- 1School of Health Science and Engineering, Shanghai University for Science and Technology, Shanghai, China
- 2Department of Orthopedics, Changzheng Hospital, Second Military Medical University, Shanghai, China
Objective: The aim of this study was to evaluate the efficacy of the pedicle screw-U rod system in treating double-level lumbar spondylolysis with or without spondylolisthesis.
Methods: A retrospective study was conducted. Twenty-six patients were included in this study and followed up at 3, 6, and 12 months. Patients without spondylolisthesis were treated with double U-shaped rods (group I), and patients with spondylolisthesis were treated with a lengthened U-shaped rod (group II). Japanese Orthopedic Association (JOA) scores, Oswestry disability index (ODI) scores, disc range of motion (ROM), intervertebral space height of fixed levels and adjacent levels, and grading the degeneration of adjacent segmental intervertebral discs were evaluated preoperatively and postoperatively.
Results: JOA and ODI scores improved significantly at 3 months both in groups I and II. The average bone grafting healing time was 6.1 ± 3.1 months for group I and 6 ± 2.8 months for group II. The intervertebral space heights of L4/L5 and L5/S1 were improved significantly at the final follow-up (p < 0.05 for both groups). Surgical segmental and adjacent segmental ROM had no significant change at the final follow-up, in comparison with data preoperatively (p > 0.05). No significant changes of intervertebral space height (L3/L4) and grading of intervertebral disc degeneration were noted before and after surgery (p = 0.141 and 0.484, respectively).
Conclusions: The pedicle screw-U rod system provided advantages of being easy in repairing symptomatic double-level lumbar spondylolysis. This technique improved disabilities of patients, preserved the lumbar spine ROM, and delayed the degeneration of adjacent segments.
Introduction
Spondylolysis is defined as an anatomic defect in vertebral pars interarticularis. Multiple-level lumbar spondylolysis is rare and accounts for approximately 0.3% among the general population and involves two levels, L4 and L5, in more than 60% (1, 2). Spondylolisthesis refers to anterior or posterior slipping of one segment of the spine on the next lower segment, with the most common cause being isthmic. Generally, conservative treatment is recommended for most symptomatic patients with spondylolysis and/or spondylolisthesis (3). However, if patients do not respond to conservative measures, surgical intervention is usually indicated.
Various techniques have been advocated for the surgical management of spondylolysis or isthmic spondylolisthesis. Among these procedures, direct repair of the pars defect stabilized with a construct consisting of a pair of pedicle screws connected by a U-shaped rod has several advantages in achieving excellent bone graft healing, preventing anterior displacement of the diseased segment, and maintaining intervertebral space height (4–6). However, double-level spondylolysis and isthmic spondylolisthesis are rare, and it is difficult to define an optimal treatment algorithm for these. In this study, we describe a retrospective study evaluating the efficacy of the U-shaped rod and screws system for the treatment of double-level lumbar spondylolysis and isthmic spondylolisthesis, and to our knowledge, there is no similar research in the literature.
Materials and methods
We retrospectively reviewed patients with double-level lumbar spondylolysis who were treated with a U-shaped rod and screws system at the Shanghai Changzheng Hospital between January 2014 and June 2016. This research was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Changzheng Hospital. Written informed consents were obtained from all participants or their guardians prior to the study. The major inclusion criteria were as follows: (1) patients had symptomatic double-level bilateral spondylolysis at L4 and L5 with or without spondylolisthesis at L4 (Grade I‒IV, Meyerding criteria) (7); (2) patients presented with severe low back pain, with or without numbness of lower limbs and sciatica; (3) Grade I to II disc changes at L3 to S1 (Pfirrmann criteria) (8); (4) patients who had been resistant to conservative treatment for at least 6 months.
