
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 13 July 2023
Sec. Neurosurgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1135818
This article is part of the Research TopicHydrocephalusView all 7 articles
Objective: In patients with hydrocephalus, laparoscopy significantly improved ventriculoperitoneal shunt (VPS) outcomes. However, abdominal complications still occur, which require revision surgeries. In this study, we aimed to examine whether laparoscopy-assisted VPS with two-point fixation (LAVPS-TPF) has better outcomes than those of VPS (open-VPS) and laparoscopy-assisted VPS with no fixation (LAVPS-NF).
Methods: We retrospectively reviewed clinical records of 105 open-VPS, 40 LAVPS-NF, and 49 LAVPS-TPF cases from 2015 to 2020. Data including body mass index, etiology, abdominal surgery history, Glasgow coma scale (GCS), operation time, in-hospital days, shunt failure, complications, and modified Rankin scores were analyzed, as well as subgroups of patients with history of abdominal surgery, GCS scores, and revision surgeries.
Results: The LAVPS-TPF group demonstrated decreased shunt failure rates at 12 months (2.04%) compared to those of the open-VPS group (14.29%, P = 0.020) and reduced abdominal shunt-related complications (P = 0.004 vs. open-VPS and LAVPS-NF) and shunt revisions. In the LAVPS-TPF group with abdominal history (n = 51), 12-month shunt failure rates (P = 0.020 vs. open-VS), repair frequency (P = 0.020 vs. open-VS), and abdominal complications (P = 0.003 and 0.006 vs. open-VS and LAVPS-NF) were reduced. In the LAVPS-TPF group with GCS scores of 13–15 (n = 152), shunt failure rates at 12 months, abdominal complications, and revision frequency were decreased (P < 0.05 vs. other groups). Compared to the LAVPS-NF group, neurological complications were also reduced (P = 0.001). Among revision surgeries (n = 28), fixed shunts resulted in improved shunt survival rates at 12 months, reduced abdominal complications, and secondary revisions (P < 0.05). Moreover, a more optimal recovery without neurological sequelae was achieved by shunt fixation than that by LAVPS-NF (P < 0.01).
Conclusions: LAVPS-TPF significantly improved shunt survival rates at 12 months and reduced the incidence of abdominal shunt-related complications compared to open-VPS and LAVPS-NF, especially in patients with history of abdominal surgery, higher GCS scores, and revision surgeries. However, further studies are required to confirm these benefits.
The ventriculoperitoneal shunt (VPS) has been widely used to treat hydrocephalus (HC) by redirecting accumulated cerebrospinal fluid (CSF) from the lateral ventricles to the abdominal cavity (1). However, abdominal complications may result in shunt failure, intracranial infection, and even death (2). The laparoscopy-assisted VPS (LAVPS) has been suggested as a safer and more effective method with lower complication rates (3, 4). Nonetheless, some patients experienced a recurrence of shunt-related abdominal complications shortly after surgery, leading to disappointing outcomes. Thus, to prevent abdominal symptoms and shunt dysfunction, we developed a novel method by fixing the abdominal catheter at the liver's falciform (FL) and round ligaments (RL) (two points). In this retrospective study, clinical records of adult patients with HC were analyzed, and outcomes after conventional laparotomy (open-VPS), LAVPS with no fixation (LAVPS-NF), and LAVPS with two-point fixation (LAVPS-TPF) were compared.
A total of 170 clinical records of 167 patients with HC who underwent either open-VPS, LAVPS-NF, or LAVPS-TPF between January 2015 and August 2020 at a single institution (selection flow in Figure 1) were analyzed. The inclusion and exclusion criteria are presented in the Supplementary Material.
The following data were recorded: patients’ age, sex, body mass index (BMI), signs and symptoms, Glasgow coma scale (GCS) scores, radiographic images, medical history, and surgical history. Based on their GCS scores at the time of admission, patients were categorized into three severity levels: mild (GCS 13–15), moderate (GCS 9–12), and severe (GCS 3–8) (5). In addition, patients were classified into communicating HC, obstructive HC, normal pressure HC (NPH), congenital HC, and acquired HC, based on their medical information. The American Society of Anesthesiologists (ASA) physical status scores evaluated by an anesthetist prior to surgery, post-surgery analgesia treatments, and complications were documented. Furthermore, post-surgical symptoms and radiographic outcomes were monitored, and modified Rankin scores (mRS) were assessed during follow-up (6).
The surgical approach was determined in discussions between senior neurosurgeons. In the open-VPS group, the draining abdominal catheter was placed into the peritoneal cavity. For both LAVPS groups, the abdominal catheter was positioned on the liver's septal surface by the gastrointestinal surgeons. The shunt latency with clear CSF drips was verified under laparoscopy before closing. Particularly, in the LAVPS-TPF group, silk was used to suture the catheter tip on the falciform ligament, and the catheter body was tied to the round ligament as the second point (Figure 2). Details and short videos are presented in the Supplementary Material.
