- 1Covalent Bio, LLC, St. Louis, MO, United States
- 2Cleveland Clinic Center for Abdominal Core Health, Cleveland Clinic, the Cleveland Clinic Foundation, Digestive Diseases and Surgery Institute, Cleveland, OH, United States
- 3Center for Abdominal Core Health, The Ohio State Wexner Medical Center, Columbus, OH, United States
- 4BD Interventional (Surgery), Warwick, RI, United States
- 5Vanderbilt University Medical Center, Nashville, TN, United States
- 6Center for Biostatistics, Department of Biomedical Informatics, The Ohio State University Wexner Medical Center, Columbus, OH, United States
Background: Permanent synthetic meshes such as polypropylene (PP) have been utilized for hernia repair for decades, but concerns remain regarding potential long-term, mesh-related complications. A resorbable polymer such as poly-4-hydroxybutyrate (P4HB) represents an alternative with high initial strength, that gradually resorbs, leaving an abdominal wall that is at least as strong as it would be in its native state. We aimed to compare early wound morbidity and clinical outcomes associated with P4HB to traditional, permanent PP in umbilical and small to medium, routine ventral hernias using data from the Abdominal Core Health Quality Collaborative (ACHQC).
Methods: Inclusion criteria for the umbilical cohort included: all Centers for Disease Control and Prevention (CDC) wound classes, all Ventral Hernia Working Group (VHWG) hernia grades, and hernia defects <3 cm. The small to medium, routine ventral hernia cohort was limited to CDC class I wounds, VHWG hernia grades I and II, and hernia defects <5 cm. The study group was comprised of P4HB meshes; the comparator group was an aggregate of PP meshes. Clinical outcomes were assessed at 30 days.
Results: There was no significant difference in early wound morbidity, readmission, or reoperation between the P4HB and PP cohorts. A small number of patients experienced SSO, with ≤4% requiring procedural intervention. None of the patients (0% in all cases) experienced skin/soft tissue necrosis, infected seroma, infected hematoma, exposed/contaminated/infected mesh, enterocutaneous fistula, graft failure, or pain requiring intervention at 30-days. However, P4HB was associated with significantly greater operative time, length of stay, and use of myofascial release compared to PP (p < 0.05 in all cases).
Conclusions: Short-term clinical outcomes associated with resorbable P4HB mesh are comparable to permanent synthetic PP mesh in umbilical and small to medium, routine ventral hernia repairs, despite significant differences in operative time and length of stay. Longer-term follow-up is needed to expand on the clinical relevance of these short-term findings.
Introduction
Poly-4-hydroxybutyrate (P4HB) is a biologically produced, fully resorbable synthetic polymer that has been used to construct meshes for hernia repair applications (1–3). Bench and preclinical studies have established the long-term strength and durability of P4HB, and clinical studies have extended these findings, documenting outcomes comparable to other mesh materials (4).
P4HB mesh has been utilized in a wide variety of patient populations, but a recent scoping review identified a knowledge gap in umbilical and small to medium-sized, routine ventral hernias (4). Permanent synthetic meshes are commonly utilized in these applications (5–9). However, the possibility of long-term, mesh-related complications such as seroma, chronic pain, infection, fistula, and bowel obstruction must be considered due to the permanent nature of these materials (10).
Meshes constructed of a fully resorbable polymer such as P4HB represent a potential advantage over permanent polymers due to their temporary status within the abdominal wall, both in terms of reducing possible mesh-related complications, as well as in decreasing the complexity of subsequent abdominal procedures (10, 11). However, it has been suggested that the resorption of these materials may provoke a more aggressive, early host tissue response in the form of increased macrophage activation (12) and inflammation (13), potentially leading to higher rates of early wound morbidity compared to permanent synthetic meshes (14). To date, this concept has only been assessed in a cohort of complex cases involving clean-contaminated and contaminated wounds, which contributed a number of confounding factors to the analysis and prevented definitive conclusions (14).
Thus, two important knowledge gaps currently exist in the scientific literature surrounding P4HB mesh use in hernia repair applications, namely a lack of clinical data in umbilical and small to medium-size ventral hernia populations, as well as an evaluation of the early wound morbidity associated with less complex or “routine” cases. The current study was designed to focus on these populations, eliminating a number of confounding factors, in an effort to better understand potential differences between resorbable, monofilament P4HB mesh compared to permanent, monofilament polypropylene mesh.
Methods
A retrospective analysis was completed utilizing data collected prospectively through the Abdominal Core Health Quality Collaborative (ACHQC) database (formerly the Americas Hernia Society Quality Collaborative—AHSQC) (15). The ACHQC is a voluntary, national database that is prospectively maintained for the purpose of improving abdominal core health through a continuous quality improvement process. At the time of this study, data were available within the ACHQC for n = 102,084 total patients (n = 43,191 ventral hernia patients) contributed by n = 424 surgeons from academic, community, and academic-affiliated hospital settings.
