- 1Department of Orthopedics, Shanghai Pudong Hospital, Fudan University Pudong Medical Center, Shanghai, China
- 2Department of Orthopedics, Seventh People's Hospital of Shanghai, Shanghai, China
Objective: This study aims to analyze the biomechanical characteristics of posterolateral plateau fractures fixed by a novel anatomical plate using finite element analysis.
Methods: A three-dimensional digital model of the full length of right tibiofibula was obtained by CT scanning. A posterolateral tibial plateau fracture model was then created. The acquired fracture model was assembled with 4 groups of internal fixations: Group A, novel anatomical plate; Group B, straight buttress plate; Group C, oblique T-shaped locking plate; Group D, two lag screws. Axial loads of 500, 1,000 and 1,500 N perpendicular to the horizontal plane were used to simulate the stress on the lateral plateau of a 65 kg person standing, walking and fast running.
Results: Vertical displacements of the posterolateral fragments in each of the four groups gradually increased under loads from 500 N to 1,500 N. The maximum displacement of the fracture fragment in four groups were all located on the lateral side of the proximal part, and the displacement gradually decreased from the proximal part to the distal end. The maximum displacement values under the axial load of 1,500 N was in the following order: novel anatomical plate (1.2365 mm) < oblique T-shaped locking plate (1.314 mm) < two lag screws (1.3747 mm) < straight buttress plate (1.3932 mm). As the axial load increased, the stress value of the different internal fixation models gradually increased. The stress behavior of the same internal fixation model under different loads was similar. The maximum stress value under the axial load of 1,500 N was in the following order: novel anatomical plate (114.63 MPa) < oblique T-shaped locking plate (277.17 MPa) < two lag screws (236.75 MPa) < straight buttress plate (136.2 MPa).
Conclusion: The patients with posterolateral plateau fractures fixed with a novel anatomical plate in standing, walking and fast running can achieve satisfactory biomechanical results, which lays the foundation for future applications. At the same time, clinical fracture types are often diverse and accompanied by damage to the soft tissue. Therefore, the ideal surgical approach and appropriate internal fixation must be selected based on the patient's injury condition.
Background
Posterolateral plateau fractures account for up to 11.7%–15.6% of all tibial plateau fractures (1, 2). It is usually difficult to be detected based on x-ray images of the knee joint alone. With the widespread use of computed tomography (CT), it has been reported that, 54.3% of lateral plateau fractures involve the posterolateral plateau (3), and 44.32% of bicondylar fractures involve the posterolateral plateau (4). Posterolateral tibial plateau fractures are also intra-articular fractures that generally require open reduction and internal fixation. The purpose of operation is to restore the alignment of the lower limb and restore the flatness of the joint surface.
The exposure is often blocked by the fibular head, which increases the difficulty of treatment. For slightly displaced fractures, two lag screws from anterior to posterior are usually used for the fixation. For the fractures requiring reduction, the posterolateral approach without fibular osteotomy can well expose the posterolateral fracture line in most cases without disturbing the stability of the knee joint and the common peroneal which is reported to achieves good reduction and clinical results (5). A posterolateral buttress plate or oblique T-shaped plate is commonly inserted through the approach. Based on the anatomical shape of the posterolateral tibial plateau, a novel anatomical plate was designed to fix the fracture through posterolateral approach, and previous clinical study has proven that the plate is safe and effective in 12 patients during a 12–34-month follow-up (6). However, there is still a lack of comparison of the effects of the novel fixation method with currently common-used fixations. The effect of surgical fixation is closely related to the biomechanical properties of the internal fixation. Finite element analysis is one of the most powerful mechanical property analysis tools in biomechanical research (7). It can simulate geometric models of various structures, assign biomaterial properties to various tissues, and can well reflect the overall trend of their biomechanical properties.
Therefore, the purpose of this study is to compare the biomechanical stability of the novel posterolateral anatomical plate of tibial plateau with three other commonly used clinical internal fixations through the finite element method, thereby providing a theoretical basis for clinically selecting appropriate internal fixation to treat the posterolateral tibial plateau.
