
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Surg. , 07 November 2024
Sec. Orthopedic Surgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1357897
 Utpal K. Dhar1
Utpal K. Dhar1 Emma Lilly Menzer1
Emma Lilly Menzer1 Maohua Lin1
Maohua Lin1 Timothy O’Connor2
Timothy O’Connor2 Nischal Ghimire3
Nischal Ghimire3 Elias Dakwar2
Elias Dakwar2 Ioannis D. Papanastassiou4
Ioannis D. Papanastassiou4 Kamran Aghayev5
Kamran Aghayev5 Chi-Tay Tsai1
Chi-Tay Tsai1 Frank D. Vrionis2*
Frank D. Vrionis2*
Objectives: Lumbar spinal stenosis (LSS) refers to a narrowing of the space within the spinal canal, which can occur at any level but is most common in the lumbar spine. Open laminectomy and minimally invasive laminectomy (MIL) procedures are the most common surgical gold standard techniques for treating LSS. This study aims to review clinical and biomechanical literature to draw comparisons between open laminectomy and various MIL techniques. The MIL variation comprises microendoscopic decompression laminotomy, unilateral partial hemilaminectomy, and microendoscopic laminectomy.
Methods: A review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. We reviewed 25 clinical, 6 finite element, and 3 cadaveric studies associated with treating LSS. We reviewed literature that discusses factors such as operation time, length of hospital stay, postoperative complications, reoperation rate, effect on elderly patients, patients’ satisfaction, and adjacent segment disease degeneration for the clinical studies, whereas the range of motion (ROM), von Mises stresses, and stability was compared in biomechanical studies.
Results: MIL involves less bone and ligament removal, resulting in shorter hospital stays and lower reoperation and complication rates than open laminectomy. It improves the quality of health-related living standards and reduces postoperative pain. Biomechanical studies suggest that laminectomy and facetectomy increase annulus stress and ROM, leading to segmental instability.
Conclusion: Although theoretically, MIL means less tissue injury, pain, and faster recovery in the short term, the long-term results depend on the adequacy of the decompression procedure and tend to be independent of MIL or open laminectomy.
Lumbar spinal stenosis (LSS) is a consequence of degeneration of the lumbar spine, categorized by narrowing of the spinal canal and the neural foramina. This narrowing can cause compression of the spinal cord and nerve roots running through these channels resulting in potentially severe pain, motor, and sensory deficits (1, 2). LSS is a common condition primarily affecting older adults due to age-related spine degeneration (1, 3). Stenosis is more likely to affect the lumbar spine than other regions, and research suggests that the probability of stenosis occurring in the lumbar spine is about five times that of the cervical spine (4). Generally, mild stenosis occurs in 22.6%–77.9% of people whereas moderate or severe stenosis takes place in 8.40%–30.4% of the population over the age of 40 (2). Open surgical laminectomy and minimally invasive decompression (MID) surgery are two common procedures for treating LSS in the absence of instability (5–11).
LSS can have substantial implications for patients and is known to be a significant driver of morbidity in the older population (12–15). There is considerable overlap in the main surgical approaches for these conditions, two of which are minimally invasive laminectomy (MIL) techniques and open laminectomy (8, 10, 16–19). MIL has become increasingly popular in recent decades due to its cost-effectiveness (20). Additionally, some research suggests that MIL techniques may also provide benefits such as reduced blood loss, shortened hospital stays, reduced pain, and improved quality of life (7, 10, 21, 22). Laminectomies, facetectomies, and MIL techniques are common methods that aim to decompress the lumbar spine in cases of LSS. Historically, open laminectomies have been the standard treatment for LSS (23–27). This procedure attempts to relieve symptoms by removing various structures, including the spinous process and laminae; however, several limitations and disadvantages are associated with this approach. For example, some clinical research has demonstrated postoperative instability, degenerative disease, and lumbar spine deformity, among other potential complications (22, 28–30). On the other hand, MIL techniques aim to minimize tissue disruption and preserve most of the posterior elements to potentially provide better load-bearing capacities and biomechanical stability (31–34).
In addition to clinical research, biomechanical research and stability analyses also provide critical insights. Various in vitro studies using human cadavers have been conducted to explore lumbar spine stability. However, this approach has limitations, such as anatomical differences between cadavers (35). Finite element analyses (FEAs) can overcome various limitations given their efficiency, consistency, and reproducibility. FEAs are a powerful tool for studying different segment motions (rotational or translational) and stress–strain relationships and providing necessary parameters for a fuller understanding (18, 31, 36). FEAs offer distinct insights from a biomechanical standpoint and can provide surgeons with valuable insights to facilitate future surgical procedures (33, 37–41). Few review papers were published in clinical studies that correlate with the biomechanical studies for the cervical spine (42, 43). The present study aims to analyze and compare the literature between laminectomy and minimally invasive surgery for both clinical and biomechanical aspects of human LSS.
Our review followed the PRISMA instruction for selecting the literature (44). A search was conducted in PubMed for articles containing the keywords “laminectomy,” “minimally invasive surgery,” “decompression techniques,” “laminotomy,” and “lumbar spinal stenosis.” A flow diagram of how the clinical and biomechanical studies were selected for the review is shown in Figure 1.
All titles and abstracts were first examined, and those that did not meet the criteria in Table 1 were removed. Subsequently, all remaining articles were reviewed in full. Studies were limited to only those looking at the human lumbar spine and written in the English language. Studies of the thoracic and cervical spine were also excluded. In the current study, MIL variance included such as microdecompressive laminotomy (MDL), windows technique (WT), unilateral microendoscopic laminectomy (MEL), microendoscopic posterior decompression (MEPD), minimally invasive decompression, unilateral partial hemilaminectomy (UPHL), and spinous process splitting decompression (SPSD). The MIL techniques that involved fusion with internal instrumentation and interbody cages were excluded in this review.
Independent reviewers (UD and EM) extracted data from all eligible studies Finally, the articles were grouped by content. All clinical studies were grouped into the following categories, “Operative time,” “Length of hospital stay,” “Postoperative complication,” “Re-operation rate,” “Effect on elderly patients,” “Patient satisfaction,” and “Adjacent segment diseases.” It is obvious that the MIL technique involves less muscle, bone, or ligament removal; hence, the blood loss would be less compared with the laminectomy procedure. Hence, we did not compare the blood losses between these procedures in our review. On the contrary, all biomechanical studies were grouped into the following categories, “FEA study” and “Cadaveric study” where laminectomy was compared with its variant.