The ACHQC database was queried for patients undergoing umbilical or small to medium, routine ventral hernias between January 2012 and September 2022. The inclusion criteria for the umbilical hernia cohort included: all Centers for Disease Control and Prevention (CDC) wound classes (16) and all Ventral Hernia Working Group (VHWG) hernia grades (17), as well as hernia defects <3 cm. Although this cohort is entitled “umbilical hernia”, ventral hernias <3 cm were also included as a surrogate for less complex umbilical hernias. The inclusion criteria for the small to medium, routine ventral hernia cohort were slightly different and limited to CDC wound class I wounds, VHWG hernia grades I and II, and hernia defects <5 cm. In this cohort, the term “small to medium, routine ventral hernia” was not defined according to a validated scale. Rather, the term was intended to differentiate this cohort from more complex cases described in the literature (e.g., CDC wound classes II, III, and IV; VHWG hernia grades III and IV; hernias >5 cm, etc.). For both cohorts, the study group was comprised of poly-4-hydroxybutyrate meshes (Phasix™ Mesh or Phasix™ ST Mesh—collectively “P4HB”; Becton, Dickinson, and Company, Warwick, RI), while the comparator group was comprised of an aggregate of permanent synthetic polypropylene meshes (Bard™ Mesh, Bard™ Soft Mesh, Ventralex™ Hernia Patch, Ventralex™ ST Hernia Patch, Ventralight™ ST Mesh, Ventrio™ Hernia Patch, and Ventrio™ ST Hernia Patch—collectively “PP”; Becton, Dickinson, and Company, Warwick, RI).
Clinical outcomes were assessed at 30 days. Primary outcomes were defined as perioperative complications, including immediate hernia recurrence, surgical site infection (SSI), surgical site occurrence (SSO) and surgical site occurrence with procedural intervention (SSOPI). Hernia recurrence was assessed by physical exam and/or computed tomography (CT) scan when possible. A pragmatic definition of recurrence was adapted from Krpata et al. (18) SSI were defined according to the CDC, (16) and SSO included SSI, wound cellulitis, non-healing incisional wound, fascial disruption, skin/soft tissue ischemia or necrosis, serous or purulent wound drainage, stitch abscess, seroma, hematoma, infected or exposed mesh, or enterocutaneous fistula. Procedural interventions for SSOPI included wound opening, wound debridement, suture excision, percutaneous drainage, and partial/complete mesh removal. Secondary outcomes included operative time, length of stay, hospital readmission, and reoperation.