Methods
The CT scan data conducted through 0.625 mm slice thickness for the full length of right tibiofibula on a healthy adult male (27 years old, 175 cm in height, 65 kg body weight) without comorbidities, such as instability, fracture, degeneration, and osteoarthritis, was obtained and used to construct a three-dimensional tibiofibula finite element model using Mimics software (v21.0, Materialize Company, Belgium). the initial model was further improved using Geomagic Studio Software (v2017, 3D system Inc., Rock Hill, USA).
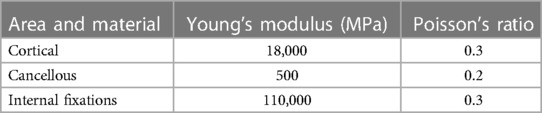
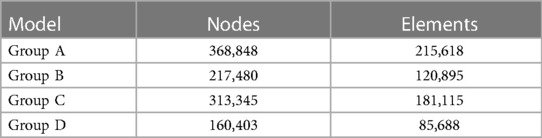
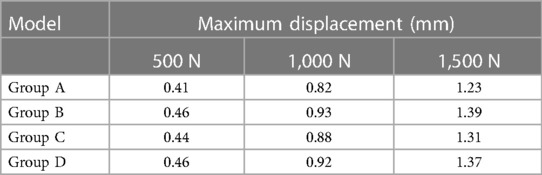
In addition, a posterolateral tibial plateau fracture model was created as previously reported (8) using SolidWorks (v2017, Dassault Systemes, S.A, Paris, France). The detailed method was as follows: A rectangle was made based on the maximum left-right diameter of the tibial plateau and the maximum anteroposterior diameter of the lateral plateau. The intersection of the posterior 1/3 of the tibial plateau and the lateral line of the rectangle was at Point a, and the intersection of the lateral 1/3 of the tibial plateau and the posterior line of the rectangle was at Point b. The perpendicular lines passing through a and b intersected at Point c. Then a line was made through Point c which angles at 120° with the straight-line ac. Since the tibial plateau has a posterior slope angle of about 10°, sagittal angle between posterolateral fracture fragment and plane of articular surface of tibial plateau was set 80°. On the coronal plane, the distance from the fracture line of the articular surface to the most distal end was 27.95 mm, which was very close to the average value of 28 mm reported in the previous study (9). (Shown in Figure 1).
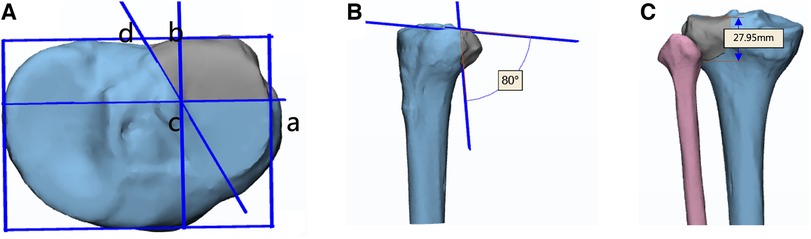
Figure 1 Model of posterolateral column fracture of the tibial plateau. (A) the angle between fracture line ac and cd on the cross plane is 120°; (B) the angle between the fracture line and the articular surface in the sagittal plane is 80°; (C) the distance from the articular surface to the distal point of the fracture line is 27.9 mm.
The acquired posterolateral fracture model of the tibial plateau was assembled with 4 groups of internal fixations on the assembly interface using the SolidWorks. The internal fixation was fixed at 5 mm below the tibial plateau using the isometric outer surface of the tibia (10). The screws were set as smooth cylinders, and 4 groups of internal fixation models were obtained, as shown in Figure 2.
