- 1Department of Joint and Orthopedics, Orthopedic Center, Zhujiang Hospital, Southern Medical University, Guangzhou, China
- 2Huiqiao Medical Center, Nanfang Hospital of Southern Medical University, Guangzhou, China
Background: The choice of postoperative weight bearing protocol after uncemented total hip arthroplasty (THA) remains controversial. The aim of this study was to assess the efficacy and safety of immediate unrestricted weight bearing (UWB) compared with partial weight bearing (PWB) in patients undergoing uncemented THA.
Methods: Relevant articles were retrieved from electronic databases. Both randomized controlled trials (RCTs) and non-RCTs were included but analyzed separately. All functional and clinical outcomes with at least 2 independent study outcomes were meta-analyzed.
Results: A total of 17 studies were investigated. No adverse effect was found regarding micromotion of the femoral stem with immediate UWB following uncemented THA. There was also no correlation between immediate UWB and failure of ingrowth fixation and higher risks of femoral stem subsidence and surgical revision in RCTs. Harris hip score was better in patients with immediate UWB than those with PWB at 1 year post surgery, but the difference was not statistically significant.
Conclusions: Immediate UWB did not have extra harm compared with PWB in patients undergoing uncemented THA. UWB was not superior to PWB. Considering the improvement of Harris score and the compliance of patients, UWB can be encouraged in THA rehabilitation.
1. Introduction
Total hip arthroplasty (THA) is the most widely performed procedure for end-stage joint diseases (1). Patient satisfaction-related outcomes, regarding pain relief, functional recovery, and improvement in mobility and quality of life, have been reported by both patients and physicians after THA (2). Cemented and uncemented prostheses are two choices of fixation for THA. Although cemented THA could provide relatively better prognosis for elderly patients (3), increasing early loosening rates have been reported (4, 5). Besides, younger patients who underwent cemented THA have exhibited higher risk of revision due to more exercise (6). Moreover, uncemented or hybrid fixation can improve survivorship in younger patients while cemented fixation are better for older patients (7–9). A recent single-center survival analysis involved 2,156 hips also reveals that uncemented THA show improved survival over cemented at younger ages (10). Thus, the use of uncemented THA has been increasingly recommended in recent years. With the increased in life expectancy along with the change of thresholds for surgery, the number of uncemented THAs is expected to raise more rapidly.
Partial weight bearing (PWB) for 6–12 weeks is still advocated for patients undergoing uncemented THA to create optimal requirements for bone and soft tissue healing as well as to reduce implant failures (11–13). However, this recommendation is frequently based on empirical belief instead of on evidence from the literature. Modern postoperative management is becoming more focused on techniques that facilitate early physiological rehabilitation, including early weight-bearing activities, functional exercises, and muscle exercises. Some studies propose that instead of negative influence on implant stability or clinical results, postoperative immediate unrestricted weight bearing (UWB) could shorten hospital stay, accelerate functional recovery, improve muscle strength, provide higher autonomy, and prevent complications (e.g., deep leg vein thrombosis, urinary tract infections, and pneumonia) (14–17). As to rehabilitation of THA, early postoperative exercise under the premise of safety is well-recognized. However, there is no uniform standard for the degree of weigh bearing. Moreover, it's still unclear that how postoperative weight bearing affect the outcome of THA.
At present, no clear evidence exists on the most optimal physical rehabilitation protocols after uncemented THA, and controversies exist on whether to use UWB or PWB procedures. Thus, the scope of the present meta-analysis was to compare the efficacy and safety of UWB and PWB in patients undergoing uncemented THA, thereby identifying the evidence-based guidelines that can be used in clinical practice.
2. Methods
2.1. Search strategies
The current meta-analysis was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement (18). Comprehensive searches of PubMed, EMBASE, Web of Science, and Cochrane Library were undertaken using Mesh headings and text words for hip arthroplasty and weight bearing. The search terms were kept broad to cover all the possibilities. To expand the search for additional articles of interest, the bibliography of all studies included in this analysis were manually cross-checked. There was no restriction on the publication date or language. All potentially eligible publications were evaluated for inclusion independently by two reviewers based on the title, abstract, and full-text articles when necessary. Conflicts on eligibility were resolved by discussion.
2.2. Selection criteria
Studies were eligible for inclusion if they met the following criteria: (1) comparative studies including randomized controlled trials (RCTs) or cohort studies; (2) all patients who underwent primary uncemented THA, or data from the subgroup with uncemented THA were analyzed separately; (3) comparing the effect between UWB and PWB after uncemented THA. Studies assessing patients with cemented THA or revision of the THA, abstracts, reviews, and case reports, were excluded. In case of duplicate publications with overlapping patient data, only the most recent or informative one was included.
2.3. Data extraction
Relevant information and outcome data were extracted by two reviewers independently according to a predefined standardized form. The items extracted from the included studies were as follows: study originations (first author, publication year, region of experiment), participants (number, age, gender, clinical characteristics, surgical approach, and prosthetic design), interventions (level of weight bearing, use of assistive devices, duration, and follow-up time), and outcomes. All data were checked for missing value, consistency, and validity.