A propensity score model (PSM) and matching algorithms were implemented to address potential treatment choice bias. The PSM is based on the probability of assignment to the treatment group, and was selected due to a good balance on the covariates, rather than Mahalanobis distance matching, which is based on covariate values (19). Propensity score matches were generated by matching patients receiving P4HB mesh with those receiving PP mesh. An a priori approach was used to select the clinical variables to include in the PSM based on known risk factors that can impact the outcome measure. The variables included in the PSM were: VHWG grade, hernia width, anti-platelet medications, age capped at 90, operation approach, number of prior hernia repairs, race, hypertension, concomitant procedure, ASA class, BMI capped 15–60, diabetes mellitus, and current smoker. One matched control was selected for each case. Logistic regression was used to estimate the propensity scores. Inverse probability weighting (IPWT) was not performed, as the current study design did not include a weighted regression approach. Standardized mean differences (SMD) were used to measure the balance following propensity score matching. An SMD of 0.1 was considered the threshold for good balance, and 0.2 was considered acceptable. Nearest neighbor matching without replacement was utilized as it is the most common form of greedy matching with similar performance as optimal matching (20); no caliper was used. Pearson's Chi-squared test was used to compare categorical variables between P4HB and PP, while Wilcoxon rank sum test was used to compare continuous variables. A p-value < 0.05 was considered statistically significant.
Results
Umbilical hernia cohort
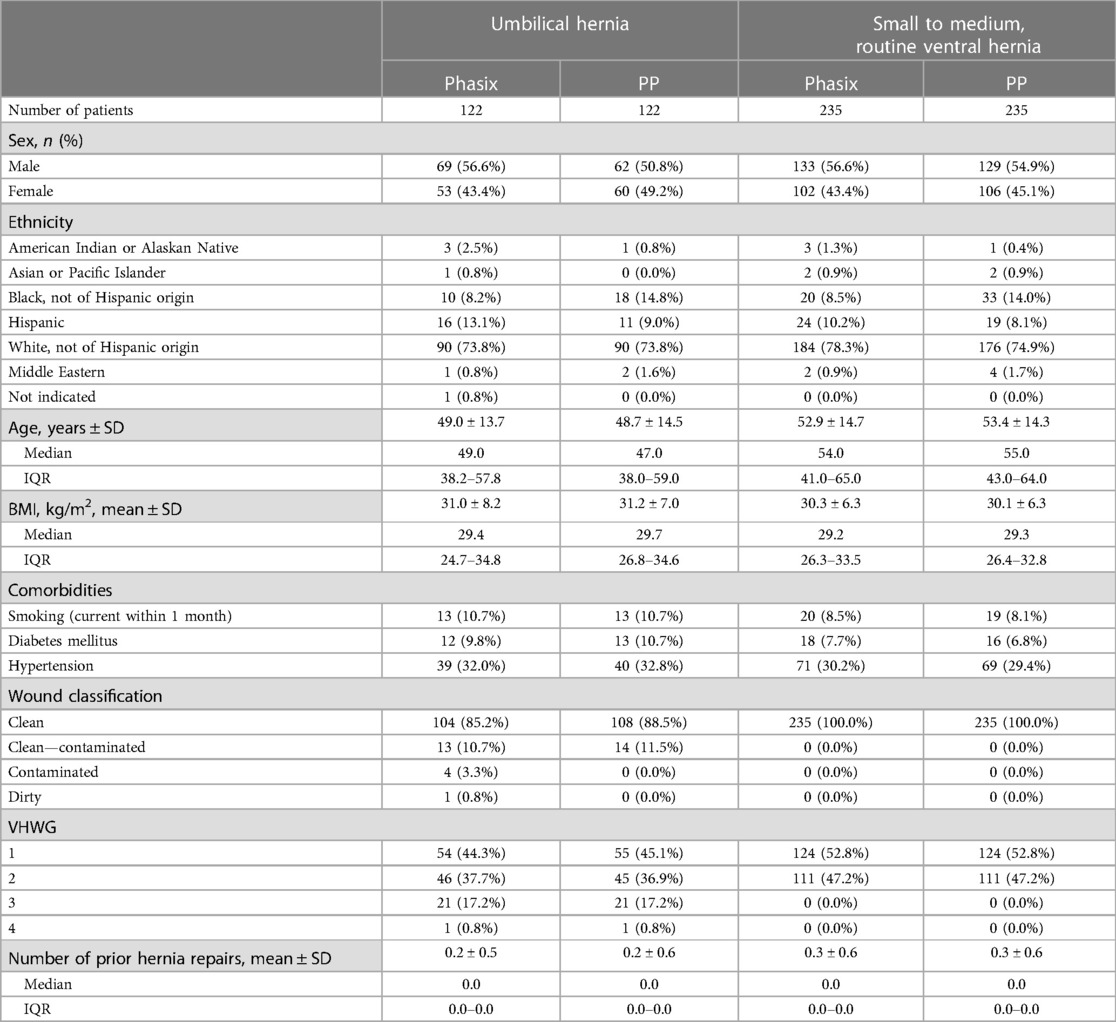
In the umbilical hernia cohort, n = 122 patients were evaluated in each group (Table 1). After propensity score matching, the P4HB and PP groups were comprised of several mesh products (Monofilament P4HB Meshes: n = 76 Phasix™ Mesh and n = 46 Phasix™ ST Mesh and Monofilament PP Meshes: n = 4 Bard™ Mesh, n = 25 Bard™ Soft Mesh, n = 4 Ventralex™ Hernia Patch, n = 42 Ventralex™ ST Hernia Patch, n = 43 Ventralight™ ST Mesh, n = 0 Ventrio™ Hernia Patch, and n = 4 Ventrio™ ST Hernia Patch, respectively.) Patients were primarily White and non-Hispanic (P4HB: 73.8% vs. PP: 73.8%; p > 0.05) with similar age (P4HB: 49.0 (38.2–57.8) years vs. PP: 47.0 (38.0–59.0) years; median (IQR); p > 0.05), BMI (P4HB: 29.4 (24.7–34.8) kg/m2 vs. PP: 29.7 (26.8–34.6) kg/m2; median (IQR); p > 0.05), comorbidities, wound classification, and number of prior repairs (P4HB: 0.0 (0.0–0.0) prior repairs vs. PP: 0.0 (0.0–0.0) prior repairs; median (IQR); p > 0.05); divided almost equally among males (P4HB: 56.6% vs. PP: 50.8%; p > 0.05) and females (P4HB: 43.4% vs. PP: 49.2%; p > 0.05).
