
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 04 March 2024
Sec. Neurosurgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1350032
 Guive Sharifi1,2
Guive Sharifi1,2 Esmaeil Mohammadi3*
Esmaeil Mohammadi3* Elham Paraandavaji2
Elham Paraandavaji2 Seyed Mohammad Tavangar4,5
Seyed Mohammad Tavangar4,5 Mohammad Amin Dabbagh Ohadi2
Mohammad Amin Dabbagh Ohadi2 Ali Jafari1,2
Ali Jafari1,2 Amin Jahanbakhshi2
Amin Jahanbakhshi2 Nader Akbari Dilmaghani2
Nader Akbari Dilmaghani2 Zahra Davoudi2
Zahra Davoudi2 Timothy R. Smith6
Timothy R. Smith6 Gelareh Banihashemi7
Gelareh Banihashemi7 Masoumeh Azadi8
Masoumeh Azadi8 Neda Hatami8
Neda Hatami8 Georgios A. Zenonos9
Georgios A. Zenonos9 Mohammadreza Mohajeri Tehrani10
Mohammadreza Mohajeri Tehrani10
Purpose: We aimed to investigate empty sella syndrome in somatotrophic pituitary adenoma for possible etiology, complications, and treatment options.
Method: Among over 2,000 skull base masses that have been managed in our center since 2013, we searched for growth hormone-producing adenomas. Clinical, surgical, and imaging data were retrospectively collected from hospital records to check for sella that lacked pituitary tissue on routine imaging.
Result: In 220 somatotrophic adenomas, 23 patients had an empty sella with surgical and follow-up data. The mean age of the sample was 46 years with the same male-to-female ratio. Five cases had partial empty sella and the rest were complete empty sellas. The most common simultaneous hormonal disturbance was high prolactin levels. Six had adenoma invasion into the clivus or sphenoid sinus and 10 had cavernous sinus intrusion. Peri-operative low-flow and high-flow cerebrospinal fluid (CSF) leaks were encountered in one and two patients, respectively, which were successfully sealed by abdominal fat. The majority of cases required growth hormone replacement therapy while it was controlled without any replacement therapy in nine patients. No pituitary hormonal disturbance occurred after transsphenoidal surgery except for hypothyroidism in one patient.
Conclusion: An empty sella filled with fluid can be detected frequently in pituitary adenomas, especially in the setting of acromegaly. The pituitary gland may be pushed to the roof of the sella and might be visible as a narrow rim on imaging or may be detected in unusual places out of the sella. The pathophysiology behind such finding originates from soft and hard tissue changes and CSF pressure alternations during abundant growth hormone production.
Empty sella syndrome (ESS) is a neuro-radiological phenomenon defined by enlarged sella turcica filled with CSF and a flattened or pressed-aside pituitary (Figure 1) (1). Previous related radiotherapy, surgery, or trauma could lead to ESS with ascertained cause, better recognized as secondary empty sella. The primary or idiopathic form is rare and corroborated for those with no definitive reason (2, 3). An incompetent diaphragm, increased intracranial pressure, and pregnancy-associated changes in pituitary gland volume are among the proposed relatable factors.
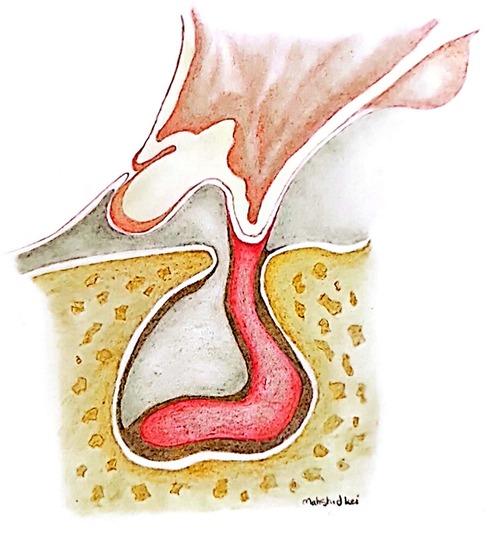
Figure 1. Anatomical illustration of the pushed-aside pituitary tissue by the arachnoid cyst in the context of empty sella.