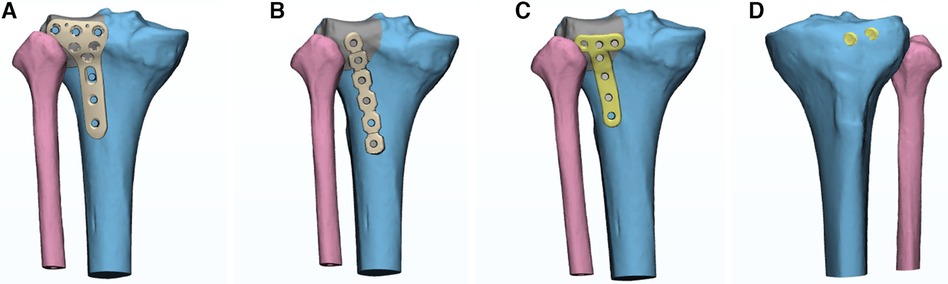
Figure 2 Internal fixation models of four groups. (A) Group A: novel anatomical plate group; (B) Group B: straight buttress plate group; (C) Group C: oblique T-shaped locking plate group; (D) Group D: two lag screws group.
The assembled 4 groups of internal fixation models were imported into Ansys (v17.0, ANSYS, Inc., Canonsburg, PA, USA) for analysis. The tibia, plates and screws were set as homogeneous and isotropic linear elastic materials in the study. In terms of boundary conditions, the distal tibia was set as the translation and rotation of the distal tibial underside was constrained in three dimensions. The models of the volume meshes were imported into Mimics software to endow material properties. The material properties of tibia, plates and screws were set according to relevant references (7, 11), as shown in Table 1. The friction coefficient of the fracture surface was set to 0.4 (12). Plates and screws were constructed as rigid connections through common nodes of shared elements. The grids of the 4 groups of internal fixation models were optimized and set, and the numbers of elements and nodes of various models in the experiment were shown in Table 2.
Previous studies have shown that under normal gait, the biomechanical load on the knee joint is approximately two to three times of the body weight (13, 14). When walking, mechanical axis of the lower limb is biased towards the medial condyle, so the medial plateau of the tibia has a larger stress area accounting for 60%, and the lateral plateau accounts for 40% of the stress. In our study, axial loads of 500, 1,000 and 1,500 N perpendicular to the horizontal plane were used to simulate the stress on the lateral plateau of a 65 kg person standing, walking and fast running (15).
Main Outcome Indicators included displacement distribution and maximum displacement of model fracture fragments in each group, as well as stress distribution and peak value of internal fixation.
Results
Vertical displacements of the posterolateral fragments in each of the four groups gradually increased under loads from 500 N to 1,500 N (Table 3). As the axial load increased, the displacement nephograms of the fracture fragments in each group showed similar distribution characteristics. Therefore, the article only provided the fracture fragment displacement cloud diagram under the axial load of 1,500 N, as shown in Figure 3. The maximum displacement of the fracture fragment in four groups were all located on the lateral side of the proximal part, and the displacement gradually decreased from the proximal part to the distal end. Under the load of 500–750–1500 N, the fracture fragment displacement of the novel anatomical plate group was the smallest, while the fracture fragment displacement of the straight buttress plate group was the largest. The maximum displacement values under the axial load of 1,500 N were in the following order: novel anatomical plate group (1.2365 mm) < oblique T-shaped locking plate group (1.314 mm) < two lag screws group (1.3747 mm) < straight buttress plate group (1.3932 mm).
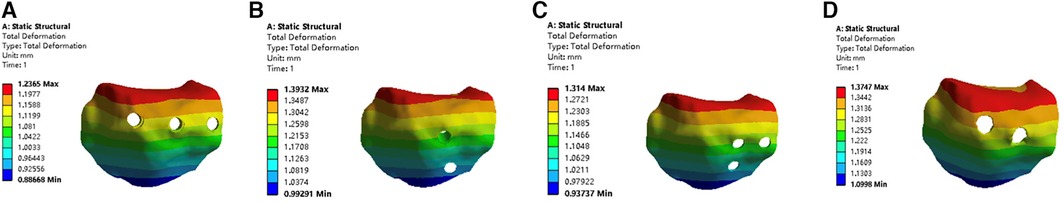
Figure 3 Vertical displacement of the posterolateral fragments of the four groups under an axial load of 1,500 N. (A) novel anatomical plate group; (B) straight buttress plate group; (C) oblique T-shaped locking plate group; (D) two lag screws group.