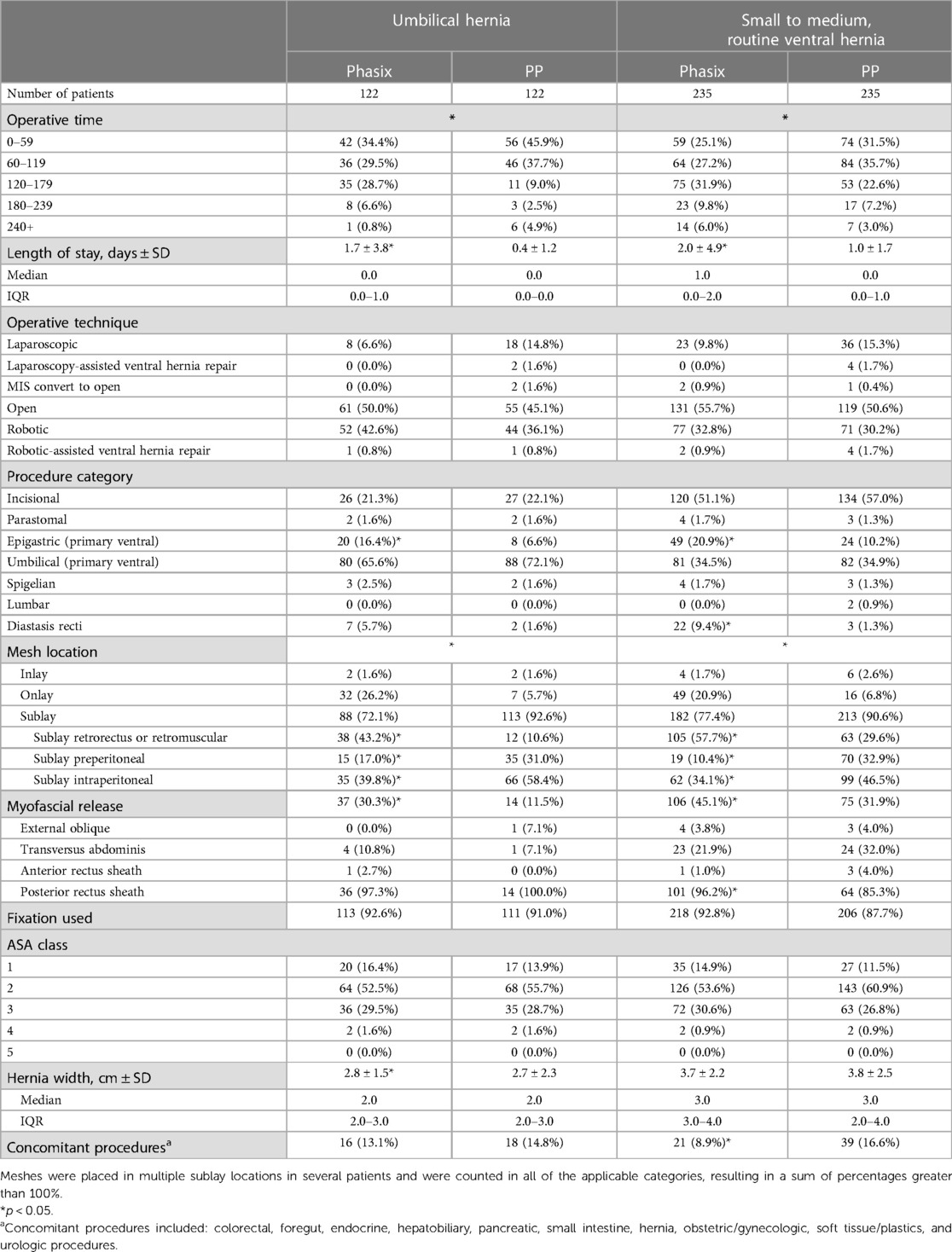
As shown in Table 2, the majority of patients in the umbilical hernia cohort underwent open (P4HB: 50.0% vs. PP: 45.1%; p > 0.05) or robotic repairs (P4HB: 42.6% vs. PP: 36.1%; p > 0.05) with sublay mesh placement (P4HB: 72.1% vs. PP: 92.6%; p > 0.05). Within the sublay category, significantly more retrorectus or retromuscular repairs were performed in the P4HB cohort (43.2%) compared to the PP cohort (10.6%, p < 0.05). Conversely, significantly more preperitoneal and intraperitoneal sublay repairs were performed in the PP cohort compared to the P4HB cohort (preperitoneal: P4HB: 17.0% and PP: 31.0%; intraperitoneal: P4HB: 39.8% and PP: 58.4%; p < 0.05 in all cases). Fixation was utilized in greater than 90% of both P4HB and PP mesh groups.
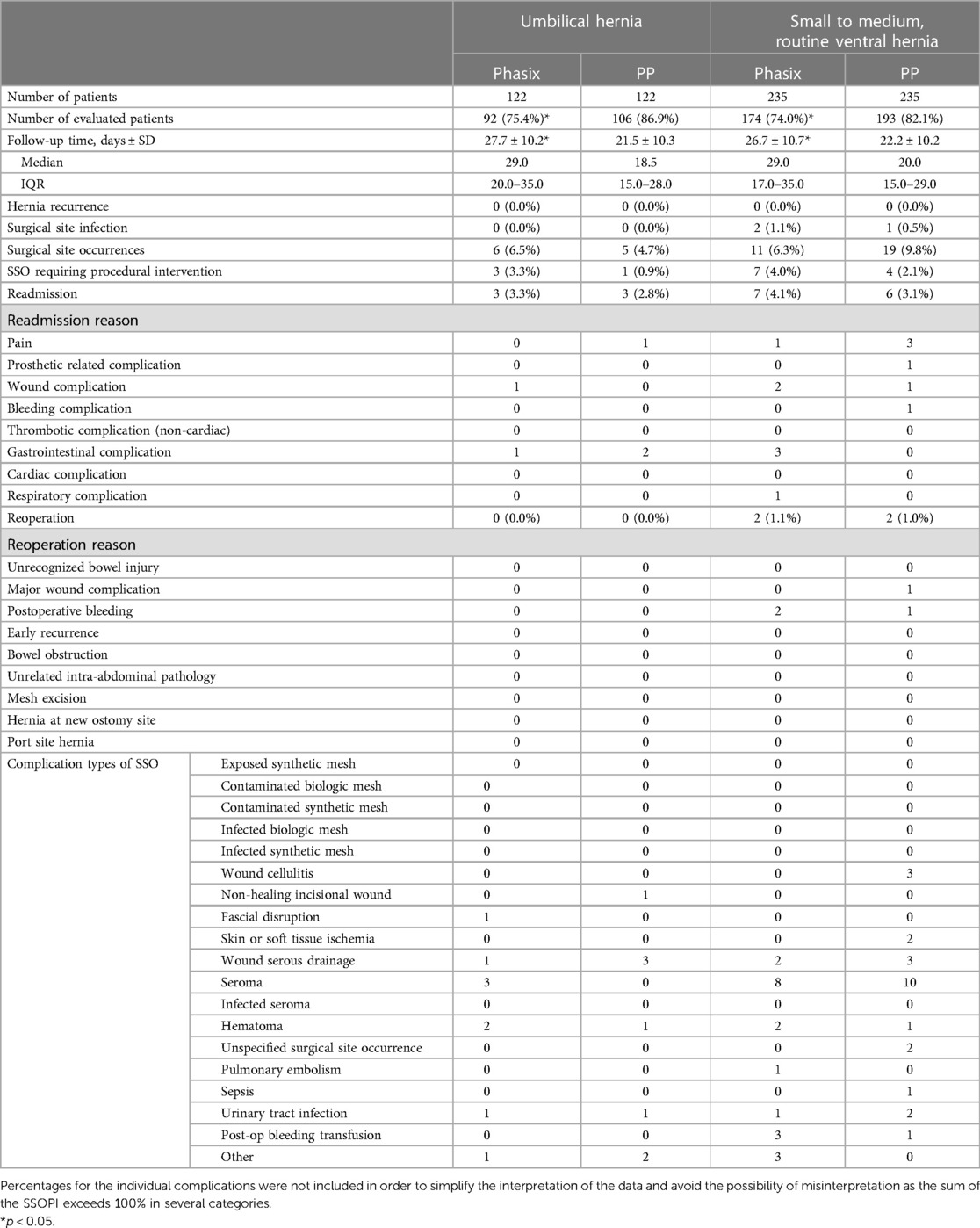
Patients in the P4HB group reported significantly longer operative time (P4HB: 36.1% ≥ 2 h vs. PP: 16.4% ≥ 2 h; p < 0.001), significantly longer length of stay (P4HB: 1.7 ± 3.8 days (median: 0.0; IQR: 0.0–1.0) vs. PP: 0.4 ± 1.2 days (median: 0.0; IQR: 0.0–0.0); p < 0.001), more epigastric hernias (P4HB: 16.4% vs. PP: 6.6%; p = 0.016), and more procedures requiring myofascial release (P4HB: 30.3% vs. PP: 11.5%; p < 0.001) compared to those receiving PP mesh (Table 2). There were no significant differences between P4HB and PP with regard to any of the short-term (30-day) postoperative complications evaluated in this study (Table 3), particularly hospital readmission, hernia recurrence, SSI, SSO, and SSOPI (p > 0.05 in all cases). A small number of patients experienced non-healing incisional wounds, fascial disruption, wound/serous drainage, seroma, and hematoma, among others. None of the patients in the umbilical hernia cohort experienced hernia recurrence, SSI, skin/soft tissue necrosis/ischemia, wound cellulitis, infected seroma, infected hematoma, exposed/contaminated/infected mesh, enterocutaneous fistula, graft failure, or pain requiring intervention at 30-days. As shown in Table 3, a small number of patients in each cohort required readmission (P4HB: 3.3%; PP: 2.8%, p > 0.05). In the P4HB cohort, readmission occurred due to wound, gastrointestinal, and unknown complications (n = 1 in each category) and in the PP cohort due to