- 1Department of Orthopaedics and Traumatology, Fondazione Policlinico Universitario A. Gemelli IRCCS-Università Cattolica del Sacro Cuore, Rome, Italy
- 2Department of Clinical Science and Translational Medicine, Section of Orthopaedics and Traumatology, University of Rome “Tor Vergata”, Rome, Italy
- 3Department of Orthopaedic Surgery (DICHIRONS), University of Palermo, Palermo, Italy
Objective: Unstable fractures of the sacrum often occur in patients with pelvic fractures and represent a real challenge for the orthopedic surgeon. Triangular osteosynthesis (TOS) and lumbopelvic fixation (LP) may represent a valid management option for the treatment of this condition. We present a systematic literature review about lumbopelvic fixation and triangular fixation as treatment option for unstable sacral fractures, to assess clinical and radiological outcomes after surgery and to evaluate appropriate indications and impact on the natural history of sacral fractures.
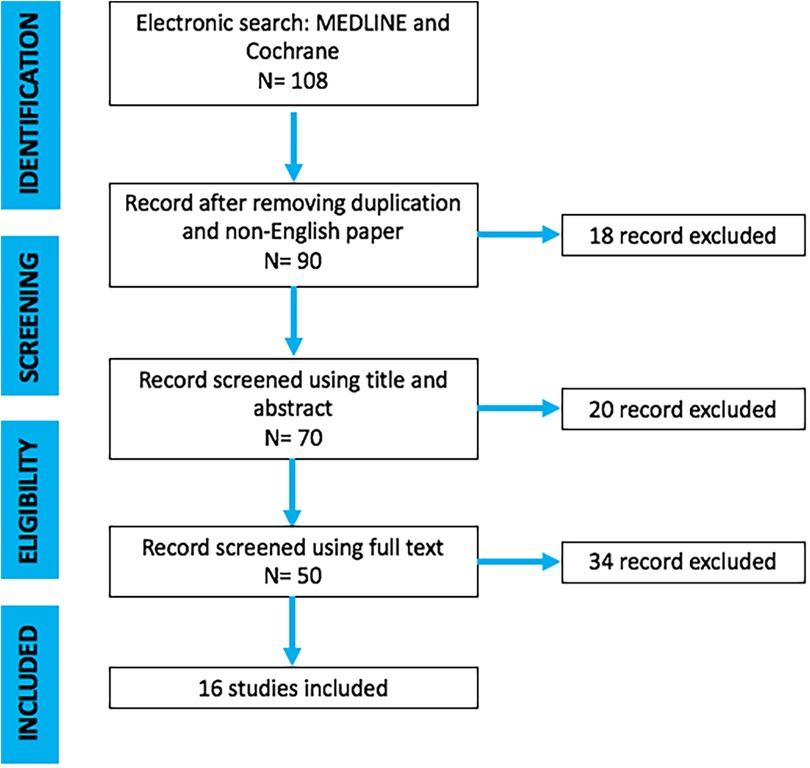
Methods: The review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 50 articles out of 108 titles, were considered eligible for the full-text analysis. Finally, 16 studies that met inclusion criteria were included in this review.
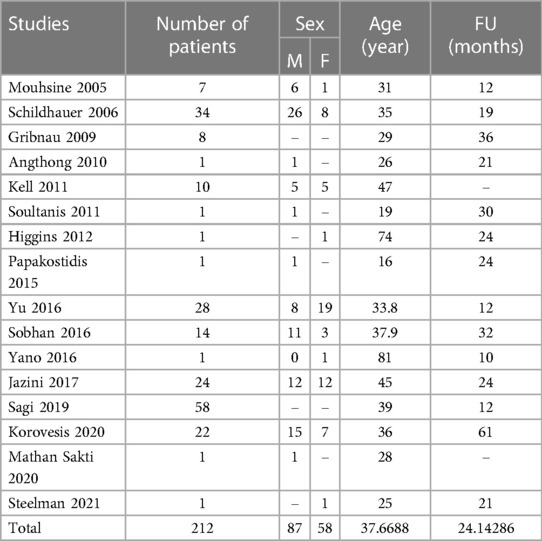
Results: Overall, 212 patients (87 males, 58 females) with sacral fractures treated with TOS triangular fixation or LP lumbopelvic fixation were collected. The mean age was 37.6 years. Mean follow-up reported in all studies was 24.14 months.
