- 1Department of Surgery, Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
- 2Department of Surgery, Shaheed Mohtarma Benazir Bhutto Medical College Lyari, Karachi, Pakistan
- 3Department of Surgery, Foundation University Medical College, Islamabad, Pakistan
- 4Department of Surgery, Shaheed Mohtarma Benazir Bhutto Medical University, Larkana, Pakistan
- 5Department of Surgery, Liaquat College of Medicine and Dentistry, Karachi, Pakistan
Background: This analysis addresses the uncertainty surrounding the efficacy of glue mesh fixation (GMF) compared with tack mesh fixation (TMF) in laparoscopic herniorrhaphy. Our meta-analysis incorporates recently conducted randomized controlled trials (RCTs) to enhance the reference for assessing the efficacy and safety of GMF.
Methods: PubMed Central, Google Scholar, Science Direct, and Cochrane Library were extensively reviewed for articles in the English language performed from inception to May 2023 using the keywords “Glue mesh repair,” “Tack mesh repair,” “Inguinal Hernia,” “Herniorrhaphy,” “Laparoscopic,” “Mesh Fixation,” and “Randomized controlled trials.”
Results: In this meta-analysis, we incorporated a total of 20 randomized controlled trials, evaluating each article individually using quality ratings. Compared with TMF, GMF demonstrated a significant reduction in the incidence of chronic pain [RR: 0.40, (0.23, 0.68)] and pain scores on postoperative day 1 [MD: −1.07, (−1.90, −0.25)]. We also used funnel plots and Egger's regression to test for publication bias.
Conclusion: In summary, this meta-analysis establishes the significance of GMF in reducing chronic pain and postoperative day 1 pain compared with TMF. However, no statistically significant difference was noted between the GMF and TMF groups concerning hematoma, seroma, operation time, recurrence rate, and total complications. Nonetheless, given the small number of cases in this study, the findings must be validated in the future by multicenter, large-sample, high-quality RCTs.
Introduction
Hernia manifests when tissue protrudes beyond its anatomical confines. The bulge is most noticeable while standing, coughing, or straining. Obesity, pregnancy, hard lifting, COPD, and aging can all cause it to be congenital or develop later in life (1). Hernias are often diagnosed clinically and confirmed with imaging such as ultrasound and MRI (2). Herniorrhaphy, a popular surgical treatment, is used to correct approximately 800,000 inguinal hernias in the United States each year (3). A crucial reason for urgent hernia therapy is strangulation, which causes a loss of blood flow to trapped tissue (4, 5). Inguinal hernias constitute more than 75% of all abdominal hernias and are predominantly found in men, making them a frequently encountered medical condition by general surgeons (6, 7). There is a greater chance of discomfort, tissue damage, and nerve entrapment when employing open surgical techniques. Consequently, it is preferable to use less invasive laparoscopic techniques such as transabdominal preperitoneal (TAPP) and completely extraperitoneal (TEP) techniques (8–10). While the TAPP method entails dissecting the abdominal wall, which increases the risk of gastrointestinal injuries, the TEP approach bypasses the abdominal cavity, preventing injury and adhesions (11). The most frequent consequence, inguinodynia (pain following surgery that lasts longer than 3 months) (12), influences surgeons' decisions between adhesive mesh and penetrative tacker techniques (13, 14).
Glue mesh fixation (GMF), compared with tack mesh fixation (TMF) provides less tension on the surrounding tissue (15). The exploration of mesh fixation with fibrin glue or cyanoacrylate tissue adhesive, as an alternative to traditional suture or tack methods, has shown remarkable results (16). The study conducted by Nizam et al. (17) demonstrated that the fibrin glue method proved to be a cost-effective approach that resulted in a reduced hospital stay compared with the TMF group. The GMF method has also reduced the risk of inguinodynia and recurrence in randomized controlled trials (RCTs) over comparative groups (18, 19).
In a prior meta-analysis conducted by Nan Hu (20) comparing GMF and TMF, it was concluded that GMF is more efficacious in diminishing the incidence of chronic pain compared with TMF. Moreover, the findings suggest a lower occurrence of hematoma in the GMF group compared with the TMF group. Notably, this meta-analysis does not reveal any disparities in the pain score on postoperative day 1, operation time, and recurrence rate between the GMF and TMF groups. Conversely, the analysis highlights a significant distinction, indicating that GMF markedly reduces the risk of total complications. Certain outcomes in the analysis were assessed using a fixed-effects model; however, it is recommended to utilize a random-effects model when incorporating studies with diverse effect sizes, as most of the studies included in this analysis consist of varied effect sizes (21).
There is only a slight variation between these two methods and requires further assessment. In this meta-analysis, we aim to address a gap in the current body of research by conducting a thorough examination of the available RCTs that investigate the impact of glue mesh vs. tack mesh in patients undergoing laparoscopic inguinal hernia repair. Our study's main objective is to conduct a thorough analysis of primary outcomes, such as chronic pain and pain on postoperative day 1, and secondary outcomes, including recurrence rate, total complications, hematoma, and seroma.
Methods
This meta-analysis was conducted by following Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (22).
Study selection
A literature search was conducted on PubMed Central, Google Scholar, Cochrane Library, and Science Direct from inception to May 2023. The search strings used in different databases are given in Supplementary Table S1. All duplicated articles were removed using Endnote ×9 (Clarivate Analytics, USA). Two separate individuals (MA and YS) carefully reviewed the remaining articles and selected articles to be analyzed that matched the inclusion criteria mentioned below. Articles were selected based on the title/abstract, and then a full-text evaluation was conducted. In case of disagreement, a third reviewer (AR) was consulted. Articles were selected based on the following eligibility criteria: (a) studies comparing GMF vs. TMF using a laparoscopic technique, (b) patients of age 18 years or above with inguinal hernia, (c) studies with at least one outcome of interest, (d) randomized controlled trials. The outcomes of interest were chronic pain, which was defined as persistent pain for more than 3 months, pain score on postoperative day 1, operation time, recurrence rate, which refers to the number of cases in which hernia recurred after the initial surgical intervention, seroma, hematoma, and total complications. Any non-human trial, language apart from English, patients under the age of 18 years, suture fixation method and open repair techniques, duplicated studies, articles irrelevant to the research purpose, and studies with incomplete information regarding outcomes were excluded.