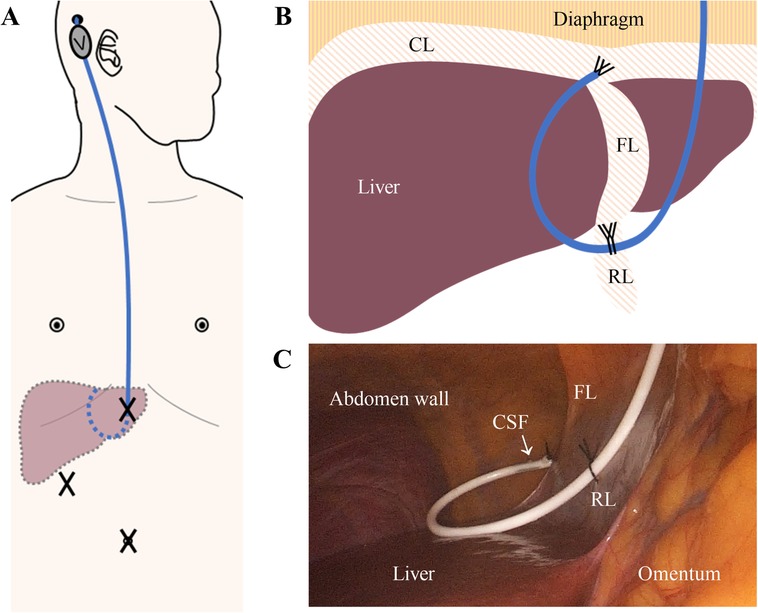
Figure 2. The two-point fixation technique. (A) Schematic diagram of the shunt (blue) subcutaneous pathway from the head to the abdomen. The subcutaneous VPS valve (V) behind the ear is connected to the ventricle and abdominal catheters. The abdominal catheter enters the abdominal cavity through the upper part of the abdominal trocars (X). Dashed lines indicate the intra-abdominal part of the shunt and liver. (B) Diagram of Two-Point Fixation to fix the catheter (blue) at livers’ FL and RL. (C) Interoperating laparoscopic photograph of the fixed catheter with clear, smoothly draining CSF. CL, coronary ligament. FL, falciform ligament. RL, round ligament. CSF, cerebrospinal fluid.
The rates of shunt failures diagnosed by a neurosurgeon at 6 and 12 months were the primary outcomes. Shunt (mostly valve) dysfunctions requiring either medicine or revision surgery were included. Secondary outcomes included shunt complications (i.e., obstruction, infection, cyst, over-drainage, and dislocation, among others), neurological complications (i.e., headache with or without vomiting, dizziness, unsteady gait and epilepsy among others), satisfaction regarding recovery (mRS = 0 or 1) (6, 7), and frequency of revision surgeries. All patients were followed up for at least 1 year.
IBM SPSS Statistics (version 26.0, New York, United States) and GraphPad Prism (version 8.0, California, United States) were used for data analysis. Chi-square tests, Fisher's exact tests, Student's t-test, and analysis of variance (ANOVA) tests were applied, with continuous variables expressed as mean ± standard deviation (SD). Survival Kaplan–Meier graphs were generated with log-rank tests performed. Statistical significance was considered when P < 0.05.
A total of 190 patient records with 105 open-VPS, 40 LAVPS-NF, and 49 LAVPS-TPF were reviewed (Table 1), including 28 revision surgeries. Sex, age, and BMI variances were found homogeneous in all three groups. Based on their GCS scores, patients were categorized into mild (n = 152), moderate (n = 27), and severe (n = 15) groups. Emergency surgery was performed on 21 patients (10 open-VPS, 2 LAVPS-NF, and 9 LAVPS-TPF).
A total of 30 abdominal catheter issues were recorded after the surgeries (20 in open-VPS, nine in LAVPS-NF, and one in LAVPS-TPF). Compared with those in open-VPS, shunt failure rates at 12 months (2.04% vs. 14.29%, P = 0.020), abdominal catheter-related complications (P = 0.004), and neurological complications (P = 0.015) were reduced in LAVPS-TPF. Although no statistical significance was found compared with the shunt failure rate at 12 months in LAVPS-NF (12.50%, P = 0.086), abdominal and neurological complications (P = 0.004 and <0.001) declined in LAVPS-TPF. However, no significant differences were observed between the LAVPS-NT and open-VPS groups for the 12-month shunt survival (P = 0.780) and abdominal shunt-related complications (P = 0.642). And the shunt non-failure survival curves were presented with statistical differences (P = 0.0134, Figure 3A). Moreover, only one revision surgery was performed in LAVPS-TPF, which was statistically lesser than open-VPS (P = 0.020) and LAVPS-NF (P = 0.042). After surgery, pain management lasted for more than 5 days in 30 patients (17 in open-VPS, 7 in LAVPS-NF, and 6 in LAVPS-TPF; P > 0.05). A total of 14 patients experienced abdominal pain after hospital discharge (10 in open-VPS, 2 in LAVPS-NF, and 2 in LAVPS-TPF; P > 0.05). In addition, 13 patients experienced headaches (6 in open-VPS, 9 in LAVPS-NF, and none in LAVPS-TPF; P < 0.001 between the two LAVPS groups). Additionally, dizziness (n = 8, P = 0.037 LAVPS-NF vs. LAVPS-TPF), unsteady gait (n = 9, P = 0.016 LAVPS-NF vs. LAVPS-TPF), and epilepsy (n = 3, P > 0.999) were reported. During follow-up, 137 patients recovered well with mRS = 0 or 1 (69 in open-VPS, 28 in LAVPS-NF, and 40 in LAVPS-TPF; P > 0.05). However, 11 patients died during follow-up (reasons for deaths included shunt construction and/or infection, brain tumor, intracranial hemorrhage, pneumonia, traumatic brain injury-related multiorgan functional deficit, and unknown causes).