Conclusion: The results presented by the different authors, highlight the effectiveness of TOS triangular fixation and LP lumbopelvic fixation for the treatment of unstable sacral fractures associated with other pelvic fractures, in terms of function, stability, cost-effectiveness, and quality of life postoperatively.
Background
Unstable fractures of the sacrum often occur in patients with pelvic fractures (1), determining a real challenge for orthopedic surgeons, due to high rates of secondary dislocation (up to 15%), mostly caused by lesions with an associated vertical instability (2). Among usual surgical treatment taken into account facing those fractures, there are iliosacral screw fixation and posterior plate as tension band osteosynthesis, but none of them can adequately prevent potential vertical displacement (3). To better deal with vertical instability, Käch and Trentz (4) in 1,994 proposed for the first time the lumbopelvic fixation as surgical option in pelvic fractures involving the sacrum, specifically those lesions described as Vertical Shear according to Young and Burgess classification (5). The surgical technique was then developed and improved during the years, undergoing a deep revisitation through the original idea from Schildauer et al. to add to the lumbopelvic fixation an ileo-sacral screw, in the so-called “Triangular osteosynthesis” (6, 7). Since then, lumbopelvic fixation and its variant, triangular fixation, became the gold standard in those cases where sacral fractures are associated to neurological deficits, persistent instability, vertical sacral fractures, lower bone quality or non-union (8–11).
The aim of this review is to analyze the available studies in the literature about lumbopelvic and triangular fixation, and assess clinical and radiological outcomes of the patients treated through those techniques, to better evaluate appropriate indications and impact on the natural history of the sacral fractures.
Methods
Study setting and design
The present investigation represents a systematic literature review reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1).
Review questions
The review questions were formulated following the PICO scheme population (P), intervention (I), comparison (C), and outcome (O) as follows:
• Do patients suffering from posterior pelvic ring lesions report better clinical outcomes in term of complete healing rate (O), when treated through TOS (Triangular osteosynthesis) or LP (lumbopelvic) (I) in comparison to other techniques (C)?
Inclusion and exclusion criteria
In this review we considered the studies published as full-text articles in indexed journals, which investigated the value of TOS and LP for the management of sacral fracture (Figure 2). Only articles written in English with available abstract were included. No publication date limits were set. Surgical technique reports, expert opinions, letter to the editor, studies on animals, unpublished reports, cadaver or in vitro investigations, review of the literature, abstracts from scientific meetings and book chapters were excluded from the present review.

Figure 2. In our traumatology department, lumbopelvic fixation (LPF) involves placing pedicular screws in L5, sometimes L4, and bilaterally in the iliac bone, connecting them with rods on each side. The procedure can be performed in an open or closed manner, depending on the surgeon's skills and the patient's needs. To enrich LPF, a 6.5 or 7.3 cannulated screw can be added, positioned in the body of S1 or S2, in which case it is referred to as Triangular Osteosynthesis (TOS). Patients is placed prone on radiolucent surgical table, and the whole procedure is performed using intra-operative image intensifier.
Search strategy and study selection
Scopus, Cochrane Library, MEDLINE via PubMed and Embase were searched using the keywords: “vertical shear”, “pelvic ring fracture”, “Pelvic ring posterior fracture”, “vertically unstable pelvic injuries”, “lumbopelvic”, “spinopelvic”, “percutaneous lumbopelvic”, “triangular osteosynthesis” and their MeSH terms in any possible combination. The reference lists of relevant studies were screened to identify other studies of interest. The search was reiterated until December 31, 2022.
Data extraction and analysis
Two independent reviewers collected the data from the included studies. Any discordances were solved by consensus with a third author. For each study included in the present analysis, the following data were extracted: Year, Types of Research Studies, demographic features, sex, age, diagnosis, previous hip surgery, pathogens, treatment performed, possible complications and outcomes, and follow-up. Numbers software (Apple Inc., Cupertino, CA) was used to tabulate the obtained data. Categorical variables are presented as frequency and percentages. Continuous variables are presented as means and standard deviation. Only one decimal digit was reported and was rounded up.