Data extraction and quality assessment
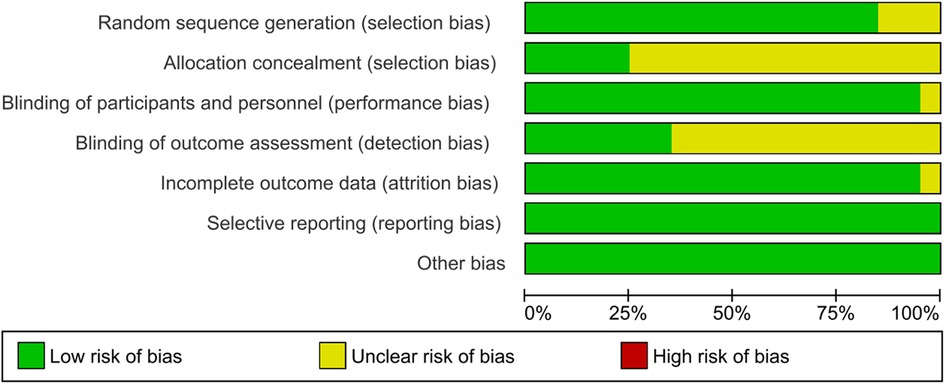
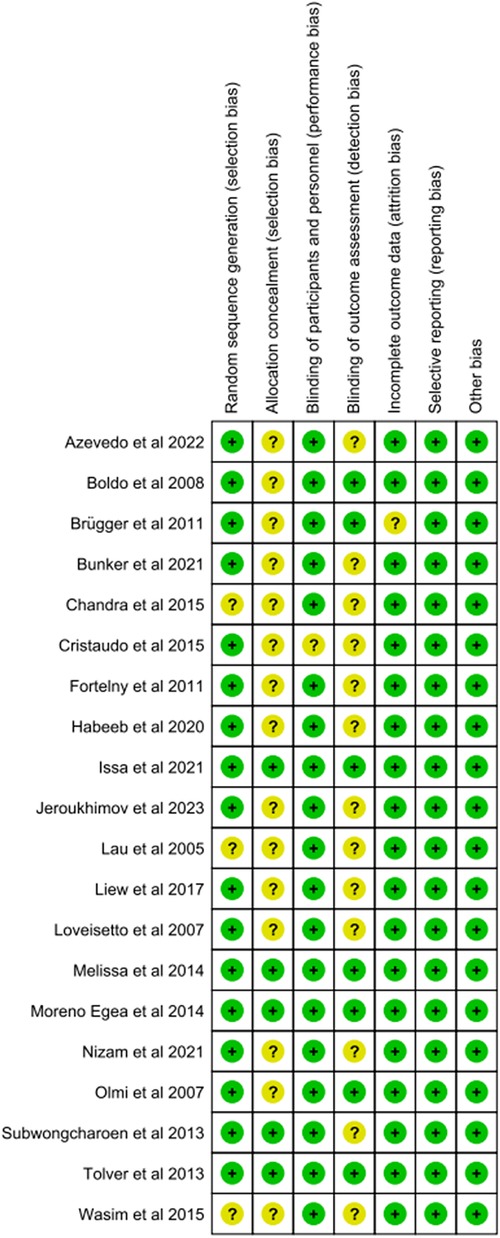
In each study, the following data were extracted: (a) study name and year, (b) the number of patients in each group (TMF vs. GMF), (c) general patient characteristics (age, gender, and BMI), (d) follow-up time, (e) type of approach used (TAPP or TEP), (f) type of tacks and glue used, and (g) outcomes of interest. The quality assessment of the selected RCTs was conducted independently by two reviewers (AR and SA) using Cochrane risk of bias (RoB 2.0) tools including (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding outcome assessment (detection bias), (5) incomplete outcome data (reporting bias), and other bias. Each was assessed individually, and the potential risk for each outcome was characterized into three groups: low risk, high risk, or unclear (23).
Statistical analysis
The statistical analysis utilized Review Manager (RevMan Version 5.4.1), which is a software provided by the Cochrane Collaboration Network. Dichotomous data were used to derive the risk ratio (RR) and corresponding 95% confidence intervals (95% CIs). Similarly, for continuous outcomes, the mean difference (MD) and their 95% CIs were obtained using a random-effects model. A p-value of less than 0.05 was judged as significant. Higgins I2 was used to measure heterogeneity. The value of I2 = 25%–50% was regarded as mild heterogeneity, 50%–75% as moderate, and >75% as high heterogeneity (24). Funnel plots were created for the outcomes that included more than 10 studies to check for any publication bias. The Egger test was performed to check if there were any publication bias. Continuous outcomes reported as median with interquartile ranges were converted to mean and standard deviations using Wan's method (25).
Results
Study selection and characteristics
After eliminating duplicates, our initial literature search yielded 3,087 relevant articles. Following the screening of titles and abstracts, 11 articles were assessed for eligibility, resulting in the exclusion of seven articles (26–32). The reasons for exclusion are outlined in Figures 1, 4. Subsequently, four additional studies (15, 19, 33, 34) were incorporated into the synthesis, along with 16 studies from previous meta-analyses (17, 35–49), particularly the one conducted by Nan Hu et al. (20). In total, this meta-analysis included a total of 20 articles (15, 17, 19, 33–49). The collective sample involves 2,928 patients with inguinal hernias, distributed as 1,582 in the TMF group and 1,346 in the GMF group, meeting the inclusion and exclusion criteria. The mean age of patients in the TMF group was 51.75 years, and in the GMF group, it was 51.39 years, with an average follow-up time of 12 months. The PRISMA flow chart, depicted in Figure 1, provides a concise overview of the outcomes derived from our extensive literature review. In addition, Table 1 furnishes the baseline characteristics of patients in each study.