Figure 3. Survival curves of shunts in all patients (A, P = 0.045), patients with history of abdominal surgeries history (B, P = 0.010), patients with Glasgow coma scale score of 13–15 (C, P = 0.019), and revision surgeries (D, P = 0.008). Open-VPS (blue), ventriculoperitoneal shunt with conventional laparotomy; LAVPS-NF (green), laparoscopy-assisted ventriculoperitoneal shunt with no fixation; LAVPS-TPF (red), LAVPS with two-point fixation.
A total of 51 patients with history of abdominal surgeries (19 open-VPS, 13 LAVPS-NF, and 19 LAVPS-TPF; Table 2) were examined, and shunt failure was documented in 13 cases (eight open-VPS and five LAVPS-NF, P = 0.003 and 0.006 for LAVPS-TPF vs. open-VPS and LAVPS-NF). Among them, six cases were reported in the open-VPS group and three cases in the LAVPS-NF group at 12 months post-surgery, while no issues were reported in the LAVPS-TPF group (P = 0.020 and 0.058 vs. open-VPS and LAVPS-NF groups, respectively). Shunt failure rates decreased in the LAVPS-TPF group (P = 0.0145, Figure 3B). Among them, six and three shunt revisions were performed in the open-VPS (P = 0.020 vs. LAVPS-TPF) and LAVPS-NF groups (P = 0.058 vs. LAVPS-TPF), respectively. After surgery, seven patients required analgesia for more than 5 days, and four patients reported persistence of abdominal pain after discharge. During follow-up, eight cases reported neurological complications with no significant differences (P > 0.05). A total of 13, six, and 16 patients of the open-VPS, LAVPS-NF, and LAVPS-TPF groups were satisfied with their recovery (P = 0.049 between the two LAVPS groups).
Then, patients of different GCS levels were investigated. Among 152 patients under mild level (79 open-VPS, 34 LAVPS-NF, and 39 LAVPS-TPF; Table 3), shunt failure occurred in 14, 7, and no patients of the open-VPS, LAVPS-NF (P = 0.694 vs. open-VPS), and LAVPS-TPF groups (P = 0.004 vs. open-VPS; P = 0.003 vs. LAVPS-NF), respectively. In the first 12 months after VPS, shunt failure occurred in 11 patients of the open-VPS group (P = 0.015 vs. LAVPS-TPF) and 4 patients of the LAVPS-NF group (P = 0.043 vs. LAVPS-TPF). The statistical difference among the three groups was observed in the shunt non-failure survival curve analysis (P = 0.021, Figure 3C). After open-VPS surgery, 13 shunt-related complications (i.e., eight obstructions, three infections, and two pseudocysts) were recorded, with 7 records in the LAVPS-NF group (P = 0.598 vs. open-VPS) and none in the LAVPS-TPF group (P = 0.005 vs. open-VPS; P = 0.003 vs. LAVPS-NF). Nine open-VPS and four LAVPS-NF were repaired thereafter with statistical significance (P = 0.029 and 0.043, respectively) compared to LAVPS-NPF (n = 0). A total of 24 patients still required analgesia after 5 days post-surgery (P > 0.05), and 12 patients had abdominal pain after discharge (P > 0.05 between the three groups). During follow-up, only one case with neurological complications (i.e., epilepsy) was recorded in the LAVPS-TPF, with P = 0.301 (vs. open-VPS, n = 12) and P = 0.001 (vs. LAVPS-NF, n = 10). Among them, four patients and seven patients manifested headaches after open-VPS (P = 0.017 vs. LAVPS-TPF) and LAVPS-NF (P = 0.003 vs. LAVPS-TPF), respectively; four patients had headaches after open-VPS (P > 0.999 vs. LAVPS-TPF) and LAVPS-NF (P = 0.043 vs. LAVPS-TPF). By the end of the follow-up, 120 patients recovered well (58 open-VPS, 27 LAVPS-NF, and 35 LAVPS-TPF; P > 0.05); however, five patients (four open-VPS and one LAVPS-NF) died.