A total of 9 biomechanical studies and 25 clinical studies were selected. In clinical studies, 16 described the mean operative time, 21 stated postoperative complications, 11 reported reoperation rate, 2 reported adjacent segment diseases, 6 reported effects on elderly patients, and almost all studies described patient satisfaction. Numerous studies also described the length of hospital stay for open laminectomy and MIL technique for LSS. Of the biomechanical studies, six FEA studies and three cadaveric studies compared the laminectomy with its variant.
Clinical studies comparing open laminectomy and MIL techniques for LSS have been conducted to evaluate the outcomes and efficacy of these surgical approaches. We reviewed the various clinical studies regarding operative time, hospital stay, operation level, age, surgical level, postoperative complications, reoperation rate, adjacent segment degeneration, and patients’ satisfaction as it relates to the open laminectomy vs. MIL techniques. Overall, clinical studies suggest that the MIL technique offers advantages such as less hospital stay, lower reoperation rate, fewer postoperative complications, and reduced chance of adjacent segment disease (ASD) than the open laminectomy. Figure 2 shows a typical MIL technique and laminectomy procedure.
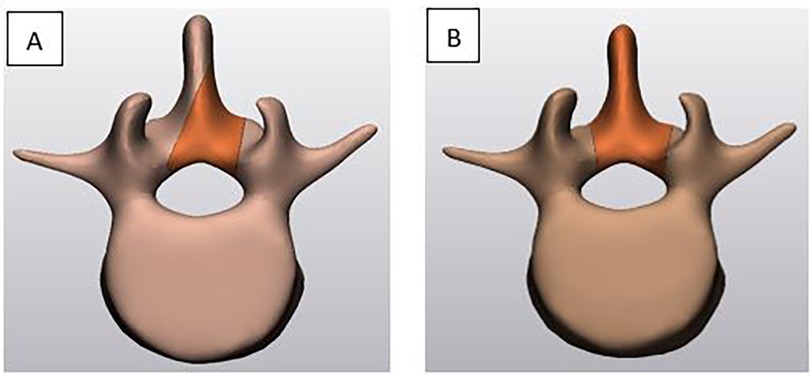
Figure 2. A typical minimally invasive unilateral laminotomy (A) versus traditional laminectomy (B).
Most clinical studies mentioned the duration of operation for open laminectomy and MIL technique for LSS. Operative time for surgical procedures can vary depending on various factors, including the complexity of the surgery, the surgeon's experience, patient-specific factors, and the specific technique used. Larger removal of the bone, ligaments, and muscle in the laminectomy leads to longer healing time but shorter operative time.
In this review, the minimum mean operative time was observed from Kanbara et al. (45) and the maximum from Cho et al. (46). In most studies, the MIL technique needs higher operative time than the open laminectomy procedure (28, 46–49). In this review, we found the average operative time per level for the MIL technique was 120 min whereas it was 90 min for the laminectomy. This time frame is the average and may not apply to every individual case.
The length of hospital stay for a laminectomy and MIL for LSS can vary based on several factors such as patient's overall health, the extent of the surgery, and the specific hospital's protocols. Several studies suggested that the MIL technique usually has a shorter hospital stay compared to open laminectomy. Lundberg et al. (20) concluded that for the patients who underwent laminectomy, the average patient's stay in the hospital was 3 days whereas less than 1 day for MIL. Ang et al. (21) also confirmed that the length of hospital stay for open laminectomy was 3 days whereas 1.1 days for the MIL procedure. Multiple clinical studies suggested that there is no significant difference in the length of hospital stay for the number of levels treated in each procedure. For example, Nerland et al. (22) showed two levels and one level laminectomy required an average of 3.1 and 3.4 days for decompression. Similarly, in the MIL group, there was no significant difference for one- or two-level decompression (1.9 days vs. 2.3 days). Mobbs et al. (10) also confirmed that the open laminectomy required a higher length of postoperative hospital stay than the minimally invasive unilateral laminectomy (55.1 vs. 100.8 h).
Several studies have examined postoperative complications and factors influencing these complications after surgery for lumbar spine diseases. Both open laminectomy and MIL procedures are safe for lumbar spinal stenosis. Multiple clinical studies demonstrated that elderly patients have a higher postoperative complication rate than that younger patients for both procedures (46, 49–54). These complications include wound infection, cerebrospinal fluid (CSF) leakage, hematoma, and nerve injury in addition to anesthesia-related complications. According to Ikuta et al. (48), the postoperative complication rate in the open laminectomy group was 14% lower compared with the MIL posterior decompression (25%). Additionally, Ang et al. (21) noticed that 3 out of 83 patients had durotomies in the MIL group and no complications for the patients with open laminectomy. Pietrantonio et al. (7) reviewed patients with LSS who underwent open laminectomy or bilateral laminotomy LSS surgical treatment. Clinical outcomes were similar between the two groups, although the complication rate was slightly above for the total laminectomy group than the bilateral laminotomy group. Harrington et al. (55) did not find any difference in postoperative complications for open and MIL procedures. Shih et al. (28) also confirmed that there was no difference in minor postoperative complications between these two procedures (30.1% vs. 34.7%) although only one patient showed wound complication in the open group. Some other researchers such as Rahman et al. (30) found a significant difference in postoperative complications between open laminectomy and minimally invasive decompression (16.1% vs. 7.9%). Details of clinical prospective and retrospective studies are shown in Table 2.
Oichi et al. (59) studied the incidence of postoperative complications between patients treated by microendoscopic laminectomy (MEL) vs. open laminectomy. Analysis of 3,072 individuals—1,536 in each group—revealed that those in the MEL group were significantly less likely to endure a postoperative complication, develop a surgical site infection (SSI), or have postoperative delirium due to longer surgical operation than those in the open laminectomy group. Horan et al. (27) also compared the outcomes of LSS patients treated via two unique surgical approaches—MIL bilateral laminotomy via unilateral approach and open laminectomy. The MIL approach was found to be better among various measures and specifically was shown to have lower complication rates than the open laminectomy.
Following lumbar spine surgery, some individuals require reoperation, although the factors putting those patients at higher risk for needing additional surgery are not clearly understood. Several studies have examined postoperative complications and elements influencing reoperation rates after surgery for lumbar spine diseases. Due to inadequate decompression in open laminotomy or MIL procedure, a patient may need revision surgery. Some studies reported that due to CSF leaking, patients need revision surgery in both the laminectomy and MIL groups. Incidental durotomy, scar tissue formation, spinal instability, adjacent segment disease, and recurrent disc herniation are the major reasons for the revision surgery. Out of 25 studies, 11 documented the reoperation rate in this review.
