- 1Department of Anesthesia, College of medicine and health sciences, University of Gondar, Gondar
- 2Department of Anesthesia, College of medicine and health sciences, Arba Minch University, Arba Minch, Ethiopia
Background: Thoraco-abdominal surgery cuts through muscle, disrupting the normal structure and function of the respiratory muscles, resulting in lower lung volumes and a higher risk of developing post-operative pulmonary complications (PPC). PPC remains an important cause of post-operative morbidity and mortality and impacts the long-term outcomes of patients after hospital discharge. This study was aimed at determining the incidence and factors associated with postoperative pulmonary complications among patients who underwent thoracic and upper abdominal surgery in the Amhara region of Ethiopia.
Methods: A multi-center follow-up study was conducted from April 1, 2022, to June 30, 2022, at comprehensive specialized hospitals in Amhara regional state, northwest Ethiopia. 424 patients were consecutively included in this study, with a response rate of 100%. A chart review and patient interview were used to collect data. A logistic regression analysis was performed to assess the strength of the association of independent variables with postoperative pulmonary complications.The crude odds ratio (COR) and adjusted odds ratio (AOR) with the corresponding 95% confidence interval were computed. Variables with a p-value of <0.05 were considered statistically significant predictors of the outcome variable.
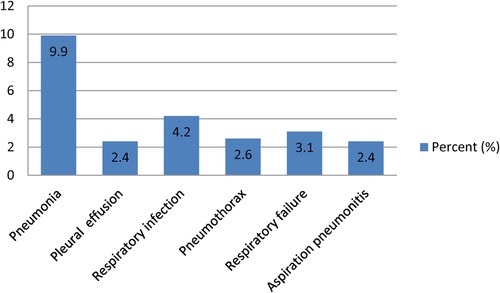
Results: The incidence of postoperative pulmonary complication was 24.5%. Emergency procedures, preoperative SpO2 < 94%, duration of surgery >2 h, patients with a nasogastric tube, intraoperative blood loss >500 ml and post-operative albumin <3.5 g/dl were factors associated with pulmonary complications. The most common complications were pneumonia (9.9%) followed by respiratory infection (4.2%).
Conclusion: The incidence of postoperative pulmonary complication after thoracic and upper abdominal surgery remains high. Preoperative SpO2, duration of surgery, patients having a nasogastric tube, intraoperative blood loss and post-operative albumin were factors associated with post-operative pulmonary complications.
1. Introduction
Surgical procedures are predicted to account for 11% of total global disease burden and 25 million disability-adjusted life years (DALYs) in Africa, the region with the highest concentration of surgical DALYs (38/1,000 population) (1). Surgery and trauma patients typically experience a sudden and significant systemic insult that commonly results in the decompensation of subclinical illnesses and creates potentially fatal effects (2). A high mortality rate in surgical units was caused by the fact that the majority of post-surgical problems were either surgical or anesthetic care-related (3).
The most common cause of morbidity following surgery is still post-operative problems involving the respiratory system (4). Postoperative pulmonary complications (PPC) are adverse changes to the respiratory system that occur after surgery and can adversely affect the patient's clinical outcome (5). A pulmonary abnormality that develops following surgery and leads to clinically significant disease or dysfunction, adversely influencing the clinical course of the initial condition, is referred to as a post-operative pulmonary complication (PPC) (6). There is no well recognized definition of PPC. Many literatures used the definition of PPC, which typically includes acute respiratory failure, weaning failure, pneumonia, atelectasis, bronchospasm, worsening of chronic obstructive pulmonary disease, pneumothorax, pleural effusion, and different kinds of upper airway obstruction (5, 7–9).
Postoperative pulmonary complications (PPC) are the leading causes of morbidity and mortality, specifically within the first postoperative week (7, 10). The incidence of PPC is inversely related to the distance of the surgical incision from the diaphragm, making patients undergoing abdominal and thoracic surgery the most vulnerable (11). Postoperative pulmonary complications are more common in thoracic and abdominal surgeries, with an incidence varying from 12% to 70% (12). The incidence is mainly related to the patient population, the type of surgery, and the presence of contributing factors (13). It has been estimated that more than 1 million PPCs occur annually in the United States, resulting in 46,200 related deaths and 4.8 million additional hospitalization days (14).
Postoperative pulmonary complications after thoracic and upper abdominal surgery may have a significant clinical and economic impact, as they are associated with a longer length of hospital stay and costs, a higher frequency of intensive care unit (ICU) admissions, and a higher number of hospital deaths (13, 15–17). PPC after thoracic and upper abdominal surgery is significantly more common in patients with cardiopulmonary disturbances and coexisting diseases (12, 18). Preoperative evaluation and pulmonary risk stratification are important parts of primary care (19). Prevention of PPC requires a multidisciplinary approach that includes optimization of co-morbidities, greater utilization of regional analgesia, balancing intravenous fluid therapy, gastric drainage, vigilance monitoring, chest physiotherapy, lung expansion maneuvers, early mobilization, and early oral feeding in the postoperative period (13, 20).