However, no significant differences were detected between the open-VPS (n = 18) and LAVPS-TPF (n = 7) groups of the moderate-level patients (Supplementary Table S1). Owing to the limited number of patients in the severe-level subgroup (eight open-VPS, four LAVPS-NF, and three LAVPS-TPF; Supplementary Table S2), statistical analysis was not performed.
A total of 28 revision surgery records (eight open-VPS, eight LAVPS-NF, and 12 LAVPS-TPF) were investigated (Table 4). Six shunts failed after open-VPS surgery (four in the first 12 months) with five repair surgeries, while seven shunts failed with five repair surgeries after LAVPS-NF (P > 0.999). Conversely, no shunt dysfunction or complication occurred in the LAVPS-TPF group (P = 0.001 vs. open-VPS; P < 0.001 vs. LAVPS-NF). The 12-month functional shunt rates were improved in the LAVPS-TPF groups (P = 0.014). The shunt failure rates declined in the LAVPS-TPF groups (P < 0.001, Figure 3D). Unsteady gait and headaches persisted after two open-VPS and six LAVPS-NF surgeries, respectively. No patients had neurological symptoms after LAVPS-TPF surgeries (P = 0.001 vs. LAVPS-NF). Post-surgery analgesia treatment lasted for more than 5 days in four patients in the three groups (P > 0.05), and abdominal pain occurred in two patients in the open-VPS group (P > 0.05). At the end of the follow-up, optimal mRS scores were noted after 7 open-VPS, 1 LAVPS-NP, and 12 LAVPS-TPF surgeries (P < 0.001 between the LAVPS-NP and LAVPS-TPF).
Shunt survival and outcomes of patients with NPH (32 open-VPS, 16 LAVPS-NF, and 8 LAVPS-TPF), the elderly (over 60 years), and patients with BMI > 24 were also analyzed with no significant difference (tables in Supplementary Material).
Since the first application of laparoscopy in HC by Dr. Rodgers in 1978, LAVPS has been suggested as a safe and effective approach in reducing the incidence of postoperative infection and complications compared to small-incision laparotomy VPS (3, 4, 8–10). The most significant advantage of LAVPS is the minimally invasive surgery with visualization that allows the accurate placement of the catheter (11–14). Different studies have demonstrated that the failure rate of laparoscopic surgery is lower (14.1%–15%) than that of laparotomy surgeries (16.9%–18.3%) (11, 15, 16). Additionally, the 30-day revision rate was significantly reduced in laparoscopic surgery (0%–1.2%), while secondary surgery rates at 6 and 12 months were not different (17, 18). In our study, the 12-month shunt failure rates were lowered by LAVPS-TPF (2.04%) rather than LAVPS-NF (12.50%) compared to open-VPS (14.29%), along with revision and complication rates.
A specific position for fixing the shunt requires further exploration. Some neurosurgeons believe that the catheter will wiggle into the pelvis with intestinal peristalsis (11, 19). However, distal shunt obstructions could be resolved by adjusting the catheter position under laparoscopy (20). In a retrospective study with 810 cases, Naftel et al. (4) concluded that blind placement of catheters in open-VPS might cause mistakes and increase the incidence of catheter distal obstruction (35.7%), which was reduced by LAVPS (4.8%). Rigante et al. (14) concur that shunt obstruction was associated with catheter position of the catheter. Thus, fixation could reduce catheter-related complications.
More studies revealed that the hepatic septal space, which is the highest position of the abdominal cavity in both supine and sitting positions, is ideal for the abdominal shunt to prevent omental wrapping and organ damage (21, 22). Svoboda et al. (23) placed the catheter through a falciform ligament defect, which reduced migration and obstruction in idiopathic NPH (iNPH). During treatment in 36 patients, Wang et al. (24) placed the catheter into the right subphrenic space through a hole of the sickle ligament with no complications during follow-up. Shao et al. (25) applied screws and vascular clips to anchor the catheter in the abdominal cavity or insert the catheter into the hepatic diaphragm through the falciform ligament. There were no catheter obstructions or infections during the 1-year follow-up. During our practice, after catheter placement at the liver's superoposterior surface, the catheter still migrated to a lower level as reported in a previous study (11, 19). To secure the distal tip safely, a silk suture was used to secure it at the falciform ligament. The highest position of both the falciform ligament and abdominal cavity, with a distance from the transition of the diaphragm and anterior abdominal wall, was determined as the fixing point. To prevent intractable hiccups, breathing issues (i.e., painful respiration and pneumothorax, among others), or pericardial injury, the distance is ∼2 cm to the diaphragm and could be adapted to anatomical variations (26).
To further enhance the benefits, a tight knot on the liver round ligament was employed to secure the catheter body on the liver septum. Additionally, the intra-abdominal region was limited to ∼15 cm to avoid a long curve reaching the omentum. In our study, infection was reported in one patient, but no patients had a distal catheter obstruction during follow-up in the LAVPS-TPF group.