Clinical evaluation
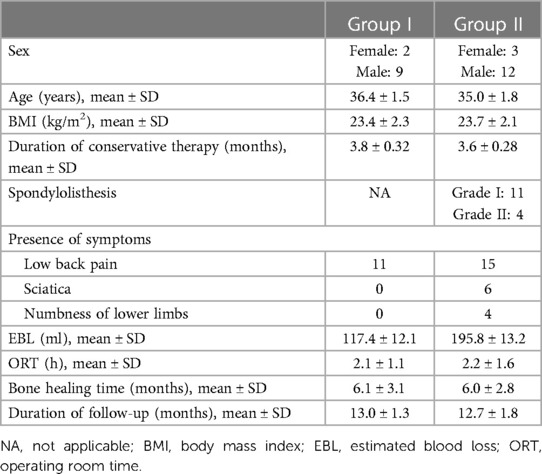
Patients were followed up at 3, 6, and 12 months. The Japanese Orthopedic Association (JOA) score and the Oswestry disability index (ODI) score were used to evaluate lumbar disability preoperatively, postoperatively, and at the last follow-up. Lumbar magnetic resonance imaging (MRI) scan was performed preoperatively for all patients to evaluate the degree of disc degeneration below and above the defect. The images were graded using the Pfirrmann grading system for the assessment of lumbar disc degeneration (8). Anteroposterior, lateral, and flexion–extension radiographs, and lumbar computed tomography (CT) scan were performed to evaluate intervertebral space height (Figure 1A), segmental range of motion (ROM) (Figures 1B,C), and bone graft healing time independently by two radiologists preoperatively and at follow-up. Bone fusion was considered to be achieved if (1) trabecular bony bridge was formed at isthmuses, (2) the contact surface between the preoperative low-density area and bone graft became indistinct, and (3) the “dog neck sign” was indistinct.
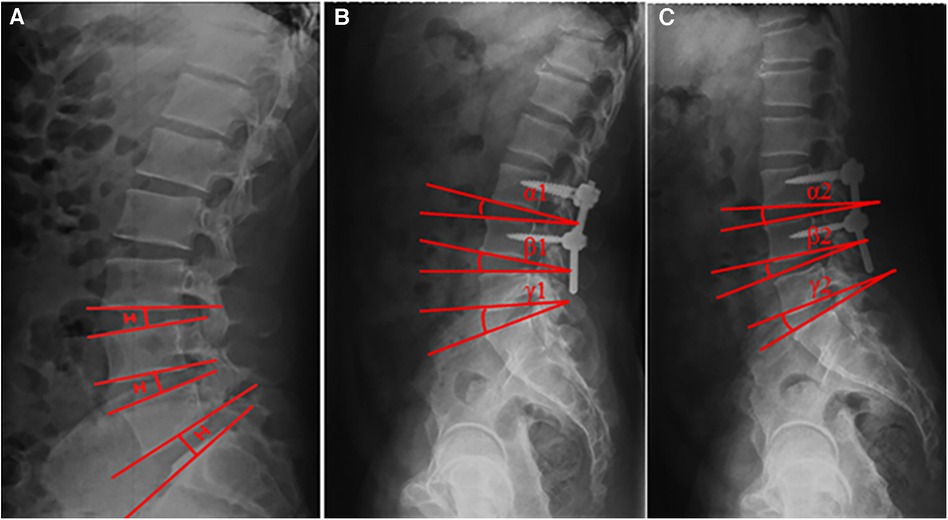
Figure 1. Measurement of intervertebral space height (A) and segmental ROM (B,C). The intervertebral space height (H) was determined by the distance between the midpoints of adjacent endplates of the vertebrae. Angles formed between the adjacent superior and inferior endplates were measured on flexion and extension images. The segmental ROM was determined by the difference between these two angles (i.e., α1–α2, β1–β2, and γ1–γ2).