Risk of bias of the included studies
We assessed the risk of bias using the Cochrane Handbook for Systematic Reviews of Interventions. All the studies included in this meta-analysis were of high quality (Figure 2, 3). The details of the risk assessment are provided in Supplementary Table S2.
Meta-analysis outcomes
Primary outcomes
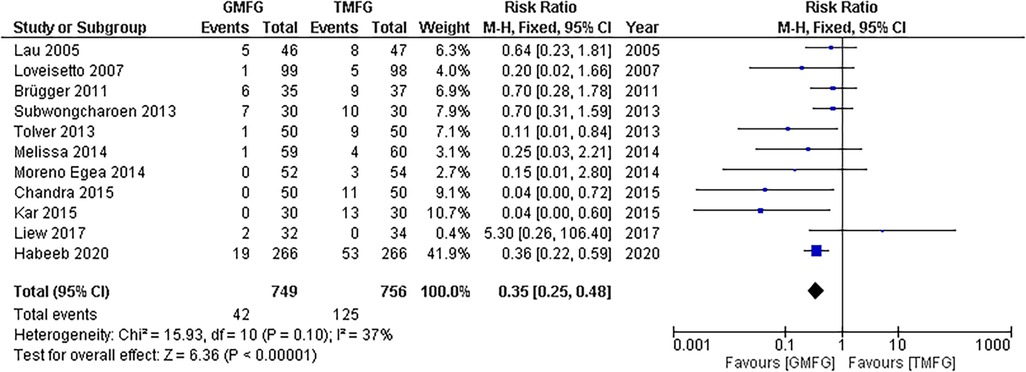
Chronic pain
A meta-analysis using a random-effects model conducted on a total of 11 studies (33, 35, 37, 39, 41, 43–46, 48, 49) consisting of 1,505 patients showed that GMF significantly reduced the incidence of chronic pain in patients who underwent laparoscopic inguinal hernia repair, in comparison with TMF [RR:0.40, 95% CI (0.23,0.68); p = 0.0007] (Figure 4). The studies demonstrated a remarkable consistency, unveiling a notable absence of statistical heterogeneity (p = 0.10; I2 = 37%).
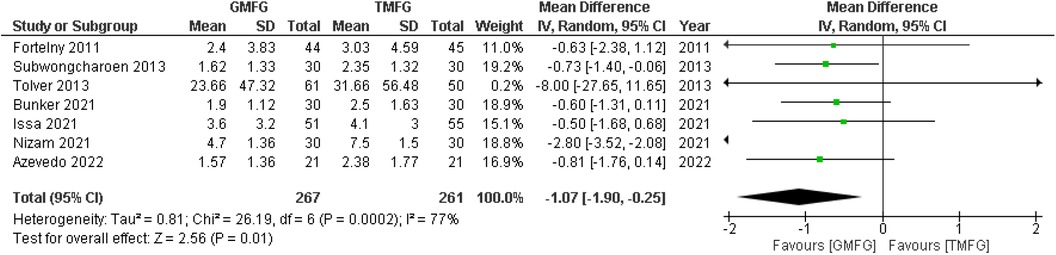
Pain score on postoperative day 1
Seven studies (17, 19, 33, 38, 40, 42, 48), consisting of 528 patients, reported pain scores on postoperative day 1. A random-effects model was used to pool the results, which showed that GMF was significantly associated with decreasing pain score on postoperative day 1 compared with the TMF [MD = −1.07, 95% CI (−1.90,−0.25), p = 0.01] (Figure 5). The analysis showed significant heterogeneity among the studies (p = 0.0002; I2 = 77%).
Leave-one-out analysis
The leave-one-out sensitivity analysis showed that the pain score on postoperative day 1 was affected by a single study, i.e., Nizam et al. (17). Removing that study resulted in a significant reduction in I2 values (p = 0.98; I2 = 0%) and overall effect [MD = −0.68, 95% CI (−1.07, −0.28), p = 0.0008] (Supplementary Figure S1).
Secondary outcomes
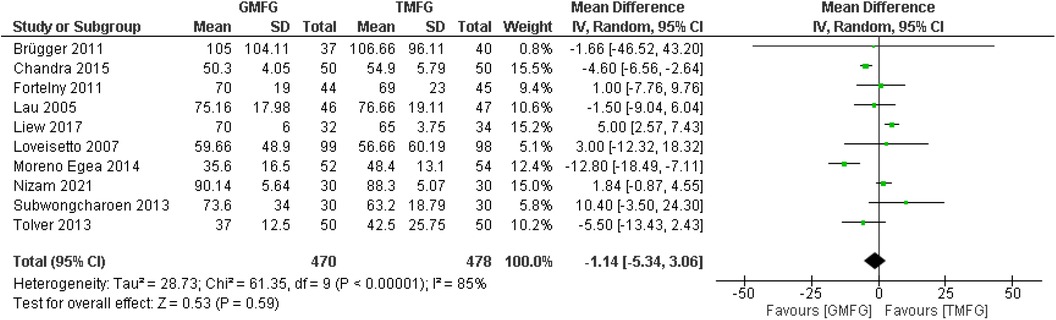
Operation time
A total of 10 studies (17, 33, 35, 37, 39, 40, 43, 44, 46, 48), consisting of 948 patients, provided data on the operation time. A random-effects model was used to pool the combined effect. The results indicated that there was no significant difference in operative time between TMF and GMF [MD = −1.14, 95% CI (−5.34, 3.06), p = 0.59] (Figure 6). There was severe heterogeneity among the studies (p < 0.00001; I2 = 85%).
Leave-one-out analysis
After systematically removing one study at a time, the results consistently showed that the overall effect was unchanged, which suggests that the results of this study were stable.