2.4. Quality assessment
Quality assessment was performed using the Physiotherapy Evidence Database (PEDro) scale for RCTs (19) and the index for non-randomized studies (MINORS) form for non-RCTs (20). The PEDro scale is a reliable tool developed to rate the quality of RCTs evaluating physical therapist interventions. It consists of a checklist of 11 criteria, 10 of which are scored. For this analysis, studies with PEDro scores of 6–10 were considered high quality, of 4–5 were considered moderate quality, and of 0 to 3 were considered low quality. The MINORS scale contains 12 items, and the items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate). For this analysis, studies with MINORS scores of 19–24 were considered high quality, of 13–18 were considered moderate quality, and of 0–12 were considered low quality.
2.5. Statistical analysis
Stata software version 15.0 (Stata Corporation, College Station, TX, USA) was used to perform the statistical analyses. Continuous outcomes were pooled as weighted mean difference (WMD) or standard mean difference (SMD) with 95% confidence interval (CI). Dichotomous outcomes were expressed as odds ratio (OR) with 95% CI. Heterogeneity among the included studies was calculated by Chi-squared Q test and I2 statistics. A random-effects model was chosen significant heterogeneity was identified (P value of Q test <0.05 or I2 > 50%). A fixed-effects model was employed if there was no evidence of heterogeneity (P > 0.05 and I2 < 50%). Sensitivity analysis was conducted by removing each study one by one to test if a particular study altered the overall effect or disproportionately contributed to the observed heterogeneity. Both RCTs and non-RCTs were included in the present meta-analysis, outcomes from different study design were pooled separately. Subgroup analysis based on follow-up time was performed when each subgroup contained at least 2 independent study outcomes. Funnel plots were used for testing publication bias when the number of the included studies exceeded ten. A P-value <0.05 was considered statistically significant.
3. Results
3.1. Search results
Overall, electronic database searches led to 1,087 articles after removal of duplicates. Three additional publications were found by reference review. Fifty-seven studies were selected for full-text review. Seventeen studies fulfilling all inclusion criteria and with sufficient outcome data were finally included in the meta-analysis. The process of literature search and study selection were described in Figure 1.
3.2. Study characteristics
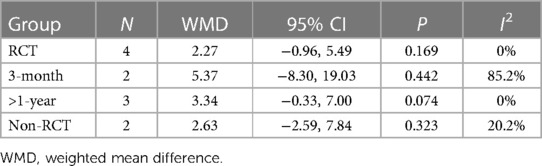
Ultimately, thirteen RCTs and four retrospective studies were eligible for inclusion (15, 16, 21–29). Most of the studies had small sample size ranged from 20 to 100 hips, only one study included more than 100 patients (21). Five studies included patients undergoing unilateral THA, four studies involved both unilateral and bilateral, while the other 10 studies did not give specific information. Surgical approach and hip type were diverse among studies. Although the specific protocols were different, essentially, patients in UWB group were instructed to bear full weight immediately after surgery without external support or with the use of cane only for balance. Patients in PWB group were allowed to bear 20–50 lb of weight for 6 weeks to 3 months using crutches. Detailed weight bearing protocols and study information were presented in Table 1. According to the quality assessment results, all the included studies obtained moderate to high quality. Distributions of quality assessment in each study were presented in Supplementary Table 1.
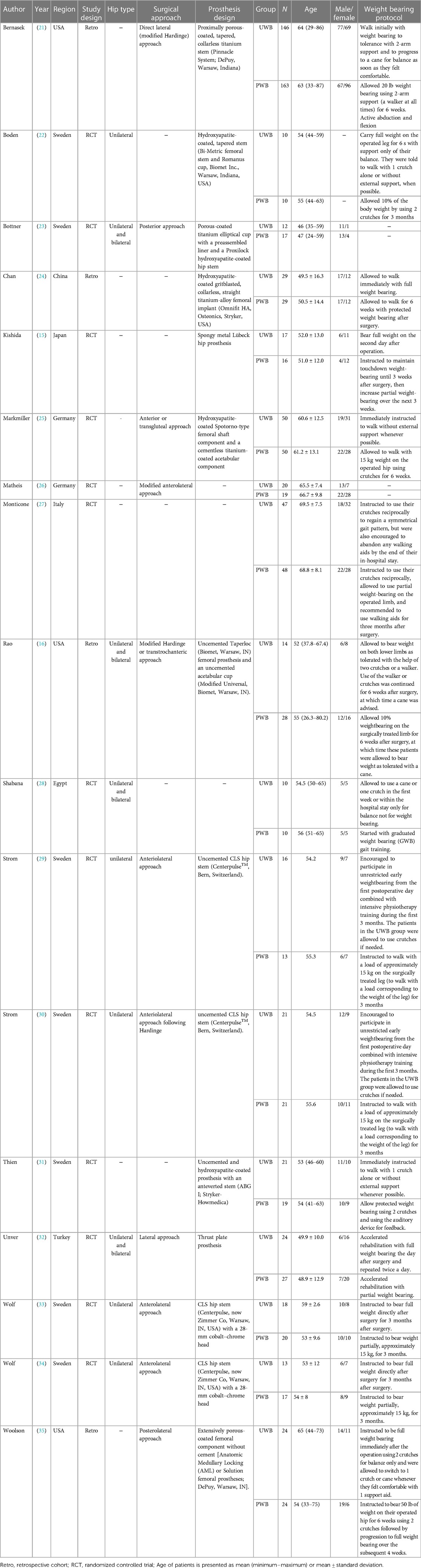
Table 1. Characteristics of included trials comparing UWB to PWB for postoperative rehabilitation of THA.