PPC is still a major problem, and there are a limited number of studies on the incidence and factors associated with post-operative pulmonary complications after thoracic and upper abdominal surgery among surgical patients in Ethiopia. Therefore, this study was aimed at determining the incidence and factors associated with postoperative pulmonary complication in patients who underwent thoracic and upper abdominal surgery at comprehensive specialized hospitals in the Amhara region of Ethiopia.
2. Methods and materials
2.1. Study design and setting
A prospective multi-center follow-up study was conducted from April 1, 2022, to June 30, 2022, at comprehensive specialized hospitals in Amhara national regional state, northwest Ethiopia. This research was carried out at four comprehensive specialty hospitals in Ethiopia's Amhara region. The research was conducted at the University of Gondar, Tibebe-Ghion, Debre-Markos, and Felege-Hiwot comprehensive specialized hospitals.
The University of Gondar comprehensive specialized hospital is located in the Amhara region's Gondar town. The hospital has nearly 400 beds and eleven operating rooms, and it serves as a referral center for numerous district hospitals. It provides service for more than seven million people.
Tibebe-Ghion and Felege-Hiwot comprehensive specialty hospitals are located in Bahir-Dar City, the region's capital, and have eleven and four operating rooms, respectively. Debre-Markos comprehensive specialty hospital is 265 kilometers from Bahir-Dar city. This referral hospital has four operating rooms and serves more than five million people.
All elective and emergency adult patients who had thoracic and upper abdominal surgery during the study period were included in the study. Intraoperative death, preoperatively intubated patients, patients who refuse to give consent and are unable to communicate, and pregnant women were excluded from the study.
2.2. Operational definition
According to European Perioperative Clinical Outcome (EPCO) diagnostic criteria and definition, a postoperative pulmonary complication is the occurrence of one or more of the following during the first postoperative week: respiratory infection, respiratory failure, pleural effusion, atelectasis, pneumothorax, bronchospasm, aspiration pneumonitis, pneumonia, acute respiratory distress syndrome, pulmonary edema, and tracheobronchitis (21).
2.3. Sample size calculation
The sample size was calculated using the single population proportion formula. Since there is no similar previous study in Ethiopia, the assumption of a 50% proportion, a 5% margin of error, and a 95% confidence interval was used.
where, n: sample size, p: proportion, d: absolute precision. 424 patients were included in the study overall after adding 10% of the non-response rate.
2.4. Sampling technique
Patients who underwent thoracic and upper abdominal surgery were consecutively included until the required sample size was reached. Patients who were admitted preoperatively to the selected hospitals and underwent elective and emergency thoracic and upper abdominal surgery were evaluated for PPC. A review of the previous surgeries per year on the log book showed that there were 1,728 surgeries, and the number of operations per three months was 432. Therefore, during the study period, 432 patients were estimated to have undergone thoracic and upper abdominal surgery at four comprehensive specialized hospitals in the Amhara region.
The sample size for each hospital was calculated using nf = (Nf/N) n, where nf is the allocated sample size of each hospital, N is the total population of the comprehensive specialized hospitals, n is the calculated sample size, and Nf is the size of each hospital's source population (Figure 1).
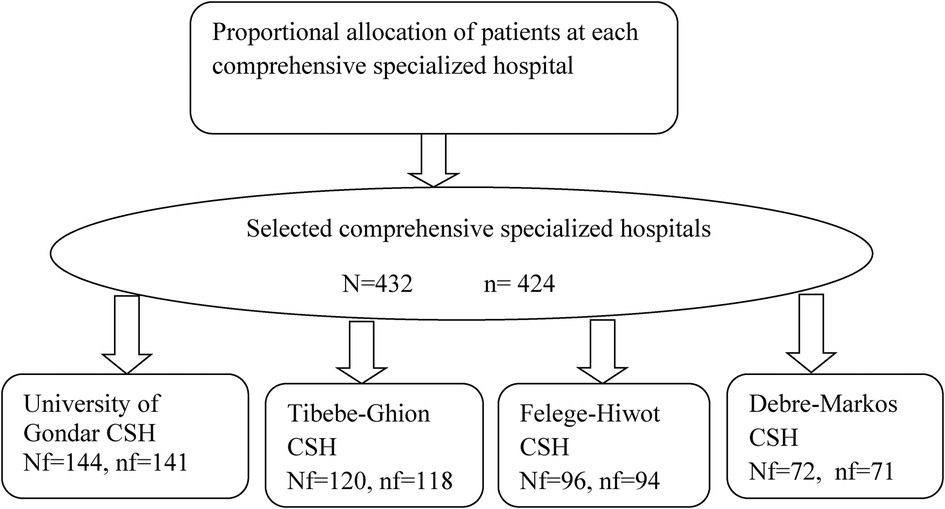
Figure 1. Proportional allocation and enrollment of patients who underwent thoracic and upper abdominal surgery at comprehensive specialized hospitals in the Amhara region, Ethiopia. CSH, Comprehensive specialized hospital.