Following open laminectomy or MIL procedure, reoperation risk may be influenced by gender, age, smoking, surgical level, wound infection, hematoma, fusion, etc. Thomé et al. (6) found no significant difference between bilateral laminotomy, unilateral laminotomy, and laminectomy. Because a large amount of bone was removed in the open laminectomy group, postoperative instability was developed, and five patients needed reoperation with instrumentation-assisted fusion. In contrast, no instrumented fusion was required in the bilateral laminotomy group, except for two patients in the unilateral laminotomy group. Mobbs et al. (10) concluded that for the unilateral laminotomy, the reoperation rate was nearly 4%, while it was 11% for the laminectomy for bilateral decompression. According to them, the progression of spinal degeneration may cause a need for reoperation, while wound infection, hematoma, and wound dehiscence cause the rest. In another study, Pietrantonio et al. (7) showed that the open laminectomy group underwent surgery four times more than the laminotomy group. In the laminotomy group, 4 patients required reoperation due to insufficient decompression while 16 patients in the laminectomy group required fusion surgery due to post-laminectomy instability. Horan et al. (27) found that 1 out of 37 patients underwent reoperation following MIL procedures; in contrast, 3 out of 25 following the laminectomy procedure underwent reoperation. In both groups, revision surgery was required due to CSF leakage. As per Ovalioglu et al.’s (52) findings, 5 of 144 patients needed repeated operation after spinous process splitting decompression while 4 of 132 patients for the conventional laminectomy group. According to Erol et al. (53), dural tears occurred in 7 of 34 patients, but none of them, who underwent microdecompressive laminotomy after 5 years of follow-up, needed revision surgery. A prospective study carried out by Morgalla et al. (50) found that 2 out of 108 patients required reoperation and fusion as a result of postoperative instability in the laminectomy, hemilaminectomy, and partial hemilaminectomy groups. Although a CSF fistula was observed in three patients, it was treated using external lumbar drainage instead of revision surgery. Ikuta et al. (48) determined that 2 out of 44 patients needed repeated operation due to the presence of postoperative epidural hematoma in the microendoscopic posterior decompression group whereas 3 out of 29 patients needed revision surgery due to disc herniation in the open laminotomy group. Ang et al. (21) reported that 2 out of 83 patients who underwent the MIL technique required revision surgery due to a higher rate of inadvertent durotomies while in the open laminectomy, no patient needed reoperation at 24 months follow-up. Liu et al. (49) suggested that unilateral laminotomy and conventional laminectomy do not require any revision surgery as no postoperative instability was observed in both groups at the final follow-up. Therefore, most clinical studies suggested that the reoperation rate is not significant between the conventional laminectomy and MIL technique.
Adjacent segment disease (ASD) occurs when an adjacent segment is adversely impacted following spine surgery, requiring reoperation. When an open laminectomy or MIL is performed on the lumbar spine, the adjacent segment may also be affected. For example, operation on L3–L4 may also impact L2–L3 or L4–L5. The affected segment can be evaluated or determined by clinical evidence or radiological analyses. When comparing open laminectomy and MIL techniques for LSS, the impact on adjacent segment disease is an important consideration. Most of the patients who required reoperation were not for the same level of restenosis. Thomé et al. (6) reported that after unilateral or bilateral laminotomy, there was no adjacent level stenosis except for one patient in a laminectomy procedure. Erol et al. (53) did not find any postoperative adjacent level stenosis in both traditional laminectomy and microdecompressive laminotomy based on 71 patients with 5 years of follow-up.
For the elderly population, MIL techniques are proposed to be the more suitable procedures for LSS. Khoo et al. (47) concluded that as the microendoscopic decompression laminotomy is associated with less bone and ligament disruption, it is more beneficial to elderly patients offering quicker recovery than an open laminectomy. Additionally, the minimally invasive decompression technique required shorter hospitalization time, and no significant complications were observed during the study. The minimally invasive lumbar spine decompression was found to be both safe and adequate for addressing lumbar degenerative diseases in elderly patients. Erol et al. (53) also suggested that less blood loss and less surgical tissue trauma help the elderly population to early mobilization in the microendoscopic laminotomy procedure. A prospective study carried out by Mobbs et al. (10) suggested that the minimally invasive unilateral laminotomy for bilateral decompression is very beneficial for elderly patients as the postoperative pain and hospital stay are less. In contrast, Yagi et al. (57) stated that the elderly Asian population had relatively smaller vertebrae, making it more difficult for adequate decompression using a unilateral approach. Some researchers such as Nerland et al. (22) did not find a statistically significant difference between laminectomy and microendoscopic decompression procedures for patients aged over 70. Similarly, Morgalla et al. (50) also did not find any difference between laminectomy, unilateral hemilaminectomy, and partial hemilaminectomy by studying patients aged over 60 in 1-year follow-up. The recovery time and improvement of quality of life were similar between the elderly and young patients showed by Aleem et al. (51).
Thomé et al. (6) compared patient satisfaction between 120 LSS patients in one of three treatment groups—those who underwent bilateral laminotomy, unilateral laminotomy, and laminectomy. While there was not a significant difference in lower back pain at rest between groups, more patients in the conventional laminectomy group reported lower back pain during walking than the other two groups. Additionally, the bilateral laminotomy was associated with greater improvements in the visual analog scale (VAS). According to this study, patient satisfaction was significantly higher among patients who underwent the bilateral laminotomy than the other two procedures in treating LSS.
Rosen et al. (1) studied Oswestry disability index (ODI) scores, visual analog scale pain scores, and short-form 36 scores following minimally invasive decompression of lumbar degenerative disease for patients aged 75 years and above. The difference between preoperative and postoperative ODI and VAS scores was significant for the minimally invasive decompression technique. Parker et al. (26) studied 54 patients who underwent one of two treatments—MIL multilevel hemilaminectomy or open multilevel hemilaminectomy—for degenerative LSS. Their primary goal was to analyze the cost-effectiveness of these two procedures. There was no significant difference between each in terms of long-term pain relief, lifestyle, and long-term efficiency. Moreover, they found that the total direct and indirect costs for these two procedures are quite similar (10). In a prospective, 1:1 randomized trial, Mobbs et al. (10) looked at several preoperative and postoperative measures to evaluate minimally invasive unilateral laminectomy for bilateral decompression (ULBD) vs. the standard open laminectomy for LSS treatment. Although there was no significant difference in ODI scores between groups, the difference in VAS scores was significantly better among the ULBD patients compared to those in the open laminectomy group. The patients in the ULBD group also used relatively less opioids than those who underwent open laminectomy. Overall, leg pain, hospital stay, and postoperative pain significantly improved with the ULBD approach compared to the open laminectomy.