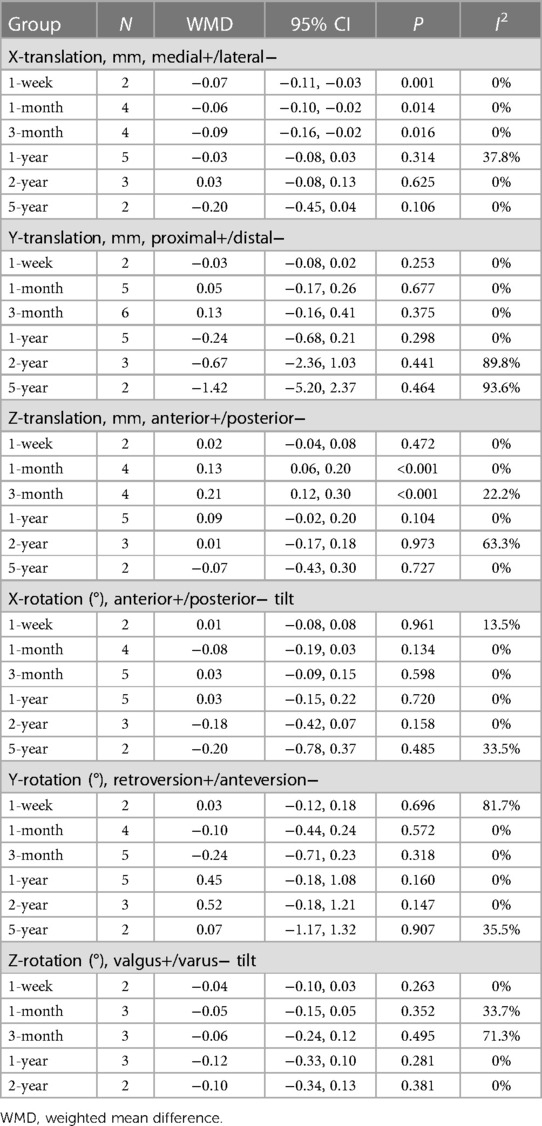
3.3. Stem micromotion
Migration of stem was measured in five studies using radiostereometric analysis (RSA). Significant difference between the UWB and PWB groups occurred at 1-week, 1-month, and 3-month, as a difference in the medial (+) or lateral (–) migration of the stem, as well as at 1-month and 3-month follow-up in anterior (+) or posterior (–) migration of the stem (Table 2). There was no significant difference in proximal (+) or distal (–) subsidence of the stem between groups; nor was there any significant difference in anterior or posterior tilt, retroversion or anteversion, and valgus or varus tilt between groups (Table 2).
3.4. Stem stability
Bone ingrowth fixation was evaluated in four RCTs and three non-RCTs based on the Engh criteria (36). Overall, the incidence of bone ingrowth fixation did not differ significantly between the UWB and PWB groups. As to RCTs, Markmiller et al. and Bottner et al. find that all cases achieve bone ingrowth fixation (23, 25). Bodén et al. shows that the bone ingrowth fixation rate is 90% in both UWB and PWB groups (22). In non-RCTs, bone ingrowth occurs in all three researches.