The increased intracranial pressure (ICP) secondary to laparoscopic pneumoperitoneum has risks and causes temporary partial or complete shunt obstruction (27), which will immediately resolve after the removal of the laparoscope. An ICP of 25 cm H2O at a pneumoperitoneum pressure of 8–15 mmHg was considered safe (28, 29). The fixation procedure does not require a higher pressure or a longer period for pneumoperitoneum. In the present study, the pneumoperitoneum pressure was controlled at 12 mmHg, with the pneumoperitoneum time controlled for no more than 60 min (29). Releasing the pneumoperitoneum pressure slowly and confirming a clear CSF drainage before exiting the laparoscope are highly suggested.
Also, in our present study, LAVPS-TPF does not need additional operating time, in-hospital days, and pain treatments. Previous studies reported lesser blood loss, shorter operating time, faster recovery, and decreased analgesic use in LAVPS (4, 11–16, 18, 30). In our research, however, in-hospital days in LAVPS-TPF were longer than those in the open-VPS group. This could be attributed to more patients with history of abdominal surgery and revision surgeries in the LAVPS-TPF group, considering the non-significant results in those subgroups.
The most common rationale for shunt failure is the mechanical obstruction of the abdominal catheter, which can be significantly decreased by LAVPS (3.8%–4.8%) compared to open-VPS surgery (19.2%–35.7%) (4, 9, 31). Dislocation and displacement were also reduced in multiple studies (3, 32–34). With smaller incisions, LAVPS also reduced intra-abdominal infectious complications (0%–1.6% in LAVPS vs. 2.6%–5% in open-VPS) (9, 11, 15, 16, 35, 36). Regarding the different disease etiologies and conditions in patients enrolled in the present study, LAVPS-TPF did not improve the outcomes of all HC patients.
In patients with an abdominal surgery history, LAVPS has the advantage to deal with the common post-surgery intraperitoneal adhesions and avoid intra-abdominal injuries (37–39). This visual approach is excellent for revision surgeries to diagnose and address abdominal complications (e.g., peritoneal adhesions and CSF pseudocysts, among others, videos available in the Supplementary Material) (32, 40–42). Though LAVPS-NF did not statistically reveal advantages in patients with an abdominal history or revision surgeries in our study, LAVPS-TFP improved the shunt survival rates, prevented revision surgeries, and promoted better recovery after surgery. It was also consistent with our assumption that the two-point fixation technique protected shunts from the omentum.
Patients under mild levels were more likely to benefit from LAVPS-TPF instead of patients under severe levels, most of whom were acquired due to brain injuries (i.e., hemorrhage and trauma). Contrary to publications that showed LAVPS reduced complications and promoted cognitive and gait recovery in patients with NPH (4, 18, 30, 43), the advantage of LAVPS-TPF was not presented in our study compared to LAVPS-NF or open-VPS.
Patients with obesity would benefit from laparoscopic assistance by reducing the incidence of infections and revision surgeries, especially in those with BMI over 30 (39). However, in the present study, there was no difference between the outcomes after open-VPS and LAVPS surgeries for patients with BMI > 24 (Supplementary Table S5). Although the fixation seemed to reduce failure rates, shunt complications, and neurological complications compared with LAVPS-NF groups, it did not improve patients’ mRS scores and outcomes. The obviously limited population of patients with higher BMI and paucity of other obesity indices (e.g., abdominal circumference and waist-to-hip ratio) could be attributed to the above findings.
As a retrospective study, the evidence level for the conclusions is relatively lower. In the present study, three senior neurosurgeons and two gastrointestinal surgeons participated in determining surgical approaches and performing surgical procedures, probably leading to inevitable systemic bias. Patients who underwent LAVPS-NF and LAVPS-TPF were limited. Future studies with larger sample sizes, randomized controlled designs, and multiple-center cooperation are required to further confirm the advantages of LAVPS-TPF. Complication-related outcomes were potentially biased, mostly from subjective symptoms such as pain, headache, and dizziness, which lacked objective evaluation in the present self-adjudicated study. Also, risk factors for complications, repair surgeries, and terrible outcomes warrant further investigation. Additionally, we only focused on adult patients with HC. Although pediatric patients can also benefit from LAVPS (44, 45), catheter fixation should be discussed carefully.
In this study, our data showed that LAVPS-TPF statistically reduced shunt failure rates and the incidence of abdominal shunt-related complications. This novel two-point fixation technique further enhanced the benefits of LAVPS, especially in patients with abdominal history, higher GCS scores, and repair surgeries. Additionally, LAVPS-TPF decreased the frequency of revision surgeries in patients with history of abdominal surgery and revision surgeries.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
J-NW and YZ performed the study; searched the literature, collected, analyzed, and interpreted data; and wrote the first draft of the manuscript. LW analyzed data and contributed to the substantial revision of the manuscript. JG and JW collected data and contributed to the revision of the manuscript. DL and HZ supervised and conceived the study, interpreted data, and wrote and revised the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Nature Science Foundation of China (grant number 81771334), which had no role in study design, data collection and analysis, decision to publish, and or preparation of the paper.