pain (n = 1) and gastrointestinal complications (n = 2). However, none of the patients in either cohort required reoperation during the follow-up period (n = 0 in all of the following categories: unrecognized bowel injury, major wound complication, postoperative bleeding, early recurrence, bowel obstruction, unrelated intraabdominal pathology, mesh excision, hernia at new ostomy site, or port site hernia).
Small to medium, routine ventral hernia cohort
In the small to medium, routine ventral hernia cohort, n = 235 patients were evaluated in each group (Table 1). After propensity score matching, the P4HB and PP groups were comprised of several mesh types (P4HB: n = 148 Phasix™ Mesh and n = 87 Phasix™ ST Mesh and PP: n = 19 Bard™ Mesh, n = 78 Bard™ Soft Mesh, n = 15 Ventralex™ Hernia Patch, n = 48 Ventralex™ ST Hernia Patch, n = 69 Ventralight™ ST Mesh, n = 2 Ventrio™ Hernia Patch, and n = 4 Ventrio™ ST Hernia Patch, respectively.) As with the umbilical hernia cohort, patients in the small to medium, routine ventral hernia cohort were again primarily White and non-Hispanic (P4HB: 78.3% vs. PP: 74.9%; p > 0.05) with similar age (P4HB: 54.0 (41.0–65.0) years vs. PP: 55.0 (43.0–64.0) years; median (IQR); p > 0.05), BMI (P4HB: 29.2 (26.3–33.5) kg/m2 vs. PP: 29.3 (26.4–32.8) kg/m2; median (IQR); p > 0.05), comorbidities, wound classification, and number of prior repairs (P4HB: 0.0 (0.0–0.0) prior repairs vs. PP: 0.0 (0.0–0.0) prior repairs; median (IQR); p < 0.05); divided almost equally among males (P4HB: 56.6% vs. PP: 54.9%; p > 0.05) and females (P4HB: 43.4% vs. PP: 45.1%; p > 0.05).
As shown in Table 2, the majority of patients in the small to medium, routine ventral hernia cohort underwent open (P4HB: 55.7% vs. PP: 50.6%; p > 0.05) or robotic repairs (P4HB: 32.8% vs. PP: 30.2%; p > 0.05) with sublay mesh placement (P4HB: 77.4% vs. PP: 90.6%; p > 0.05). Within the sublay category, significantly more retrorectus or retromuscular repairs were performed in the P4HB cohort (57.7%) compared to the PP cohort (29.6%, p < 0.05). Conversely, significantly more preperitoneal and intraperitoneal sublay repairs were performed in the PP cohort compared to the P4HB cohort (preperitoneal: P4HB: 10.4% and PP: 32.9%; intraperitoneal: P4HB: 34.1% and PP: 46.5%; p < 0.05 in all cases). Meshes were placed in multiple sublay locations in several patients and were counted in all of the applicable categories, resulting in a sum of percentages greater than 100% (Table 2). Fixation was utilized in greater than 85% of both P4HB and PP mesh groups.