2.5. Data collection instrument and procedure
The data were collected through interviews and chart reviews. Two trained data collectors were assigned at each center to collect the data, consisting of demographic characteristics and perioperative surgical and anesthetic-related variables of the patient. Postoperative pulmonary complications were assessed in the patient's chart. Physician and nursing notes, order sheets, anesthesia records, operative reports, and diagnostic studies were reviewed.
Patients were considered as having post-operative pulmonary complication (PPC) when one or more of the following: pneumonia, tracheo-bronchitis, atelectasis, respiratory failure, respiratory infection, bronchospasm, aspiration pneumonitis, pulmonary edema, pneumothorax, and pleural effusion were occurred during the first postoperative week. Patients were monitored daily, and follow-up started on the day of the surgery and ended within 7 days postoperatively. The data collectors report to the physicians when they observe a pulmonary complication.
2.6. Data quality control
To ensure the quality of the data, a pre-test was conducted on 22 (5%) of the patients who were not included in the main study at the University of Gondar comprehensive specialized hospital. Data collectors and supervisors were trained for data collection procedures. The supervisors monitored the data collector and checked for completeness every day following data collection. The collected data was reviewed for completeness, accuracy, and clarity.
2.7. Data processing and analysis
Epi-Data version 4.6 was used to enter the data and SPSS version 20 for analysis. Socio-demographic, surgical, and anesthetic variables of the patients were analyzed and presented in tables. Model fitness was checked by the Hosmer-Lemeshow test. Bivariable and multivariable logistic regression analyses were performed to determine the association between dependent and independent variables. Variables with a p-value of less than 0.2 in binary logistic regression were transferred into the multivariable logistic regression model to analyze the factors associated with postoperative pulmonary complications after thoracic and upper abdominal surgery. Both the crude odds ratio (COR) and the adjusted odds ratio (AOR) with the corresponding 95% confidence interval (CI) were calculated to show the strength of the association of risk factors with post-operative pulmonary complications. Variables with a p-value of less than 0.05 in the multivariate logistic regression were considered statistically significant predictors of pulmonary complications after upper abdominal and thoracic surgery.
2.8. Ethical consideration
The research and ethical review committee of the college of medicine and health sciences at the University of Gondar granted its approval for the study, which was then carried out. Each hospital's medical director provided a letter of permission for the study to be carried out. The patient was told about the study, and each participant gave written informed consent to the data collectors. Avoiding using personal identifiers allowed for the preservation of confidentiality throughout the entire study. The patients' participation in the study was voluntary, and those who did not want to participate or who changed their minds about participating at any time were allowed to do so.
3. Results
3.1. Socio-demographic and clinical characteristics of the patients
A total of 424 patients who underwent thoracic and upper abdominal surgery were included in this study, with a response rate of 100%. The majority of patients, 256 (60.4%), were males with a median age of 37 years. Most of the patients, 320 (75.5%), were classified as ASA I. Only 24 (5.7%) patients were smokers, and 35 (8.3%) were alcohol drinkers. 258 (60.8%) procedures were emergency operations. The majority of the patients', 364 (85.8%), preoperative hemoglobin was >10 g/dl (Table 1).
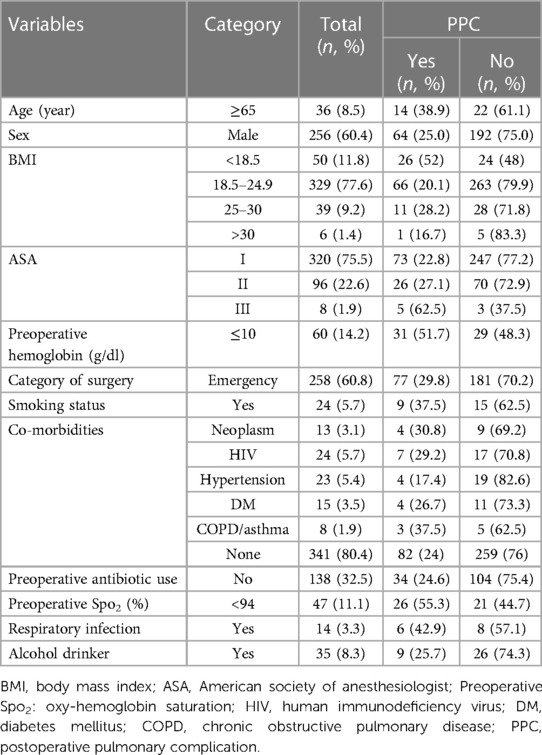
Table 1. Socio-demographic and clinical characteristics of the patients who underwent thoracic and upper abdominal surgery at comprehensive and specialized hospitals in Amhara region, Ethiopia.
3.2. Surgical and anesthetic related characteristics of patients
The majority of patients underwent upper abdominal surgery, which accounts for 96.9% of operations, and about 23.8% of patients had a nasogastric tube in situ. About 66.3% of patients had a blood loss of less than 500 ml. Only 3 (0.7%) patients underwent laparoscopic operations, and the majority of the patients received opioid. The majority of patients’ (71.7%) postoperative albumin level was greater than 3.5 g/dl (Table 2).