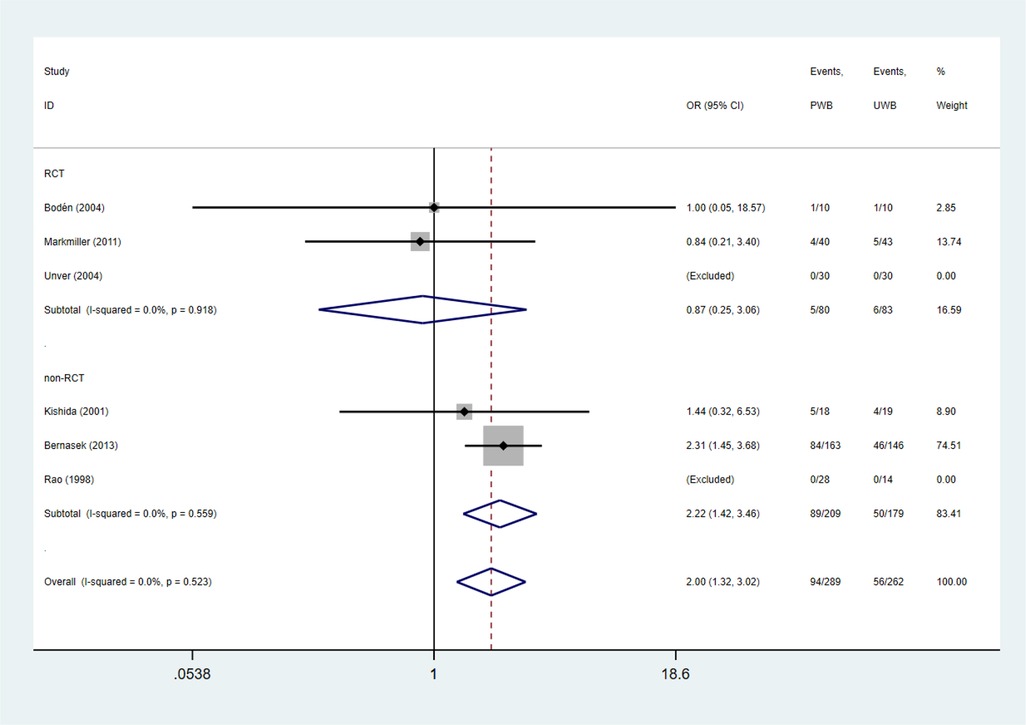
Radiolucent lines were assessed in three RCTs and non-RCTs, respectively. The incidence of radiolucent lines was higher in UWB group than that in PWB group in non-RCTs (OR = 2.22, 95% CI, 1.42, 3.46; P = 0.00; I2 = 0%). However, in RCTs with more rigorous design, no significant difference was found between groups (OR = 0.87, 95% CI, 0.25, 3.06; P = 0.830; I2 = 0%; Table 3 and Figure 2).
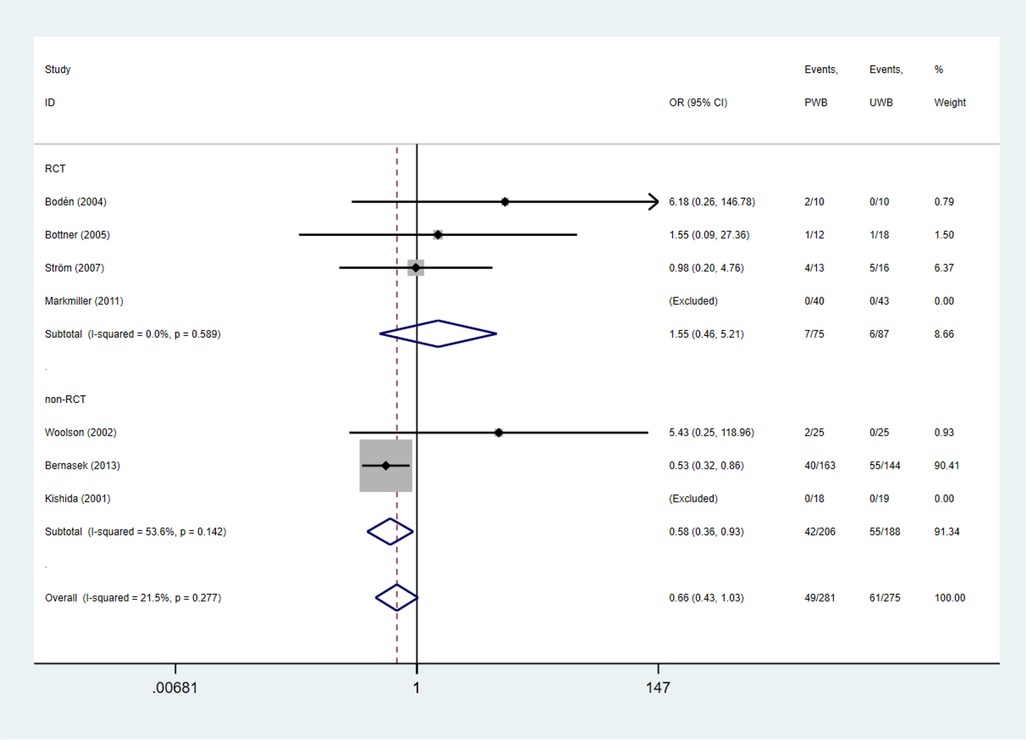
Femoral component subsidence (>1 mm) was evaluated in four RCTs and three non-RCTs. The incidence of femoral component subsidence (>1 mm) did not differ significantly between the UWB and PWB groups (RCTs: OR = 1.55, 95% CI, 0.46, 5.21; P = 0.477; I2 = 0%). Whereas, UWB group exhibited a lower incidence of femoral component subsidence relative to PWB group in non-RCTs (OR = 0.58, 95% CI, 0.36, 0.93; P = 0.023; I2 = 53.6%; Table 3 and Figure 3).
