
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 15 December 2023
Sec. Orthopedic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1215280
This article is part of the Research TopicModern Advances in ArthroplastyView all 9 articles
Introduction: Robotic-arm assisted medial unicompartmental knee arthroplasty (RA-UKA) is associated with improved accuracy of implant positioning and excellent early functional outcomes. However, there is paucity of evidence regarding outcomes following RA-UKA for isolated lateral compartment osteoarthritis. The purpose of this study was to assess the short-term clinical and patient reported outcomes of lateral compartment UKA, utilising robotic-arm assistance.
Methods: This was a retrospective study of prospectively collected data of 21 consecutive patients who underwent lateral RA-UKA. The study included 9 (42.9%) males and 12 (57.1%) females with a mean age of 63.4 ± 9.2 years. The Oxford Knee Score (OKS) was measured pre-operatively and at 1-year post-operatively, while range of motion (ROM) and complications were also recorded.
Results: There was significant improvement of OKS at 1 year's follow up compared with the baseline score (21.8 ± 5.6 vs. 45.2 ± 2.8 respectively; p < 0.001). There was also an improvement in pre-operative ROM when compared to ROM at 1 year's follow up (123.5° ± 8° vs. 131.5° ± 6.3° respectively; p < 0.001). None of the study patients underwent revision surgery within 1 year's follow-up.
Conclusion: In our study, lateral RA-UKA resulted in significant improvements in clinical and patient reported outcomes with low complications rates. Further long-term comparative studies are needed to assess the utility of lateral RA-UKA vs. conventional UKA.
Total knee arthroplasty (TKA) represents a successful and effective form of treatment for patients suffering with end-stage arthritis of the knee (1). However, a significant proportion of these patients have disease, isolated to a single compartment of the knee. It has previously been reported that over 40% of patients who undergo TKA would be suitable for a unicompartmental knee arthroplasty (UKA) (2). UKA is less invasive than TKA with preservation of the unaffected compartments and ligamentous structures (3). There is strong evidence to suggest superior outcomes can be achieved compared to total knee arthroplasty (TKA) in relation to safety, cost-effectiveness and patient-reported outcomes, particularly in patients with severe comorbidities (1, 4–6). However, it is not without limitations; although there are fewer early post-operative complications (7, 8), UKA is associated with higher revision rates than TKA, yet it is not clear whether this is related to advancement of the disease or implant failure (9). Nonetheless, even when incorporating revision costs, UKA maintains a lower overall mean healthcare cost than TKA at 10 years post-operatively, accentuating its value in reducing the financial burden on healthcare systems in an era of an aging population (10).
Lateral compartment UKA is far less frequent compared to medial UKA owing to the medial compartment being associated with a higher incidence of osteoarthritis and osteonecrosis (11). Due to the anatomical and kinematic differences between the medial and lateral compartments, implants used for medial UKA may not be suitable for lateral UKA (12, 13). Moreover, the less constrained nature of the lateral compartment increases the technical complexity of performing a lateral UKA. The lateral flexion gap is greater than the extension gap, and there is increased lateral-sided laxity compared to the more constrained medial compartment (13–15). This increases the risk of bearing dislocation when mobile bearing implants are utilised (13, 16). However, advancement of surgical techniques and implant design have resulted in reduced rates of dislocations associated with lateral UKAs (17, 18). Due to the infrequency of lateral UKA being performed, there is a paucity of evidence on long-term survivorship, however mid-term results are very encouraging with studies reporting up to 100% survivorship (19, 20).
The evolution of surgical technology has resulted in the development of robotic-arm assistance, aiming to increase the precision and accuracy of bone cuts in order to enhance component alignment, optimise soft tissue balance, minimise surgical trauma and improve reproducibility of component placement (21–25). The use of a robotic arm for UKA has been shown to improve limb alignment and component positioning, reduce peri-operative pain, improve functional recovery, and reduce time to discharge compared with conventional jig-based knee arthroplasty (24, 26–31). The aim of this study was to assess clinical and patient reported outcomes following robotic-arm assisted lateral UKA (RA-UKA).