Patients in the P4HB group reported significantly longer operative time (P4HB: 47.7% ≥ 2 h vs. PP: 32.8% ≥ 2 h; p = 0.022), significantly longer length of stay (P4HB: 2.0 ± 4.9 days (median: 1.0; IQR: 0.0–2.0) vs. PP: 1.0 ± 1.7 days (median: 0.0; IQR: 0.0–1.0); p = 0.020), more epigastric hernias (P4HB: 20.9% vs. PP: 10.2%; p = 0.001), significantly more procedures requiring myofascial release (P4HB: 45.1% vs. PP: 31.9%; p = 0.003) and significantly fewer concomitant procedures (P4HB: 8.9% vs. PP: 16.6%; p = 0.013) compared to those receiving PP mesh (Table 2). There were no significant differences between P4HB and PP with regard to any of the short-term (30-day) postoperative complications evaluated in this study (Table 3), particularly hospital readmission, hernia recurrence, SSI, SSO, and SSOPI (p > 0.05 in all cases). A small number of patients experienced wound cellulitis, skin/soft tissue ischemia, wound/serous drainage, seroma, and hematoma, among others. None of the patients in the small to medium, routine ventral hernia cohort experienced hernia recurrence, non-healing incisional wound, fascial disruption, skin/soft tissue necrosis, infected seroma, infected hematoma, exposed/contaminated/infected mesh, enterocutaneous fistula, graft failure, or pain requiring intervention at 30-days. As shown in Table 3, a small number of patients in each cohort required readmission (P4HB: 4.1%; PP: 3.1%; p > 0.05). In the P4HB cohort, readmission occurred due to pain (n = 1), wound complications (n = 2), gastrointestinal complications (n = 3), and respiratory complications (n = 1). In the PP cohort, readmission occurred due to pain (n = 3) and prosthetic-related, wound, or bleeding complications (n = 1 in each category). Similarly, a small number of patients in each cohort required reoperation during the follow-up period (P4HB: 1.1%; PP: 1.0%; p > 0.05). In the P4HB cohort, reoperation occurred due to postoperative bleeding (n = 2) and in the PP cohort due to major wound complications and postoperative bleeding (n = 1 in each category).
Discussion
Permanent synthetic meshes such as PP have been successfully utilized in hernia repair for several decades, but long-term, mesh-related complications remain concerning. Resorbable polymers such as P4HB gradually resorb, returning the abdominal wall to its native state without the presence of a foreign material over the long-term. However, there is some concern about the potential impact of these resorbable materials on the early host tissue response and subsequent wound morbidity related to increased macrophage activation (12) or inflammatory response (13). The current study was therefore designed to compare early wound morbidity and clinical outcomes associated with a fully resorbable hernia mesh material (P4HB) to a traditional, permanent material (PP) in umbilical and small to medium-sized, routine ventral hernias.
No significant differences were observed between the P4HB and PP cohort with regard to the primary outcomes of early wound morbidity or the secondary outcomes of readmission and reoperation (p > 0.05 in all cases). However, differences were observed between the P4HB and PP cohorts for the secondary outcomes of operative time and length of hospital stay. Resorbable P4HB meshes were associated with significantly longer operative times, significantly longer length of hospital stay, and significantly more frequent use of myofascial release compared to permanent PP mesh in both the umbilical hernia and small to medium, routine ventral hernia cohorts. This is likely attributed to aspects of the surgical techniques employed in these cases and demonstrates the “real-world” nature of the data obtained through the ACHQC. The majority of the P4HB meshes were implanted in the retrorectus/retromuscular tissue plane, while PP meshes were implanted predominantly in the intraperitoneal tissue plane. Additionally, ∼30%–40% of the cases in this study utilized a robotic technique (Table 2). It is well known that a robotic, retromuscular/preperitoneal repair (i.e., extended totally extraperitoneal—eTEP) is a much lengthier procedure than a robotic intraperitoneal mesh repair. P4HB repairs utilized myofascial release significantly more frequently than PP, even in the umbilical hernia cohort. The results of this study provide unique insight into how surgeons are utilizing P4HB mesh, namely via robotic, retromuscular repairs with myofascial release in small, uncomplicated hernias, leading to longer operative time and length of hospital stay. Despite “overtreating” these small hernias and the slightly higher number of more complex cases in the P4HB group in this study, early wound morbidity and clinical outcomes were comparable between P4HB and PP groups. The longer operative times and length of hospital stay reported in the P4HB cohort would otherwise favor the PP cohort, yet we did not observe any significant differences in clinical observations of wound occurrences, suggesting that the fully resorbable P4HB did not negatively impact early wound morbidity as speculated in previous studies involving complex patients with clean-contaminated or contaminated wounds (14).
The results of this study compare well with the published literature, including a pilot study involving P4HB mesh in small to medium-sized, routine ventral hernias in which Plymale et al. (21) reported 0.0% SSI, 19.4% SSO (primarily seroma) and 12.9% readmission at a median follow up of 414 days. In a retrospective case review of the National Surgery Quality Improvement (NSQIP) database, Wagner et al. (22) reported 11.8% SSI, 14.5% wound complication, and 11.8% readmission in CDC Class I (low-risk) ventral hernia repairs. However, both of these studies involved much larger defects and longer follow-up time than the current study, which likely contributed to the higher rates of wound morbidity observed in these studies relative to the current study.