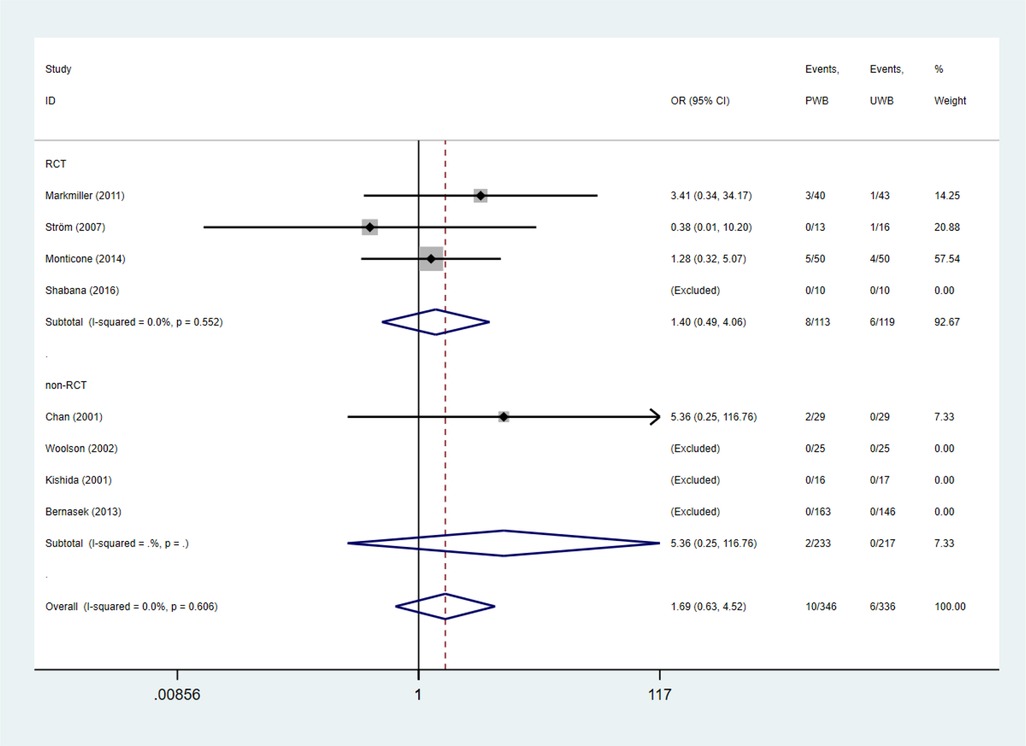
3.5. Complications
The incidences of symptomatic deep venous thrombosis, infection, dislocation, and surgical revision were also estimated (37). No significant difference was found between the UWB and PWB groups regarding the abovementioned complication (Table 4 and Figure 4).
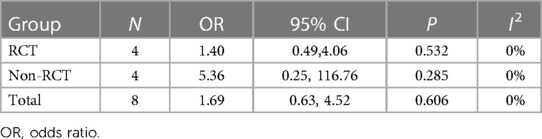
Table 4. Mean differences (95% CI) for postoperative complications in trials accessing the safety of UWB versus PWB.
3.6. Harris Hip score
Four RCTs and two retrospective studies provided enough data to calculate the difference between pre- and postoperative Harris hip score. Pooled results showed that UWB group improved Harris hip score by 2.27 (95% CI, −0.96, 5.49; P = 0.169; I2 = 0%) in RCTs and by 2.63 (95% CI, −2.59, 7.84; P = 0.323; I2 = 20.2%) in non-RCTs compared with PWB group (Table 5). However, the improvement did not reach statistical significance.
Subgroup analysis was conducted with data from RCTs. No significant difference was found between UWB and PWB groups in Harris hip score at 3-month and ≥1-year follow-up (Table 5).
3.7. Sensitivity analysis
Sensitivity analysis was performed in all assessed outcomes. In all parameters, no individual study was found to alter the direction and size of the overall effect size.
4. Discussion
The optimum form of postoperative weight bearing protocol after uncemented THA remains controversial. It is concerned that PWB following uncemented THA may inhibit functional recovery and increase the risk of complications (9, 38), whereas UWB may cause micromovement at the bone-implant interface, jeopardizing stability, and ingrowth of implant (39). By integrating data from 17 studies, this meta-analysis established some levels of evidence to support the use of immediate UWB after uncemented THA. There was no statistically significant difference between UWB and PWB groups regarding micromotion of the femoral stem, ingrowth fixation, femoral component subsidence, revision, and complications. In RCTs, the outcome of Harris hip score in the UWB group was better than that in the PWB group at 1 year post surgery, but the difference was not statistically significant (P = 0.074).