Results
Descriptive data are given in (Figure 1). After screening 108 articles by title and abstract, 50 were considered eligible for the full-text analysis. 58 articles were excluded because they did not fulfill inclusion criteria. Finally, 16 studies (Tables 1–3) that met the inclusion criteria were included in this review (Figure 1). All these studies had a retrospective and case report descriptive design.
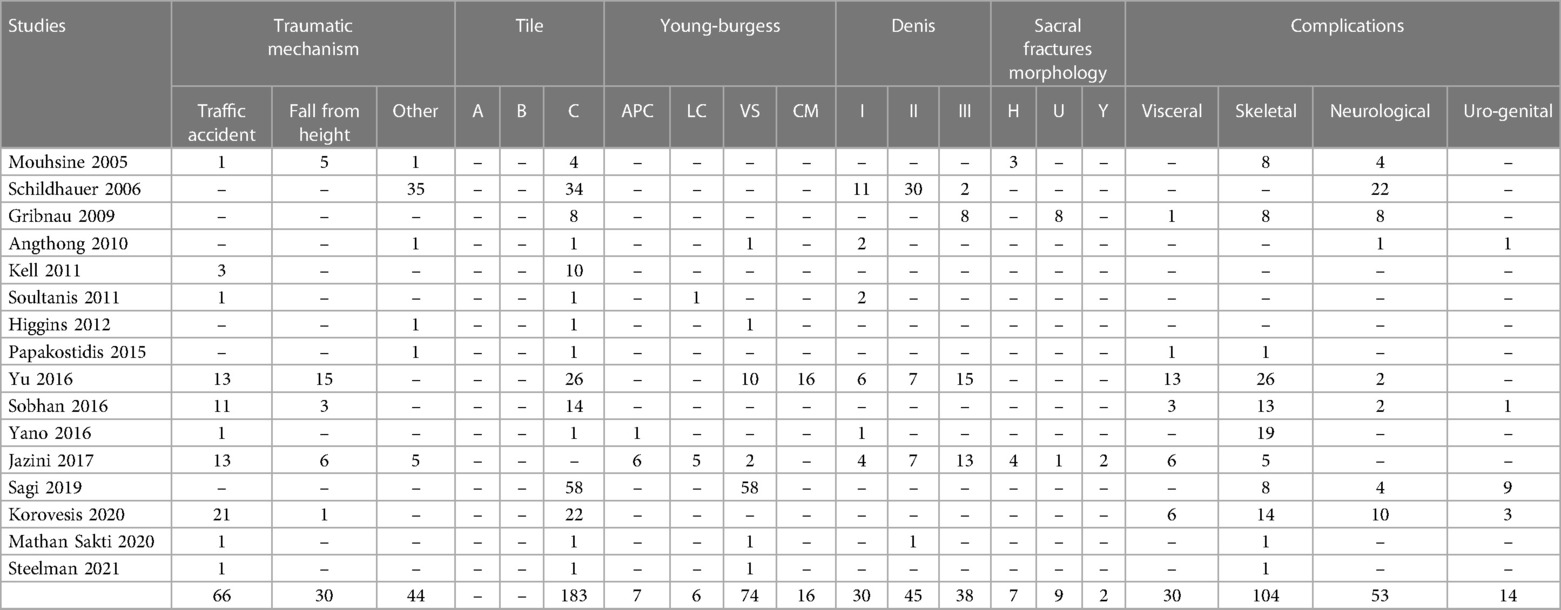
Overall, 212 patients (87 males, 58 females) suffering from pelvic fractures were collected. The mean age was 37.3 years. Mean follow-up, reported in all studies, was 24.7 months (Table 1). The causes of injury consisted in traffic accidents—most common mechanism of injury—(66 cases) followed by falls from height (30 cases) and others (44 cases) (Tables 2, 3).
The most common type of fracture was the Tile C reported in 183 patients (Table 2).
According to the Young-Burgess classification for pelvic ring injuries, 7 patients were identified as Anterior-Posterior Compression (APC), 6 with Lateral Compression (LC), 74 with Vertical Shear (VS) and 16 with Combined Mechanism (CM) (Table 2).
As regards sacral fractures, according to the Denis classification: 30 patients had a zone one I fracture; 45 had a zone II and 38 had a zone III (Table 2).