As the axial load increased, the stress value of the different internal fixation models gradually increased (Table 4). Since the stress behavior of the same internal fixation model under different loads was similar, the article only provided the stress distribution cloud diagram of the internal fixations under the load of 1,500 N, as shown in Figure 4. The maximum stress of the fixation in the novel anatomical plate group was around the most distal screw hole, and the stress distribution is relatively uniform. The stress of the straight buttress plate group was mainly focused on the tails of four distal screws and the local area of the plate between them, and the maximum value was around the most distal screw hole. The stress distribution in oblique T-shaped locking plate group was focused on local areas of the connection between the plate head and the stem and on the screw located while the maximum stress was found on the middle screw hole. In the two lag screws group, the stress maximum was mainly focused on head closing to the end cap. The maximum stress value under the axial load of 1,500 N were in the following order: novel anatomical plate group (114.63 MPa) < oblique T-shaped locking plate group (277.17 MPa) < two lag screws group (236.75 MPa) < straight buttress plate group (136.2 MPa).

Table 4 Maximum stress experienced by internal fixation devices under different loads of each group.

Figure 4 Stress distribution of the four groups under an axial load of 1,500 N.(A) novel anatomical plate group; (B) straight buttress plate group; (C) oblique T-shaped locking plate group; (D) two lag screws group.
Discussion
The prognosis of tibial plateau fractures is related to the quality of anatomical reduction of the joint surface and stable osteosynthesis to enable early knee mobilization (5). Currently, there are two difficulties in treating posterolateral tibial plateau fractures. One is the surgical approach. The posterolateral tibial plateau is surrounded by the fibular head, posterolateral complex (PLC), common peroneal nerve, popliteal nerve and vessels. Access to the posterior region of the knee is often considered a difficult task due to the depth of the operative field and the presence of vascular and nervous elements that pass through it. It is hard to achieve effective reduction through the anterolateral surgical approach which is most familiar to orthopedic surgeons. Approaches used in posterior tibial plateau fractures (PTPFs) have undergone significant changes in recent years (16–18). However, if the posterolateral surgical approach is chosen, the surgeons will face the second difficulty, that is the choice of internal fixation method. The existing internal fixation methods cannot achieve sufficient and effective fixation, and inappropriate internal fixation will inevitably increase the detachment of the posterolateral knee joint structure, increasing the risk of blood vessel and nerve damage.
The anterolateral approach is the most commonly used and familiar surgical approach by orthopedic surgeons because it is safe and simple to operate. After fracture reduction, two lag screws from anterior to posterior are usually used fixation method. The fixation can be completed through the anterolateral approach and is mostly used for large, complete posterolateral fractures. However, it is difficult to directly expose the posterolateral fracture through this approach. Although the posterolateral articular surface can be directly viewed through the joint space above the fibular head, it is difficult to maintain reduction. When the posterolateral fracture is comminuted or the bone fragment is small, sometimes only one screw can be fixed to the posterolateral fracture fragment, and it is rather difficult to fix the fracture effectively. Previous research found that compared with lateral anatomic 3.5 mm L-shaped locking plate, two lag screws and posterolateral 3.5 mm six-hole straight buttress plate fixations of posterolateral tibial plateau fractures achieved less stability (10). This was similar to the results of the current study.