A total of 21 patients that underwent lateral RA-UKA were included in this study. Data was retrospectively analysed from a prospectively collected database. All procedures were performed at a single tertiary referral centre. Inclusion criteria included all patients that underwent lateral RA-UKA with a minimum follow-up time of 1 year. All procedures were conducted using the MAKO Robotic Arm Interactive Orthopaedic System (Mako Surgical Corporation, Kalamazoo, MI, USA). The MAKO protocol involves the generation of a three-dimensional reconstruction model of the patient's knee, based on a pre-operative computer tomography (CT) scan. This model is then uploaded into the MAKO system's software, enabling the development of a personalised pre-operative plan and implant templating (Figure 1). All patients received the Restoris MCK Partial Knee implant (Mako Surgical Corporation, Kalamazoo, MI, USA). Patient demographic data included age, gender, body mass index (BMI) and American Society of Anaesthesiologists (ASA) grade. Patient reported and clinical outcomes were assessed using pre-operative and 1-year post-operative Oxford Knee Scores (OKS) and range of motion (ROM). Passive ROM was measured using a goniometer with the patient in a supine position.
All procedures were performed via a medial parapatellar approach with a medial arthrotomy that provides optimal access for the intra-incisional pin placement. This approach also allows access to other knee compartments and is preferred for revision surgery. Placement of the navigation pins for the femoral and tibial arrays were done within the original incision, which negated the necessity for separate incisions, potentially bearing further morbidity. Two bicortical femoral pins were placed anteromedially at the distal femoral shaft, avoiding the anterior aspect of the femoral component. The two bicortical tibial reference pins were placed at the level of the tibial tubercle, distal to the tibial tray. Following array placement, enabling intra-operative measurement of the alignment and kinematics; bone registration was performed by mapping knee landmarks displayed on the robotic system's screen. To achieve optimal ligament balancing, the knee was positioned in a comfortable position in space, partially correcting the valgus deformity while being mindful of avoiding overcorrection. We aimed to achieve lower limb alignment in the individual's constitutional alignment. Through careful observation of kinematics alignment and visualization of tracking, adjustments were made to the plan as needed in order to attain the desired alignment. Bone resection was performed within haptic boundaries using a high-speed oscillating saw and a burr. Optical motion capture technology was utilised for the assessment of flexion-extension gaps, limb alignment, ligamentous laxity and ROM with trial implants inserted. Once the implants had been chosen based on pre-operative planning and intra-operative trialling, the definitive fixed bearing Restoris MCK implants were cemented (Figure 2).
Twenty-one patients who underwent lateral RA-UKA and had minimum 1 year follow-up were included in the study. There were 9 (42.9%) males and 12 (57.1%) females. The mean age of the study cohort was 63.4 ± 9.2 years (range 51–80 years). Mean BMI was 32.4 ± 4.3. Two thirds of the study participants were classified as ASA II, while nearly a quarter were classified as ASA III (Table 1). Mean pre-operative valgus alignment measured on AP radiographs was 8.8 ± 2.6° (range 5–15°) (Table 1).
Lateral RA-UKA was associated with a statistically significant improvement in PROMs as measured by the OKS at 1 year's follow up (21.8 ± 5.6 pre-operatively vs. 45.2 ± 2.8 at 1 year's follow up, p < 0.001). The mean difference in OKS during the study was 23.4 ± 4.2. Figure 3 illustrates a box plot of the delta-OKS values. A statistically significant improvement in ROM post-operatively was also evident at the 1-year post-operative timepoint (mean pre-operative flexion of 123.5° ± 8° vs. 131.5° ± 6.3° at 1 year follow up; p < 0.001) (Table 2). Mean delta-ROM was 8° ± 5° (Figure 4).
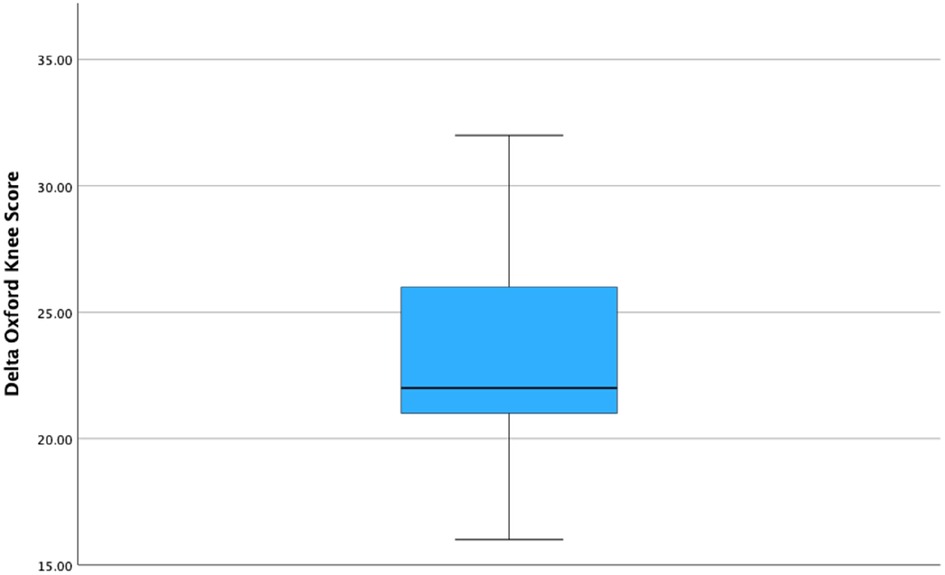
Figure 3. Boxplot, illustrating the delta Oxford knee score among patient undergoing robotic-arm assisted UKA.