In terms of sacral fractures morphology, 7 were H-Type; 9 U-type; 2 Y-type (Table 2).
All patients had associated injuries (Table 2): 30 had also visceral lesions, among these 14 reported iliac artery bleeding, 6 severe pulmonary injuries. Among them were recorded: one bilateral pulmonary contusion, two unilateral pulmonary contusions, one bilateral pneumothorax, one unilateral pneumothorax, and one unilateral lung laceration. Other lesions were not specified. There were also 104 reported musculoskeletal associated injuries. The most common skeletal injury was lumbar lesion with 44 patients, and among these 3 had lumbar burst fractures, 2 were L5-S1 fracture dislocations, 39 had concomitant lumbar vertebral fractures and the others were not specified. Neurological associated injuries were reported in 53 patients, 4 with a pre-operative perineal neurological impairment, 4 had alterations of bladder and intestinal function, 3 developed sensorial impairment due to a complete cauda syndrome and 1 only partial cauda syndrome, 26 patients developed neurological non specified symptoms, 22 patients had non specified neurological deficit, 4 had lumbosacral plexus injuries and 10 patients had nerve root deficit; at last 14 patients reported bladder injuries (Table 2).
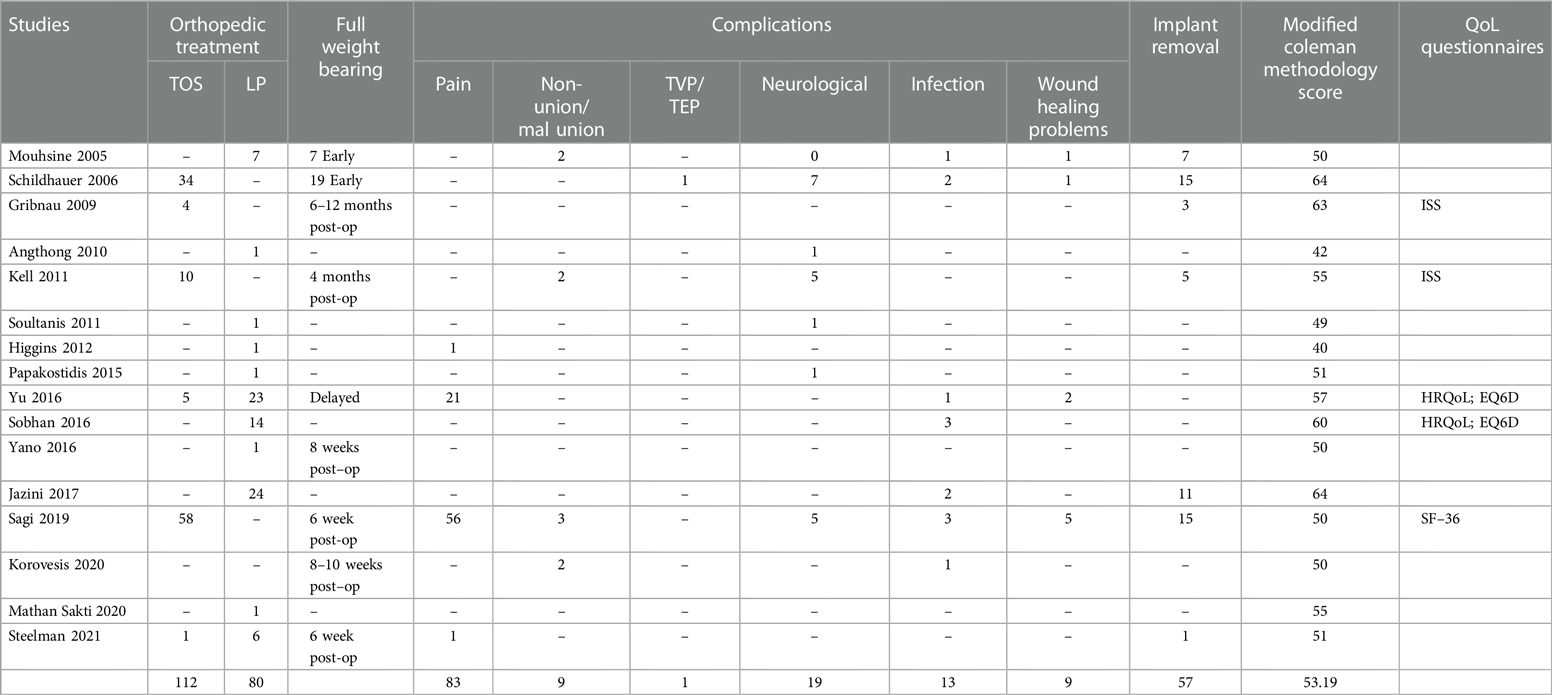
As regards the types of surgery, 112 were treated with TOS (Triangular Osteosynthesis), 101 underwent L5 to ilium fixation, 9 patients had also L4 involved in the fixation. 2 had fixation from L3 to L4 and ilium and for the other patients the treatment was not specified; 80 patients were treated with LP (Lumbopelvic) osteosynthesis, the other 23 patients were treated with other surgical techniques not relevant for this article (Table 3).