Empty sella has been detected in ACTH and GH-secreting adenomas (2). Previous reports suggest higher rates of peri-operative cerebrospinal fluid (CSF) leakage and hormonal dysfunction in corticotropic adenomas and empty sella (4). Additionally, controversy exists around the role of transsphenoidal resection in acromegaly patients with coexisting empty sella (5).
Concomitance of empty sella and somatotrophic adenoma has been reported in prior small series and case reports while hormonal outcomes and long-term complications after surgery remain unclear. In this study, we report our experience with transsphenoidal surgery of GH-producing adenomas in a series of patients with coexisting empty sella and report procedural hardships and drawbacks.
For this case series, we followed the PROCESS guideline (6) and retrospectively searched for empty sella cases in our database of more than 2,000 adenomas who underwent surgical resection between 2013 and 2020. All cases were operated on in a single tertiary academic center by the same surgery team. Prior to the surgery, patients were evaluated by an expert team including a neurologist who examined the patients, an endocrinologist who made the diagnosis of central acromegaly by established criteria (7), and a radiologist who evaluated the pituitary dynamic magnetic resonance imaging (MRI). Patients who had a previous history of interventional treatment (surgery or radiation therapy), known neurological disease, or GH/IGF1 (insulin-like growth factor) secreting ectopic tumors were excluded [using chest computed tomography (CT) scan]. We collected our data through hospital documents and follow-up of outpatient records. Further information was gathered via phone calls with the patients. All patients were followed up through routine clinic visits and perpetual imaging at the first month, sixth month, and then annual evaluations. Every enrolled participant was followed up for at least 3 years, post-operatively. Any record with a lack of surgical or medical data was excluded. No age or sex limit was placed in this work. The study design and conduct were in accordance with the Declaration of Helsinki (8) and our Institutional Review Board (IRB). The research was conducted using de-identified data following the acquisition of informed consent.
Dynamic pituitary gland study MR images on a 1.5 T scanner with a standard head coil, along with axial and coronal non-contrast head CT scans were obtained preoperatively for all patients. Emptiness of sella was decided on midsagittal T1-weighted MR imaging (2). This was approved by an expert radiologist. Total empty sella was defined as a pituitary gland with less than 2.0-mm height or fluid filling of more than 50% of turcica's space, and partially empty sella was defined as a pituitary gland with a height greater than 2.1-mm or fluid filling between 50% and 33% of sellar space or its depth (9). The maximum tumor size (diameter) was measured on the coronal plane using a T1-weighted post-enhanced image. Tumors with a maximum diameter greater than 10 mm were categorized as macroadenomas (maximize area >100 mm2). Suprasellar extension of tumors was defined as growth toward the diaphragm sella or above the inferior optic chiasm plane. Extension to the left or right from the midline was also examined as a lateral extension of the tumoral tissue. Bony invasion was defined as a tumor growth in the sphenoid sinus documented with MRI or during the surgery.
All patients underwent endonasal transsphenoidal surgery (TSS) for adenoma resection. All operations were performed by the lead surgeon (G.Sh) and the same team. Every specimen was sent to a pathologist for confirmation of GH-producing adenoma using immunohistochemistry. After tumor removal, due to the tendency of such adenomas to grow in extra-sellar locations, we thoroughly investigated different aspects and angles of sella to make sure no remnant was left. CSF leakage was classified as no observable leak, little amount of CSF leaks as a result of transient increase in intracranial pressure which is termed as a “low-flow” CSF leak, and “high-flow” continuous CSF leak observed intraoperatively in the setting of openings in the ventricular system or connections with cisterns (10, 11). In case of CSF leakage, abdominal fat and/or fascia were used as packing material for reconstruction.
Basal fasting GH, IGF1, and 75-gram oral glucose tolerance were assessed for patients before and after surgery. Other hormonal conditions were also recorded before surgery and followed up accordingly. Unfortunately, as the 75-gram oral glucose tolerance testing was not recorded for every patient, we excluded it from this report. We also reported coexisting hormonal problems.