We would like to gratefully acknowledge Xiao-Ming Shuai, MD, PhD, and Xing-Hua Liu, MD, PhD, of the Dept. of Gastrointestinal Surgery for performing laparoscopic procedures. We also thank Harley R and Enago™ for the language and grammar editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1135818/full#supplementary-material
BMI, body mass index; GCS, Glasgow coma scale; HC, hydrocephalus; VPS, ventriculoperitoneal shunt; LAVPS, laparoscopy-assisted ventriculoperitoneal shunt; open-VPS, conventional VPS with laparotomy; LAVPS-NF, conventional LAVPS with no fixation; LAVPS-TPF, novel LAVPS with two-point fixation; CSF, cerebrospinal fluid; NPH, normal pressure hydrocephalus; iNPH, idiopathic NPH; mRS, modified Rankin scores.
1. Kahle KT, Kulkarni AV, Limbrick DD, Warf BC. Hydrocephalus in children. Lancet. (2016) 387(10020):788–99. doi: 10.1016/S0140-6736(15)60694-8
2. Dakurah TK, Adams F, Iddrissu M, Wepeba GK, Akoto H, Bankah P, et al. Management of hydrocephalus with ventriculoperitoneal shunts: review of 109 cases of children. World Neurosurg. (2016) 96:129–35. doi: 10.1016/j.wneu.2016.06.111
3. Phan S, Liao J, Jia F, Maharaj M, Reddy R, Mobbs RJ, et al. Laparotomy vs minimally invasive laparoscopic ventriculoperitoneal shunt placement for hydrocephalus: a systematic review and meta-analysis. Clin Neurol Neurosurg. (2016) 140:26–32. doi: 10.1016/j.clineuro.2015.10.025
4. Naftel RP, Argo JL, Shannon CN, Taylor TH, Tubbs RS, Clements RH, et al. Laparoscopic versus open insertion of the peritoneal catheter in ventriculoperitoneal shunt placement: review of 810 consecutive cases. J Neurosurg. (2011) 115(1):151–8. doi: 10.3171/2011.1.JNS101492
5. Mehta R, Chinthapalli K. Glasgow coma scale explained. BMJ. (2019) 365:l1296. doi: 10.1136/bmj.l1296
6. Patel N, Rao VA, Heilman-Espinoza ER, Lai R, Quesada RA, Flint AC. Simple and reliable determination of the modified Rankin scale score in neurosurgical and neurological patients: the mRS-9Q. Neurosurgery. (2012) 71(5):971–5; discussion 975. doi: 10.1227/NEU.0b013e31826a8a56
7. Langezaal LCM, van der Hoeven E, Mont'Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. (2021) 384(20):1910–20. doi: 10.1056/NEJMoa2030297
8. Rodgers BM, Vries JK, Talbert JL. Laparoscopy in the diagnosis and treatment of malfunctioning ventriculo-peritoneal shunts in children. J Pediatr Surg. (1978) 13(3):247–53. doi: 10.1016/S0022-3468(78)80395-9
9. Schubert F, Fijen B, Krauss J. Laparoscopically assisted peritoneal shunt insertion in hydrocephalus: a prospective controlled study. Surg Endosc Other Interv Tech. (2005) 19(12):1588–91. doi: 10.1007/s00464-005-0164-z
10. Khaitan L, Brennan EJ Jr. A laparoscopic approach to ventriculoperitoneal shunt placement in adults. Surg Endosc. (1999) 13(10):1007–9. doi: 10.1007/s004649901157
11. Schucht P, Banz V, Trochsler M, Iff S, Krähenbühl AK, Reinert M, et al. Laparoscopically assisted ventriculoperitoneal shunt placement: a prospective randomized controlled trial. J Neurosurg. (2015) 122(5):1058–67. doi: 10.3171/2014.9.JNS132791
12. Park YS, Park IS, Park KB, Lee CH, Hwang SH, Han JW. Laparotomy versus laparoscopic placement of distal catheter in ventriculoperitoneal shunt procedure. J Korean Neurosurg Soc. (2010) 48(4):325–9. doi: 10.3340/jkns.2010.48.4.325
13. Raysi Dehcordi S, De Tommasi C, Ricci A, Marzi S, Ruscitti C, Amicucci G, et al. Laparoscopy-assisted ventriculoperitoneal shunt surgery: personal experience and review of the literature. Neurosurg Rev. (2011) 34(3):363–70; discussion 370–1. doi: 10.1007/s10143-011-0309-6
14. Rigante L, Navarro R, Roser F. Minimal exposure maximal precision ventriculoperitoneal shunt: how I do it. Acta Neurochir (Wien). (2019) 161(8):1619–22. doi: 10.1007/s00701-019-03968-4
15. Turner RD, Rosenblatt SM, Chand B, Luciano MG. Laparoscopic peritoneal catheter placement: results of a new method in 111 patients. Neurosurgery. (2007) 61(3 Suppl):167–72; discussion 172–4. doi: 10.1227/01.neu.0000289730.27706.e6