Surgical procedure
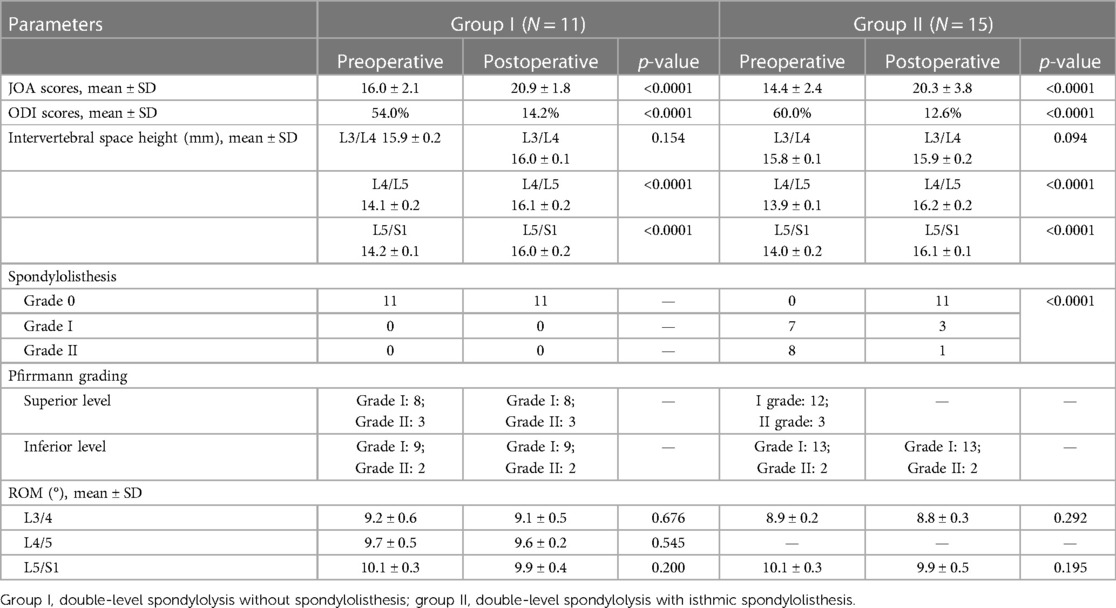
Double-level spondylolysis without spondylolisthesis (group I) (Figure 2): The procedure was similar to those reported previously (4–6). The defect in the L5 pars was exposed, and cancellous bone autograft harvested from the iliac crest was placed in the defect and impacted. A universal pedicle screw was inserted into the pedicle on each side at L5. After that, a U-shaped rod was placed under the L5 spinous process and pushed to lock onto the pedicle screws. In this way, the rod was firmly fixed against the spinous process and the laminae, which promotes compression of the graft in the defect and stabilizes the posterior arch. The process was repeated for the second lytic vertebrae.

Figure 2. Preoperative and postoperative images obtained in a 26-year-old male diagnosed with double-level lumbar spondylolysis. (A–C) Spondylolysis at L4 and L5. (D–F) Postoperative radiographs.
Double-level spondylolysis with spondylolisthesis (group II) (Figure 3): The defect in the L4 and L5 pars was exposed, and cancellous bone autograft harvested from the iliac crest was placed in the defect and impacted. A universal pedicle screw was inserted into the pedicle on each side at L4 and L5. Decompression was performed if necessary. A ring incision was made on one side of the L4/L5 annulus, and the disk material was removed with pituitary rongeurs. After removal of the disk, a U-shaped rod was placed under the L5 spinous process, and the arm of the rod was pushed to lock onto the pedicle screws and secured both sides. Finally, reduction was performed, and bone chips procured from the decompression was compressed into the disk space for bony fusion.