We found 31 somatotrophic adenomas with empty sella among 220 acromegaly patients who underwent transsphenoidal endoscopic surgery in our center. Eight records were excluded because of missing surgical characteristics. As a result, 23 patients were included. The mean age of the sample was 46 years and women accounted for 11/23 of the sample. The most prominent manifestation was an increase in the size of the hands, feet, and face in 19/23 patients. Other complaints were an increase in weight (more than 10 kg) in seven, headaches in six, and visual problems in five patients. One of the patients used octreotide and cabergoline, one used only octreotide, and another patient used levothyroxine before the surgery for less than 3 months.
Preoperative MRI revealed 5/23 patients with partial empty sella and the rest with total empty sella (Figures 2, 3). Macroadenoma was discovered in 12 patients. The mean adenoma area was measured at 1.6 cm2. The pituitary gland was superiorly dislocated and visible as a rim of soft tissue in patients with total empty sella. The tumor was found to have an extension to suprasellar and parasellar regions in two and eight patients, respectively. Tumor invasion to the sphenoid sinus or clivus occurred in six patients. There was no evidence of apoplexy in any of the patients. During the surgery, low-flow and high-flow leaks were encountered in one and two patients, respectively, which were uneventfully sealed by abdominal fat. None of the patients reported postsurgical rhinorrhea or other signs of CSF leak during the follow-up. The CSF leakage rate was twice as high in this sample compared to the total case mix (4.7%). Further details are provided in Table 1.
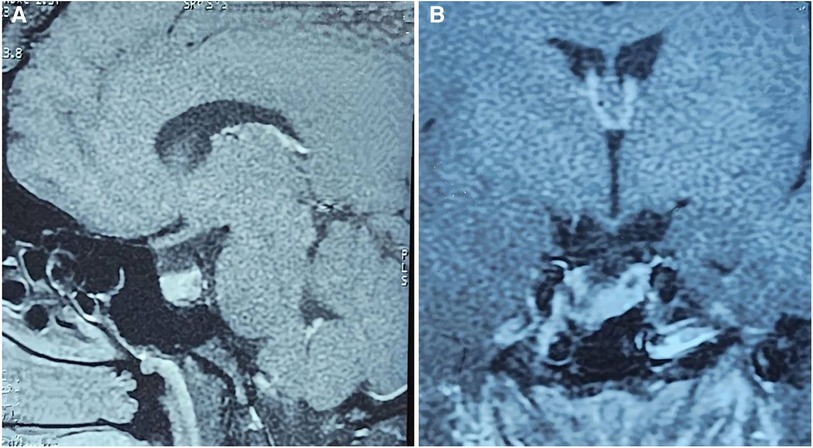
Figure 2. Sagittal (A) and coronal (B) views of dynamic MRI of the sellar region in patients with empty sella.
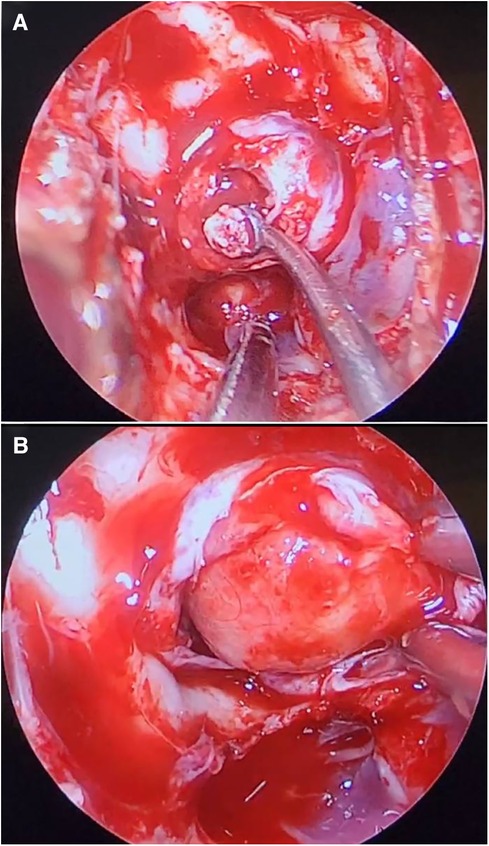
Figure 3. Endoscopic transnasal transsphenoidal surgery removal of a growth hormone-producing adenoma (A). Arachnoid extrusion is visible upon removal of sphenoid bone (B).