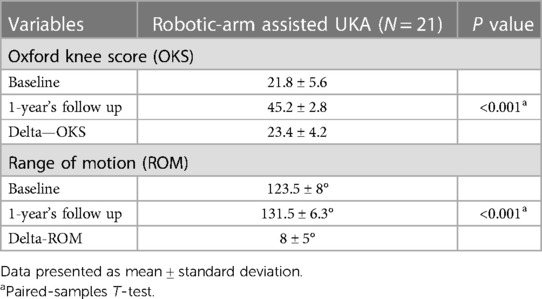
Table 2. Table depicting patient reported outcome measures and range of motion pre-operatively and at one year follow-up.
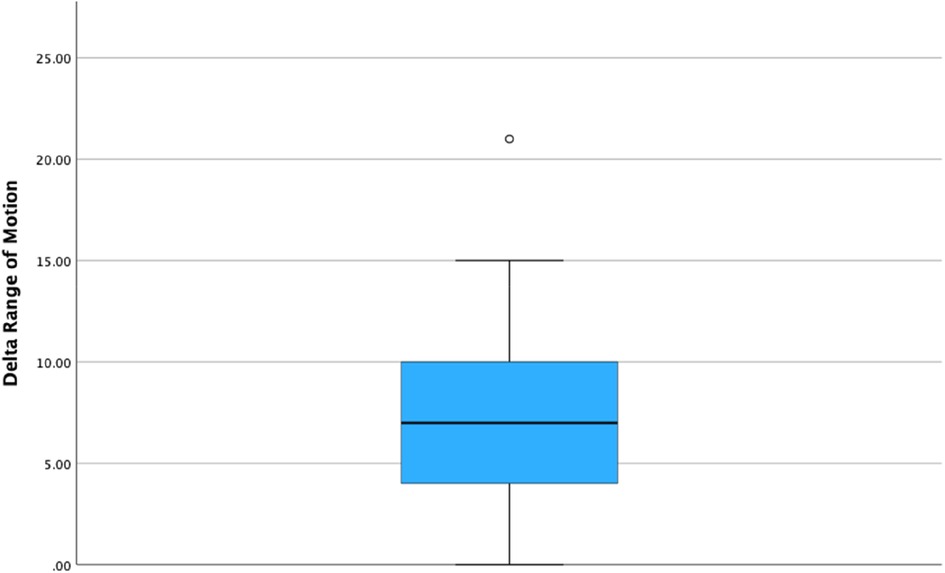
Figure 4. Figure illustrating the delta range of motion among patient undergoing roboticarm assisted UKA.
Correlational analyses did not reveal any significant relationship between pre-operative valgus deformity and Delta-OKS or Delta-ROM (Table 3). Furthermore, no significant correlation was evident between the delta-ROM and delta-OKS (Table 3 and Figures 5–7 illustrate).
