- Department of Ophthalmology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Background: Kaposiform hemangioendothelioma (KHE) is a rare and invasive vascular tumor that mainly occurs in children and is rarely seen in adults. We report a case of KHE found on the eyelid of an adult patient.
Case report: We present an adult patient in whom KHE recurred 6 months after tumor resection. He underwent second surgical resection and intraoperative chemotherapy. There was no evidence of recurrence at the 3-year follow-up.
Conclusion: KHE in adults is easy to be misdiagnosed. KHE can be treated by surgical resection. Complete resection of the tumor and intraoperative chemotherapy may help prevent a recurrence.
1 Introduction
Kaposiform hemangioendothelioma (KHE) is a rare vascular tumor commonly seen in infants, with a high incidence rate and mortality. The main pathological characteristics are abnormal angiogenesis and lymphangiogenesis (1). The vascular channels form a group of glomerular nodules with variable lumina and a surrounding pericytic layer (2). KHE often grows in an invasive way, showing dilated erythema or purple soft tissue mass, which is common in limbs and the trunk, followed by the retroperitoneum, and rarely in the head and neck (3, 4). There are not many treatment options for KHE; surgical resection is the main therapeutic option, but KHE often recurred after incomplete excision (5). Here we report a case of recurrent KHE in the eyelid of an adult male.
2 Case presentation
A 23-year-old male patient with recurrent blepharal KHE was hospitalized 6 months after the first tumor resection. The tumor had an undefined reddish strawberry hyperplasia appearance, invading the inner canthus and inner one-third part of the upper and lower eyelids but did not cause the Kasabach–Merritt phenomenon (KMP) (Figure 1A). The patient was cured and was relapse-free after surgical resection of the tumor with accurate control of negative cutting edge and intraoperative prophylactic administration of bleomycin at the edge and the base of the tumor body. Histopathological findings confirmed a diagnosis of low-grade malignant kaposiform hemangioendothelioma (Figures 2A,B) with a positive stain of CD34 and negative HHV8. Blepharal kaposiform hemangioendothelioma in adults has been rarely reported. The effect of intraoperative application of anti-tumor agents such as bleomycin on the prevention of tumor recurrence remains to be further observed and studied.
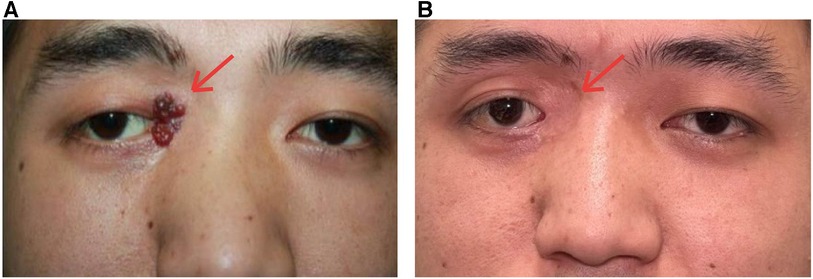
Figure 1. Surgical removal of the KHE combined with chemotherapy prevented the tumor recurrence in the 3-year follow-up. (A) Preoperation: the recurrent tumor had invaded the inner canthus and inner one-third part of the upper and lower eyelids. (B) The tumor was completely removed and combined with bleomycin treatment during the operation. No recurrence was noticed.

Figure 2. Histologic analysis of the mass. (A) Photomicrographs showing a nodular distribution of infiltrative angiomatous nodules [hematoxylin and eosin (H&E), original magnification: ×100]. (B) Angiomatous nodules were composed of crisscross spindle cell bundles and crescent vascular channels, with fibrin microthrombi in the lumen (H&E, original magnification: ×200).
No evidence of tumor recurrence was observed at the 3-year follow-up (Figure 1B).
3 Discussion
Standard therapy is yet to be established for recurrent KHE, because of its rarity and the associated difficulties in conducting clinical trials. Here we report such a rare case of KHE in the eyelid of an adult patient.
KHE is a rare invasive vascular tumor, which has no self-healing tendency and can cause red blood cell destruction, thrombocytopenia, and so on. KHE is classified as a vascular tumor with medium malignant potential by the World Health Organization (WHO) (2). KHE usually occurs in children's limbs and trunks, and is rarely observed in either adults or on the eyelid. About 42%–71% of KHE is known to be accompanied by KMP (1), which is a triad of microangiopathic hemolytic anemia, thrombocytopenia, and consumptive coagulation dysfunction (6, 7).