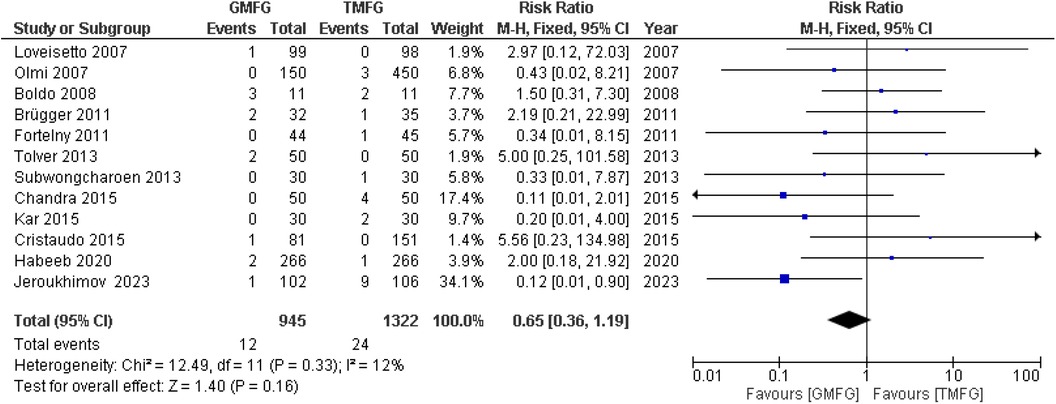
Recurrence rate
A total of 12 studies (15, 33, 34, 36, 37, 39–41, 44, 47–49), consisting of 2,267 patients, reported the incidence of hernia recurrence. A random-effects model was used to pool the combined effect. The studies demonstrated a remarkable consistency, unveiling a notable absence of statistical heterogeneity (p = 0.33; I2 = 12%). The results for the incidence of recurrence rate showed no significant difference between the two groups [RR = 0.80, 95% CI (0.36, 1.78) p = 0.58] (Figure 7).
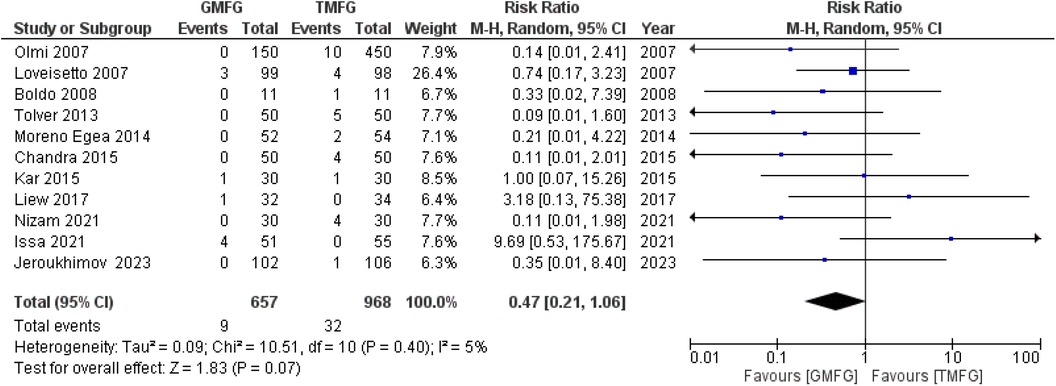
Hematoma
A total of 11 studies (15, 17, 35, 36, 39, 42, 44, 46–49), consisting of 1,625 patients, reported the incidence of hematoma. The incidence of hematoma in the GMF group was 9/657 (1.36%), and it was 32/968 (3.3%) in the TMF group. The studies demonstrated a remarkable consistency, unveiling a notable absence of statistical heterogeneity (p = 0.40, I2 = 5%). A random-effects model was used to pool the combined effect. The results did not show a significant difference between patients in the GMF group and those in the TMF group [RR: 0.47, 95% CI (0.21, 1.06); p = 0.07] (Figure 8).
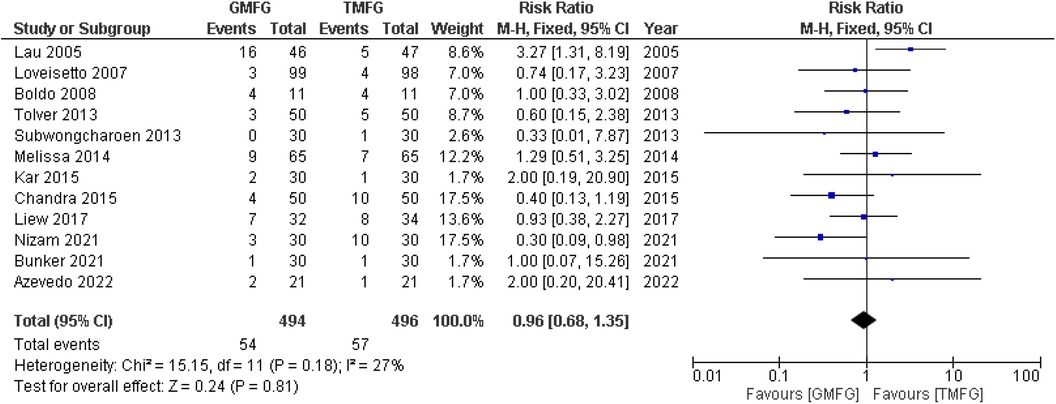
Seroma
A total of 12 studies (17, 19, 33, 35, 36, 38, 39, 43, 44, 45, 48, 49), consisting of 990 patients, reported the occurrence of seroma. The incidence of seroma in the GMF group was 54/494 (10.9%), and the incidence of seroma in the TMF group was 57/496 (11.4%). The studies demonstrated a remarkable consistency, unveiling a notable absence of statistical heterogeneity (p = 0.18, I2 = 27%). A random-effects model was used to pool the combined effect, which showed that no significant difference was observed between both groups [RR: 0.93, 95% CI (0.59, 1.46); p = 0.75] (Figure 9).