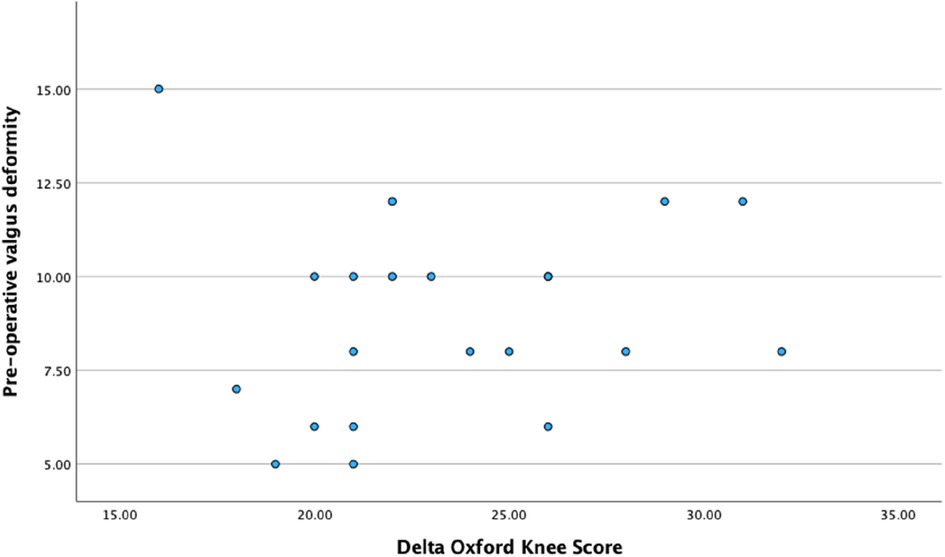
Figure 5. Scatter plot illustrating the relationship between pre-operative valgus deformity and delta Oxford knee score.
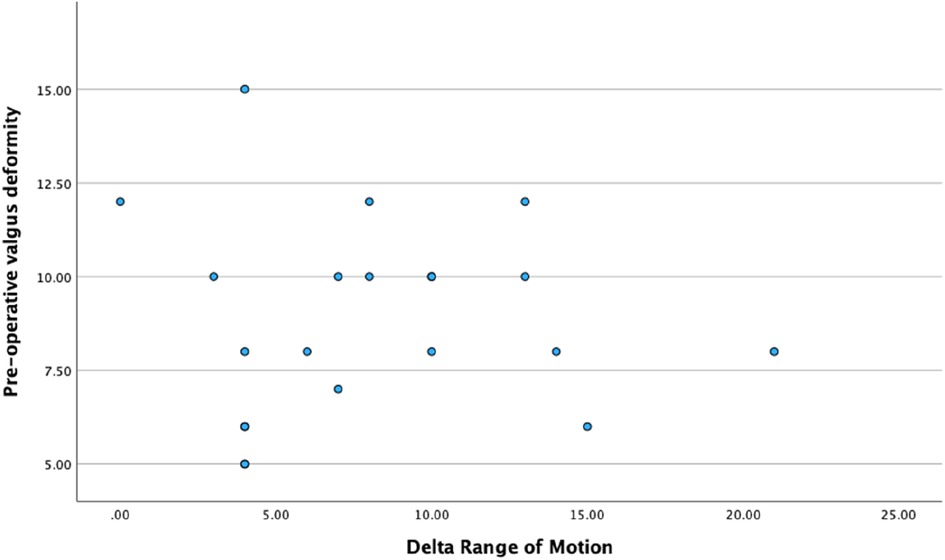
Figure 6. Scatter plot illustrating the relationship between pre-operative valgus deformity and delta range of motion.
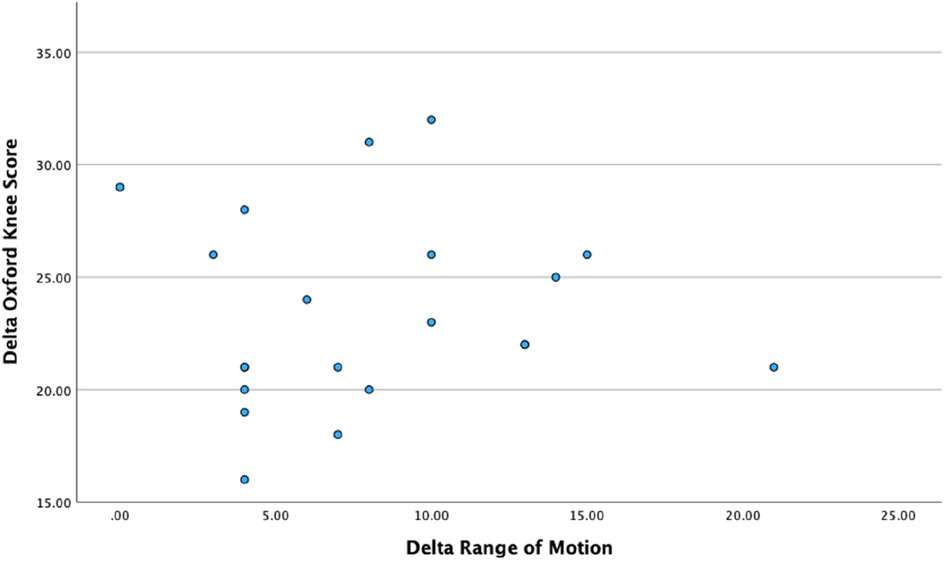
Figure 7. Scatter plot illustrating the relationship between delta range of motion and delta Oxford knee score.