16. Nigim F, Thomas AJ, Papavassiliou E, Schneider BE, Critchlow JF, Chen CC, et al. Ventriculoperitoneal shunting: laparoscopically assisted versus conventional open surgical approaches. Asian J Neurosurg. (2014) 9(2):72–81. doi: 10.4103/1793-5482.136717
17. Gravbrot N, Aguilar-Salinas P, Walter CM, Dumont TM. Laparoscopically assisted ventriculoperitoneal shunt placement is not cost-effective nor preventive for distal shunt malfunction. World Neurosurg. (2020). 137:e308–e314. doi: 10.1016/j.wneu.2020.01.193
18. Catapano JS, Mezher AW, Wang DJ, Whiting AC, Mooney MA, Bohl MA, et al. Laparoscopic-assisted ventriculoperitoneal shunt placement and reduction in operative time and total hospital charges. World Neurosurg. (2020) 135:e623–e8. doi: 10.1016/j.wneu.2019.12.086
19. Liang YM, Guo GY, Bao YH, Ding SH, Pan YH, Wu HB, et al. No special management for peritoneal catheter in ventriculo-peritoneal shunt is required. Chinese Journal of Neurosurgery. (2011) 27(4):331–4. doi: 10.3760/cma.j.issn.1001-2346.2011.04.003
20. Kusano T, Miyazato H, Shimoji H, Hirayasu S, Isa T, Shiraishi M, et al. Revision of ventriculo-peritoneal shunt under laparoscopic guidance in patients with hydrocephalus. Surg Laparosc Endosc. (1998) 8(6):474–6. doi: 10.1097/00019509-199812000-00015
21. Yang X, Liang R, Zhang Y. An unusual complication of ventriculoperitoneal shunt with bladder perforation and extrusion through the urethra orifice in an adult male patient. Int J Neurosci. (2019) 129(1):101–2. doi: 10.1080/00207454.2018.1486305
22. Li B, Zhang Q, Liu J, Yu H, Hu S. Clinical application of a laparoscope in ventri-peritoneal shunting. Minim Invasive Ther Allied Technol. (2007) 16(6):367–9. doi: 10.1080/13645700701699547
23. Svoboda SM, Park H, Naff N, Dorai Z, Williams MA, Youssef Y. Preventing distal catheter obstruction in laparoscopic ventriculoperitoneal shunt placement in adults: the “falciform technique”. J Laparoendosc Adv Surg Tech A. (2015) 25(8):642–5. doi: 10.1089/lap.2015.0196
24. Wang G, Yu J, Luan Y, Han Y, Fu S. Novel type of peritoneocentesis trocar-assisted distal ventriculoperitoneal shunt placement with supervision via a one-port laparoscope. Exp Ther Med. (2017) 14(4):3413–8. doi: 10.3892/etm.2017.4926
25. Shao Y, Li M, Sun JL, Wang P, Li XK, Zhang QL, et al. A laparoscopic approach to ventriculoperitoneal shunt placement with a novel fixation method for distal shunt catheter in the treatment of hydrocephalus. Minim Invasive Neurosurg. (2011) 54(1):44–7. doi: 10.1055/s-0031-1271680
26. Seiler C, Glättli A, Metzger A, Czerniak A. Injury to the diaphragm and its repair during laparoscopic cholecystectomy. Surg Endosc. (1995) 9(2):193–4. doi: 10.1007/BF00191964
27. Uzzo RG, Bilsky M, Mininberg DT, Poppas DP. Laparoscopic surgery in children with ventriculoperitoneal shunts: effect of pneumoperitoneum on intracranial pressure–preliminary experience. Urology. (1997) 49(5):753–7. doi: 10.1016/S0090-4295(97)00233-1
28. Kamine TH, Papavassiliou E, Schneider BE. Effect of abdominal insufflation for laparoscopy on intracranial pressure. JAMA Surg. (2014) 149(4):380–2. doi: 10.1001/jamasurg.2013.3024
29. Staikou C, Tsaroucha A, Mani A, Fassoulaki A. Transcranial Doppler monitoring of middle cerebral flow velocity in a patient with a ventriculoperitoneal shunt undergoing laparoscopy. J Clin Monit Comput. (2012) 26(6):487–9. doi: 10.1007/s10877-012-9380-y
30. Nigim F, Critchlow JF, Schneider BE, Chen C, Kasper EM. Shunting for hydrocephalus: analysis of techniques and failure patterns. J Surg Res. (2014) 191(1):140–7. doi: 10.1016/j.jss.2014.03.075
31. Chen J, Liu C, Zhu H, Fu M, Lin F, Liu J, et al. [Laparoscopic ventriculoperitoneal shunt with temporary external drainage for hydrocephalus: a comparison with conventional ventriculoperitoneal shunt]. Nan Fang Yi Ke Da Xue Xue Bao. (2012) 32(12):1836–40. doi: 10.3969/j.issn.1673-4254.2012.12.034