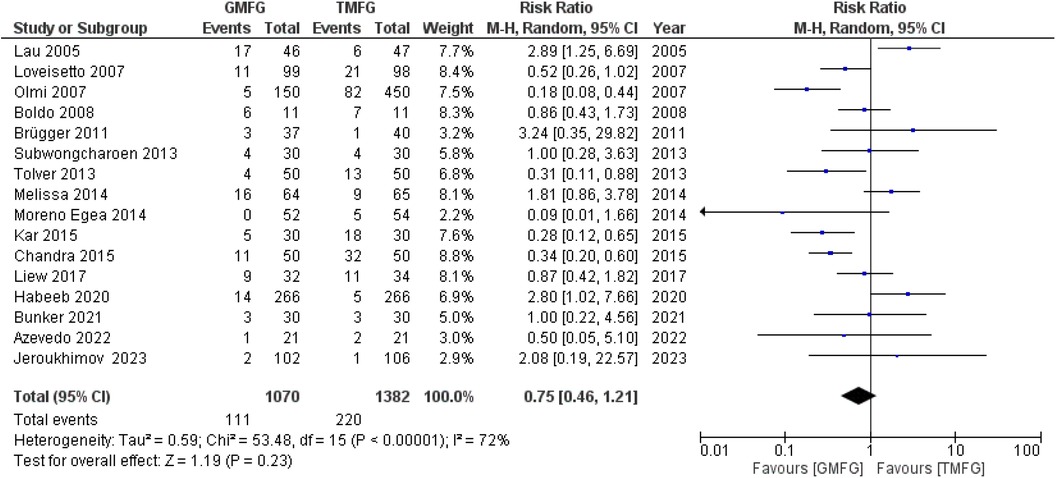
Total complications
A total of 16 studies (15, 19, 33, 35–39, 41, 43–49), consisting of 2,452 patients, reported the incidence of total complications. There was severe statistical heterogeneity found among the studies (p < 0.00001, I2 = 72%). A random-effects model was used to pool the combined effect. The results did not show any significant difference between the two groups [RR: 0.75, 95% CI (0.46, 1.21); p = 0.23] (Figure 10).
Leave-one-out analysis
To identify the source of significant heterogeneity, a sensitivity analysis was conducted. By systematically excluding studies one by one, it was determined that the results remained unchanged, indicating the robustness and stability of this study's findings.
Publication bias
To assess publication bias, we employed various methods, including funnel plots and Egger's regression. Six funnel plots were used for the outcomes of chronic pain, operation time, recurrence rate, hematoma, seroma, and total complications (Supplementary Figures S2–S7). The funnel plots displayed a symmetrical distribution of studies, indicating a lack of asymmetry and no indication of publication bias. In addition, statistical tests using Egger's regression did not yield significant results, further supporting the absence of publication bias in our analysis. Egger's test was performed for chronic pain (p-value = 0.31), operative time (p-value = 0.44), recurrence rate (p-value = 0.82), hematoma (p-value = 0.58), seroma (p-value = 0.68), and total complications (p-value = 0.74).
Discussion
In this meta-analysis, we compared the usage of GMF and TMF in laparoscopic inguinal hernia repair. We concluded that GMF is significantly associated with a lower incidence of chronic pain and postoperative pain score on day 1. However, there was no evidence to suggest that GMF reduces operation time, hematoma, recurrence rate, total complications, and seroma. In laparoscopic inguinal hernia surgery, three primary techniques are employed for securing the mesh. Of these, the application of suture fixation patches is intricate, time-intensive, and infrequently implemented (50). Currently, the prevailing approach in clinical settings involves the frequent utilization of glue or tacks for mesh fixation. The EHS classification system (51), akin to its predecessors, lacks a formal Delphi methodology and a rigorous validity evaluation, which leads to a weak recommendation in the HerniaSurge guidelines (52) for research purposes. It was not employed in the source studies reviewed here, and therefore, the impact of hernia classification on chronic pain and other outcomes was not assessed, aligning with the non-objective of this pragmatic review of RCTs (53).
Postoperative pain following inguinal hernia repair is a prevalent occurrence. The outcomes of our meta-analysis indicated a noteworthy decrease in the prevalence of persistent pain within the GMF group (5.6%) in comparison with the TMF group (16.5%), aligning with the findings of a prior meta-analysis conducted by Nan Hu (20). Numerous studies propose that chronic pain often stems from factors such as nerve traction injury, suture-related issues, mesh interaction, scar tissue compression, and injuries to the pubic tubercle periosteum and spermatic cord (54). Opting for GMF mitigates the risk of nerve damage and compression, while also sparing the periosteum from harm, thereby resulting in a substantial reduction in the incidence of chronic pain (55). In a similar vein, this meta-analysis revealed a statistically significant distinction in pain scores on the first day post-surgery, indicating that GMF resulted in a lower score compared with TMF. Notably, this discovery contradicts the outcomes reported in an earlier meta-analysis (20). In the GMF, the glue was applied to secure the mesh, yet the disparity in operation time between the two groups lacked statistical significance. This suggests that incorporating a glue-fixed mesh in laparoscopic inguinal hernia surgery is unlikely to markedly prolong the procedure, and it remains a straightforward process. Similar outcomes were observed in a previous analysis (20). Local hematoma is a frequent complication in inguinal hernia surgery, often stemming from vascular injury. In laparoscopic procedures, it demands careful attention as it can escalate into a sizable retroperitoneal hematoma, potentially requiring reoperation in unstable patients (56). The higher incidence of hematoma in the TMF may be attributed to injuries in the peritoneum or small muscle vessels, whereas the GMF, steering clear of tissue trauma, displayed a lower occurrence of hematoma (40, 57). However, our analysis indicates a lower hematoma incidence in GMF (1.36%) compared with TMF (3.3%), although this difference lacks statistical significance. Due to the limited sample size, future studies with a larger sample size are needed to thoroughly investigate potential differences in hematoma incidence between GMF and TMF. An RCT conducted by Lau et al. (43) has determined that the occurrence of seroma formation is elevated in the GMF group. This phenomenon has been ascribed to a more pronounced inflammatory response prompted by fibrin glue, potentially amplifying exudation and, consequently, the development of seromas (58). However, our analysis did not reveal a statistically significant difference between the two groups, aligning with the conclusions drawn from previous meta-analyses (55, 57). The recurrence rate determines the success rate of inguinal hernia repair. The rate of hernia recurrence in this meta-analysis was 1.26% in the GMF group and 1.81% in the TMF group. The lack of a statistically significant difference between the two groups implies that utilizing glue for mesh fixation does not enhance the risk of hernia recurrence. These results are consistent with the conclusions reached in earlier meta-analyses (20, 57). This meta-analysis also indicates that the GMF had a lower overall complication rate of 10.37% when compared with the TMF, which has a rate of 15.91%. This reduction, however, is not statistically significant, showing that employing adhesive in laparoscopic tension-free inguinal hernia repair is still a safe option. These findings contradict the conclusions of a study conducted by Nan et al. (20), which asserted that GMF is linked to a lower occurrence of overall complications compared with TMF. This disparity could be explained by the omission of several studies that reported overall complication rates for both groups. Furthermore, the use of fixed-effects models for analysis rather than random-effects models, as advised when dealing with studies of varied sizes, may have contributed to the inconsistency of the results (21).