A previous meta-analysis shows greater proximal or distal femoral stem subsidence in UWB compared with PWB groups at 3-month follow-up (40), which is contradict with our findings. In the analysis of femoral stem micromotion, the present study only included RCTs, and analyzed data of the CLS femoral stem along and around the three axes measured with RSA. Whereas Tian et al. integrated both RCTs and non-RCTs, and included data measured with conventional radiographs (41). Thus, our study may be more validity. In addition, significant differences were found in medial or lateral translation and anterior or posterior translation at 1- and 3-month follow-up, while these significant differences did not maintain at further measurement. The initial stability of the uncemented implants is dependent on the mechanical match between the prosthetic stem and the intramedullary canal. The long-term stability is determined by mechanical fit and bone ingrowth (25). If the initial mechanical match has not been achieved, the femoral stem prosthesis will descend along the medullary cavity in the weight bearing activities until a tight matching occur (16). Thus, in the first postoperative three months, the higher femoral subsidences of patients in the UWB group might be because the prosthesis and the medullary cavity did not achieve the best matching. When the weight bearing increased gradually in the PWB group, the femoral stem subsidence began to catch up, and thus the femoral subsidences of the two groups tended to be consistent at one or more years after THA.
Femoral stem subsidence greater than 1–1.5 mm during the first two years after uncemented THA has been shown to predict an increased risk of early or midterm revision (29). In this meta-analysis, we showed that there was no significant difference of the test results of UWB compared with PWB groups in the incidences of femoral component subsidence (>1 mm), and subsequently the incidences of revision in four RCTs. These findings added support for allowing UWB after uncemented THA.
Several included studies use an auditory device calibrated to between 10% of body weight to 30 kg of loading to instruct the patients (22, 29–31, 33, 34). However, some patients do not strictly follow the instruction to full extent. In some studies, patients in the PWB group put almost twice the recommended weight on the operated leg (29, 33, 34). This might contribute to the insignificant test results between UWB and PWB groups. Thus, further studies with more rigorous design are needed to verify our findings.
Several potential limitations should be noted. Publication bias could not be tested by Deeks funnel plot and Egger's asymmetry testing due to extremely limited number of studies in each outcome. Although 17 publications were included, some of the analyses only involved a small number of studies with small sample sizes, which might be insufficient to draw definite conclusion. The influence of some confounding factors, which have been suggested to be important factors in stability and ingrowth (i.e., such as prosthesis design (16, 42, 43), surgical approach (21, 36), and the use and duration of assistive devices (12, 32)), could not be controlled due to limited amount of data. Thus, results from the present meta-analysis should be interpreted with caution. Future prospective, multi-institutional, well-designed trials with larger sample size are needed to testify our results.
Several reasons may be responsible for the limited investigations on the effects of immediate UWB after uncemented THA. There is inherent fear that allowing patients to bear weight unrestrictedly may lead to higher risk of subsidence and revision. Thus, it may seem unethical to randomize patients between groups with different weight bearing regimes if the risk of one group is a failure of fixation. The current meta-analysis revealed no statistically significant evidence of additional harm of immediate UWB after uncemented THA. This finding may eliminate some of the doubt of immediate UWB after uncemented THA, and provide evidence-based support to encourage more future studies on this topic.
5. Conclusion
In conclusion, within the current literature, immediate UWB did not have extra harm and might have potential benefit in functional outcomes compared with PWB in patients who underwent uncemented THA. UWB was not superior to PWB. Considering the improvement of Harris score and the compliance of patients, UWB can be encouraged in THA rehabilitation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
LH, WH, and DZ conceived and designed the analysis; WQ and XZ acquired the data; WQ and ZL analyzed and interpreted the data; LH, WH, and YL drafted and revised the article; All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1225649/full#supplementary-material
References
1. Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet (London, England). (2012) 380(9855):1768–77. doi: 10.1016/S0140-6736(12)60607-2
2. Judge A, Arden NK, Kiran A, Price A, Javaid MK, Beard D, et al. Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Joint Surg Br. (2012) 94(3):412–8. doi: 10.1302/0301-620X.94B3.27425
3. Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PloS one. (2013) 8(7):e68903. doi: 10.1371/journal.pone.0068903
4. Meding JB, Ritter MA, Davis KE, Hillery M. Cemented and uncemented total hip arthroplasty using the same femoral component. Hip Int. (2016) 26(1):62–6. doi: 10.5301/hipint.5000296
5. González-Bravo C, Ortega MA, Buján J. Wear risk prevention and reduction in total hip arthroplasty. A personalized study comparing cement and cementless fixation techniques employing finite element analysis. J Pers Med. (2021) 11(8):780. doi: 10.3390/jpm11080780
6. Gromov K, Pedersen AB, Overgaard S, Gebuhr P, Malchau H, Troelsen A. Do rerevision rates differ after first-time revision of primary THA with a cemented and cementless femoral component? Clin Orthop Relat Res. (2015) 473(11):3391–8. doi: 10.1007/s11999-015-4245-6
7. Gwynne-Jones DP, Lash HWR, James AW. The morscher press-fit acetabular component: an independent long-term review at 18-22 years. J Arthroplasty. (2017) 32(8):2444–9. doi: 10.1016/j.arth.2017.02.052
8. Hallan G, Dybvik E, Furnes O, Havelin LI. Metal-backed acetabular components with conventional polyethylene: a review of 9113 primary components with a follow-up of 20 years. J Bone Joint Surg Br. (2010) 92(2):196–201. doi: 10.1302/0301-620X.92B2.22179
9. Hook S, Moulder E, Yates PJ, Burston BJ. The exeter universal stem: a minimum ten-year review from an independent centre. J Bone Joint Surg Br. (2006) 88(12):1584–90. doi: 10.1302/0301-620X.88B12.18345
10. Fowler A-K, Gray AR, Gwynne-Jones DP. Hybrid fixation for total hip arthroplasty showed improved survival over cemented and uncemented fixation: a single-center survival analysis of 2156 hips at 12−18 years. J Arthroplasty. (2019) 34(11):2711–7. doi: 10.1016/j.arth.2019.06.031
11. Youm T, Maurer SG, Stuchin SA. Postoperative management after total hip and knee arthroplasty. J Arthroplasty. (2005) 20(3):322–4. doi: 10.1016/j.arth.2004.04.015
12. Hol AM, van Grinsven S, Lucas C, van Susante JL, van Loon CJ. Partial versus unrestricted weight bearing after an uncemented femoral stem in total hip arthroplasty: recommendation of a concise rehabilitation protocol from a systematic review of the literature. Arch Orthop Trauma Surg. (2010) 130(4):547–55. doi: 10.1007/s00402-009-1017-3
13. Moreno-Romero M, Ordas-Bayon A, Gomez-Rice A. Partial two-stage exchange for infected total hip arthroplasty: a treatment to take into account. J Pers Med. (2023) 13(1):137. doi: 10.3390/jpm13010137
14. Eisele R, Weickert E, Eren A, Kinzl L. The effect of partial and full weight-bearing on venous return in the lower limb. J Bone Joint Surg Br. (2001) 83(7):1037–40. doi: 10.1302/0301-620X.83B7.0831037
15. Kishida Y, Sugano N, Sakai T, Nishii T, Haraguchi K, Ohzono K, et al. Full weight-bearing after cementless total hip arthroplasty. Int Orthop. (2001) 25(1):25–8. doi: 10.1007/s002640000221
16. Rao RR, Sharkey PF, Hozack WJ, Eng K, Rothman RH. Immediate weightbearing after uncemented total hip arthroplasty. Clin Orthop Relat Res. (1998) 349:156–62. doi: 10.1097/00003086-199804000-00019
17. Barker KL, Newman MA, Hughes T, Sackley C, Pandit H, Kiran A, et al. Recovery of function following hip resurfacing arthroplasty: a randomized controlled trial comparing an accelerated versus standard physiotherapy rehabilitation programme. Clin Rehabil. (2013) 27(9):771–84. doi: 10.1177/0269215513478437
18. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. (2009) 339:b2700. doi: 10.1136/bmj.b2700
19. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. (2003) 83(8):713–21. doi: 10.1093/ptj/83.8.713
20. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x
21. Bernasek TL, Thatimatla NK, Levering M, Haidukewych GJ. Effect of immediate full weight bearing on abductor repair and clinical function after THA through a modified hardinge approach. Orthopedics. (2013) 36(3):e266–70. doi: 10.3928/01477447-20130222-12
22. Bodén H, Adolphson P. No adverse effects of early weight bearing after uncemented total hip arthroplasty: a randomized study of 20 patients. Acta Orthop Scand. (2004) 75(1):21–9. doi: 10.1080/00016470410001708040
23. Bottner F, Zawadsky M, Su EP, Bostrom M, Palm L, Ryd L, et al. Implant migration after early weightbearing in cementless hip replacement. Clin Orthop Relat Res. (2005) 436:132–7. doi: 10.1097/01.blo.0000160380.15429.fb
24. Chan YK, Chiu KY, Yip DK, Ng TP, Tang WM. Full weight bearing after non-cemented total hip replacement is compatible with satisfactory results. Int Orthop. (2003) 27(2):94–7. doi: 10.1007/s00264-002-0419-4