Biomechanical studies play a crucial role in comparing different surgical techniques for LSS, such as open laminectomy and MIL techniques. These studies aim to assess the effects of each technique on the biomechanical properties of the spine, including spinal stability, range of motion (ROM), and load distribution. For example, calculating the von Mises stress after the surgical operation in the adjacent intervertebral disc can predict the possibility of adjacent segment degeneration diseases. The changing ROM after open laminectomy or MIL technique can notify how biomechanically stable the spinal column is postsurgery. The larger the removal of posterior elements or ligaments, the greater the risk of spinal stability. We have overviewed six FEA and four cadaveric studies comparing laminectomy and MIL techniques.
Using a motion segment model, Lee et al. (31) evaluated the biomechanical effects of four common decompression approaches—unilateral laminectomy, unilateral laminectomy with unilateral facetectomy, unilateral laminectomy with bilateral facetectomy, and total bilateral laminectomy—for treating LSS. Under all conditions (flexion, extension, bending, torque, anterior or posterior shear), the healthy spine had a higher ROM compared to that of the disc degeneration models. Notably, this research found that for the models in which unilateral or bilateral facet joints were removed, there was a higher ROM compared with the sole laminectomy model. According to the authors, the removal of facet joints increases the annulus stress for all motions. Researchers concluded that total bilateral laminectomy with facetectomy would result in biomechanical instability for most motions.
Ivanov et al. (18) saw similar outcomes for the various MIL techniques through FEA. For younger patients, in most of the MIL models, the ROM did not vary with the intact spine model. However, the ROM was higher when hemilaminectomy was performed. In extension, flexion, and rotation conditions, the highest von Mises stress was observed in the hemilaminectomy model compared with other MIL models. In all physiological loading conditions, the stress on the pars interarticularis was higher in the medial facetectomy and lateral fenestration models. A clinical study suggested (60) that the pedicles are the weakest structure after the pars interarticularis. Hence, increasing stress on the pars interarticularis might lead to stress fracture after such surgeries.
Segmental motion and von Mises stress were studied by Bresnahan et al. (61) in evaluating the effects of graded posterior element removal for treating LSS. They compared two common LSS surgical techniques [complete laminectomy (OPEN) and bilateral interlaminar laminotomies (IL)] with a less invasive approach, the microendoscopic decompression for stenosis (MEDS) procedure, and for each procedure, 25%, 18%, and 25% of the posterior bony elements were removed, respectively. For the flexion condition, the resultant motion of the OPEN model was 1.8-fold higher than the intact model, and in the extension condition, it was four times higher. For left and right axial rotation, the IL or OPEN models had more than two times higher segmental motion than the intact model. There was no difference observed between the three models and the intact model for left and right lateral bending. In all physiological motions, only the MEDS model showed good correlation with the intact model. That means the posterior bony elements can be removed up to 15% without destabilizing effect. The von Mises stress on the annulus was similar in intact, MEDS, and IL models for all loading conditions. In the OPEN model, this stress was 3.6 times higher than the intact model at the surgical level which also led to spinal instability. A summary of biomechanical studies is shown in the Table 3.
Ahuja et al. (33) carried out a finite element study to determine the effects of removing facet joints in unilateral and bilateral procedures on biomechanical stability. According to this study, the removal of 45% of the unilateral facet joint increased the mediolateral spinal mobility by 30% for both flexion and extension. For the 100% removal of the unilateral facet joint, anteroposterior spinal mobility increased by 40% while mediolateral mobility increased by 80% for flexion. When the facet joints were completely removed on both sides, the anteroposterior mobility increased by 80% in flexion and 90% in extension. In flexion, for the excision of 45% of facet joints, the intradiscal pressure in L4–L5 increased by 30% for unilateral while it increased by nearly 20% for bilateral scenarios. When the facet joint was completely removed, the facet load at L4–L5 increased by more than 100% in extension for bilateral and by 60% for unilateral.
Matsumoto et al. (36) compared the conventional decompression techniques with the graded transforaminal endoscopic lateral recess decompression (TE-LRD) in a moderate disc degeneration model. In normal disc degeneration, although there are differences in 50% and 100% TE-LRD in flexion, the 100% TE-LRD had seven times higher ROM than the 50% TE-LRD in extension. The bilateral laminectomy had a higher ROM than the unilateral for both flexion and extension. The differences between the TE-LRD and all laminectomy models for left and right lateral bending are negligible. In contrast, in the severe disc degeneration model, the difference between 50% and 100% TE-LRD models was negligible for both flexion, extension, and lateral bending loading. Overall, the bilateral laminectomy model had a higher ROM than all models except for rotation. Although 50% TE-LRD increased the facet joint stress, this technique had the least amount of annulus stresses compared with bilateral laminectomy. Hence, 50% TE-LRD was found to be the most effective technique for spinal stability compared with conventional laminectomy or facetectomy. Table 2 shows the FEA and cadaveric studies that involved the open laminectomy and MIL procedures.
Lin et al. (63) investigated how graded posterior bone and ligaments affect the von Mises stresses on the annulus and spinal column by FE analyses. According to their findings, there is little impact on the annulus at the surgical level for the unilateral laminotomy while the ROM increases for the flexion and rotation of the laminectomy associated with the facetectomy. They also created eight layers of the annulus in their models and found that the outmost layer has the maximum von Mises stresses than the inner layer. According to their shear stress analysis, flexion showed higher streses compared with extension, bending, or torque. Overall, when the laminectomy was associated with the facetectomy, the shear stress was approximately 24% higher than the intact model.
Bisschop et al. (38) found that single-level laminectomy does not affect the adjacent segments but increases the ROM at the index level. According to this study, the ROM increased by 7%–12% after single-level laminectomy. For the adjacent level, there were slight effects for lateral bending and no changes were observed for flexion, extension, or axial rotation. It is also interesting to note that the spinal stiffness was not significantly affected in both adjacent segments and index level. Finally, based on the cadaveric biomechanical study, it was concluded that no instrumentation is required for biomechanical stability when the laminectomy is performed at a single level.
To elucidate distinctions between the laminectomy and bilateral laminotomy of the human lumbar spine, Lee et al. (41) used a cadaveric simulation model and measured segmental motion and stiffness. They identified that the average ROM at the surgical level for the bilateral laminotomy increased by 14.3% while this increased by 32% after laminectomy for flexion and extension. After laminotomies, stiffness was reduced by 11.8% and by 27.2% after laminectomy, which was significantly different. Although some have stated there are differences in axial rotation compared to the intact model, Lee et al. (41) did not find any effect for axial rotation or lateral bending. Consequently, the laminotomies resulted in better biomechanical stability than the laminectomy in decompressing the spine.