The limitations identified in this meta-analysis encompass (1) the inclusion of a small number of studies with limited sample sizes; (2) potential language bias due to the restriction to English literature; (3) the inevitable impact on the results from variations in techniques, procedures, mesh materials and types, glue compositions, and mechanical fixation materials across studies; (4) the unavailability of relevant data on cost considerations, preventing an analysis on cost-effectiveness to guide a preference for either method; (5) some studies overlooking the importance of randomization, double-blinding, and allocation concealment in randomized controlled trials, thus influencing the strength of evidence; and (6) inconsistency in follow-up durations among studies, with some lacking sufficient short-term follow-up to adequately assess and compare recurrence rates between the two groups.
In conclusion, this comprehensive meta-analysis compared GMF and TMF in laparoscopic inguinal hernia repair. GMF demonstrated a significant reduction in chronic pain incidence and postoperative pain scores on the first day compared with TMF. Operation time, recurrence rate, hematoma, seroma, and overall complication rates showed no significant differences between the two methods. The recurrence rate was notably low in both groups, with GMF exhibiting a slightly lower overall complication rate. Despite some contradictions with previous meta-analyses, our analysis emphasizes the safety and efficacy of both fixation methods. Limitations include the small number of studies, potential language bias, variations in techniques, and the absence of cost-effectiveness analysis due to data unavailability. Future research with larger sample sizes and comprehensive considerations is warranted.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
SR: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. AR: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZA: Writing – original draft, and Writing – review & editing. SE: Writing – original draft, and Writing – review & editing. SB: Writing – original draft, and Writing – review & editing. MA: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. UK: Data curation, Investigation, Software, Supervision, Writing – original draft, Writing – review & editing. YS: Investigation, Project administration, Software, Validation, Writing – original draft, Writing – review & editing, Conceptualization. SJ: Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. FA: Data curation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. DR: Visualization, Project administration, Supervision, Writing – original draft, Writing – review & editing. SK: Formal Analysis, Validation, Project administration, Supervision, Writing – original draft, Writing – review & editing. MK: Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2024.1321325/full#supplementary-material
References
1. Slater BJ, Pimpalwar A. Abdominal wall defects. Neoreviews. (2020) 21(6):e383–91. doi: 10.1542/NEO.21-6-E383
2. Inguinal Hernia - PubMed. https://pubmed.ncbi.nlm.nih.gov/30020704/ (Accessed December 16, 2023).
3. Morrison Z, Kashyap S, Nirujogi VL. Adult inguinal hernia. StatPearls. Published online (2023).https://pubmed.ncbi.nlm.nih.gov/30725926/ (Accessed June 10, 2023).
4. Ihedioha U, Alani A, Modak P, Chong P, O’Dwyer PJ. Hernias are the most common cause of strangulation in patients presenting with small bowel obstruction. Hernia. (2006) 10(4):338–40. doi: 10.1007/S10029-006-0101-7
6. Berndsen MR, Guðbjartsson T, Berndsen FH. Inguinal hernia - review. Laeknabladid. (2019) 105(9):385–91. doi: 10.17992/LBL.2019.09.247
7. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. (2003) 362(9395):1561–71. doi: 10.1016/S0140-6736(03)14746-0
8. Hope W, Bhimji S. Laparoscopic inguinal hernia repair. StatPearls. Published online (2023).Available online at: https://pubmed.ncbi.nlm.nih.gov/28613576/ (Accessed June 10, 2023).
9. Cunha-E-Silva JA, De Oliveira FMM, Ayres AFSMC, Iglesias ACRG. Conventional inguinal hernia repair with self-fixating mesh versus totally extraperitoneal laparoscopic repair with polypropylene mesh: early postoperative results. Rev Col Bras Cir. (2017) 44(3):238–44. doi: 10.1590/0100-69912017003003
10. Kalra T, Soni RK, Sinha A. Comparing early outcomes using non absorbable polypropylene mesh and partially absorbable composite mesh through laparoscopic transabdominal preperitoneal repair of inguinal hernia. J Clin Diagn Res. (2017) 11(8):PC13–6. doi: 10.7860/JCDR/2017/27982.10478
11. Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc. (2011) 25(9):2773–843. doi: 10.1007/S00464-011-1799-6
12. Barbosa CDA, Oliveira DC, De-Melo-Delgado NM, Mafra JGDA, Dos Santos RS, Moreira WC. Inguinodynia: review of predisposing factors and management. Rev Col Bras Cir. (2021) 47:1–7. doi: 10.1590/0100-6991E-20202607
13. Dias BG, Santos MPD, Chaves ABJ, Willis M, Gomes MC, Andrade FT, et al. Inguinodynia in patients submitted to conventional inguinal hernioplasty. Rev Col Bras Cir. (2017) 44(2):112–5. doi: 10.1590/0100-69912017002001
14. Reinpold W. Risk factors of chronic pain after inguinal hernia repair: a systematic review. Innov Surg Sci. (2017) 2(2):61–8. doi: 10.1515/ISS-2017-0017