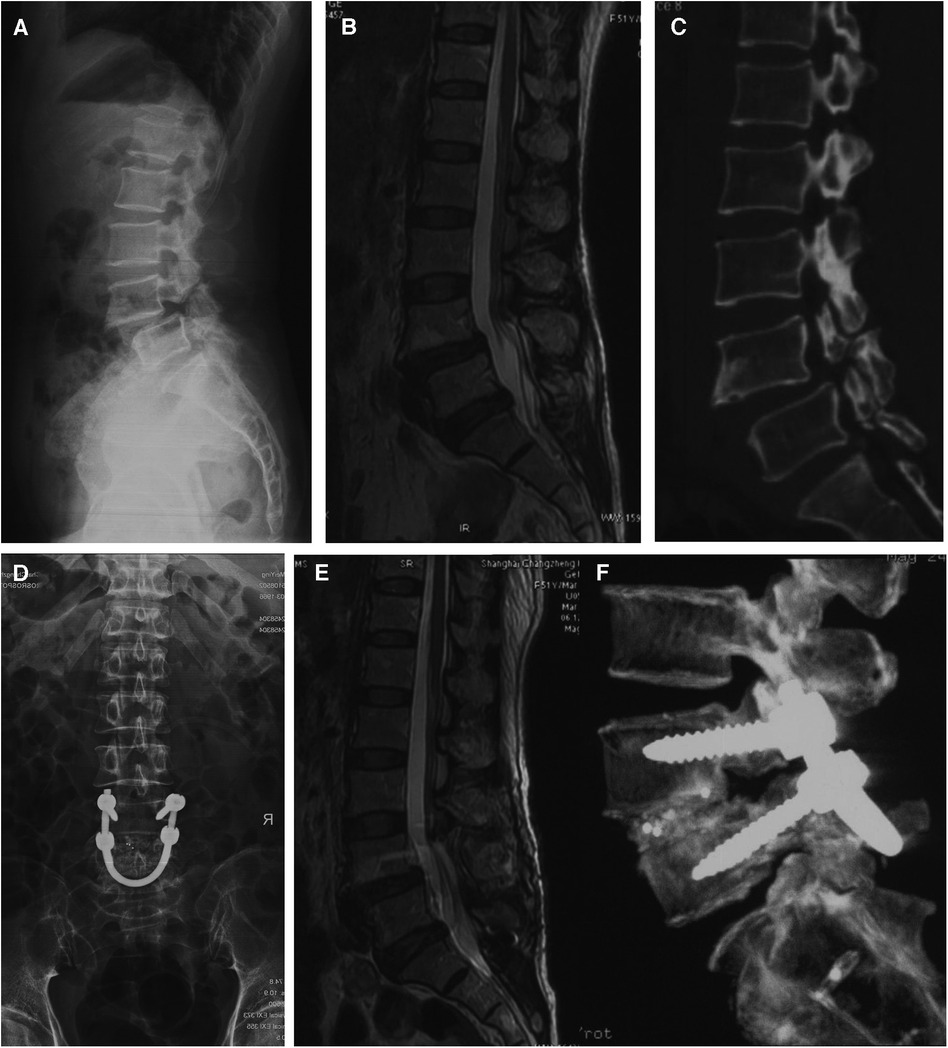
Figure 3. Preoperative and postoperative images obtained in a 51-year-old female diagnosed with double-level lumbar spondylolysis. (A–C) Spondylolysis at L4 and L5, and spondylolisthesis at L4. (D–F) Postoperative radiographs.
Statistical analysis
Statistical analysis was performed using the SPSS 19.0 software (SPSS Inc., Chicago, IL). Differences in radiological parameters between two time points were compared using Student's t-test and the Wilcoxon signed-rank test. A two-tailed p-value <0.05 was considered to be statistically significant.
Results
Twenty-six patients (21 men and 5 women) with double-level bilateral spondylolysis at L4 and L5 were eligible for the study. Their age ranged from 15 to 56 years, with an average of 35.7 years. Fifteen patients had Grade I or II spondylolisthesis at L4. Of the 26 patients, neurogenic symptoms were present in 10 patients, all of whom had spondylolisthesis. Patient demographic characteristics are shown in Table 1. No herniated lumbar disc was observed.