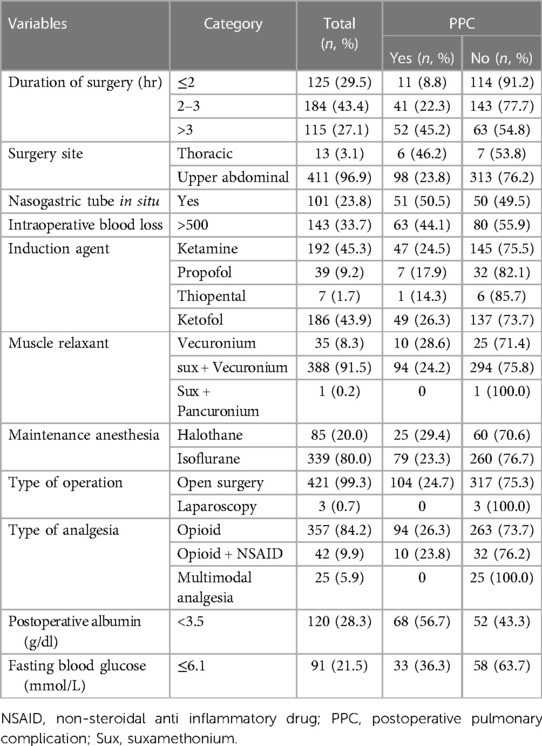
Table 2. Surgical and anesthetic related characteristics of patients who underwent thoracic and upper abdominal surgery at comprehensive specialized hospitals in Amhara region, Ethiopia.
3.3. Incidence of post-operative pulmonary complications after thoracic and upper abdominal surgery
The overall incidence of postoperative pulmonary complications after thoracic and upper abdominal surgery was 104 (24.5%) (95% CI: 20.5–28.5). The most common complications were pneumonia (42, 9.9%), followed by respiratory infection (18, 4.2%), and respiratory failure (13, 3.1%) (Figure 2). The majority of the complications occurred within the first three days of the post-operative period (Figure 3). From the total PPCs that occurred, 95 patients had a single PPC, seven patients had two PPC, and two patients had three postoperative pulmonary complications.
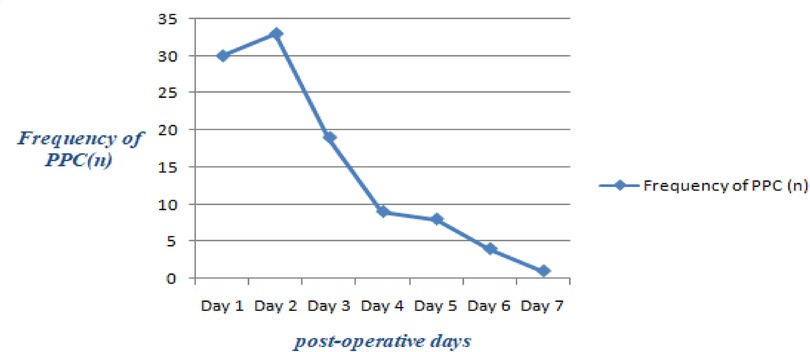
Figure 3. The frequency of post-operative pulmonary complications in the respective post-operative days of a week.
3.4. Factors associated with post-operative pulmonary complication after thoracic and upper abdominal surgery
In the bi-variable logistic regression analysis, variables like age, ASA, preoperative anemia, category of surgery, preoperative Spo2, duration of surgery, NG tube in situ, intraoperative blood loss, post-operative albumin, and post-operative fasting blood glucose had a p-value of <0.2 and were considered as potential factors associated with post-operative pulmonary complications (Table 3).