Pre-operative high prolactin levels were found in 4/23 patients as the most common simultaneous hormonal imbalance. Post-operative transient diabetes mellitus was found only in 1/23 patients which resolved over the follow-up period. Endocrinology results were available for 17 cases. At the last follow-up, normal GH and IGF1 were recorded in 9/17 patients without any medication. In addition, hormonal levels were controlled in 5/17 patients with medication after surgery, and 3/17 patients still had high levels of GH/IGF1. None of the patients reported any continuing or emergent symptoms after surgery except patient #9 who became hypothyroid. More details are provided in Table 2.
Here we stated our experience of pituitary surgery of somatotrophic adenomas with concomitant empty sella syndrome. Approximately 14% of GH-producing adenomas were detected to present with a sella filled with fluid. This entity has been observed in a wide range from 15% to much higher rates, as Bjerr et al. (12) encountered empty sella in half of their acromegaly patients. Some believe empty sella is an incidental finding in acromegaly adenoma situation (5) while others justify this coexistence. Liu et al. proposed empty sella coexistence with acromegaly relatable to the paracrine effects of GH (2). In other words, due to the anabolic effects of GH on soft and hard tissues, it has been stipulated that the sellar anatomy of acromegaly cases might be larger. Similarly, it is shown that in such instances the diaphragm of sella is firmer and less compliant, making pituitary tissue and adenomas more susceptible to growing to the extra-sellar areas. Empty sella is a known sequel to idiopathic intracranial hypertension (IIH), which is more prevalent in women (7). On the other hand, GH is a predisposing element for IIH likely due to association with higher levels of α-Klotho, an important protein in CSF homeostasis (2, 13). However, mechanistic studies are required to evaluate this association. Adenoma infraction and hemorrhage are among other implausible reasons for ESS, but they were not observed in any of the enrolled participants.
High levels of prolactin were the most common coexisting hormonal problem followed by abnormal levels of TSH. Additionally, for ESS differential diagnosis, ectopic GH/IGF1 secreting adenoma in the bronchus and sphenoid sinus should be excluded (14, 15).
Despite inconsistencies in surgical outcomes, TSS remains the gold standard treatment for adenomas with coexisting empty sella although a great deal of attention should be paid to explore sella's roof as well as higher extra-sellar regions (5). High levels of prolactin were the most common coexisting hormonal problem followed by abnormal levels of TSH. GH/IGF1 levels were controlled without any medications in 53% of the cases with other hormones adjusting with it. This was similar to previous studies, interpretable as half of the cases will be curable with no need for hormonal regimens (2, 5). However, cases with empty sella may require hormonal therapies to a higher extent than regular adenomas that could maintain the hormonal needs with no further assistance (50%–70%) (16, 17). Anterior pituitary malfunction and diabetes insipidus after surgery were seen in a previous study by Wang et al. in 18% and 37% of cases, respectively. Nevertheless, this complication occurred only in one of our patients. Few studies have mentioned risk factors for poor surgical outcomes (5, 18). Complete emptiness of sella has been referred to as a major risk factor for a poorer cure rate (5, 18). Higher GH levels and larger adenomas are other suggested risk factors for poor outcomes (18, 19). CSF leakage was the most frequent complication of surgery in our sample. CSF leakage is a common complication after TSS which could potentially lead to infection and neurologic complications (20, 21). CSF leakage in empty sella entity was twice higher compared to our total case mix, possibly due to higher intracranial pressure. Similar findings in acromegaly patients with empty sella have been found in prior works (5). Wang et al. showed this complication to be related to larger tumors accompanying empty sella (18). However, in certain cases with high suspicion of tumor remnant, it might be decided to open the occupying arachnoid cyst in order to ease access to different aspects of the sellar region. However, the use of fat tissue extracted from the abdomen for the reconstruction of defects and leaks in our sample has been found to be effective and is the readily available method (22).
Despite the efforts to collect comprehensive information, our study was limited by missing data. Mechanistic investigations are needed to clarify the exact pathophysiology behind the tendency of arachnoid cysts and empty sella with various adenoma subtypes.