The posterolateral approach can directly expose the posterolateral plateau area. During the operation, the posterior split bone fragments are lifted up. After the collapsed tibial platform is raised and reduced, autogenous bone or artificial bone can be filled in. The approach facilitates reduction and bone grafting which also helps the maintenance of reduction. During the operation, the lateral head of the gastrocnemius muscle is stretched medially, and the biceps femoris muscle and common peroneal nerve are stretched lateral to protect the PLC of the knee joint. Huo et-al (19) followed up 200 patients with posterolateral fractures of the tibial plateau for 1 year after surgery, and compared the advantages and disadvantages of the posterolateral approach with the anterolateral approach, and concluded that it is more suitable for some comminuted posterolateral fractures. He reported the posterolateral approach increased the HSS score by 6.1 points compared with the anterolateral approach when the diameter of the fracture fragment was less than 20 mm.
After reduction, a straight buttress plate or an oblique T-shaped locking plate is usually used for support and fixation. The posterolateral buttress plate has been proven to achieve “adequate stability” for posterolateral shearing tibial plateau fracture as the vertical displacement of the fragment under axial load was no more than 1 mm (8). However, the fixation methods are not anatomical plates which require reshaping to ensure that the plates are fit to the posterior surface of the tibia, and special attention must be paid to avoid damage to the anterior tibial artery. The study showed the stress distribution of novel anatomical plate was relatively uniform. Based on previous studies (20, 21), a displacement of 2 mm was regarded as acceptable and a displacement that could shorten the healing time with a small range of motion. Naturally, the smaller the maximum displacement, the greater the postoperative stability of the fracture. As a result, the novel anatomical plate provides adequate mechanical stability, and the overall stability is higher than the other three sorts of fixations.
The novel anatomical plate better fits the shape of the posterolateral tibial plateau. The proximal end of the plate wraps the posterolateral plateau without being restricted by the fibular head. The proximal universal screw-hole design can ensure that the screws are implanted in parallel to the joint surface, thereby achieving the “raft effect” to effectively support the articular surface. This finite element analysis showed the plate achieved better biomechanical properties. The short design of the modified plate can avoid injury to the branches of the posterior tibial artery. MAY (22) measured the distance between the point where the anterior tibial artery passes through the interosseous membrane and the tibial plateau and the top of the fibula on digital subtraction angiography images of 219 lower limbs, which were (50.9 ± 6.9) and (36.5 ± 6.0) mm, respectively. Moreover, the anterior tibial artery has poor mobility due to the traction of the interosseous membrane fibers, so the length of the plate should be especially paid attention for the posterolateral approach.
The limitations of this study are as follows. The experiment gave a single axial static load, but the real tibial plateau force is multi-directional and dynamic (23), and the failure of fracture fixation may also be caused by repeated application of load. The finite element model is an ideal model and ignores the impact of soft tissue on the surrounding Impact, only consider the excellence of the internal fixation from biomechanics. The fracture model is established as an ideal single split fracture, but clinically there are various types of fractures, and they are often accompanied by damage to the soft tissue around the knee joint. Therefore, it needs to be based on select the ideal surgical approach and appropriate internal fixation according to the patient's injury condition. The experiment adopts the finite element analysis method, while ignoring the influence of the fibular support and failing to fully simulate the stress on the tibial plateau. Therefore, the next step will be to conduct biomechanical experiments on fake bone models and cadaver bone models to verify the finite element results.