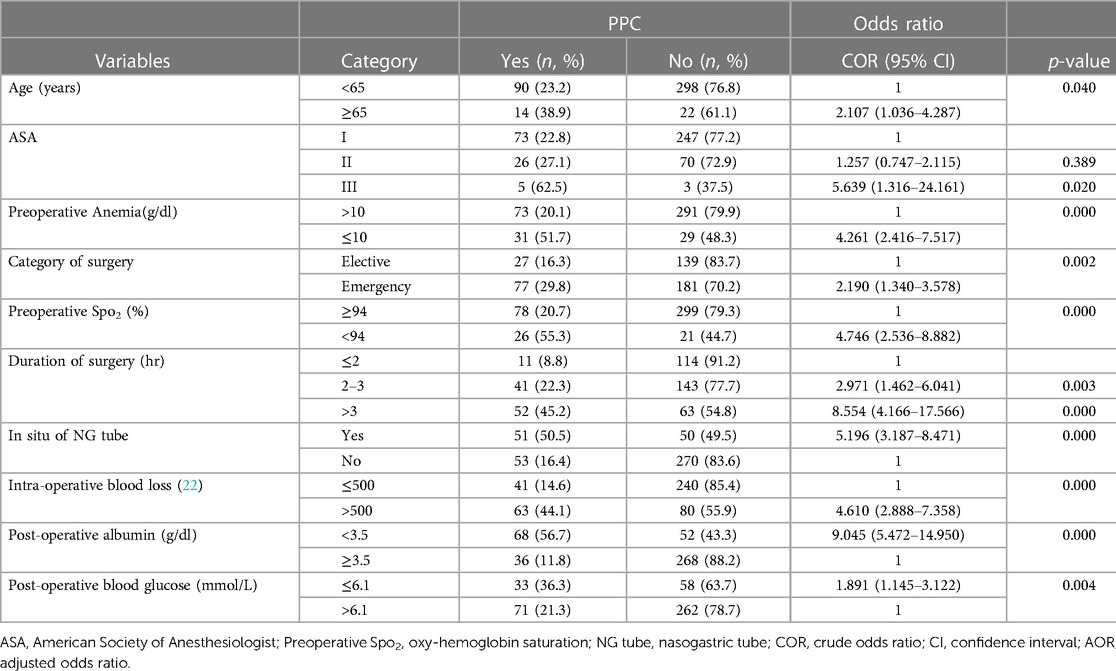
Table 3. Bi-variable logistic regression analysis of factors associated with post-operative pulmonary complications after thoracic and upper abdominal surgery at comprehensive specialized hospitals in Amhara region, Ethiopia.
In multi-variable logistic regression analysis, variables such as category of surgery, preoperative Spo2, duration of surgery, NG tube in situ, intra-operative blood loss, and post-operative albumin had a p-value of <0.05 and were considered significant associated factors for PPC (Table 4).
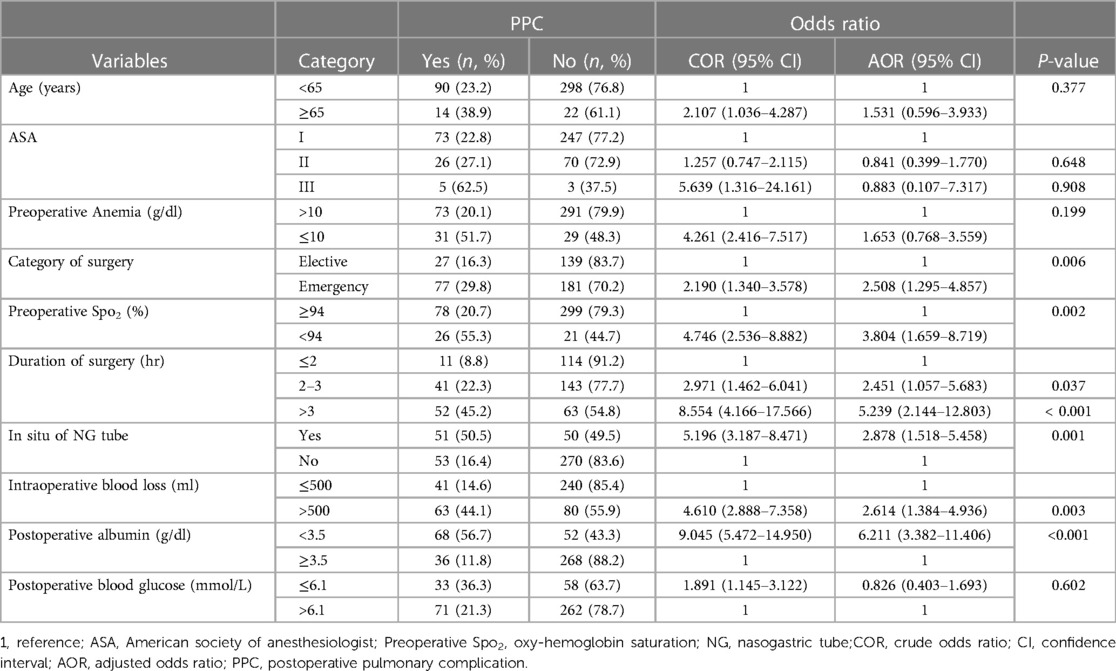
Table 4. Multi-variable logistic regression analysis of factors associated with post-operative pulmonary complications after thoracic and upper abdominal surgery at comprehensive specialized hospitals in Amhara region, Ethiopia.
In this study, emergency patients were 2.5 times (AOR: 2.508, 95% CI: 1.295–4.857) more likely to develop PPC than elective patients. Patients with preoperative Spo2 < 94% were 3.8 times (AOR: 3.804, 95%CI: 1.659–8.719) more likely to have PPC than patients with preoperative Spo2 ≥ 94%. Patients with prolonged surgical duration (>2 h) were 2.5 times more likely to develop PPC than patients whose operations lasted ≤2 h (AOR: 2.451, 95%CI: 1.057–5.683). Patients with an NG tube were 2.9 times (AOR: 2.878, 95%CI: 1.518–5.458) more likely to develop PPC than patients without NG tube in situ. Patients with intra-operative blood loss of >500 ml were 2.6 times more likely to develop PPC than patients with blood loss of ≤500 ml (AOR: 2.614, 95%CI: 1.384–4.936). The odds of developing PPC were 6.2 folds (AOR: 6.211, 95%CI: 3.382–11.406) increased in patients with postoperative albumin level <3.5 g/dl compared to patients with postoperative albumin ≥3.5 g/dl (Table 4).