Weight bearing was described (Table 3) by many of the papers taken into account, and according to them an early weight bearing was achieved in 40 patients (21 treated with LP and 19 with TOS), between 30 days and 3 months a full weight bearing was reached by 64 patients (7 LP and 57 TOS). Ten patients (TOS) started full weight-bearing in 4 months, 4 patients in 6–12 months (12). Weight bearing was simply described as delayed in 28 patients (5 TOS and 23 LP), in 24 no weight bearing restrictions were reported (LP). Five studies do not report weight bearing data.
Post-operative complications were reported, especially infections and chronic pain (Table 3). The most common was pain due to the hardware, this was observed in 83 patients (62 treated with TOS and 21 with LP); non-union or malunion were observed in 9 patients; one patient reported TVP (13); 19 patients had neurological complications (among them, 2 drop foot, 2 radicular impingement, 1 cauda equina syndrome); 13 patients experienced wound infection (treated with debridement, antibiotics and in some cases with removal of the hardware) wound healing problems were reported in 9 cases.
In 57 patients implant removal was necessary to deal with the complications, 18 were treated with TOS and 44 with LP.
In 7 studies the authors used function questionnaires to evaluate outcome. Two studies used the injury severity score (ISS), 2 the Majed score, 2 the HRQoL (Health Related Quality of Life), 1 the SF36V2, 1 the SMFA and 1 the Matta criteria.
The Modified Coleman Methodology Score (mCMS) was used to evaluate the quality of studies, with a mean score for all studies of 53.18.
Discussion
Our review confirms the heterogeneity of the data in the existing literature in terms of surgical management for unstable lumbosacral fractures (12–27).
Sacral fracture resulting in spinopelvic dissociation with neurological damage are high-energy injuries that occur rarely in polytrauma patients (The infrequency of these cases, the severity of the associated injuries and the absence of an accepted management flowchart make them highly morbid. If left untreated either intentionally or through misdiagnosis, progressive neurological dysfunction or painful deformity may occur (28, 29).
Misdiagnosis is frequent especially on plain radiographs, owing to the complexity of pelvic ring imaging, where the sacrum inclination and the overlaying bowel gas make the identification of the fracture very difficult. For this reason, multiplanar CT scan with 3D reconstructions is necessary for a correct and precise diagnosis of these unstable fractures and for the identification of associated injuries (13, 15, 30, 31).
Conservative treatment is discouraged while open reduction external fixation has proved to be a valid surgical option with good outcome (31–33).
The main role of surgery for the treatment of posterior pelvic ring lesions includes pelvic ring reconstruction, lumbopelvic stability restoration, fracture displacement prevention and correction to improve neurological deficiency. Even when treated correctly, with restoring of the spinopelvic stability and fracture consolidation, patients who have suffered this type of injury may develop sequelae from the injury itself or from the type of treatment. According to the literature, less than 50% of patients who have suffered complex sacral fractures return to their previous working conditions and functionality (34).