25. Markmiller M, Weiss T, Kreuz P, Rüter A, Konrad G. Partial weightbearing is not necessary after cementless total hip arthroplasty: a two-year prospective randomized study on 100 patients. Int Orthop. (2011) 35(8):1139–43. doi: 10.1007/s00264-010-1089-2
26. Matheis C, Stöggl T. Strength and mobilization training within the first week following total hip arthroplasty. J Bodyw Mov Ther. (2018) 22(2):519–27. doi: 10.1016/j.jbmt.2017.06.012
27. Monticone M, Ambrosini E, Rocca B, Lorenzon C, Ferrante S, Zatti G. Task-oriented exercises and early full weight-bearing contribute to improving disability after total hip replacement: a randomized controlled trial. Clin Rehabil. (2014) 28(7):658–68. doi: 10.1177/0269215513519342
28. Shabana M, Hafez MA, Ayad K, Abd Elfatah M, Zaky LA. Immediate unrestricted versus graduated weight bearing following primary cementless total hip arthroplasty: a randomized controlled trial. Ann Joint. (2017) 2(2):6. doi: 10.21037/aoj.2017.01.03
29. Ström H, Nilsson O, Milbrink J, Mallmin H, Larsson S. Early migration pattern of the uncemented CLS stem in total hip arthroplasties. Clin Orthop Relat Res. (2007) 454:127–32. doi: 10.1097/01.blo.0000238785.98606.9d
30. Ström H, Nilsson O, Milbrink J, Mallmin H, Larsson S. The effect of early weight bearing on migration pattern of the uncemented CLS stem in total hip arthroplasty. J Arthroplasty. (2007) 22(8):1122–9. doi: 10.1016/j.arth.2006.11.015
31. Thien TM, Ahnfelt L, Eriksson M, Strömberg C, Kärrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop. (2007) 78(6):730–8. doi: 10.1080/17453670710014491
32. Unver B, Karatosun V, Gunal I, Angin S. Comparison of two different rehabilitation programmes for thrust plate prosthesis: a randomized controlled study. Clin Rehabil. (2004) 18(1):84–91. doi: 10.1191/0269215504cr705oa
33. Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H. Periprosthetic bone mineral density and fixation of the uncemented CLS stem related to different weight bearing regimes: a randomized study using DXA and RSA in 38 patients followed for 5 years. Acta Orthop. (2010) 81(3):286–91. doi: 10.3109/17453674.2010.487238
34. Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H. The effects of different weight-bearing regimes on press-fit cup stability: a randomised study with five years of follow-up using radiostereometry. Int Orthop. (2012) 36(4):735–40. doi: 10.1007/s00264-011-1413-5
35. Woolson ST, Adler NS. The effect of partial or full weight bearing ambulation after cementless total hip arthroplasty. J Arthroplasty. (2002) 17(7):820–5. doi: 10.1054/arth.2002.34809
36. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. (1987) 69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732
37. De la Torre-Escuredo B, Gómez-García E, Álvarez-Villar S. Bone impaction grafting with trabecular metal augments in large defects in young patients: unravelling a new perspective in surgical technique. BMC Musculoskelet Disord. (2020) 21(1):581. doi: 10.1186/s12891-020-03591-w
38. Leali A, Fetto J, Moroz A. Prevention of thromboembolic disease after non-cemented hip arthroplasty. A multimodal approach. Acta Orthop Belg. (2002) 68(2):128–34.12050997
39. Radl R, Aigner C, Hungerford M, Pascher A, Windhager R. Proximal femoral bone loss and increased rate of fracture with a proximally hydroxyapatite-coated femoral component. J Bone Joint Surg Br. (2000) 82(8):1151–5. doi: 10.1302/0301-620X.82B8.0821151
40. Tian P, Li ZJ, Xu GJ, Sun XL, Ma XL. Partial versus early full weight bearing after uncemented total hip arthroplasty: a meta-analysis. J Orthop Surg Res. (2017) 12(1):31. doi: 10.1186/s13018-017-0527-x
41. De la Torre B, Barrios L, De la Torre-Mosquera J. Analysis of the risk of wear on cemented and uncemented polyethylene liners according to different variables in hip arthroplasty. Materials (Basel). (2021) 14(23):7243. doi: 10.3390/ma14237243
42. Rahmy AI, Tonino AJ, Tan WD. Quantitative analysis of technetium−99m-methylene diphosphonate uptake in unilateral hydroxyapatite-coated total hip prostheses: first year of follow-up. J Nucl Med. (1994) 35(11):1788–91. doi: 10.1097/00004728-199411000-00034
Keywords: total hip arthroplasty, uncemented, partial weight bearing, unrestricted weight bearing, rehabilitation
Citation: Huang L, Han W, Qi W, Zhang X, Lv Z, Lu Y and Zou D (2023) Early unrestricted vs. partial weight bearing after uncemented total hip arthroplasty: a systematic review and meta-analysis. Front. Surg. 10:1225649. doi: 10.3389/fsurg.2023.1225649
Received: 19 May 2023; Accepted: 31 October 2023;
Published: 15 November 2023.
Edited by:
Andrew Robert Gray, University of Otago, New Zealand© 2023 Huang, Han, Qi, Zhang, Lv, Lu and Zou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yao Lu b2F5dWxAc211LmVkdS5jbg== Danfeng Zou MTM2MDkwNjA2MzZAMTM5LmNvbQ==
 Li Huang1
Li Huang1 Yao Lu
Yao Lu