4. Discussion
The incidence of post-operative pulmonary complications following thoracic and upper abdominal surgery at comprehensive and specialized hospitals in Amhara region was 24.5% (95% CI: 20.5–28.5). This suggests that post-operative pulmonary complications after thoracic and upper abdominal surgery were still significant.
A study conducted in Albania showed that the incidence of PPC was 27.3% which is in line with our finding (23). In our study, the incidence of postoperative pulmonary complications was higher compared to previous studies in China and Brazil, with the incidence of PPC being 9.7%, 11.5%, and 19%, respectively (24–26). This relatively higher incidence of post-operative pulmonary complications may be due to the grade and complexity of surgery, since all patients in our study underwent major surgery.
The incidence of PPC was lower than in previous studies conducted in Zimbabwe; about 42.4% of the patients who underwent thoracic and abdominal surgeries developed PPC (27). The incidence of PPC in our study was also lower than a study done in Turkey; 58.3% of patients after upper abdominal surgery had PPC (28). This might be due to the higher percentage of ASA-class I and younger patients in our study.
In our study, different types of pulmonary complications were identified in the post-operative period. Among those complications, pneumonia was the most common, followed by respiratory infection and respiratory failure, which is similar to other previous studies (24, 28–30).
The results of our study demonstrated that the incidence of post-operative pulmonary complications after thoracic and upper abdominal surgery was significantly associated with emergency procedures, preoperative Spo2 < 94%, prolonged duration of surgery >2 h, patients with an NG tube, intra-operative blood loss >500 ml and a postoperative albumin level <3.5 g/dl. Clinical measures targeted at these factors are essential to prevent the development of PPC.
Our study demonstrated that emergency patients were more than twice as likely to develop PPC than elective patients, and it was one of the main factors for postoperative pulmonary complications, which is consistent with other studies (17, 31, 32). This may be due to the urgent nature of the procedure, the clinical characteristics of patients, as well as preoperative diagnoses and surgical strategies adopted in emergency situations, which carry higher risks for PPC due to impaired bowel motility and obstructive bowel lesions predisposing to PPC (33).
Patients with preoperative Spo2 < 94% were more likely to develop PPC than patients with preoperative Spo2 ≥ 94% and this finding is in agreement with similar studies (24, 31, 34). A longer duration of surgery was associated with PPC. The reasons may be that the prolonged operation duration means prolonged anesthesia time that depresses movements of inter-costal muscles, alters the shape and motion of the chest wall, and diminishes ribcage excursion, affecting lung mechanics and resulting in a decrease in functional residual capacity (35). In our study, patients with prolonged surgical times were more likely to develop PPC than those whose surgeries lasted less than 2 h, which was consistent with previous studies (27, 31, 34).
Patients with an NG tube were more likely to develop PPC than patients without an NG tube, which was in agreement with previous studies (16, 36, 37). The exact mechanism of how NG tube usage is associated with PPC is not clear, but interference with cough due to discomfort, incomplete closure of the glottis, fostering transfer of microorganisms from the oro-pharynx to the airways, and favoring silent aspiration are possible mechanisms (38).
In our study, patients with intra-operative blood loss of >500 ml were more likely to develop PPC than patients with blood loss of less than 500 ml which was in line with previous studies (12, 30). Excessive blood loss during surgical procedures calls for judicious replacement to restore a normovolemic state. However, infusion of large volumes of fluids intra-operatively is associated with a higher incidence of PPC (39).
Our study revealed that the risk of developing PPC was higher in patients with a postoperative albumin level less than 3.5 g/dl compared to those with a postoperative albumin level greater than 3.5 g/dl. This finding was in agreement with other studies (24, 34). This could be due to a low blood protein level, which results in vascular endothelial dysfunction, or by reducing colloid osmotic pressure. It contributes to PPC by decreasing the oncotic forces that favor the retention of fluid in the microvasculature (40).
5. Limitation of the study
This study has certain shortcomings that must be considered. First, we have not performed follow-up after seven days of the postoperative period. The long-term risk of PPC after surgery in this study remains unclear. Furthermore, the attending physician was in charge of the diagnosis of PPCs; thus, potential estimation bias for actual PPC incidence was unavoidable.
6. Conclusion and recommendation
The incidence of post-operative pulmonary complications after thoracic and upper abdominal surgery was a common postoperative morbidity. The most common complication was pneumonia, followed by respiratory infection and respiratory failure. Pre-operative SpO2 of less than 94%, duration of surgery more than 2 h, patients with NG tubes, intra-operative blood loss greater than 500 ml, and post-operative albumin less than 3.5 g/dl were factors associated with post-operative pulmonary complications.