The patients were followed up for a mean duration of 12.9 ± 2.8 months. The JOA and ODI scores in both groups demonstrated statistically significant postoperative improvement. The mean JOA scores significantly improved from 16.0 ± 2.1 to 20.9 ± 1.8 in group I and from 14.4 ± 2.4 to 20.3 ± 3.8 in group II, respectively. Mean ODI scores improved significantly from 54% to 14.2% in group I and from 60% to 12.6% in group II (Figure 4). Sciatica and numbness of lower limbs improved effectively in the 10 patients. The average time of bone graft healing was 6.1 months in group I and 6.0 months in group II. Postoperative lumbar ROM had no significant differences with preoperative lumbar ROM at final follow-up in both groups (p > 0.05). The mean intervertebral space height of L4/L4 and L5/S1 levels increased from 14.1 ± 0.2 to 16.1 ± 0.2 mm and 14.2 ± 0.1 to 16.0 ± 0.2 mm (p < 0.001), respectively, after surgery in group I. The mean intervertebral space height of L4/L5 and L5/S1 levels changed from 13.9 ± 0.1 to 15.9 ± 0.2 mm and 14.0 ± 0.2 to 16.1 ± 0.1 mm mm (p < 0.001), respectively, in group II. The mean degree of listhesis (%) at the L4/L5 level in group II improved significantly at last follow-up (p < 0.0001) (Table 2). There were no signs of permanent nerve injury, breakage or loosening of the internal fixation, and other complications at the follow-up periods.
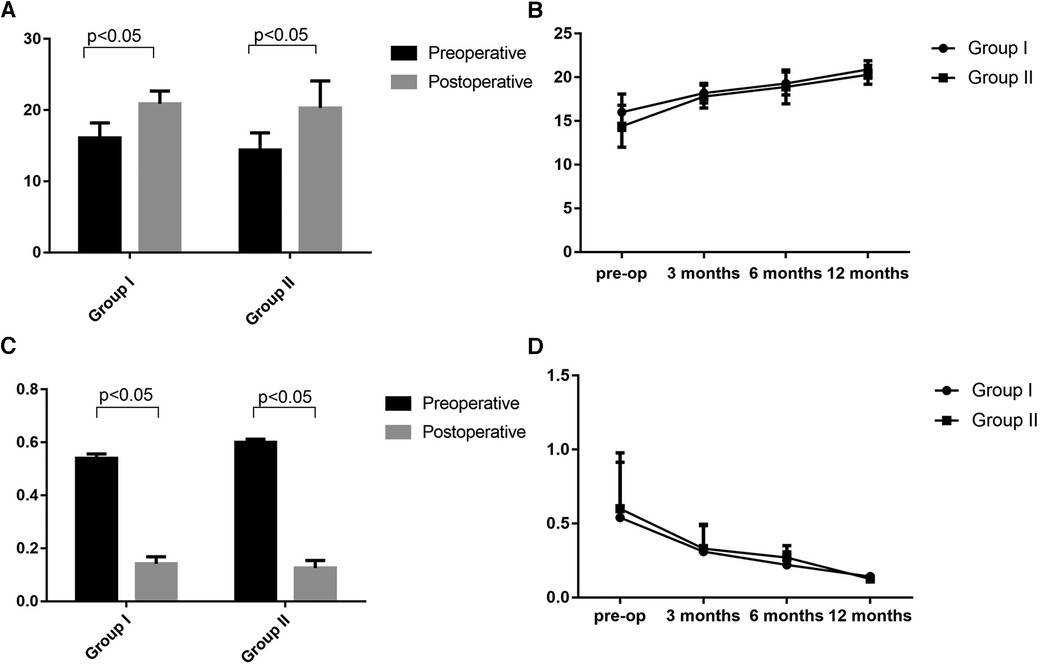
Figure 4. Preoperative and postoperative lumbar JOA (A,B) and ODI scores (C,D). Group I: double-level spondylolysis without spondylolisthesis. Group II: double-level spondylolysis with spondylolisthesis.