Another cadaveric study by Bisschop et al. (62) aimed to determine factors influencing spinal stability after lumbar laminectomy. They documented that following the laminectomy procedure the shear stiffness (SS), shear yield force (SYF), and shear force to failure (SFF) declined by 24%, 41%, and 44%, respectively. The SFF had a comparatively lower value in both treated and untreated segments for female specimens. However, bone characteristics were not related to shear stiffness as it was more associated with SYF and SFF. The authors suggest that to evaluate postoperative instability risk, it is important to know the patient's disc shape, bone mineral contents, or density rather than the pedicle or facet geometry, as pedicle sections and facet geometry did not effectively forecast instability after lumbar laminectomy.
Bisschop et al. (37) also investigated how shear loading affects the biomechanical stability of the human lumbar spine after laminectomy. The authors present that bone mineral density (BMD) and disc degeneration affect torsional strength and stiffness respectively. [In both untreated and laminectomy groups, the early torsion stiffness (ETS) or late torsional stiffness (LTS) is increased with the BMD.] Similarly, ETS or LTS also increases with degeneration for both untreated and laminectomy groups. According to their study after laminectomy, there was an approximately 44% reduction in the strength for shear loading while the reduction in stiffness was about 20%.
LSS is a medical condition that occurs when the spinal canal in the lumbar spine narrows, putting pressure on the spinal cord and nerves. One of the challenges is that the effectiveness of different treatments can vary widely depending on the individual patient.
Most articles showed the average operating time for the MIL technique to be higher than the laminectomy procedure. In our review, only a few studies did not find the differences between the two techniques (20, 21). The length of hospital stays for an open laminectomy and MIL technique can vary depending on several factors, including the patient's specific condition, the complexity of the surgery, and the surgeon's approach. Most of the clinical studies showed that the traditional laminectomy typically requires a longer hospital stay than the MIL technique. According to our review, the average hospital stay for the laminectomy procedure and MIL technique was 3 days and 1 day, respectively (21). The patients who underwent one- or two-level open laminectomy or MIL procedure for LSS required the same length of hospital stay (22). Because of the lengthier hospital stay, clinical studies show that the hospitalization cost is also higher in the open laminectomy procedure than in the MIL technique (20).
When comparing the complication rates for open laminectomy and MIL techniques in the treatment of LSS, it's essential to consider that specific complications can vary depending on various factors such as patient characteristics, surgeon expertise, and the specific procedure performed. Some researchers suggested (7, 21, 22, 45, 58) that the postoperative complication rate is higher in the total laminectomy than the unilateral or bilateral laminectomy. Because of larger soft tissue disruption, the surgical site infection could be higher in open laminectomy (59). However, some studies did not find any significant difference between the two procedures when comparing the postoperative complication rate (27, 28).
Regarding comparing reoperation rates for open laminectomy vs. MIL techniques for LSS, it is important to note that specific rates can vary depending on the study, surgeon's experience, patient characteristics, and other factors. Unintentional durotomy, inadequate decompression, postoperative instability, scar tissue development, spinal instability, adjacent segment degeneration, and recurrent disc herniation are the primary sources for revision surgery. The majority of studies (6, 7, 10, 27, 53, 56) have indicated that MIL techniques result in lower postoperative complication rates, which in turn lead to reduced reoperation rates compared to traditional laminectomy. In contrast, only one clinical study (21) manifested that the MIL technique required more revision surgery than the conventional laminectomy due to inadequate decompression. Some studies (49, 52) did not find significant differences between these two procedures when compared to the reoperation rate for the LSS. Overall, the literature suggested that the reoperation rate for laminectomy ranged from 7% to 20%, while the reoperation rate for MIL techniques ranged from 2% to 10%.
In this review, only two papers reported the adjacent segment disease after open laminectomy or MIL procedure. Of them, only one patient experienced adjacent segment disease after an open laminectomy procedure. Older patients have been bringing osteophytes that reduce mobility; in these patients, stability may not be affected after MIL or open laminectomy procedure. Many papers (10, 47, 53) suggested that less bone disruption and less postoperative pain are more beneficial to the elderly population as it allows early mobilization. A small number of studies (22, 50) did not find significant difference between these procedures when comparing the young and elderly patients.
Patient satisfaction with the surgical treatment of LSS can depend on several factors, including the specific procedure performed, individual patient experiences, and expectations. Many articles (1, 6, 10) suggested that the VAS, ODI, and Japanese Orthopaedic Association (JOA) scores improved in the MIL group compared to open laminectomy. Some studies (16, 64, 65) have suggested that open laminectomy may be associated with a higher risk of the adjacent segment disease. The removal of the lamina alters the stability and load distribution of the spine, potentially leading to increased stress on the adjacent segments over time. This increased stress can contribute to the degeneration of the adjacent discs or the development of spinal instability.
Biomechanical studies showed that the von Mises stress on the upper adjacent level was relatively higher than the lower adjacent level. Furthermore, it has been clinically shown that the rostral side has higher ASD than the caudal side when patients were treated by laminectomy, MIL, or lumbar fusion procedure (64). In biomechanical studies (34, 38, 66), we observed that measuring the stress on the annulus fibrosus is of greater interest, as the stress changes in the nucleus are not significant. In the cadaveric study, one researcher (41) suggested that when the laminectomy involved only a single level, no instrumentation was required as the single-level laminectomy did not significantly affect the total spinal biomechanics column.
LSS is a complex condition that requires careful diagnosis and individualized treatment. With ongoing research and innovation in this field, we will likely continue to see improvements in diagnostic techniques, treatment options, and outcomes for patients with this condition. This study suggests that MIL may have a lower reoperation and complication rate than open or traditional laminectomy. As the MIL involves less bone disruption, this technique may be biomechanically more stable. Despite these challenges, advances in medical research have led to improved diagnostic and treatment options for LSS. In addition, studies have shown that exercise programs and other conservative measures can be effective in managing symptoms and improving the quality of life for patients with LSS. Minimally invasive spine surgeries have gained popularity in recent years due to their potential benefits, including smaller incisions, less tissue disruption, reduced postoperative pain, and quicker recovery times. These advantages often contribute to shorter hospital stays compared to traditional open procedures.
UD: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. EM: Data curation, Investigation, Resources, Writing – original draft, Writing – review & editing. ML: Writing – review & editing. TO’C: Writing – review & editing. NG: Writing – review & editing. ED: Writing – review & editing. IP: Writing – original draft, Writing – review & editing. KA: Writing – original draft, Writing – review & editing. C-TT: Conceptualization, Data curation, Funding acquisition, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FV: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
The authors declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Boca Raton Regional Hospital Foundation and the Helene and Stephen Weicholz Foundation (award # SP 19-579).