Surgical team members should place more emphasis on detecting and reducing modifiable risk factors during the peri-operative period, and close post-operative follow-up is important for a better outcome for the patient after thoracic and upper abdominal operations.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical committee of school of medicine at University of Gondar. The patients/participants provided their written informed consent to participate in this study.
Author contributions
BE, BA, HT, and SA contributed to the study's idea and design, data collection, analysis, and interpretation, manuscript drafting, and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgements
The departments of anesthesia and surgery provided excellent cooperation, which the authors appreciate for their contributions during the data collection period.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ozgediz D, Riviello R. The “other” neglected diseases in global public health: surgical conditions in sub-Saharan Africa. PLoS Med. (2008) 5(6):e121. doi: 10.1371/journal.pmed.0050121
2. Sawyer RG, Leon CAT. Common complications in the surgical intensive care unit. Crit Care Med. (2010) 38(9):S483–93. doi: 10.1097/CCM.0b013e3181ec68c9
3. Okafor UV. An audit of unplanned postoperative intensive care unit admissions in Enugu, Nigeria: causes and outcome. South Afr J Crit Care. (2009) 25(1):16–9.
4. Reeve J. Physiotherapy interventions to prevent postoperative pulmonary complications following lung resection. What is the evidence? What is the practice? (2008).
5. Miskovic A, Lumb A. Postoperative pulmonary complications. Br J Anaesth. (2017) 118(3):317–34. doi: 10.1093/bja/aex002
6. Sharafkhaneh A, Falk JA, Minai OA, Lipson DA. Overview of the perioperative management of lung volume reduction surgery patients. Proc Am Thorac Soc. (2008) 5(4):438–41. doi: 10.1513/pats.200708-130ET
7. Langeron O, Carreira S, Le SacHé F, Raux M. Postoperative pulmonary complications updating. Ann Fr Anesth Reanim. (2014) 33:480–3. doi: 10.1016/j.annfar.2014.07.741
8. Canet J, Mazo V. Postoperative pulmonary complications. Minerva Anestesiol. (2010) 76(2):138.20150855
9. Conde MV, Adams SG, Hines R. Overview of the management of postoperative pulmonary complications. Waltham, MA: UpToDate (2014).
10. Bevacqua BK. Pre-operative pulmonary evaluation in the patient with suspected respiratory disease. Indian J Anaesth. (2015) 59(9):542. doi: 10.4103/0019-5049.165854
12. Rock P, Rich PB. Postoperative pulmonary complications. Curr Opin Anesthesiol. (2003) 16(2):123–31. doi: 10.1097/00001503-200304000-00004
13. Upadhyay SP, Samanth U, Tellicherry SS, Lahiri GK, Saikia PP, Mallick PN. Prevention of postoperative pulmonary complications-multidisciplinary approach. J Anesth Surg. (2014) 2(2):1–8.
14. Fisher BW, Majumdar SR, McAlister FA. Predicting pulmonary complications after nonthoracic surgery: a systematic review of blinded studies. Am J Med. (2002) 112(3):219–25. doi: 10.1016/S0002-9343(01)01082-8
15. Berg S, Bittner EA. Postoperative care handbook of the Massachusetts general hospital. Massachusetts: Lippincott Williams & Wilkins (2017).
16. Gupta S, Fernandes RJ, Rao JS, Dhanpal R. Perioperative risk factors for pulmonary complications after non-cardiac surgery. J Anaesthesiol Clin Pharmacol. (2020) 36(1):88. doi: 10.4103/joacp.JOACP_54_19
17. Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat M, Rajesh P, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax. (2010) 65(9):815–8. doi: 10.1136/thx.2009.123083
18. Arruda KA, Cataneo DC, Cataneo AJM. Surgical risk tests related to cardiopulmonary postoperative complications: comparison between upper abdominal and thoracic surgery. Acta Cir Bras. (2013) 28:458–66. doi: 10.1590/S0102-86502013000600010
19. Gupta H, Gupta PK, Fang X, Miller WJ, Cemaj S, Forse RA, et al. Development and validation of a risk calculator predicting postoperative respiratory failure. Chest. (2011) 140(5):1207–15. doi: 10.1378/chest.11-0466
20. Henriksen M, Jensen MB, Hansen H, Jespersen T, Hessov I. Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition. (2002) 18(2):147–52. doi: 10.1016/S0899-9007(01)00748-1
21. Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol: EJA. (2015) 32(2):88–105. doi: 10.1097/EJA.0000000000000118
22. Gelaw KA, Aweke AM, Astawesegn FH, Demissie BW, Zeleke LB. Surgical site infection and its associated factors following cesarean section: a cross sectional study from a public hospital in Ethiopia. Patient Saf Surg. (2017) 11:1–7. doi: 10.1186/s13037-017-0131-3