According to a 2016 study, only 26 cases of KHE in adults were found from 1993 to 2016, including only one case pertaining to the eyelid, and none of them was accompanied by KMP (8). The review by Schmid et al. confirmed that the incidence rate of KMP decreases with the age of patients (7). KMP is also not found in this case. However, even if there is no KMP, KHE should also be taken into account in the diagnosis when there is an enlarged purplish red mass, which is helpful in the early diagnosis and treatment to improve the prognosis of patients.
Clinical diagnosis of KHE is challenging due to the variety of clinical manifestations (3). The diagnosis requires an analysis of clinical presentations, laboratory examinations, and histopathological examinations (1). The gold standard for diagnosis is tissue biopsy; histologically, it is an isolated and fusional nodule formed by spindle-shaped endothelial cell bundles and crescent vascular channels, and the tumor margin is often ambiguous and irregular (9). In immunohistochemical staining, vascular endothelial markers of spindle cells, including CD31 and CD34, were positive (9). In this case, the diagnosis of KHE was made based on the combined pathological examination results from the first operation and the patient's clinical manifestations, Postoperative histopathological result confirmed the diagnosis of KHE.
Tufted angioma (TA), juvenile hemangioma (JH), infantile hemangioma (IH), and congenital hemangioma can be similar to KHE. Most of them can be differentiated by histology and immunophenotype (10). TA is a superficial benign tumor; some authors think that KHE and TA represent two ends of the histological spectrum, and now they have been combined (2). KHE is characterized by round nodules and red cell sequestration, but JH lacks these features (2). IH expresses the glucose transporter 1 (GLUT1), which is not found in KHE (10).
There is no systematic treatment for KHE. Surgical resection is the preferred treatment for KHE at present, but its application is limited due to the difficulty of total excision and incomplete resection may have a high risk of recurrence (10, 11). In addition to surgery, drug therapy can also be used. Corticosteroids and chemotherapy are first-line therapies, and recently, sirolimus has also been used for treatment (12, 13). In this case, the patient underwent his first tumor resection in another hospital, and the postoperative pathological examination results indicated KHE but no further therapy was administered. Recurrence was noted 6 months later, but the cause of recurrence was unknown. It has been reported that recurrence occurs in about 15% of patients even after surgical resection (11). Despite taking extra care to leave clear margins after each operation, there was a patient who experienced recurrences (14). During the second operation, we confirmed that the surgical margin was negative through frozen sections and added bleomycin for local chemotherapy. Considering that if KHE could not be completely resected through surgery, drug chemotherapy was generally recommended (12). There is a case showed that surgical resection combined with chemotherapy is effective for recurrent tumor, even in patients with stage IV cancer (15). Also, in the treatment of hemangiomas, intratumoral injection of bleomycin may have a sclerosing effect on potentially residual or recalcitrant tumor tissue (16). No recurrence was found in the follow-up after the operation.
4 Conclusion
In conclusion, we successfully treated an adult patient with recurrent blepharal KHE. In this case, surgical resection combined with chemotherapy was effective during the 3-year follow-up. It is important to select the appropriate treatment method for each individual case of a rare tumor. Further studies of treatments for recurrent blepharal KHE are warranted.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
WL: Writing – original draft, Writing – review & editing. DZ: Writing – review & editing. SZ: Writing – original draft. HC: Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by National Natural Science Foundation of China (General Program 82371061), Natural Science Foundation of Hubei Province of China (2019CFB152), and Science Research Foundation of Union Hospital (2022xhyn046).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ji Y, Chen S, Yang K, Xia C, Li L. Kaposiform hemangioendothelioma: current knowledge and future perspectives. Orphanet J Rare Dis. (2020) 15(1):39. doi: 10.1186/s13023-020-1320-1