The 6 studies using TOS fixation (12, 13, 15, 20, 24) showed that this is a reliable form of fixation that allows early full weight-bearing while preventing loss of reduction and it's mostly recommended for comminuted vertical shear trans-foraminal sacral fractures (24). This surgical technique guarantees pelvic stability by combining indirect lumbopelvic fixation and direct screw fixation of the sacral fracture. Compared to direct fixation TOS may avoid excessive exposure, additional bleeding, and extra operation. However, some complications such as L5-S1 facet joint distraction with the need for a second surgery, and iatrogenic nerve injury, have been described in 3 of the 5 studies (12, 13, 24). Two studies (15, 27) did not report neither malunion nor nerve impairment after surgery. The main limitation of TOS technique is that it requires a highly skilled surgeon specialized in the treatment of pelvic ring fractures as it is a very complicated procedure (35, 36).
The 11 authors that used LP fixation (14, 16–26) showed that spinopelvic fixation is a good technique for sacral fractures with lumbopelvic dissociation, as it allows immediate mobilization, as well as weight bearing in the postoperative period (29). Pain, neurological impairment and infection rates were low, and mobilization was earlier. The benefits of minimally invasive LPF, however, may come with increased elective reoperations for removal of instrumentation. The main limitation of lumbopelvic fixation is that it cannot correct directly the sacral fracture leading in many cases to malunion or non -union.
In conclusion, lumbopelvic instable fractures include many severe injuries and are difficult to fix with a good outcome. LP and TOS have in many cases, showed satisfactory clinical outcomes in the treatment of LPF.
This study has some limitations. First, most of the studies included in the analysis were retrospective case series with no comparative group; unfortunately, no higher quality studies have been performed on the subject due to its high complexity; in fact, it is not possible to perform randomized clin- ical trials or double-blind controlled studies. Second, there is variability in age groups and also follow-up. Third, there is a lack of homogeneity in reporting fracture classification, evaluation scales, treatment, and outcomes.
Conclusion
More accurate studies and stronger evidence are needed in order to address LP and TOS as gold standards in pelvic lesions involving posterior pelvic ring. However, actual findings in Literature suggest a good clinical and radiographic recovery through these surgical technique in the treatment of those fractures, especially when lumbar fracture are associated to the pelvic lesion, with a relative earlier weight bearing.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
GR: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DD: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RD: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. PF: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LC: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GM: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FL: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tile M. Fractures of the pelvis. In: Schröder G, editor. The Rationale of Operative Fracture Care. Berlin: Springer (1987). p. 239–90.
2. Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. (2003) 17:399–405. doi: 10.1097/00005131-200307000-00001
3. Dudda M, Hofmann M, Schildhauer TA. Sakrumfrakturen und lumbopelvine instabilitäten bei beckenringverletzungen. Unfallchirurg. (2013) 116:972–8. doi: 10.1007/s00113-012-2335-4
4. Kaech K, Trenz O. Distraction spondylodesis of the sacrum in “vertical shear lesions” of the pelvis. Unfallchirurg. (1994) 97:28–38.8153638
5. Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. (1986) 160(2):445–51. doi: 10.1148/radiology.160.2.3726125
6. Josten C, Schildhauer TA, Muhr G. Therapy of unstable sacrum fractures in pelvic ring. Results of of osteosynthesis with early mobilization. Chirurg. (1994) 65:970–5.7821078