23. Kodra N, Shpata V, Ohri I. Risk factors for postoperative pulmonary complications after abdominal surgery. Open Access Maced J Med Sci. (2016) 4(2):259–63. doi: 10.3889/oamjms.2016.059
24. Jin Y, Xie G, Wang H, Jin L, Li J, Cheng B, et al. Incidence and risk factors of postoperative pulmonary complications in noncardiac Chinese patients: a multicenter observational study in university hospitals. BioMed Res Int. (2015) 2015. doi: 10.1016/j.annfar.2014.07.741
25. Ávila A, Fenili R. Incidence and risk factors for postoperative pulmonary complications in patients undergoing thoracic and abdominal surgeries. Rev Col Bras Cir. (2017) 44:284–92. doi: 10.1590/0100-69912017003011
26. Silva DR, Gazzana MB, Knorst MM. Merit of preoperative clinical findings and functional pulmonary evaluation as predictors of postoperative pulmonary complications. Rev Assoc Med Bras. (2010) 56:551–7. doi: 10.1590/S0104-42302010000500016
27. Tadyanemhandu C, Mukombachoto R, Nhunzvi C, Kaseke F, Chikwasha V, Chengetanai S, et al. The prevalence of pulmonary complications after thoracic and abdominal surgery and associated risk factors in patients admitted at a government hospital in Harare, Zimbabwe-a retrospective study. Perioper Med. (2017) 6(1):1–8. doi: 10.1186/s13741-017-0066-3
28. Kanat F, Golcuk A, Teke T, Golcuk M. Risk factors for postoperative pulmonary complications in upper abdominal surgery. ANZ J Surg. (2007) 77(3):135–41. doi: 10.1111/j.1445-2197.2006.03993.x
29. Fernandes A, Rodrigues J, Lages P, Lança S, Mendes P, Antunes L, et al. Root causes and outcomes of postoperative pulmonary complications after abdominal surgery: a retrospective observational cohort study. Patient Saf Surg. (2019) 13(1):1–9. doi: 10.1186/s13037-019-0221-5
30. Denu ZA, Yasin MO, Berhe TBMA. Postoperative pulmonary complications and associated factors among surgical patients (2015).
31. Canet J, Gallart L, Gomar C, Paluzie G, Valles J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. J Am Soc Anesthesiol. (2010) 113(6):1338–50.
32. Scholes RL, Browning L, Sztendur EM, Denehy L. Duration of anaesthesia, type of surgery, respiratory co-morbidity, predicted VO2max and smoking predict postoperative pulmonary complications after upper abdominal surgery: an observational study. Aust J Physiother. (2009) 55(3):191–8. doi: 10.1016/S0004-9514(09)70081-9
33. de Cleva R, de Assumpção MS, Sasaya F, Chaves NZ, Santo MA, Fló C, et al. Correlation between intra-abdominal pressure and pulmonary volumes after superior and inferior abdominal surgery. Clinics. (2014) 69:483–6. doi: 10.6061/clinics/2014(07)07
34. Gebeyehu G, Eshetu A, Aweke S. Incidence and associated factors of postoperative pulmonary complications after abdominal surgery in the public hospital, Addis Ababa, Ethiopia. Anesthesiol Res Pract. (2022) 2022. doi: 10.1155/2022/8223903
35. Saraswat V. Effects of anaesthesia techniques and drugs on pulmonary function. Indian J Anaesth. (2015) 59(9):557. doi: 10.4103/0019-5049.165850
36. McAlister FA, Bertsch K, Man J, Bradley J, Jacka M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med. (2005) 171(5):514–7. doi: 10.1164/rccm.200408-1069OC
37. Smith PR, Baig MA, Brito V, Bader F, Bergman MI, Alfonso A. Postoperative pulmonary complications after laparotomy. Respiration. (2010) 80(4):269–74. doi: 10.1159/000253881
39. Arslantas MK, Kara HV, Tuncer BB, Yildizeli B, Yuksel M, Bostanci K, et al. Effect of the amount of intraoperative fluid administration on postoperative pulmonary complications following anatomic lung resections. J Thorac Cardiovasc Surg. (2015) 149(1):314–21.e1. doi: 10.1016/j.jtcvs.2014.08.071
Keywords: pulmonary complication, thoracic surgery, upper abdominal surgery, respiratory failure, anesthetics
Citation: Admass BA, Ego BY, Tawye HY and Ahmed SA (2023) Post-operative pulmonary complications after thoracic and upper abdominal procedures at referral hospitals in Amhara region, Ethiopia: a multi-center study. Front. Surg. 10:1177647. doi: 10.3389/fsurg.2023.1177647
Received: 1 March 2023; Accepted: 25 April 2023;
Published: 15 May 2023.
Edited by:
Mohsen Ibrahim, Sapienza University of Rome, ItalyReviewed by:
Sabrine Hemmes, The Netherlands Cancer Institute (NKI), NetherlandsCathrine Tadyanemhandu, Fatima College of Health Sciences, United Arab Emirates
© 2023 Admass, Ego, Tawye and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biruk Adie Admass YmlydWthZGllQHlhaG9vLmNvbQ==
 Biruk Adie Admass
Biruk Adie Admass Birhanu Yilma Ego2
Birhanu Yilma Ego2