Thank individuals who contributed to the study or manuscript preparation but who did not fulfill all the criteria of authorship.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rosen DS, O’Toole JE, Eichholz KM, Hrubes M, Huo D, Sandhu FA, et al. Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery. (2007) 60:503–9. doi: 10.1227/01.NEU.0000255332.87909.58
2. Ishimoto Y, Yoshimura N, Muraki S, Yamada H, Nagata K, Hashizume H, et al. Associations between radiographic lumbar spinal stenosis and clinical symptoms in the general population: the Wakayama spine study. Osteoarthritis Cartilage. (2013) 21(6):783–8. doi: 10.1016/j.joca.2013.02.656
3. Liang H, Lu S, Jiang D, Fei Q. Clinical outcomes of lumbar spinal surgery in patients 80 years or older with lumbar stenosis or spondylolisthesis: a systematic review and meta-analysis. Eur Spine J. (2020) 29:2129–42. Springer Science and Business Media Deutschland GmbH. doi: 10.1007/s00586-019-06261-1
4. Patel P, Sohal A. Electrodiagnostic evaluation of spinal stenosis. In: StatPearls. Treasure Island, FL: StatPearls Publishing (2024). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK562227/
5. Kaptan H, Kasimcan O, Cakiroglu K, Ilhan MN, Kilic C. Lumbar spinal stenosis in elderly patients. Ann N Y Acad Sci. (2007) 1100:173–8. doi: 10.1196/annals.1395.015
6. Thomé C, Zevgaridis D, Leheta O, Bäzner H, Pöckler-Schöniger C, Wöhrle J, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. (2005) 3(2):129–41. doi: 10.3171/spi.2005.3.2.0129
7. Pietrantonio A, Trungu S, Famà I, Forcato S, Miscusi M, Raco A. Long-term clinical outcomes after bilateral laminotomy or total laminectomy for lumbar spinal stenosis: a single-institution experience. Neurosurg Focus. (2019) 46(5):E2. doi: 10.3171/2019.2.FOCUS18651
8. Awaya T, Nishimura Y, Eguchi K, Nagashima Y, Ando R, Akahori S, et al. Radiological analysis of minimally invasive microscopic laminectomy for lumbar canal stenosis with a focus on multilevel stenosis and spondylolisthesis. World Neurosurg. (2022) 164:e224–34. doi: 10.1016/j.wneu.2022.04.079
9. Javalkar V, Cardenas R, Tawfik TA, Khan IR, Bollam P, Banerjee AD, et al. Reoperations after surgery for lumbar spinal stenosis. World Neurosurg. (2011) 75:737–42. doi: 10.1016/j.wneu.2010.10.043
10. Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. (2014) 21(2):179–86. doi: 10.3171/2014.4.SPINE13420
11. Du WJ, Wang J, Wang Q, Yuan LJ, Lu ZX. Endoscopic modified total laminoplasty for symptomatic lumbar spinal stenosis. J Spinal Cord Med. (2022) 45(1):58–64. doi: 10.1080/10790268.2020.1762827
12. Suzuki A, Nakamura H. Microendoscopic lumbar posterior decompression surgery for lumbar spinal stenosis: literature review. Medicina (Kaunas). (2022) 58(3):384. doi: 10.3390/medicina58030384
13. Yang F, Wang Y, Ma Y, Hu X, Li X, Ma Z, et al. Single-segment central lumbar spinal stenosis: correlation with lumbar x-ray measurements. J Back Musculoskelet Rehabil. (2021) 34(4):581–7. doi: 10.3233/BMR-200051
14. Hermansen E, Austevoll IM, Hellum C, Storheim K, Myklebust TÅ, Aaen J, et al. Comparison of 3 different minimally invasive surgical techniques for lumbar spinal stenosis: a randomized clinical trial. JAMA Netw Open. (2022) 5(3):e224291. doi: 10.1001/jamanetworkopen.2022.4291
15. Minetama M, Kawakami M, Teraguchi M, Kagotani R, Mera Y, Sumiya T, et al. Supervised physical therapy vs. home exercise for patients with lumbar spinal stenosis: a randomized controlled trial. Spine J. (2019) 19(8):1310–8. doi: 10.1016/j.spinee.2019.04.009
16. Yolcu YU, Helal A, Alexander AY, Bhatti AU, Alvi MA, Abode-Iyamah K, et al. Minimally invasive versus open surgery for degenerative spine disorders for elderly patients: experiences from a single institution. World Neurosurg. (2021) 146:e1262–9. doi: 10.1016/j.wneu.2020.11.145
17. Lak AM, Abunimer AM, Rahimi A, Tafel I, Chi J, Lu Y, et al. Outcomes of minimally invasive versus open surgery for intermediate to high-grade spondylolisthesis: a 10-year retrospective, multicenter experience. Spine (Phila Pa 1976). (2020) 45(20):1451–8. doi: 10.1097/BRS.0000000000003573
18. Ivanov A, Faizan A, Sairyo K, Ebraheim N, Biyani A, Goel VK. Minimally invasive decompression for lumbar spinal canal stenosis in younger age patients could lead to higher stresses in the remaining neural arch—a finite element investigation. Minim Invasive Neurosurg. (2007) 50(1):18–22. doi: 10.1055/s-2006-947996
19. Chou D, Mummaneni P, Anand N, Nunley P, La Marca F, Fu KM, et al. Treatment of the fractional curve of adult scoliosis with circumferential minimally invasive surgery versus traditional, open surgery: an analysis of surgical outcomes. Global Spine J. (2018) 8(8):827–33. doi: 10.1177/2192568218775069
20. Lundberg J, Langevin JP. Lumbar microlaminectomy vs traditional laminectomy. Fed Pract. (2017) 34(12):32–5.30766247
21. Ang CL, Phak-Boon Tow B, Fook S, Guo CM, Chen JLT, Yue WM, et al. Minimally invasive compared with open lumbar laminotomy: no functional benefits at 6 or 24 months after surgery. Spine J. (2015) 15(8):1705–12. doi: 10.1016/j.spinee.2013.07.461
22. Nerland US, Jakola AS, Solheim O, Weber C, Rao V, Lønne G, et al. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ. (2015) 350:h1603. doi: 10.1136/bmj.h1603
23. Vergara P, Akhunbay-Fudge CY, Kotter MR, Charles Laing RJ. Minimally invasive versus open surgery for lumbar synovial cysts. World Neurosurg. (2017) 108:555–9. doi: 10.1016/j.wneu.2017.09.039