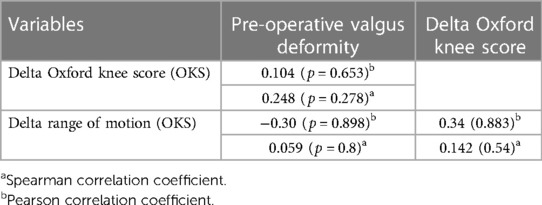
Table 3. Correlation among delta Oxford knee score, range of motion and pre-operative valgus deformity.
Following the application of varus stress to bring the knee into its native alignment, ligament balancing was assessed across various flexion-extension cycles. The robotic system provides real-time feedback regarding ligament balancing, depicted as the deviation in millimetres (mm) from the optimal tracking of the prosthesis at different angles. Negative values signify ligamentous tightness and positive values represent laxity. Figure 8 depicts the intra-operative balancing graph for one of the study's participants, spanning from full extension to beyond 90° of flexion. Among the 21 patients in this study, we noted the mean laxity in extension was 0.5 ± 0.4 mm; at 30° flexion 0.8 ± 0.4 mm; at 60° flexion 1.3 ± 0.6 mm; and at 90° flexion 1.6 ± 0.7 mm.
None of the patients in our study cohort required revision surgery. One patient developed a superficial infection post-operatively which resolved following oral antibiotic treatment. No other complications or issues were recorded during the recovery phase or at the post-operative follow up appointments.
Lateral UKA is a more demanding and technically challenging procedure compared to medial UKA. The introduction of robotic-arm assistance provides the opportunity to create an elaborate and personalised pre-operative plan, in addition to evaluating knee kinematics and alignment intra-operatively. Given the complexities of UKA and potential consequence of errors, the aim of our study was to assess the clinical and patient reported outcomes utilising robotic-arm assistance. We found that lateral RA-UKA resulted in significant improvement of functional outcomes, using ROM and OKS as surrogate measures.
Our findings are in concordance with previous studies. Burger et al., in their study encompassing 171 lateral RA-UKAs, reported an improvement in Knee Injury and Osteoarthritis Outcome Scores (KOOS) and excellent mid-term survivorship (32). Authors also reported a mean Forgotten Joint Score (FJS) of 81 at 2 years' follow up. Excellent KOOS scores were also reported by another study, with a mean improvement of 54 points at 3 years following lateral RA-UKA (33). This study also reported superior mean FJS scores (85.1) (33). Canetti et al. studied return to sporting activity between patients undergoing lateral RA-UKA compared with lateral UKA using the conventional technique at mean follow up of just over 3 years (34). Authors reported that lateral RA-UKA was associated with a significantly quicker return to sports compared with the conventional technique (4.2 ± 1.8 months vs. 10.5 ± 6.7 months). Favourable outcomes with the utilisation of robotic-arm assistance in lateral UKA have been reported by several other studies (35–40), showcasing the positive impact of precise bone cuts and accurate implant positioning.
With respect to correlational analyses, no significant relationship was illustrated between pre-operative valgus deformity, Delta-ROM and Delta-OKS. A possible explanation could involve our small sample size. However, an alternative interpretation could embrace the fact that robotic arm-assistance consistently led to significant improvement in PROMs and functional outcomes. This highlights that the severity of the pre-operative valgus deformity did not influence improvements seen in ROM and PROMs, thus emphasising the reproducibility of outcomes using robotic technology. Heckmann et al. evaluated the mid-term outcomes of 84 patients who underwent lateral RA-UKA and also found no correlation between degree of correction and PROMs in their study (36), further highlighting the reliability and reproducibility of using a robotic arm. Interestingly, this study also included four patients with well-controlled inflammatory arthritis without any reported complications.