In conclusion, sella occupied with arachnoid is a coexisting feature of a considerable number of somatotropic pituitary adenomas, a higher rate than what is previously stipulated, which could push aside the pituitary tissue to the margins of sella or upper locations. Although the exact etiology of this entity remains unclear, coexisting idiopathic intracranial hypertension as well as anatomical changes due to growth hormone overexpression and diaphragm incompliance could lead to displaced adenoma. Appropriate preoperative imaging and thorough evaluation of the sella region are advised in suspected cases. Transsphenoidal surgery provides satisfactory results and infrequent complications with a comparable number of regular adenomas without empty sella. The most frequently encountered complicating event is cerebrospinal fluid leakage which could be managed at the same success rate as other skull-based surgeries.
The deidentified data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by institutional review board of Tehran University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
GS: Investigation, Writing – original draft, Writing – review & editing, Conceptualization. EM: Investigation, Writing – original draft, Writing – review & editing, Methodology, Supervision. EP: Investigation, Writing – review & editing. NA: Writing – review & editing. ST: Writing – review & editing. AO: Formal Analysis, Writing – original draft, Writing – review & editing. AJ: Conceptualization, Writing – review & editing. AJ: Conceptualization, Writing – review & editing. ZD: Conceptualization, Investigation, Writing – review & editing. MM: Writing – review & editing. GB: Writing – review & editing. MA: Data curation, Writing – review editing. NH: Data curation, Writing – reveiew editing. GZ: Writing – review & editing. TS: Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to acknowledge the hard work of Mahshid Kamangari for the preparation of the artistic illustration.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. De Marinis L, Bonadonna S, Bianchi A, Maira G, Giustina A. Primary empty sella. J Clin Endocrinol Metab. (2005) 90(9):5471–7. doi: 10.1210/jc.2005-0288
2. Liu W, Zhou H, Neidert MC, Schmid C, Bernays RL, Ni M, et al. Growth hormone secreting pituitary microadenomas and empty sella - an under-recognized association? Clin Neurol Neurosurg. (2014) 126:18–23. doi: 10.1016/j.clineuro.2014.08.012
3. Möller-Goede DL, Brändle M, Landau K, Bernays RL, Schmid C. Pituitary apoplexy: re-evaluation of risk factors for bleeding into pituitary adenomas and impact on outcome. Eur J Endocrinol. (2011) 164(1):37–43. doi: 10.1530/eje-10-0651
4. Manavela MP, Goodall CM, Katz SB, Moncet D, Bruno OD. The association of Cushing’s disease and primary empty sella turcica. Pituitary. (2001) 4(3):145–51. doi: 10.1023/a:1015310806063
5. Sasagawa Y, Hayashi Y, Tachibana O, Oishi M, Fukui I, Iizuka H, et al. Clinical characteristics of acromegalic patients with empty sella and their outcomes following transsphenoidal surgery. Pituitary. (2017) 20(4):403–8. doi: 10.1007/s11102-017-0798-6
6. Agha RA, Sohrabi C, Mathew G, Franchi T, Kerwan A, O’Neill N, et al. The PROCESS 2020 guideline: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int Surg J. (2020) 84:231–5. doi: 10.1016/j.ijsu.2020.11.005
7. Giustina A, Barkan A, Casanueva FF, Cavagnini F, Frohman L, Ho K, et al. Criteria for cure of acromegaly: a consensus statement. J Clin Endocrinol Metab. (2000) 85(2):526–9. doi: 10.1210/jcem.85.2.6363
8. Association WM. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310(20):2191–4. doi: 10.1001/jama.2013.281053
9. Mehta GU, Bakhtian KD, Oldfield EH. Effect of primary empty sella syndrome on pituitary surgery for Cushing’s disease. J Neurosurg. (2014) 121(3):518–26. doi: 10.3171/2014.3.jns132012