24. Wong AP, Lall RR, Dahdaleh NS, Lawton CD, Smith ZA, Wong RH, et al. Comparison of open and minimally invasive surgery for intradural-extramedullary spine tumors. Neurosurg Focus. (2015) 39(2):E11. doi: 10.3171/2015.5.FOCUS15129
25. McClelland S, Goldstein JA. Minimally invasive versus open spine surgery: what does the best evidence tell us? J Neurosci Rural Pract. (2017) 8(2):194–8. doi: 10.4103/jnrp.jnrp_472_16
26. Parker SL, Fulchiero EC, Davis BJ, Adogwa O, Aaronson OS, Cheng JS, et al. Cost-effectiveness of multilevel hemilaminectomy for lumbar stenosis-associated radiculopathy. Spine J. (2011) 11(8):705–11. doi: 10.1016/j.spinee.2011.04.024
27. Horan J, Husien MB, Bolger C. Bilateral laminotomy through a unilateral approach (minimally invasive) versus open laminectomy for lumbar spinal stenosis. Br J Neurosurg. (2021) 35(2):161–5. doi: 10.1080/02688697.2020.1777253
28. Shih P, Wong AP, Smith TR, Lee AI, Fessler RG. Complications of open compared to minimally invasive lumbar spine decompression. J Clin Neurosci. (2011) 18(10):1360–4. doi: 10.1016/j.jocn.2011.02.022
29. Rajasekaran S, Thomas A, Kanna RM, Prasad Shetty A. Lumbar spinous process splitting decompression provides equivalent outcomes to conventional midline decompression in degenerative lumbar canal stenosis: a prospective, randomized controlled study of 51 patients. Spine (Phila Pa 1976). (2013) 38(20):1737–43. doi: 10.1097/BRS.0b013e3182a056c1
30. Rahman M, Summers LE, Richter B, Mimran RI, Jacob RP. Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the “classic” open approach. Minim Invasive Neurosurg. (2008) 51(2):100–5. doi: 10.1055/s-2007-1022542
31. Lee KK, Teo EC. Effects of laminectomy and facetectomy on the stability of the lumbar motion segment. Med Eng Phys. (2004) 26(3):183–92. doi: 10.1016/j.medengphy.2003.11.006
32. Nong L, Zhou D, Xu N, Du R, Jiang X. Lamina replacement with titanium plate fixation improves spinal stability after total lumbar laminectomy. Comput Methods Biomech Biomed Engin. (2015) 18(16):1753–9. doi: 10.1080/10255842.2014.953491
33. Ahuja S, Moideen AN, Dudhniwala AG, Karatsis E, Papadakis L, Varitis E. Lumbar stability following graded unilateral and bilateral facetectomy: a finite element model study. Clin Biomech (Bristol, Avon). (2020) 75:105011. doi: 10.1016/j.clinbiomech.2020.105011
34. Subramaniam V, Chamberlain RH, Theodore N, Baek S, Safavi-Abbasi S, Senoğlu M, et al. Biomechanical effects of laminoplasty versus laminectomy. Spine (Phila Pa 1976). (2009) 34(16):E573–8. doi: 10.1097/BRS.0b013e3181aa0214
35. Bisson EF, Mummaneni P V, Virk MS, Knightly J, Ali Alvi M, Goyal A, et al. Open versus minimally invasive decompression for low-grade spondylolisthesis: analysis from the Quality Outcomes Database. J Neurosurg Spine. (2020) 33(3):349–59. doi: 10.3171/2020.3.SPINE191239
36. Matsumoto K, Shah A, Kelkar A, Parajuli D, Sudershan S, Goel VK, et al. Biomechanical evaluation of a novel decompression surgery: transforaminal full-endoscopic lateral recess decompression (TE-LRD). N Am Spine Soc J. (2020) 5:100045. doi: 10.1016/j.xnsj.2020.100045
37. Bisschop A, Van Dieën JH, Kingma I, Van Der Veen AJ, Jiya TU, Mullender MG, et al. Torsion biomechanics of the spine following lumbar laminectomy: a human cadaver study. Eur Spine J. (2013) 22(8):1785–93. doi: 10.1007/s00586-013-2699-3
38. Bisschop A, Van Engelen SJPM, Kingma I, Holewijn RM, Stadhouder A, Van Der Veen AJ, et al. Single level lumbar laminectomy alters segmental biomechanical behavior without affecting adjacent segments. Clin Biomech. (2014) 29(8):912–7. doi: 10.1016/j.clinbiomech.2014.06.016
39. Spina NT, Moreno GS, Brodke DS, Finley SM, Ellis BJ. Biomechanical effects of laminectomies in the human lumbar spine: a finite element study. Spine J. (2021) 21(1):150–9. doi: 10.1016/j.spinee.2020.07.016
40. Gong X, Zhang A, Han Q, Wang Y, Liu Y, Jiao J, et al. Biomechanical effects of individualized artificial titanium alloy lamina implantation after laminectomy: a finite element analysis. Front Bioeng Biotechnol. (2022) 10:1019510. doi: 10.3389/fbioe.2022.1019510
41. Lee MJ, Bransford RJ, Bellabarba C, Chapman JR, Cohen AM, Harrington RM, et al. The effect of bilateral laminotomy versus laminectomy on the motion and stiffness of the human lumbar spine: a biomechanical comparison. Spine (Phila Pa 1976). (2010) 35(19):1789–93. doi: 10.1097/BRS.0b013e3181c9b8d6
42. Lin M, Paul R, Dhar UK, Doulgeris J, O'Connor TE, Tsai CT, et al. A review of finite element modeling for anterior cervical discectomy and fusion. Asian Spine J. (2023) 17(5):949–63. doi: 10.31616/asj.2022.0295
43. Dhar UK, Menzer EL, Lin M, Hagerty V, O’Connor T, Tsai CT, et al. Factors influencing cage subsidence in anterior cervical corpectomy and discectomy: a systematic review. Eur Spine J. (2023) 32:957–68. Springer Science and Business Media Deutschland GmbH. doi: 10.1007/s00586-023-07530-w
44. Moher D, Liberati A, Tetzlaff J, Altman DG, Antes G, Atkins D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. Public Library of Science. doi: 10.1371/journal.pmed.1000097
45. Kanbara S, Yukawa Y, Ito K, Machino M, Kato F. Surgical outcomes of modified lumbar spinous process-splitting laminectomy for lumbar spinal stenosis. J Neurosurg Spine. (2015) 22(4):353–7. doi: 10.3171/2014.9.SPINE1457