Conclusions
The results of the finite element analysis show that the novel anatomical plate has better biomechanical stability than the traditional commonly used straight buttress plate, oblique T-shaped locking plate and two lag screws when simulating the stress on the lateral plateau of a 65 kg person standing, walking and fast running. It shows good biomechanical stability, laying the foundation for its future applications. However, the clinical fracture types are often diverse and accompanied by damage to the soft tissue around the knee joint. Therefore, the ideal surgical approach and appropriate internal fixation must be selected based on the patient’s injury condition.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
ZJ: Conceptualization, Data curation, Writing – original draft. XJ: Funding acquisition, Supervision, Writing – review & editing. DL: Resources, Writing – original draft. JZ: Writing – review & editing. BY: Writing – review & editing. CY: Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Scientific Research Foundation provided by of Pudong Health Committee of Shanghai (No. PW2021A-09), Youth Scientific Research Foundation provided by Shanghai Municipal Health Commission (No. 20204Y0121), Natural Science Foundation of Shanghai (Grant No. 22ZR1455800), Program for the Outstanding Clinical Discipline Project of Shanghai Pudong (Grant No. PWYgy2021-04), and Program for Clinical Medicine Innovation Fund Project of Fudan Zhangjiang Institute (No. KP9202101).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Giordano V, Pires RE, Pimenta FS, Campos TVO, Andrade MAP, Giannoudis PV. Posterolateral fractures of the tibial plateau revisited: a simplified treatment algorithm. J Knee Surg. (2022) 35(9):959–70. doi: 10.1055/s-0040-1721026
2. Gao W, Qi X, Zhao K, Feng X, Yang Y, Liu P, et al. Lateral locking plate plus antero-posterior lag screws techniques for the management of posterolateral tibial plateau fracture: preliminary clinical results and biomechanical study. Arch Orthop Trauma Surg. (2023) 143(6):3163–72. doi: 10.1007/s00402-022-04554-7
3. Yi Z, Hui S, Binbin Z, Jianfei T, Huipeng S, Jiong M, et al. A new strategy to fix posterolateral depression in tibial plateau fractures: introduction of a new modified frosch approach and a “barrel hoop plate” technique. Injury. (2020) 51(3):723–34. doi: 10.1016/j.injury.2020.01.023
4. Zhu Y, Meili S, Dong MJ, Zhai QL, Yao L, Wang JC, et al. Pathoanatomy and incidence of the posterolateral fractures in bicondylar tibial plateau fractures: a clinical computed tomography-based measurement and the associated biomechanical model simulation. Arch Orthop Trauma Surg. (2014) 134(10):1369–80. doi: 10.1007/s00402-014-2037-1
5. Alencar Neto JB, Rego IEQ, Lopes MBG, Lima LL, Clazzer R, Ariel de Lima D. Outcomes of the carlson approach in the treatment of posterior tibial plateau fractures. Rev Bras Ortop (Sao Paulo). (2023) 58(2):313–9. doi: 10.1055/s-0042-1749201
6. Jian Z, Ao R, Zhou J, Jiang X, Zhang D, Yu B. A new anatomic locking plate for the treatment of posterolateral tibial plateau fractures. BMC Musculoskelet Disord. (2018) 19(1):319. doi: 10.1186/s12891-018-2216-2
7. Yan B, Huang X, Xu Y, Zou C. A novel locking buttress plate designed for simultaneous medial and posterolateral tibial plateau fractures: concept and comparative finite element analysis. Orthop Surg. (2023) 15(4):1104–16. doi: 10.1111/os.13660
8. Zhang W, Luo CF, Putnis S, Sun H, Zeng ZM, Zeng BF. Biomechanical analysis of four different fixations for the posterolateral shearing tibial plateau fracture. Knee. (2012) 19(2):94–8. doi: 10.1016/j.knee.2011.02.004
9. Chang SM, Zheng HP, Li HF, Jia YW, Huang YG, Wang X, et al. Treatment of isolated posterior coronal fracture of the lateral tibial plateau through posterolateral approach for direct exposure and buttress plate fixation. Arch Orthop Trauma Surg. (2009) 129(7):955–62. doi: 10.1007/s00402-009-0829-5
