi: 10.1097/AOG.0000000000000057
33. Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O. Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open. (2019) 3(6):750–8. doi: 10.1002/bjs5.50213
34. Olsson A, Kiwanuka O, Sandblom G, Stackelberg O. Evaluation of functional outcomes following rectus diastasis repair-an up-to-date literature review. Hernia. (2021) 25(4):905–14. doi: 10.1007/s10029-021-02462-0
Keywords: diastasis recti abdominis, risk factor, incontinence, prolapse, hernia abdominalis
Citation: Sartori A, Tfaily A, Botteri E, Andreuccetti J, Lauro E, Caliskan G, Verlato G and Di Leo A (2024) Rectus muscle diastasis in Italian women: determinants of disease severity, and associated disorders. Front. Surg. 11:1360207. doi: 10.3389/fsurg.2024.1360207
Received: 22 December 2023; Accepted: 19 February 2024;
Published: 11 March 2024.
Edited by:
Francesco Giovinazzo, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Victor Radu, Life Memorial Hospital, RomaniaStefano Bona, Humanitas Research Hospital, Italy
© 2024 Sartori, Tfaily, Botteri, Andreuccetti, Lauro, Caliskan, Verlato and Di Leo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giuseppe Verlato Z2l1c2VwcGUudmVybGF0b0B1bml2ci5pdA==
 Alberto Sartori
Alberto Sartori Ahmad Tfaily
Ahmad Tfaily Emanuele Botteri3
Emanuele Botteri3 Jacopo Andreuccetti
Jacopo Andreuccetti Gulser Caliskan
Gulser Caliskan Giuseppe Verlato
Giuseppe Verlato