Both cohorts of the current study exhibited similar hospital readmission rates at 30 days, regardless of mesh type or patient population. Patients in the P4HB cohort reported a 3.3% hospital readmission in the umbilical hernia cohort and 4.0% in the small to medium, routine ventral hernia cohort (p > 0.05). Similarly, patients in the PP cohort reported a 2.8% hospital readmission in the umbilical hernia cohort and 3.1% in the small to medium, routine ventral hernia cohort (p > 0.05). These findings are in agreement with the published literature which has reported 30-day readmission rates of ∼5%–13% in similar cohorts (23–27).
The current study is not without limitations, most notably its retrospective nature, focus on short-term, 30-day clinical outcomes, and the potential for selection bias inherent to data derived from a voluntary database. However, the data generated provide unique insight into the “real-world” use of these biomaterials in low-risk umbilical and ventral hernia repairs without the confounding factors that may have influenced wound morbidity in previously reported complex cases (14). Furthermore, the 30-day follow-up period represents a critical look into the potential contribution of resorbable materials to early wound morbidity. While the current data demonstrate comparable early wound morbidity between the P4HB and PP cohorts, future studies should be conducted with appropriate long-term follow-up to further develop the clinical relevance and implications of these early findings and support the long-term efficacy of P4HB mesh in routine hernia repair. Additionally, cost was not evaluated in this study, however, the economic impact of utilizing P4HB mesh is an important consideration and will be evaluated in future studies.
Conclusions
Short-term clinical outcomes associated with resorbable P4HB mesh are comparable to permanent synthetic PP mesh in both umbilical and small to medium, routine ventral hernia repairs. Longer-term clinical follow-up is needed to expand on the clinical relevance of these short-term findings.
Data availability statement
The raw data supporting the conclusions of this article may be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
CD: Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. MR: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. BP: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. KB: Data curation, Formal analysis, Resources, Visualization, Writing – review & editing. L-CH: Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Writing – review & editing. JM: Data curation, Formal analysis, Investigation, Resources, Software, Validation, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This project was sponsored by Becton, Dickinson and Company (BD) of Warwick, Rhode Island (USA), and KB and AB are employees of BD. CD is the owner of Covalent Bio, LLC, which received consulting fees from BD for this project, as well as other, unrelated projects.
Conflict of interest
CD reports consulting fees from BD during the conduct of the study. CD also reports consulting fees from BD, Johnson & Johnson, Medtronic, SurgiMatrix, Tissium, Surgical Innovation Associates, Americas Hernia Society Quality Collaborative, Colorado Therapeutics, TelaBio, Osteogenics, Polynovo, MedSkin Solutions, and Aran Biomedical outside the submitted work. In addition, CD is the owner of Covalent Bio, LLC and holds the following issued patents: 2009293001, 2334257, 2,334,257UK, 602009046407.8, 2,334,257FR, 16/043,849 and 2,737,542. MR reports salary support from the ACHQC and stock options from Ariste Medical. BP reports salary support from the ACHQC and research support from BD and Advanced Medical Solutions. KB reports employment by Becton Dickinson (BD) during the conduct of this study, as well as outside of the current work. AB reports employment by Becton Dickinson (BD) during the conduct of this study, as well as outside of the current work. L-CH has nothing to disclose. JM reports salary support from the ACHQC.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Martin D, Williams S. Medical applications of poly-4-hydroxybutyrate: a strong flexible absorbable biomaterial. Biochem Engr J. (2003) 16:97–105. doi: 10.1016/S1369-703X(03)00040-8
2. Martin DP, Badhwar A, Shah DV, Rizk S, Eldridge SN, Gagne DH, et al. Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J Surg Res. (2013) 184(2):766–73. doi: 10.1016/j.jss.2013.03.044
3. Williams SF, Martin DP, Moses AC. The history of GalaFLEX P4HB scaffold. Aesthet Surg J. (2016) 36(suppl 2):S33–42. doi: 10.1093/asj/sjw141
4. Deeken CR, Chen DC, Lopez-Cano M, Martin DP, Badhwar A. Fully resorbable poly-4-hydroxybutyrate (P4HB) mesh for soft tissue repair and reconstruction: a scoping review. Front Surg. (2023) 10:1157661. doi: 10.3389/fsurg.2023.1157661
5. Kaufmann R, Halm JA, Eker HH, Klitsie PJ, Nieuwenhuizen J, van Geldere D, et al. Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. Lancet. (2018) 391(10123):860–9. doi: 10.1016/S0140-6736(18)30298-8
6. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. (2004) 240(4):578–83. doi: 10.1097/01.sla.0000141193.08524.e7
7. Aslani N, Brown CJ. Does mesh offer an advantage over tissue in the open repair of umbilical hernias? A systematic review and meta-analysis. Hernia. (2010) 14(5):455–62. doi: 10.1007/s10029-010-0705-9
8. Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J, et al. Guidelines for treatment of umbilical and epigastric hernias from the European hernia society and Americas hernia society. Br J Surg. (2020) 107(3):171–90. doi: 10.1002/bjs.11489
9. Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. (2000) 343(6):392–8. doi: 10.1056/NEJM200008103430603
10. Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. (2016) 316(15):1575–82. doi: 10.1001/jama.2016.15217
11. Rios-Diaz AJ, Cunning JR, Talwar AA, Christopher A, Broach RB, Hsu JY, et al. Reoperation through a prosthetic-reinforced abdominal wall and its association with postoperative outcomes and longitudinal health care utilization. JAMA Surg. (2022) 157(10):908–16. doi: 10.1001/jamasurg.2022.3320
12. Orenstein SB, Qiao Y, Kaur M, Klueh U, Kreutzer DL, Novitsky YW. Human monocyte activation by biologic and biodegradable meshes in vitro. Surg Endosc. (2010) 24(4):805–11. doi: 10.1007/s00464-009-0664-3
13. Kim M, Oommen B, Ross SW, Lincourt AE, Matthews BD, Heniford BT, et al. The current status of biosynthetic mesh for ventral hernia repair. Surg Technol Int. (2014) 25:114–21. 25396323.25396323
14. Sahoo S, Haskins IN, Huang LC, Krpata DM, Derwin KA, Poulose BK, et al. Early wound morbidity after open ventral hernia repair with biosynthetic or polypropylene mesh. J Am Coll Surg. (2017) 225(4):472–80.e1. doi: 10.1016/j.jamcollsurg.2017.07.1067
15. Poulose BK, Roll S, Murphy JW, Matthews BD, Todd Heniford B, Voeller G, et al. Design and implementation of the americas hernia society quality collaborative (AHSQC): improving value in hernia care. Hernia. (2016) 20(2):177–89. doi: 10.1007/s10029-016-1477-7
16. Surgical Site Infection Event Protocol, Centers for Disease Control and Prevention (CDC). https://wwwcdcgov/nhsn/pdfs/pscmanual/9pscssicurrentpdf (Accessed Feb 15, 2017) pp. 1–31.
17. Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF, et al. Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery. (2010) 148(3):544–58. doi: 10.1016/j.surg.2010.01.008
18. Krpata DM, Petro CC, Prabhu AS, Tastaldi L, Zolin S, Fafaj A, et al. Effect of hernia mesh weights on postoperative patient-related and clinical outcomes after open ventral hernia repair: a randomized clinical trial. JAMA Surg. (2021) 156(12):1085–92. doi: 10.1001/jamasurg.2021.4309
19. Ripollone JE, Huybrechts KF, Rothman KJ, Ferguson RE, Franklin JM. Implications of the propensity score matching paradox in pharmacoepidemiology. Am J Epidemiol. (2018) 187(9):1951–61. doi: 10.1093/aje/kwy078
20. Zakrison TL, Austin PC, McCredie VA. A systematic review of propensity score methods in the acute care surgery literature: avoiding the pitfalls and proposing a set of reporting guidelines. Eur J Trauma Emerg Surg. (2018) 44(3):385–95. doi: 10.1007/s00068-017-0786-6
21. Plymale MA, Davenport DL, Dugan A, Zachem A, Roth JS. Ventral hernia repair with poly-4-hydroxybutyrate mesh. Surg Endosc. (2018) 32(4):1689–94. doi: 10.1007/s00464-017-5848-7
22. Wagner V, Levy BE, Castle JT, Plymale M, Roth JS, Totten C. Absorbable mesh in a contaminated field: hernia repair outcomes. Updates Surg. (2023) 75(5):1337–42. doi: 10.1007/s13304-022-01433-z
23. Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. (2015) 313(5):483–95. doi: 10.1001/jama.2014.18614
24. Baltodano PA, Webb-Vargas Y, Soares KC, Hicks CW, Cooney CM, Cornell P, et al. A validated, risk assessment tool for predicting readmission after open ventral hernia repair. Hernia. (2016) 20(1):119–29. doi: 10.1007/s10029-015-1413-2
25. Lovecchio F, Farmer R, Souza J, Khavanin N, Dumanian GA, Kim JY. Risk factors for 30-day readmission in patients undergoing ventral hernia repair. Surgery. (2014) 155(4):702–10. doi: 10.1016/j.surg.2013.12.021
26. Nguyen MT, Li LT, Hicks SC, Davila JA, Suliburk JW, Leong M, et al. Readmission following open ventral hernia repair: incidence, indications, and predictors. Am J Surg. (2013) 206(6):942–8; discussion 948–9. doi: 10.1016/j.amjsurg.2013.08.022
Keywords: hernia recurrence, poly-4-hydroxybutyrate, P4HB, surgical site infection (SSI), umbilical hernia, ventral hernia
Citation: Deeken CR, Rosen MJ, Poulose BK, Bradbury K, Huang L-C, Ma J and Badhwar A (2023) Early wound morbidity and clinical outcomes associated with P4HB mesh compared to permanent synthetic mesh in umbilical and small to medium, routine ventral hernia repairs. Front. Surg. 10:1280991. doi: 10.3389/fsurg.2023.1280991
Received: 21 August 2023; Accepted: 22 September 2023;
Published: 10 October 2023.
Edited by:
Jose Bueno-Lledo, La Fe Hospital, SpainReviewed by:
Luis Tallon-Aguilar, Virgen del Rocío University Hospital, SpainAmaniel Kefleyesus, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland
Giulio Mari, Desio Hospital, Italy
Jason Wink, University of Pennsylvania, United States
© 2023 Deeken, Rosen, Poulose, Bradbury, Huang, Ma and Badhwar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amit Badhwar YW1pdC5iYWRod2FyQGJkLmNvbQ==
 Corey R. Deeken
Corey R. Deeken Michael J. Rosen2
Michael J. Rosen2 Li-Ching Huang
Li-Ching Huang Amit Badhwar
Amit Badhwar