15. Jeroukhimov I, Dykman D, Hershkovitz Y, Poluksht N, Nesterenko V, Yehuda AB, et al. Chronic pain following totally extra-peritoneal inguinal hernia repair: a randomized clinical trial comparing glue and absorbable tackers. Langenbecks Arch Surg. (2023) 408(1):190. doi: 10.1007/S00423-023-02932-2
16. Ibrahim SR, Ward PJ. Tissue adhesives for hernia mesh fixation: a literature review. Cureus. (2020) 12(9):e10494. doi: 10.7759/CUREUS.10494
17. Nizam S, Saxena N, Yelamanchi R, Sana S, Kardam D. Mesh fixation with fibrin glue versus tacker in laparoscopic totally extraperitoneal inguinal hernia repair. ANZ J Surg. (2021) 91(10):2086–90. doi: 10.1111/ANS.17165
18. Sajid MS, Ladwa N, Kalra L, McFall M, Baig MK, Sains P. A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg. (2013) 206(1):103–11. doi: 10.1016/J.AMJSURG.2012.09.003
19. Azevedo MA, Oliveira GBTD, Malheiros CA, Roll S. Are there differences in chronic pain after laparoscopic inguinal hernia repair using the transabdominal technique comparing with fixation of the mesh with staples, with glue or without fixation? A clinical randomized, double-blind trial. Arq Bras Cir Dig. (2022) 35:e1670. doi: 10.1590/0102-672020220002E1670
20. Hu N, Xie H, Wang DC, Lei YH, Wei J, Yu M, et al. Efficacy and safety of glue mesh fixation for laparoscopic inguinal hernia: a meta-analysis of randomized controlled trials. Asian J Surg. (2023) 46(9):3417–25. doi: 10.1016/J.ASJSUR.2023.03.146
21. Kanters S. Fixed- and random-effects models. Methods Mol Biol. (2022) 2345:41–65. doi: 10.1007/978-1-0716-1566-9_3
22. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. (2009) 339:b2700. doi: 10.1136/BMJ.B2700
23. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. doi: 10.1136/BMJ.L4898
24. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327(7414):557–60. doi: 10.1136/BMJ.327.7414.557
25. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14(1):135. doi: 10.1186/1471-2288-14-135
26. Lozada-Hernández EE, Mayagoitía-González JC, Smolinski-Kurek RL, Montiel-Hinojosa L, Hernández-Villegas L, Morales-Vargas JM, et al. Prevention of incisional hernia with a reinforced tension line (RTL) versus primary suture only in midline laparotomies: 3-year follow-up in a randomized clinical trial. Hernia. (2022) 26(2):447–56. doi: 10.1007/S10029-020-02338-9
27. Albertsmeier M, Hofmann A, Baumann P, Riedl S, Reisensohn C, Kewer JL, et al. Effects of the short-stitch technique for midline abdominal closure: short-term results from the randomised-controlled ESTOIH trial. Hernia. (2022) 26(1):87–95. doi: 10.1007/S10029-021-02410-Y
28. Yıldırım MB, Sahiner IT. The effect of mesh fixation on migration and postoperative pain in laparoscopic TEP repair: prospective randomized double-blinded controlled study. Hernia. (2023) 27(1):63–70. doi: 10.1007/S10029-022-02587-W
29. Thölix AM, Kössi J, Harju J. Postoperative pain and pain-related health-care contacts after open inguinal hernia repair with Adhesix™ and Progrip™: a randomized controlled trial. Hernia. (2022) 26(4):1095–104. doi: 10.1007/S10029-021-02549-8
30. Emral AC, Anadol AZ, Kozan R, Cetinkaya G, Altiner S, Aytac AB. Comparison of the results of using a self-adhesive mesh and a polypropylene mesh in open inguinal hernia repair: a prospective randomized controlled study. Pol Przegl Chir. (2022) 94(6):46–53. doi: 10.5604/01.3001.0015.7674
31. Qureshi S, Ghazanfar S, Leghari AA, Zubair M, Chisti S, Memon F, et al. A comparative follow up study of transabdominal preperitoneal mesh repair in inguinal hernias with or without mesh fixation. J Pak Med Assoc. (2021) 71(1(A)):28–30. doi: 10.47391/JPMA.827
32. Koch O, von Rahden BHA, Wykypiel H, Schoppmann SF, Függer R, Rosanelli G, et al. Planning and design of a prospective randomised multi-centre trial on the repair of large hiatal hernias with sutures vs. pledgeted sutures vs. absorbable mesh. Zentralbl Chir. (2021) 146(2):204–9. doi: 10.1055/A-1369-9694
33. Subwongcharoen S, Ruksakul K. A randomized controlled trial of staple fixation versus N-butyl-2-cyanoacrylate fixation in laparoscopic inguinal hernia repair. J Med Assoc Thai. (2013) 96(Suppl 3):8–13. https://europepmc.org/article/med/23682517
34. Cristaudo A, Nayak A, Martin S, Adib R, Martin I. A prospective randomised trial comparing mesh types and fixation in totally extraperitoneal inguinal hernia repairs. Int J Surg. (2015) 17:79–82. doi: 10.1016/J.IJSU.2015.03.018
35. Liew W, Wai YY, Kosai NR, Gendeh HS. Tackers versus glue mesh fixation: an objective assessment of postoperative acute and chronic pain using inflammatory markers. Hernia. (2017) 21(4):549–54. doi: 10.1007/S10029-017-1611-1
36. Boldo E, Armelles A, de Lucia GP, Martin F, Aracil JP, Miralles JM, et al. Pain after laparoscopic bilateral hernioplasty: early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc. (2008) 22(5):1206–9. doi: 10.1007/s00464-007-9587-z
37. Brügger L, Bloesch M, Ipaktchi R, Kurmann A, Candinas D, Beldi G. Objective hypoesthesia and pain after transabdominal preperitoneal hernioplasty: a prospective, randomized study comparing tissue adhesive versus spiral tacks. Surg Endosc. (2012) 26(4):1079–85. doi: 10.1007/S00464-011-2003-8