2. Chundriger Q, Tariq MU, Abdul-Ghafar J, Ahmed A, Din NU. Kaposiform hemangioendothelioma: clinicopathological characteristics of 8 cases of a rare vascular tumor and review of literature. Diagn Pathol. (2021) 16(1):23. doi: 10.1186/s13000-021-01080-9
3. Fernández Y, Bernabeu-Wittel M, García-Morillo JS. Kaposiform hemangioendothelioma. Eur J Intern Med. (2009) 20(2):106–13. doi: 10.1016/j.ejim.2008.06.008
4. Zhang G, Gao Y, Liu X. Kaposiform haemangioendothelioma in a nine-year-old boy with Kasabach-Merritt phenomenon. Br J Haematol. (2017) 179(1):9. doi: 10.1111/bjh.14837
5. Jung SC, Jung TY, Lee TK, Kim YJ, Beak HJ, Kim SS. Kaposiform hemangioendothelioma of skull base with dura invasion in a pediatric patient: a case report. Childs Nerv Syst. (2023) 39(11):3289–94. doi: 10.1007/s00381-023-06025-96
6. Pati S, Das MK, Rana A, Das E, Sarkar S, Sherpa N, et al. Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon. Indian J Pediatr. (2021) 88(11):1142–4. doi: 10.1007/s12098-021-03817-2
7. Schmid I, Klenk AK, Sparber-Sauer M, Koscielniak E, Maxwell R, Häberle B. Kaposiform hemangioendothelioma in children: a benign vascular tumor with multiple treatment options. World J Pediatr. (2018) 14(4):322–9. doi: 10.1007/s12519-018-0171-5
8. Vashi P, Abboud E, Bier-Laning C, Gupta D. Adult-onset kaposiform hemangioendothelioma of the tongue: case report and review of the literature. Curr Oncol. (2016) 23(5):e517–20. doi: 10.3747/co.23.3239
9. Liu Q, Jiang L, Wu D, Kan Y, Fu F, Zhang D, et al. Clinicopathological features of kaposiform hemangioendothelioma. Int J Clin Exp Pathol. (2015) 8(10):13711–8.26722599
10. Putra J, Gupta A. Kaposiform haemangioendothelioma: a review with emphasis on histological differential diagnosis. Pathology. (2017) 49(4):356–62. doi: 10.1016/j.pathol.2017.03.001
11. Wong BL, Lee VN, Tikka T, Kim D, Dwivedi RC. Kaposiform haemangioendothelioma of the head and neck. Crit Rev Oncol Hematol. (2016) 104:156–68. doi: 10.1016/j.critrevonc.2016.06.005
12. Martin MC, Harrington H, Wong WW. Massive congenital kaposiform hemangioendothelioma of the eyelid in a neonate. J Craniofac Surg. (2011) 22(6):e38–41. doi: 10.1097/SCS.0b013e318231e139
13. Wang H, Guo X, Duan Y, Zheng B, Gao Y. Sirolimus as initial therapy for kaposiform hemangioendothelioma and tufted angioma. Pediatr Dermatol. (2018) 35(5):635–8. doi: 10.1111/pde.13600
14. Kim MG, Choi YS, Park SJ, Chong SM. Kaposiform hemangioendothelioma of the breast in an adult female. Clin Breast Cancer. (2011) 11(2):135–7. doi: 10.1016/j.clbc.2011.03.008
15. Terada J, Toyoda Y, Takeuchi E, Tanida N, Ito S, Yorita K, et al. Surgical resection combined with perioperative chemotherapy for a patient with locally recurrent, previously stage IV thymic small-cell carcinoma: a case report. Thorac Cancer. (2022) 13(23):3415–9. doi: 10.1111/1759-7714.14717
16. Xu S, Yu Y, ElHakim H, Cui X, Yang H. The therapeutic effect of the combination of intratumor injection of bleomycin and electroresection/electrocautery on the hemangiomas in hypopharynx and larynx through suspension laryngoscopy. Ann Otol Rhinol Laryngol. (2019) 128(6):575–80. doi: 10.1177/0003489419831715
Keywords: kaposiform hemangioendothelioma, adult eyelid, recurrence, bleomycin, rare
Citation: Liu W, Zhao D, Zhou S and Chen H (2024) Case Report: Recurrent blepharal kaposiform hemangioendothelioma in an adult patient. Front. Surg. 10:1306566. doi: 10.3389/fsurg.2023.1306566
Received: 4 October 2023; Accepted: 20 November 2023;
Published: 4 January 2024.
Edited by:
Wenbo Zhang, University of Texas Medical Branch at Galveston, United StatesReviewed by:
Wanlin Fan, University Hospital of Cologne, GermanyZhenyang Zhao, University of Michigan, United States
© 2024 Liu, Zhao, Zhou and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shirui Zhou bTIwMjI3NTk4NEBodXN0LmVkdS5jbg== Hong Chen Y2hlbmhvbmdreTUzQGhvdG1haWwuY29t
 Wei Liu
Wei Liu Shirui Zhou
Shirui Zhou Hong Chen
Hong Chen