Van der List et al. assessed PROMs in patients undergoing medial (143 knees) vs. lateral (36 knees) RA-UKA and found no significant differences in Western Ontario and McMaster University Arthritis (WOMAC) scores or FJS (37). Interestingly, authors reported that optimal alignment differed between the two groups. Patients in the medial RA-UKA group in whom neutral alignment was achieved (−1° to −3°), demonstrated superior FJS. Whereas, in the lateral RA-UKA cohort, superior FJS and WOMAC scores were seen with slight under-correction (3°–7°) (37). Khamsaisy et al. found that there was an increased risk of overcorrection as well as a greater difficulty in predicting post-operative alignment when performing lateral RA-UKA compared to medial RA-UKA (35).The intrinsic laxity of the lateral compartment may explain the increased risk of overcorrection during lateral UKA, highlighting the importance of being mindful of the soft tissue differences between the medial and lateral compartments when performing lateral UKA.
Although our study reports on the short-term results of lateral RA-UKA, studies in the literature have portrayed positive results with regards to longer-term survivorship of lateral RA-UKA. Zambianchi et al. reported 100% survivorship of the 67 lateral RA-UKA performed with mean follow up of 36.3 months (33). Thein et al. and Batallier et al. also reported 100% survivorship in their short-term studies analysing lateral RA-UKA (39, 41). A systematic review evaluating mid-term follow-up of RA-UKA (which included seven studies that analysed lateral RA-UKA) reported a survivorship of 96% (26). There were no studies reporting on long-term survivorship of lateral RA-UKA owing to the relative novelty of robotic technology combined with the infrequency that lateral UKA is performed.
Our study has limitations. Firstly, our cohort size is relatively small and a comparator group was not applicable. Moreover, this is a series performed by a high-volume surgeon (senior author) at centres where the use of the robotic arm has increased significantly over the preceding years. However, given the short learning curve with robotic-arm assistance, we believe our findings could be generalisable to lower-volume institutions. Further studies are needed to evaluate longer-term outcomes and survivorship, in addition to ascertaining the reproducibility of excellent outcomes by less experienced surgeons.
In conclusion, the use of robotic arm-assistance for lateral UKA was shown to be associated with a significant improvement in clinical outcomes, irrespective of the severity of the pre-operative deformity, with low complication and reoperation rates. Further multi-centre comparative studies assessing longer-term outcomes and survivorship of lateral RA-UKA are needed.
The data that support the conclusions of this article are available to other researchers by the authors, upon reasonable request.
This research is approved by the local ethics board.
WW: Manuscript Preparation, Data Interpretation. JC: Manuscript Preparation. AF: Manuscript Preparation, Data Interpretation. RP: Manuscript Preparation. FH: Hypothesis Generation, Manuscript Preparation. All authors contributed to the article and approved the submitted version.
WW, JC, AF and RP did not receive any financial support and do not have any conflicts of interest. FH reports board membership of the Bone and Joint Journal and the Annals of the Royal College of Surgeons; consultancy for Smith & Nephew, Corin, MatOrtho and Stryker; payment for lectures including service on speakers’ bureaus for Smith & Nephew and Stryker; royalties paid by Smith & Nephew, MatOrtho, Corin and Stryker, all outside the submitted work.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the national joint registry for England and Wales. Bone Joint J. (2015) 97-B(6):793–801. doi: 10.1302/0301-620X.97B6.35155
2. Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP. Unicondylar knee arthroplasty in the UK national health service: an analysis of candidacy, outcome and cost efficacy. Knee. (2009) 16(6):473–8. doi: 10.1016/j.knee.2009.04.006
3. Liddle AD, Pandit H, Judge A, Murray DW. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the national joint registry for England and Wales. Bone Joint J. (2015) 97-B(11):1506–11. doi: 10.1302/0301-620X.97B11.35551