10. Zhan R, Chen S, Xu S, Liu JK, Li X. Postoperative low-flow cerebrospinal fluid leak of endoscopic endonasal transsphenoidal surgery for pituitary adenoma–wait and see, or lumbar drain? J Craniofac Surg. (2015) 26(4):1261–4. doi: 10.1097/scs.0000000000001691
11. Luginbuhl AJ, Campbell PG, Evans J, Rosen M. Endoscopic repair of high-flow cranial base defects using a bilayer button. Laryngoscope. (2010) 120(5):876–80. doi: 10.1002/lary.20861
12. Bjerre PER, Lindholm J, Videbæk H. The spontaneous course of pituitary adenomas and occurrence of an empty sella in untreated acromegaly*. J Clin Endocrinol Metab. (1986) 63(2):287–91. doi: 10.1210/jcem-63-2-287
13. Neidert MC, Sze L, Zwimpfer C, Sarnthein J, Seifert B, Frei K, et al. Soluble α-Klotho: a novel serum biomarker for the activity of GH-producing pituitary adenomas. Eur J Endocrinol. (2013) 168(4):575–83. doi: 10.1530/eje-12-1045
14. Hong JF, Ding XH, Wang SS. Coexistence of ectopic pituitary adenoma and empty sella in a patient with acromegaly: a case report and review of literature. Neurol India. (2012) 60(3):304–6. doi: 10.4103/0028-3886.98517
15. Osella G, Orlandi F, Caraci P, et al. Acromegaly due to ectopic secretion of GHRH by bronchial carcinoid in a patient with empty sella. J Endocrinol Investig. (2003) 26(2):163–9. doi: 10.1007/BF03345146
16. Marquez Y, Tuchman A, Zada G. Surgery and radiosurgery for acromegaly: a review of indications, operative techniques, outcomes, and complications. Int J Endocrinol. (2012) 2012:386401. doi: 10.1155/2012/386401
17. Rotermund R, Mader MM, Burkhardt T, Matschke J, Aberle J, Krajewski K, et al. Real-life analysis of 280 patients with surgically treated acromegaly: a single-center experience from 2008 to 2015. Neurosurgical Focus FOC. (2020) 48(6):E9. doi: 10.3171/2020.3.focus2061
18. Wang Q, Guo X, Gao L, Wang Z, Deng K, Lian W, et al. Surgical outcome of growth hormone-secreting pituitary adenoma with empty sella using a new classification. World Neurosurg. (2017) 105:651–8. doi: 10.1016/j.wneu.2017.06.071
19. Oldfield EH, Jane JA Jr, Thorner MO, Pledger CL, Sheehan JP, Vance ML. Correlation between GH and IGF−1 during treatment for acromegaly. J Neurosurg. (2017) 126(6):1959–66. doi: 10.3171/2016.8.jns161123
20. Sharifi G, Mohammadi E, Jafari A, Jamali E, Sabouri S, Akbari N. A case of Meckel’s cave epidermoid cyst with unilateral abducens nerve paresis as the sole presentation. Interdiscip Neurosurg. (2022) 30:101613. doi: 10.1016/j.inat.2022.101613
21. Sharifi G, Mohammadi E, Jafari A, Akbari N, Sabouri S. A rare case of pituitary TSH secreting microadenoma (TSHoma) complicated with sellar primitive persistent trigeminal artery; an operative implication and radiologic emphasis. Interdiscip Neurosurg. (2021) 26:101326. doi: 10.1016/j.inat.2021.101326
Keywords: empty sella, acromegaly, adenoma, surgery, endoscopic surgery
Citation: Sharifi G, Mohammadi E, Paraandavaji E, Tavangar SM, Dabbagh Ohadi MA, Jafari A, Jahanbakhshi A, Akbari Dilmaghani N, Davoudi Z, Smith TR, Banihashemi G, Azadi M, Hatami N, Zenonos GA and Mohajeri Tehrani M (2024) Empty sella in somatotropic pituitary adenomas; a series of 23 cases. Front. Surg. 11:1350032. doi: 10.3389/fsurg.2024.1350032
Received: 5 December 2023; Accepted: 8 February 2024;
Published: 4 March 2024.
Edited by:
Mario Ganau, Oxford University Hospitals NHS Trust, United KingdomReviewed by:
Guilherme Finger, The Ohio State University, United States© 2024 Sharifi, Mohammadi, Paraandavaji, Tavangar, Dabbagh Ohadi, Jafari, Jahanbakhshi, Akbari Dilmaghani, Davoudi, Smith, Banihashemi, Azadi, Hatami, Zenonos, and Mohajeri Tehrani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Esmaeil Mohammadi ZXNtYWVpbG11aGFtbWFkaUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.