Discussion
The incidence of lumbar pars defect involving double levels is rare, with few reports of double-level lumbar spondylolysis in the literature. Double-level spondylolysis associated with spondylolisthesis is even rarer. The principle of double-level lumbar spondylolysis and spondylolisthesis treatment was the same as that for single-level spondylolisthesis (9). Direct pars defect repair with different kinds of internal fixation was adopted by different authors for treatment of symptomatic multiple-level lumbar spondylolysis (10–12), and they all achieved good results. However, these procedures had their own defects. A metal wire combined with bone grafting required prolonged immobilization with a lumbar brace, and a screw-hook combined with bone grafting was complicated and with a high risk of dura sac or nerves injury due to improperly positioned (13–16). Direct pars repair with the pedicle screw-U rod system is an alternative surgical procedure for multiple-level lumbar spondylolysis, providing stable fixation, excellent lumbar spine mobility, and improved JOA and ODI scores. In this study, we described the surgical outcome of 26 cases with double-level lumbar spondylolysis who were treated with the pedicle screw-U rod system.
It is reported that the incidence of multiple-level lumbar spondylolysis is higher in males (9, 17). Consistent with the trends reported in the literature, 21 of the 26 patients were male in our series. In this study, 15 had associated spondylolisthesis and most of them presented with neurogenic symptoms such as intermittent radiating leg pain and lower limb numbness. These patients underwent direct pars defect repair including placing the pedicle screws above and below the slip, securing the arms of the U rod at both sides following a posterior lumbar intervertebral fusion. For patients without spondylolisthesis, direct pars defect repair with the pedicle screw-U rod system was performed, just as reported previously (5). For these two groups, JOA and ODI scores improved significantly at the final follow-up postoperatively, and none of the patients complained of permanent low back pain, sciatica, or numbness of lower limbs. The rational for the pedicle screw-U rod system is to avoid the drawbacks of fusion, and the aim is to save a spinal motion segment to retain lumbar spine mobility and to restore normal anatomy. Ulibarri et al. evaluated the biomechanical property of the pedicle screw-U rod system in treating single-level spondylolysis and suggested that it provided excellent stability in interbody flexion–extension and torsion compared to the normal spine, which may be beneficial in maintaining adjacent-level motion and prevention of stress shielding (16). In the present study, there were no statistically significant differences in segmental lumbar ROM between preoperative and postoperative periods for both groups. Bone healing was achieved in all patients. These findings indicated that the pedicle screw-U rod system could effectively relieve the symptoms and provide rigid intrasegmental fixation with minimal intersegmental motion interference compared with traditional segmental fusion. Chen et al. showed similar results in treating single-level lumbar isthmic spondylolysis that there was no statistically significant difference in the ROM of the intervertebral disks before and after surgery (5).
Sairyo et al. conducted a three-dimensional finite element analysis, which demonstrated that lumbar spondylolysis increased disc stresses at the affected as well as cranial adjacent levels, and it might lead to disc degeneration at both levels, while direct pars defect repair could improve the biomechanical environment of diseased and adjacent intervertebral discs (18). In our study, increasing adjacent intervertebral degeneration was not observed in both groups at 12 months postoperatively. The surgical intervertebral space height was improved significantly (p < 0.05), and adjacent intervertebral space height had no differences (p > 0.05) before and after surgery. In the 15 patients with spondylolisthesis, there was no change in the spondylolisthesis grade at the latest follow-up. These findings showed that the pedicle screw-U rod system could provide enough force and stability to prevent a second slip of surgical segments and would not put extra burden on the intervertebral space discs both in surgical and adjacent segments.