10. Ren D, Liu Y, Lu J, Xu R, Wang P. A novel design of a plate for posterolateral tibial plateau fractures through traditional anterolateral approach. Sci Rep. (2018) 8(1):16418. doi: 10.1038/s41598-018-34818-5
11. Gao S, Yao QC, Geng L, Lu J, Li M, An K, et al. A finite element analysis of the supportive effect of a new type of rotary support plate on lateral tibial plateau fractures. Ann Transl Med. (2022) 10(18):1020. doi: 10.21037/atm-22-4529
12. Chen P, Lu H, Shen H, Wang W, Ni B, Chen J. Newly designed anterolateral and posterolateral locking anatomic plates for lateral tibial plateau fractures: a finite element study. J Orthop Surg Res. (2017) 12(1):35. doi: 10.1186/s13018-017-0531-1
13. Taylor WR, Heller MO, Bergmann G, Duda GN. Tibio-femoral loading during human gait and stair climbing. J Orthop Res. (2004) 22(3):625–32. doi: 10.1016/j.orthres.2003.09.003
14. Lu Y, Bai H, Wang Q, Ren C, Li M, Li Z, et al. The study of biomechanics and finite element analysis on a novel plate for tibial plateau fractures via anterolateral supra-fibular-head approach. Sci Rep. (2023) 13(1):13516. doi: 10.1038/s41598-023-40842-x
15. Hu Z, Ren W, Zhang W, Li L, Xu W. Potential problem and solution of lateral plate postposition for the posterolateral tibial plateau fracture. J Orthop Surg Res. (2023) 18(1):984. doi: 10.1186/s13018-023-04397-x
16. Mancini N, Salvato D, Delmastro E, Belluati A, Salini V, Placella G. A modified frosch approach for posterior tibial plateau fractures: technical note and case series. Injury. (2023) 54(Suppl 1):S9–s14. doi: 10.1016/j.injury.2021.03.030
17. Foster B, Rodriguez-Buitrago A, Obremskey WT. Prone posteromedial approach for posterior column tibial plateau fractures. J Orthop Trauma. (2020) 34(Suppl 2):S35–s36. doi: 10.1097/bot.0000000000001832
18. Frosch KH, Balcarek P, Walde T, Stürmer KM. A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures. J Orthop Trauma. (2010) 24(8):515–20. doi: 10.1097/BOT.0b013e3181e5e17d
19. Huo Y, Xu G, Yin Z, Yu J, Sun X, Li L, et al. Effects of surgical approaches and morphological characteristics on the follow up outcomes of patients with posterolateral tibial plateau fractures. Medicine (Baltimore). (2020) 99(17):e19854. doi: 10.1097/md.0000000000019854
20. Kfuri M, Schatzker J. Revisiting the schatzker classification of tibial plateau fractures. Injury. (2018) 49(12):2252–63. doi: 10.1016/j.injury.2018.11.010
21. Schatzker J, Kfuri M. Revisiting the management of tibial plateau fractures. Injury. (2022) 53(6):2207–18. doi: 10.1016/j.injury.2022.04.006
22. May H, Kastan O, Emre TY, Cetin M, Unal M, Kose O. Anterior tibial artery and its clinical importance in the posterolateral approach to the tibial plateau: an angiographic study on 219 lower limbs. J Knee Surg. (2022) 35(7):725–30. doi: 10.1055/s-0040-1716849
Keywords: finite element analysis, tibial plateau fracture, plate, screw, biomechanic study
Citation: Jian Z, Jiang X, Li D, Zhou J, Yu B and Yi C (2024) Finite element analysis of a novel anatomical plate in posterolateral plateau fractures. Front. Surg. 11:1346462. doi: 10.3389/fsurg.2024.1346462
Received: 29 November 2023; Accepted: 1 July 2024;
Published: 15 July 2024.
Edited by:
Longpo Zheng, Tongji University, ChinaReviewed by:
Stefano Marco Paolo Rossi, Fondazione Poliambulanza Istituto Ospedaliero, ItalyKonstantinos Markatos, Salamina Medical Center, Greece
Wenguang Gu, First Affiliated Hospital of Harbin Medical University, China
Xing Wu, Tongji University, China
© 2024 Jian, Jiang, Li, Zhou, Yu and Yi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhen Jian, amlhbnpoZW4yMUAxMjYuY29t; Chengqing Yi, eWNxMzAwMEAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Zhen Jian
Zhen Jian Xinhua Jiang1†
Xinhua Jiang1†