4. Prats-Uribe A, Kolovos S, Berencsi K, Carr A, Judge A, Silman A, et al. Unicompartmental compared with total knee replacement for patients with multimorbidities: a cohort study using propensity score stratification and inverse probability weighting. Health Technol Assess. (2021) 25(66):1–126. doi: 10.3310/hta25660
5. Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. (2009) 91(1):52–7. doi: 10.1302/0301-620X.91B1.20899
6. Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, et al. Total vs. partial knee replacement in patients with medial compartment knee osteoarthritis: the TOPKAT RCT. Health Technol Assess. (2020) 24(20):1–98. doi: 10.3310/hta24200
7. Ode Q, Gaillard R, Batailler C, Herry Y, Neyret P, Servien E, et al. Fewer complications after UKA than TKA in patients over 85 years of age: a case-control study. Orthop Traumatol Surg Res. (2018) 104(7):955–9. doi: 10.1016/j.otsr.2018.02.015
8. Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol. (2015) 25(5):799–806. doi: 10.1007/s00590-015-1610-9
9. Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the national joint registry for England and Wales. Lancet. (2014) 384(9952):1437–45. doi: 10.1016/S0140-6736(14)60419-0
10. Burnett Iii RA, Yang J, Courtney PM, Terhune EB, Hannon CP, Della Valle CJ. Costs of unicompartmental compared with total knee arthroplasty: a matched cohort study over ten years. Bone Joint J. (2021) 103-B(6 Supple A):23–31. doi: 10.1302/0301-620X.103B6.BJJ-2020-2259.R1
11. Han SB, Lee SS, Kim KH, Im JT, Park PS, Shin YS. Survival of medial vs. lateral unicompartmental knee arthroplasty: a meta-analysis. PLoS One. (2020) 15(1):e0228150. doi: 10.1371/journal.pone.0228150
12. Streit MR, Walker T, Bruckner T, Merle C, Kretzer JP, Clarius M, et al. Mobile-bearing lateral unicompartmental knee replacement with the Oxford domed tibial component: an independent series. J Bone Joint Surg Br. (2012) 94(10):1356–61. doi: 10.1302/0301-620X.94B10.29119
13. Kennedy JA, Mohammad HR, Yang I, Mellon SJ, Dodd CAF, Pandit HG, et al. Oxford domed lateral unicompartmental knee arthroplasty. Bone Joint J. (2020) 102-B(8):1033–40. doi: 10.1302/0301-620X.102B8.BJJ-2019-1330.R2
14. McEwen P, Balendra G, Doma K. Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J. (2019) 101-B(3):331–9. doi: 10.1302/0301-620X.101B3.BJJ-2018-0544.R1
15. Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K. The flexion gap in normal knees. An MRI study. J Bone Joint Surg Br. (2004) 86(8):1133–6. doi: 10.1302/0301-620X.86B8.15246
16. Scott RD. Lateral unicompartmental replacement: a road less traveled. Orthopedics. (2005) 28(9):983–4. doi: 10.3928/0147-7447-20050901-34
17. Pandit H, Jenkins C, Beard DJ, Price AJ, Gill HS, Dodd CA, et al. Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee. (2010) 17(6):392–7. doi: 10.1016/j.knee.2009.10.007
18. Weston-Simons JS, Kendrick BJ, Mentink MJ, Pandit H, Gill HS, Murray DW. An analysis of dislocation of the domed Oxford lateral unicompartmental knee replacement. Knee. (2014) 21(1):304–9. doi: 10.1016/j.knee.2013.04.008
19. Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. (2003) 85(10):1968–73. doi: 10.2106/00004623-200310000-00016
20. Plancher KD, Briggs KK, Chinnakkannu K, Dotterweich KA, Commaroto SA, Wang KH, et al. Isolated lateral tibiofemoral compartment osteoarthritis: survivorship and patient acceptable symptom state after lateral fixed-bearing unicompartmental knee arthroplasty at mean 10-year follow-up. J Bone Joint Surg Am. (2022) 104(18):1621–8. doi: 10.2106/JBJS.21.01523
21. Huang T, Long Y, George D, Wang W. Meta-analysis of gap balancing vs. measured resection techniques in total knee arthroplasty. Bone Joint J. (2017) 99-B(2):151–8. doi: 10.1302/0301-620X.99B2.BJJ-2016-0042.R2
22. Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing vs. measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. (2010) 468(1):102–7. doi: 10.1007/s11999-009-1112-3
23. Petrie JR, Haidukewych GJ. Instability in total knee arthroplasty: assessment and solutions. Bone Joint J. (2016) 98-B(1 Suppl A):116–9. doi: 10.1302/0301-620X.98B1.36371
24. Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. (2018) 100-B(7):930–7. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1