The efficacy of direct pars defect repair in treating spondylolysis-associated spondylolisthesis still remains obscure. Mohi Eldin reported that direct pars defect repair was useful for fusion of the pars defect with a minimal degree of isthmic spondylolisthesis (19). Chen et al. (5) and Koptan et al. (20) both suggested that direct pars defect repair was applicable to spondylolysis with grade I spondylolisthesis. However, several authors thought that in cases with an isthmic slip of over 25%, the affected motion segment would not be biomechanically normal even after a successful bony healing of the pars defect. Liu et al. demonstrated that multiple lumbar spondylolysis with spondylolisthesis could not be treated by direct pars defect repair as this procedure achieved inadequate segmental stability (9). In the present research, we used the pedicle screw-U rod system to fix L4 and L5 spondylolysis with L4 spondylolisthesis, without considering the level of vertebral slip. A lengthened U-shaped rod was passed beneath the spinous process of L5 and was locked onto pedicle screws at L4 and L5. Intervertebral fusion was also performed at the L4/L5 level. The bone chips procured during posterior decompression were used as interbody grafts instead of a cage, which showed a similar result as in the literature (21). This procedure would effectively restore L4 to normal position and decrease the forward shear stress on L4. Although this procedure sacrificed the mobility of the L4/L5 segment, it preserved the mobility of L3/L4 and L5/S1 segments (p > 0.05, compared with preoperative mobility). At the latest follow-up, none of the patients had a second spondylolisthesis on L4, and the JOA and ODI scores improved significantly at 12 months postoperatively.
However, several limitations could not be ignored. First, this was a retrospective study conducted at a single institution, and the relative small sample size limited the power of our analysis. Second, no control groups were set, which might reduce the reliability of the research. Third, a mean of 12 months of follow-up might be a little short to evaluate the efficiency of the surgery.
Conclusion
The pedicle screw-U rod system provided significant improvements in directly repairing symptomatic double-level lumbar pars defects with or without spondylolisthesis. This technique showed improvements in low back pain, sciatica, and numbness of lower limbs in patients with spondylolysis and spondylolisthesis. It could also preserve the ROM of lumbar spine and would not aggravate the degeneration of adjacent segments.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Changzheng Hospital, Second Military Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JJ: Data curation, Writing – original draft. TL: Methodology, Writing – original draft. XC: Data curation. RG: Writing – review & editing. XZ: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This research was supported by the National Natural Science Foundation of China (grant no. 82372434) and the “Deep Blue” Talent Project (grant no. SL27).
Acknowledgments
We would like to thank all the patients who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sakai T, Sairyo K, Takao S, Nishitani H, Yasui N. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine. (2009) 34:2346–50. doi: 10.1097/BRS.0b013e3181b4abbe
2. Stewart TD. The age incidence of neural-arch defects in Alaskan natives, considered from the standpoint of etiology. J Bone Joint Surg Am. (1953) 35-A:937–50. doi: 10.2106/00004623-195335040-00012
3. McNeely ML, Torrance G, Magee DJ. A systematic review of physiotherapy for spondylolysis and spondylolisthesis. Man Ther. (2003) 8:80–91. doi: 10.1016/S1356-689X(02)00066-8
4. Altaf F, Osei NA, Garrido E, Al-Mukhtar M, Natali C, Sivaraman A, et al. Repair of spondylolysis using compression with a modular link and screws. J Bone Joint Surg Br. (2011) 93:73–7. doi: 10.1302/0301-620X.93B1.24732