46. Cho DY, Lin HL, Lee WY, Lee HC. Split-spinous process laminotomy and discectomy for degenerative lumbar spinal stenosis: a preliminary report. J Neurosurg Spine. (2007) 6(3):229–39. doi: 10.3171/spi.2007.6.3.229
47. Khoo LT, Fessler RG. Microendoscopic decompressive laminotomy for the treatment of lumbar stenosis. Neurosurgery. (2002) 51(5 Suppl):S146–54.12234442
48. Ikuta K, Arima J, Tanaka T, Oga M, Nakano S, Sasaki K, et al. Short-term results of microendoscopic posterior decompression for lumbar spinal stenosis. Technical note. J Neurosurg Spine. (2005) 2(5):624–33. doi: 10.3171/spi.2005.2.5.0624
49. Liu X, Yuan S, Tian Y. Modified unilateral laminotomy for bilateral decompression for lumbar spinal stenosis: technical note. Spine (Phila Pa 1976). (2013) 38(12):E732–7. doi: 10.1097/BRS.0b013e31828fc84c
50. Morgalla MH, Noak N, Merkle M, Tatagiba MS. Lumbar spinal stenosis in elderly patients: Is a unilateral microsurgical approach sufficient for decompression? Clinical article. J Neurosurg Spine. (2011) 14(3):305–12. doi: 10.3171/2010.10.SPINE09708
51. Aleem IS, Rampersaud YR. Elderly patients have similar outcomes compared to younger patients after minimally invasive surgery for spinal stenosis. Clin Orthop Relat Res. (2014) 472(6):1824–30. doi: 10.1007/s11999-013-3411-y
52. Ovalioglu TC, Ozdemir Ovalioglu A, Canaz G, Gunes M, Babur M, Emel E. Efficacy of spinous process splitting decompression compared with conventional laminectomy for degenerative lumbar stenosis. World Neurosurg. (2022) 164:e1233–42. doi: 10.1016/j.wneu.2022.06.015
53. Celik SE, Celik S, Göksu K, Kara A, Ince I. Microdecompressive laminatomy with a 5-year follow-up period for severe lumbar spinal stenosis. J Spinal Disord Tech. (2010) 23(4):229–35. doi: 10.1097/BSD.0b013e3181a3d889
54. Watanabe K, Matsumoto M, Ikegami T, Nishiwaki Y, Tsuji T, Ishii K, et al. Reduced postoperative wound pain after lumbar spinous process-splitting laminectomy for lumbar canal stenosis: a randomized controlled study. Clinical article. J Neurosurg Spine. (2011) 14(1):51–8. doi: 10.3171/2010.9.SPINE09933
55. Harrington JF, French P. Open versus minimally invasive lumbar microdiscectomy: comparison of operative times, length of hospital stay, narcotic use and complications. Minim Invasive Neurosurg. (2008) 51(1):30–5. doi: 10.1055/s-2007-1004543
56. Fu YS, Zeng BF, Xu JG. Long-term outcomes of two different decompressive techniques for lumbar spinal stenosis. Spine (Phila Pa 1976). (2008) 33(5):514–8. doi: 10.1097/BRS.0b013e3181657dde
57. Yagi M, Okada E, Ninomiya K, Kihara M. Postoperative outcome after modified unilateral-approach microendoscopic midline decompression for degenerative spinal stenosis: clinical article. J Neurosurg Spine. (2009) 10(4):293–9. doi: 10.3171/2009.1.SPINE08288
58. Ercegovic Z, Moranjkic M, Korkut D. Spinal instability following surgery for degenerative lumbar stenosis. Acta Medica Saliniana. (2012) 41(1):22–8. doi: 10.5457/ams.v41i1.261
59. Oichi T, Oshima Y, Chikuda H, Ohya J, Matsui H, Fushimi K, et al. In-hospital complication rate following microendoscopic versus open lumbar laminectomy: a propensity score-matched analysis. Spine J. (2018) 18(10):1815–21. doi: 10.1016/j.spinee.2018.03.010
60. Cyron BM, Hutfon WC. The fatigue strength of the lumbar neural arch in spondylolysis. J Bone Joint Surg Br. (1978) 60-B(2):234–8. doi: 10.1302/0301-620X.60B2.659472
61. Bresnahan L, Ogden AT, Natarajan RN, Fessler RG. A biomechanical evaluation of graded posterior element removal for treatment of lumbar stenosis: comparison of a minimally invasive approach with two standard laminectomy techniques. Spine (Phila Pa 1976). (2009) 34(1):17–23. doi: 10.1097/BRS.0b013e318191438b
62. Bisschop A, van Royen BJ, Mullender MG, Paul CPL, Kingma I, Jiya TU, et al. Which factors prognosticate spinal instability following lumbar laminectomy? Eur Spine J. (2012) 21(12):2640–8. doi: 10.1007/s00586-012-2250-y
63. Lin M, Doulgeris J, Dhar UK, O'Corner T, Papanastassiou ID, Tsai CT, et al. Effect of graded posterior element and ligament removal on annulus stress and segmental stability in lumbar spine stenosis: a finite element analysis study. Front Bioeng Biotechnol. (2023) 11:1237702. doi: 10.3389/fbioe.2023.1237702
64. Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am. (2019) 30:299–304. W.B. Saunders. doi: 10.1016/j.nec.2019.02.003
65. Zhong J, O’Connell B, Balouch E, Stickley C, Leon C, O’Malley N, et al. Patient outcomes after single-level coflex interspinous implants versus single-level laminectomy. Spine (Phila Pa 1976). (2021) 46(13):893–900. doi: 10.1097/BRS.0000000000003924
Keywords: laminectomy, minimum invasive surgery, lumbar spinal stenosis, finite element analysis, human lumbar spine
Citation: Dhar UK, Menzer EL, Lin M, O’Connor T, Ghimire N, Dakwar E, Papanastassiou ID, Aghayev K, Tsai C-T and Vrionis FD (2024) Open laminectomy vs. minimally invasive laminectomy for lumbar spinal stenosis: a review. Front. Surg. 11:1357897. doi: 10.3389/fsurg.2024.1357897
Received: 18 December 2023; Accepted: 7 October 2024;
Published: 7 November 2024.
Edited by:
Alessandro Frati, Sapienza University of Rome, ItalyReviewed by:
Mauro Dobran, Marche Polytechnic University, ItalyCopyright: © 2024 Dhar, Menzer, Lin, O'Connor, Ghimire, Dakwar, Papanastassiou, Aghayev, Tsai and Vrionis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frank D. Vrionis, ZnZyaW9uaXNAYmFwdGlzdGhlYWx0aC5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.