32. Sellier A, Monchal T, Joubert C, Bourgouin S, Desse N, Bernard C, et al. Update about ventriculoperitoneal shunts: when to combine visceral and neurosurgical management? J Visc Surg. (2019) 156(5):423–31. doi: 10.1016/j.jviscsurg.2019.03.003
33. Alyeldien A, Jung S, Lienert M, Scholz M, Petridis AK. Laparoscopic insertion of the peritoneal catheter in ventriculoperitoneal shunting. Review of 405 consecutive cases. Int J Surg. (2016) 33(Pt A):72–7. doi: 10.1016/j.ijsu.2016.07.052
34. He M, Ouyang L, Wang S, Zheng M, Liu A. Laparoscopy versus mini-laparotomy peritoneal catheter insertion of ventriculoperitoneal shunts: a systematic review and meta-analysis. Neurosurg Focus. (2016) 41(3):E7. doi: 10.3171/2016.5.FOCUS1637
35. Targarona EM, Balagué C, Knook MM, Trías M. Laparoscopic surgery and surgical infection. Br J Surg. (2000) 87(5):536–44. doi: 10.1046/j.1365-2168.2000.01429.x
36. Varela JE, Wilson SE, Nguyen NT. Laparoscopic surgery significantly reduces surgical-site infections compared with open surgery. Surg Endosc. (2010) 24(2):270–6. doi: 10.1007/s00464-009-0569-1
37. Schievink WI, Wharen RE Jr., Reimer R, Pettit PD, Seiler JC, Shine TS. Laparoscopic placement of ventriculoperitoneal shunts: preliminary report. Mayo Clin Proc. (1993) 68(11):1064–6. doi: 10.1016/S0025-6196(12)60899-4
38. Moris D, Chakedis J, Rahnemai-Azar AA, Wilson A, Hennessy MM, Athanasiou A, et al. Postoperative abdominal adhesions: clinical significance and advances in prevention and management. J Gastrointest Surg. (2017) 21(10):1713–22. doi: 10.1007/s11605-017-3488-9
39. Khalid SI, Nunna RS, Maasarani S, Shanker RM, Behbahani M, Edmondson CP, et al. Laparoscopic-assisted versus mini-open laparotomy for ventriculoperitoneal shunt placement in the Medicare population. Neurosurgery. (2021) 88(4):812–8. doi: 10.1093/neuros/nyaa541
40. Logghe H, Maa J, McDermott M, Oh M, Carter J. Laparoscopic shunt revision avoids many complications of open shunt revision and has outcomes similar to first-time shunt placement. Am Surg. (2015) 81(3):305–8. doi: 10.1177/000313481508100335
41. Fahy AS, Tung S, Lamberti-Pasculli M, Drake J, Kulkarni A, Gerstle JT. Laparoscopic revision of ventriculoperitoneal shunts in pediatric patients may result in fewer subsequent peritoneal revisions. J Laparoendosc Adv Surg Tech A. (2019) 29(1):82–7. doi: 10.1089/lap.2018.0128
42. Martin K, Baird R, Farmer JP, Emil S, Laberge JM, Shaw K, et al. The use of laparoscopy in ventriculoperitoneal shunt revisions. J Pediatr Surg. (2011) 46(11):2146–50. doi: 10.1016/j.jpedsurg.2011.07.001
43. Rinaldo L, Lanzino G, Elder BD. Predictors of distal malfunction after ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus and effect of general surgery involvement. Clin Neurol Neurosurg. (2018) 174:75–9. doi: 10.1016/j.clineuro.2018.09.009
44. Fahy AS, Tung S, Lamberti-Pasculli M, Drake J, Kulkarni AV, Gerstle JT. Laparoscopic insertion of ventriculoperitoneal shunts in pediatric patients—a retrospective cohort study. J Pediatr Surg. (2019) 54(7):1462–6. doi: 10.1016/j.jpedsurg.2018.07.001
Keywords: hydrocephalus, ventriculoperitoneal shunt, laparoscopy-assisted ventriculoperitoneal shunt, two-point fixation, shunt survival, liver ligaments
Citation: Wu J-N, Zhou Y-J, Wang L, Gan J-L, Wang J, Zhao H-Y and Lei D-Q (2023) Two-point fixation enhanced the outcome of laparoscopy-assisted ventriculoperitoneal shunt in adult patients with hydrocephalus: a retrospective study. Front. Surg. 10:1135818. doi: 10.3389/fsurg.2023.1135818
Received: 9 February 2023; Accepted: 26 June 2023;
Published: 13 July 2023.
Edited by:
Altay Sencer, Istanbul University, TürkiyeReviewed by:
Duygu Dolen, Yale University, United States© 2023 Wu, Zhou, Wang, Gan, Wang, Zhao and Lei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong-Yang Zhao aHl6aGFvNzUwQHNpbmEuY29t De-Qiang Lei bGRxdHpAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.