7. Perna A, Proietti L, Smakaj A, Velluto C, Meluzio MC, Rovere G, et al. The role of femoral obliquity angle and T1 pelvic angle in predicting quality of life after spinal surgery in adult spinal deformities. BMC Musculoskelet Disord. (2021) 22(Suppl 2):999. doi: 10.1186/s12891-021-04823-3
8. Hoffmann MF, Dudda M, Schildhauer TA. Unilaterale trianguläre lumbopelvine stabilisierung: indikationen und technik [Unilateral triangular lumbopelvic stabilization: indications and techniques]. Unfallchirurg. (2013) 116(11):985–90. doi: 10.1007/s00113-012-2337-2
9. Rovere G, Fusco A, Smakaj A, De Mauro D, De Vitis R, Padua L, et al. Preliminary data on the neurophysiological evaluation of male sexual dysfunction in patients with pelvic ring fractures: a multicenter retrospective study. Eur Rev Med Pharmacol Sci. (2023) 27(8):3457–66. doi: 10.26355/eurrev_202304_32116
10. Rovere G, Perna A, Meccariello L, De Mauro D, Smimmo A, Proietti L, et al. Epidemiology and aetiology of male and female sexual dysfunctions related to pelvic ring injuries: a systematic review. Int Orthop. (2021) 45(10):2687–97. doi: 10.1007/s00264-021-05153-8
11. Smakaj A, De Mauro D, Rovere G, Pietramala S, Maccauro G, Parolini O, et al. Clinical application of adipose derived stem cells for the treatment of aseptic non-unions: current stage and future perspectives-systematic review. Int J Mol Sci. (2022) 23(6):3057. doi: 10.3390/ijms23063057
12. Keel MJ, Benneker LM, Siebenrock KA, Bastian JD. Less invasive lumbopelvic stabilization of posterior pelvic ring instability: technique and preliminary results. J Trauma. (2011) 71(3):E62–70. doi: 10.1097/TA.0b013e3182092e66
13. Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. (2006) 20(1 Suppl):S44–51. doi: 10.1097/01.bot.0000202392.24999.7c
14. Mouhsine E, Wettstein M, Schizas C, Borens O, Blanc CH, Leyvraz PF, et al. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J. (2006) 15(6):857–63. doi: 10.1007/s00586-004-0858-2
15. Gribnau AJ, van Hensbroek PB, Haverlag R, Ponsen KJ, Been HD, Goslings JC. U-shaped sacral fractures: surgical treatment and quality of life. Injury. (2009) 40(10):1040–8. doi: 10.1016/j.injury.2008.11.027
16. Angthong C, Wunnasinthop S, Sanpakit S. Complex lumbosacral fracture-dislocation with pelvic ring disruption and vertical shear sacral fracture: a case report of late presentation and review of the literature. Ulus Travma Acil Cerrahi Derg. (2010) 16(6):561–6.21153953
17. Soultanis K, Karaliotas GI, Mastrokalos D, Sakellariou VI, Starantzis KA, Soucacos PN. Lumbopelvic fracture-dislocation combined with unstable pelvic ring injury: one stage stabilisation with spinal instrumentation. Injury. (2011) 42(10):1179–83. doi: 10.1016/j.injury.2010.06.002
18. Higgins TF, Rothberg DL, Daubs MD. Spinopelvic dissociation as a complication of iliac crest bone graft harvest using an acetabular reamer. J Spinal Disord Tech. (2012) 25(6):345–9. doi: 10.1097/BSD.0b013e3182204d73
19. Papakostidis C, Harwood P, Dimitriou R, Dunsmuir R, Millner P, Giannoudis PV. Unique combination of lumbosacral junction injury with open pelvic ring disruption and acetabulum fracture: case report. Spine (Phila Pa 1976). (2005) 30(16):E477–80. doi: 10.1097/01.brs.0000174280.85073.ca
20. Yu YH, Lu ML, Tseng IC, Su CY, Hsu YH, Yeh WL, et al. Effect of the subcutaneous route for iliac screw insertion in lumbopelvic fixation for vertical unstable sacral fractures on the infection rate: a retrospective case series. Injury. (2016) 47(10):2212–7. doi: 10.1016/j.injury.2016.06.021
21. Sobhan MR, Abrisham SM, Vakili M, Shirdel S. Spinopelvic fixation of sacroiliac joint fractures and fracture-dislocations: a clinical 8 years follow-up study. Arch Bone Jt Surg. (2016) 4(4):381–6.27847854
22. Yano S, Aoki Y, Watanabe A, Nakajima T, Takazawa M, Hirasawa H, et al. Less invasive lumbopelvic fixation technique using a percutaneous pedicle screw system for unstable pelvic ring fracture in a patient with severe multiple traumas. J Neurosurg Spine. (2017) 26(2):203–7. doi: 10.3171/2016.7.SPINE16323