5. Chen XS, Zhou SY, Jia LS, Gu XM, Fang L, Zhu W. A universal pedicle screw and V-rod system for lumbar isthmic spondylolysis: a retrospective analysis of 21 cases. PLoS One. (2013) 8:e63713. doi: 10.1371/journal.pone.0063713
6. Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine. (1999) 24:1252–6. doi: 10.1097/00007632-199906150-00014
8. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. (2001) 26:1873–8. doi: 10.1097/00007632-200109010-00011
9. Liu X, Wang L, Yuan S, Tian Y, Zheng Y, Li J. Multiple-level lumbar spondylolysis and spondylolisthesis. J Neurosurg Spine. (2015) 22:283–7. doi: 10.3171/2014.10.SPINE14415
10. Ogawa H, Nishimoto H, Hosoe H, Suzuki N, Kanamori Y, Shimizu K. Clinical outcome after segmental wire fixation and bone grafting for repair of the defects in multiple level lumbar spondylolysis. J Spinal Disord Tech. (2007) 20:521–5. doi: 10.1097/BSD.0b013e3180335c1f
11. Chung CH, Chiu HM, Wang SJ, Hsu SY, Wei YS. Direct repair of multiple levels lumbar spondylolysis by pedicle screw laminar hook and bone grafting: clinical, CT, and MRI-assessed study. J Spinal Disord Tech. (2007) 20:399–402. doi: 10.1097/01.bsd.0000211253.67576.90
12. Eingorn D, Pizzutillo PD. Pars interarticularis fusion of multiple levels of lumbar spondylolysis. A case report. Spine. (1985) 10:250–2. doi: 10.1097/00007632-198504000-00010
13. Karatas AF, Dede O, Atanda AA, Holmes LJ, Rogers K, Gabos P, et al. Comparison of direct pars repair techniques of spondylolysis in pediatric and adolescent patients: pars compression screw versus pedicle screw-rod-hook. Clin Spine Surg. (2016) 29:272–80. doi: 10.1097/BSD.0b013e318277cb7d
14. Schlenzka D, Seitsalo S, Poussa M, Osterman K. Operative treatment of symptomatic lumbar spondylolysis and mild isthmic spondylolisthesis in young patients: direct repair of the defect or segmental spinal fusion? Eur Spine J. (1993) 2:104–12. doi: 10.1007/BF00302712
15. Schlenzka D, Remes V, Helenius I, Tommi L, Pekka T, Timo Y, et al. Direct repair for treatment of symptomatic spondylolysis and low-grade isthmic spondylolisthesis in young patients: no benefit in comparison to segmental fusion after a mean follow-up of 14.8 years. Eur Spine J. (2006) 15:1437–47. doi: 10.1007/s00586-006-0072-5
16. Ulibarri JA, Anderson PA, Escarcega T, Mann D, Noonan KJ. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine. (2006) 31:2067–72. doi: 10.1097/01.brs.0000231777.24270.2b
17. Wiltse LL, Widell EH Jr., Jackson DW. Fatigue fracture: the basic lesion is inthmic spondylolisthesis. J Bone Joint Surg Am. (1975) 57:17–22. doi: 10.2106/00004623-197557010-00003
18. Sairyo K, Goel VK, Faizan A, Vadapalli S, Biyani S, Ebraheim N. Buck’s direct repair of lumbar spondylolysis restores disc stresses at the involved and adjacent levels. Clin Biomech. (2006) 21:1020–6. doi: 10.1016/j.clinbiomech.2006.06.011
19. Mohi Eldin M. Minimal access direct spondylolysis repair using a pedicle screw-rod system: a case series. J Med Case Rep. (2012) 6:396. doi: 10.1186/1752-1947-6-396
20. Koptan WM, ElMiligui YH, ElSharkawi MM. Direct repair of spondylolysis presenting after correction of adolescent idiopathic scoliosis. Spine J. (2011) 11:133–8. doi: 10.1016/j.spinee.2011.01.012
Keywords: pedicle screw-U rod system, range of motion, spondylolisthesis, spondylolysis, health-related quality of life
Citation: Jiang J, Lin T, Chen X, Gao R and Zhou X (2024) Using the pedicle screw-U rod system for the treatment of double-level lumbar spondylolysis and isthmic spondylolisthesis. Front. Surg. 11:1308389. doi: 10.3389/fsurg.2024.1308389
Received: 6 October 2023; Accepted: 18 January 2024;
Published: 2 February 2024.
Edited by:
Baogan Peng, The Third Medical Center of People’s Liberation Army General Hospital, ChinaReviewed by:
Osvaldo Mazza, Bambino Gesù Children’s Hospital (IRCCS), ItalyIoannis Siasios, Papageorgiou General Hospital, Greece
© 2024 Jiang, Lin, Chen, Gao and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuhui Zhou eGh6aG91c3BpbmVAMTYzLmNvbQ== Rui Gao cmdhb3NwaW5lQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Jinghao Jiang1,2,†
Jinghao Jiang1,2,† Xuhui Zhou
Xuhui Zhou