25. Fontalis A, Kayani B, Asokan A, Haddad IC, Tahmassebi J, Konan S, et al. Inflammatory response in robotic-arm-assisted vs. conventional jig-based TKA and the correlation with early functional outcomes: results of a prospective randomized controlled trial. J Bone Joint Surg Am. (2022) 104(21):1905–14. doi: 10.2106/JBJS.22.00167
26. Robinson PG, Clement ND, Hamilton D, Blyth MJG, Haddad FS, Patton JT. A systematic review of robotic-assisted unicompartmental knee arthroplasty: prosthesis design and type should be reported. Bone Joint J. (2019) 101-B(7):838–47. doi: 10.1302/0301-620X.101B7.BJJ-2018-1317.R1
27. Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional vs. robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. (2019) 101-B(1):24–33. doi: 10.1302/0301-620X.101B1.BJJ-2018-0564.R2
28. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. (2013) 471(1):118–26. doi: 10.1007/s11999-012-2407-3
29. Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN. Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc. (2011) 19(9):1496–503. doi: 10.1007/s00167-011-1483-3
30. Kayani B, Haddad FS. Robotic unicompartmental knee arthroplasty: current challenges and future perspectives. Bone Joint Res. (2019) 8(6):228–31. doi: 10.1302/2046-3758.86.BJR-2019-0037
31. Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted. Bone Joint Res. (2017) 6(11):631–9. doi: 10.1302/2046-3758.611.BJR-2017-0060.R1
32. Burger JA, Kleeblad LJ, Laas N, Pearle AD. Mid-term survivorship and patient-reported outcomes of robotic-arm assisted partial knee arthroplasty. Bone Joint J. (2020) 102-B(1):108–16. doi: 10.1302/0301-620X.102B1.BJJ-2019-0510.R1
33. Zambianchi F, Franceschi G, Rivi E, Banchelli F, Marcovigi A, Khabbazè C, et al. Clinical results and short-term survivorship of robotic-arm-assisted medial and lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2020) 28(5):1551–9. doi: 10.1007/s00167-019-05566-4
34. Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg. (2018) 138(12):1765–71. doi: 10.1007/s00402-018-3042-6
35. Khamaisy S, Gladnick BP, Nam D, Reinhardt KR, Heyse TJ, Pearle AD. Lower limb alignment control: is it more challenging in lateral compared to medial unicondylar knee arthroplasty? Knee. (2015) 22(4):347–50. doi: 10.1016/j.knee.2015.02.018
36. Heckmann ND, Antonios JK, Chen XT, Kang HP, Chung BC, Piple AS, et al. Midterm survivorship of robotic-assisted lateral unicompartmental knee arthroplasty. J Arthroplasty. (2022) 37(5):831–6. doi: 10.1016/j.arth.2022.01.023
37. van der List JP, Chawla H, Villa JC, Pearle AD. Different optimal alignment but equivalent functional outcomes in medial and lateral unicompartmental knee arthroplasty. Knee. (2016) 23(6):987–95. doi: 10.1016/j.knee.2016.08.008
38. Gaudiani MA, Samuel LT, Diana JN, DeBattista JL, Coon TM, Moore RE, et al. Robotic-arm assisted lateral unicompartmental knee arthroplasty: 5-year outcomes & survivorship. J Orthop Surg (Hong Kong). (2023) 31(1):10225536221138986. doi: 10.1177/10225536221138986
39. Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2019) 27(4):1232–40. doi: 10.1007/s00167-018-5081-5
40. Zambianchi F, Franceschi G, Banchelli F, Marcovigi A, Ensini A, Catani F. Robotic arm-assisted lateral unicompartmental knee arthroplasty: how are components aligned? J Knee Surg. (2022) 35(11):1214–22. doi: 10.1055/s-0040-1722346
Keywords: lateral unicompartmental arthroplasty, MAKO arthroplasty, MAKO robot, lateral unicompartmental knee arthroplasty (LUKA), unicompartmental knee arthroplasty
Citation: Wignadasan W, Chang J, Fontalis A, Plastow R and Haddad FS (2023) Short term outcomes following robotic arm-assisted lateral unicompartmental knee arthroplasty. Front. Surg. 10:1215280. doi: 10.3389/fsurg.2023.1215280
Received: 1 May 2023; Accepted: 29 November 2023;
Published: 15 December 2023.
Edited by:
Carl Haasper, Orthopaedic Surgery Bremerhaven-Wesermünde, GermanyReviewed by:
Stefano Marco Paolo Rossi, Fondazione Poliambulanza Istituto Ospedaliero, Italy© 2023 Wignadasan, Chang, Fontalis, Plastow and Haddad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Warran Wignadasan d2FycmFuLndpZ25hZGFzYW5AZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.