23. Jazini E, Weir T, Nwodim E, Tannous O, Saifi C, Caffes N, et al. Outcomes of lumbopelvic fixation in the treatment of complex sacral fractures using minimally invasive surgical techniques. Spine J. (2017) 17(9):1238–46. doi: 10.1016/j.spinee.2017.04.032
24. Sagi HC, Militano U, Caron T, Lindvall E. A comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma. (2009) 23(5):313–9; discussion 319–21. doi: 10.1097/BOT.0b013e3181a32b91
25. Korovessis P, Spastris P, Syrimpeis V, Tsekouras V, Petrou S. Contemporary less invasive spinal instrumentation for AO C-type posterior pelvic ring injuries. Eur Spine J. (2020) 29(10):2521–33. doi: 10.1007/s00586-019-06180-1
26. Sakti YM, Mafaza A, Lanodiyu ZA, Sakadewa GP, Magetsari R. Management of complex pelvic fracture and sacral fracture denis type 2 using spanning unilateral fixation of L5 to S2AI screw. Int J Surg Case Rep. (2020) 77:543–8. doi: 10.1016/j.ijscr.2020.11.053
27. Steelman K, Russell R, Vaidya R. Bilateral vertical shear sacroiliac joint dislocations treated with bilateral triangular osteosynthesis in a young female: a case report. Trauma Case Rep. (2021) 33:100485. doi: 10.1016/j.tcr.2021.100485
28. Bellabarba C, Stewart JD, Ricci WM, DiPasquale TG, Bolhofner BR. Midline sagittal sacral fractures in anterior-posterior compression pelvic ring injuries. J Orthop Trauma. (2003) 17:32–7. doi: 10.1097/00005131-200301000-00005
29. Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML Jr, Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. (2006) 20(7):447–57. doi: 10.1097/00005131-200608000-00001
30. Gupta P, Barnwell JC, Lenchik L, Wuertzer SD, Miller AN. Spinopelvic dissociation: multidetector computed tomographic evaluation of fracture patterns and associated injuries at a single level 1 trauma center. Emerg Radiol. (2016) 23:235–40. doi: 10.1007/s10140-016-1383-4
31. Yi C, Hak DJ. Traumatic spinopelvic dissociation or U-shaped sacral fracture: a review of the literature. Injury. (2012) 43:402–8. doi: 10.1016/j.injury.2010.12.011
32. De Mauro D, Rovere G, Smakaj A, Marino S, Ciolli G, Perna A, et al. Gibson approach and surgical hip dislocation according to Ganz in the treatment of femoral head fractures. BMC Musculoskelet Disord. (2021) 22(Suppl 2):961. doi: 10.1186/s12891-021-04800-w
33. Daniels AH, DePasse JM, Eltorai AE, Palumbo MA. Perpendicular iliac screw placement for reinforcement of spinopelvic stabilization. Orthopedics. (2016) 39:e1209–12. doi: 10.3928/01477447-20160729-02
34. Bucholz RW, Heckman JD, Court-Brown CM, Torneta P 3rd. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Lippincott Williams & Wilkins (2009).
35. De Mauro D, Rovere G, Are L, Smakaj A, Aprato A, Mezzadri U, et al. Spring plates as a valid additional fixation in comminuted posterior wall acetabular fractures: a retrospective multicenter study. J Clin Med. (2023) 12(2):576. doi: 10.3390/jcm12020576
Keywords: lumbopelvic fixation, triangular fixation, pelvis, internal fixators, infix, osteosynthesis
Citation: Rovere G, De Mauro D, Smakaj A, Sassara G, De Vitis R, Farsetti P, Camarda L, Maccauro G and Liuzza F (2024) Triangular osteosynthesis and lumbopelvic fixation as a valid surgical treatment in posterior pelvic ring lesions: a systematic review. Front. Surg. 11:1266393. doi: 10.3389/fsurg.2024.1266393
Received: 24 July 2023; Accepted: 7 February 2024;
Published: 22 February 2024.
Edited by:
Carl Haasper, Orthopaedic Surgery Bremerhaven-Wesermünde, GermanyReviewed by:
Giovanni Noia, Azienda Ospedaliero-Universitaria Ospedali Riuniti di Foggia, ItalyOsvaldo Mazza, Bambino Gesù Children’s Hospital (IRCCS), Italy
© 2024 Rovere, De Mauro, Smakaj, Sassara, De Vitis, Farsetti, Camarda, Maccauro and Liuzza. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giuseppe Rovere Z2l1c2VwcGUucm92ZXJlMDJAaWNhdHQuaXQ=
 Giuseppe Rovere
Giuseppe Rovere Domenico De Mauro1
Domenico De Mauro1 Amarildo Smakaj
Amarildo Smakaj Rocco De Vitis
Rocco De Vitis Lawrence Camarda
Lawrence Camarda