38. Bunkar SK, Verma K, Jhunjhunwala A, Singh A. A randomized controlled clinical trial of N-butyl cyanoacrylate glue fixation versus tacker fixation of mesh in endoscopic totally extraperitoneal hernia repair. Indian J Surg. (2021):1–6. doi: 10.1007/S12262-021-03118-0/METRICS
39. Chandra P, Phalgune D, Shah S. Comparison of the clinical outcome and complications in laparoscopic hernia repair of inguinal hernia with mesh fixation using fibrin glue vs tacker. Indian J Surg. (2016) 78(6):464–70. doi: 10.1007/S12262-015-1410-9
40. Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, et al. The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc. (2012) 26(1):249–54. doi: 10.1007/S00464-011-1862-3
41. Habeeb TAAM, Mokhtar MM, Sieda B, Osman G, Ibrahim A, Metwalli AM, et al. Changing the innate consensus about mesh fixation in trans-abdominal preperitoneal laparoscopic inguinal hernioplasty in adults: short and long term outcome. Randomized controlled clinical trial. Int J Surg. (2020) 83:117–24. doi: 10.1016/J.IJSU.2020.09.013
42. Issa M, Tacey M, Geraghty J, Das A, Dhir A, Mori K, et al. Cyanoacrylate glue versus absorbable tacks in mesh fixation for laparoscopic extraperitoneal inguinal hernia repair: a randomized controlled trial. Surg Laparosc Endosc Percutan Tech. (2021) 31(3):291–7. doi: 10.1097/SLE.0000000000000915
43. Lau H. Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg. (2005) 242(5):670–5. doi: 10.1097/01.SLA.0000186440.02977.DE
44. Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, et al. Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg. (2007) 245(2):222–31. doi: 10.1097/01.SLA.0000245832.59478.C6
45. Melissa CS, Bun TAY, Wing CK, Chung TY, Wai NEK, Tat LH. Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg. (2014) 259(3):432–7. doi: 10.1097/SLA.0B013E3182A6C513
46. Moreno-Egea A. Is it possible to eliminate sutures in open (Lichtenstein technique) and laparoscopic (totally extraperitoneal endoscopic) inguinal hernia repair? A randomized controlled trial with tissue adhesive (n-hexyl-α-cyanoacrylate). Surg Innov. (2014) 21(6):590–9. doi: 10.1177/1553350613517944
47. Olmi S, Scaini A, Erba L, Guaglio M, Croce E. Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery. (2007) 142(1):40–6. doi: 10.1016/J.SURG.2007.02.013
48. Tolver MA, Rosenberg J, Juul P, Bisgaard T. Randomized clinical trial of fibrin glue versus tacked fixation in laparoscopic groin hernia repair. Surg Endosc. (2013) 27(8):2727–33. doi: 10.1007/S00464-012-2766-6
49. Wasim K, Mela A, Hanief D, Mushtaq A, Imran S, Gilkar I. Comparative study of fibrin sealant versus use of tackers in inguinal hernia repair. Cukurova Med J. (2015) 40(3):457–65. doi: 10.17826/CUTF.08823
50. Ielpo B, Nuñez J, Ferri V, Silva J, Quijano Y, Vicente E, et al. Laparoscopic inguinal hernia repair: cost-effectiveness analysis of trend modifications of the technique. Updates Surg. (2021) 73(5):1945–53. doi: 10.1007/S13304-021-01005-7
51. Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. (2009) 13(4):343–403. doi: 10.1007/S10029-009-0529-7
52. HerniaSurge Group. International guidelines for groin hernia management. Hernia. (2018) 22(1):1–165. doi: 10.1007/S10029-017-1668-X
53. Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials. (2009) 10:37. doi: 10.1186/1745-6215-10-37
54. Nguyen DK, Amid PK, Chen DC. Groin pain after inguinal hernia repair. Adv Surg. (2016) 50(1):203–20. doi: 10.1016/J.YASU.2016.04.003
55. Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, et al. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc. (2012) 26(5):1269–78. doi: 10.1007/S00464-011-2025-2
56. Zeb MH, Pandian TK, El Khatib MM, Naik ND, Chandra A, Morris DS, et al. Risk factors for postoperative hematoma after inguinal hernia repair: an update. J Surg Res. (2016) 205(1):33–7. doi: 10.1016/J.JSS.2016.06.002
57. Habib Bedwani NAR, Kelada M, Smart N, Szydlo R, Patten DK, Bhargava A. Glue versus mechanical mesh fixation in laparoscopic inguinal hernia repair: meta-analysis and trial sequential analysis of randomized clinical trials. Br J Surg. (2021) 108(1):14–23. doi: 10.1093/BJS/ZNAA002
Keywords: inguinal hernia, laparoscopic herniorrhaphy, glue mesh fixation, tack mesh fixation, hernia
Citation: Raja S, Raja A, Ansari Z, Eman S, Bajaj S, Ahmed M, Kumar U, Shah YH, Jawahar S, Aftab F, Rajani D, Kumar S and Khatri M (2024) Safety and efficacy revisited: a systematic review and meta-analysis of glue versus tack mesh fixation in laparoscopic inguinal herniorrhaphy. Front. Surg. 11:1321325. doi: 10.3389/fsurg.2024.1321325
Received: 13 October 2023; Accepted: 22 January 2024;
Published: 9 February 2024.
Edited by:
Gabriel Sandblom, Karolinska Institutet (KI), SwedenReviewed by:
Juan Manuel Suárez-Grau, Virgen del Rocío University Hospital, SpainJacopo Andreuccetti, Civil Hospital of Brescia, Italy
Bengt Novik, Karolinska Institutet (KI), Sweden
© 2024 Raja, Raja, Ansari, Eman, Bajaj, Ahmed, Kumar, Shah, Jawahar, Aftab, Rajani, Kumar and Khatri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sandesh Raja c2FuZGVzaHJhamE3MEBnbWFpbC5jb20=
 Sandesh Raja
Sandesh Raja Adarsh Raja
Adarsh Raja Ziyan Ansari1
Ziyan Ansari1 Muhammad Ahmed
Muhammad Ahmed Yawar Hussain Shah
Yawar Hussain Shah Deepak Rajani
Deepak Rajani Satesh Kumar
Satesh Kumar Mahima Khatri
Mahima Khatri