- 1Department of Surgery, East Carolina University, Brody School of Medicine, Greenville, NC, United States
- 2Department of Specialty Medicine, Rocky Vista University, College of Osteopathic Medicine, Parker, CO, United States
- 3Department of Spine Surgery, NeuroSpine Zürich, Zürich, Switzerland
- 4Institute for Clinical and Experimental Trauma-Immunology, University Hospital Ulm, Ulm, Germany
- 5University of Colorado, Boulder, CO, United States
- 6CNine Biosolutions LLC, Birmingham, AL, United States
Editorial on the Research Topic
The impact of COVID-19 on immune system-related complications in surgical patients
A key lesson learned from the coronavirus disease 2019 (COVID-19) pandemic is reflected by the finding that patients with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection have a significantly increased mortality and complication rates after surgery, compared to surgical patients who are SARS-CoV-2 negative (1–3). This phenomenon has been primarily attributed to respiratory failure from SARS-CoV-2 pneumonia and acute respiratory distress syndrome (ARDS) subsequent to mechanical ventilation for general anesthesia during surgical procedures (4). In addition to the well-known pulmonary complications, young patients with COVID-19 are particularly susceptible to adverse effects originating from a dysfunction of the innate immune system (5–7). This includes the release of a “cytokine storm” and activation of the complement system which promotes a systemic environment of hyperinflammation and hypercoagulability (8–15). These pathophysiological changes may contribute to the increased perioperative risk of thromboembolic complications and the high postoperative mortality observed in surgical patients with COVID-19 (16–20). The current special edition in Frontiers in Surgery was designed to improve the understanding of the immune-mediated pathophysiological events that lead to adverse outcomes in the vulnerable population of COVID-19 patients undergoing surgical procedures.
An authoritative review from an international consensus group coherently summarized the current state-of-the-art in the field as it pertains to the pathogenesis of SARS-CoV-2-mediated immune-thrombotic complications after surgery Bunch et al. The authors introduced the new entity of “COVID-associated coagulopathy” and explained the underlying hypothesis related to SARS-CoV-2-induced endothelitis as the root cause of an imbalance between fibrinolysis and fibrinolytic shutdown Bunch et al. The clinical implications pertain to adjudicating the timing of elective surgical procedures in COVID-19 patients and to monitor the “rollercoaster” stages of COVID-associated coagulopathy by point-of-care-guided viscoelastic hemostatic assays, such as thromboelastography (Figure 1). The authors furthermore provided specific clinical recommendations for perioperative anticoagulation in COVID-19 patients for a variety of surgical subspecialties, including general surgery, cardiothoracic and vascular surgery, reconstructive surgery, obstetrics, orthopedics, and neurosurgery Bunch et al. A retrospective observational cohort study from the Middle East confirmed the notion of an increased perioperative mortality in COVID-19 patients undergoing orthopedic surgery and spine procedures during the early surges of the pandemic in 2020 with a demonstrated protective effect of SARS-CoV-2 vaccinations in 2021 Kim et al. These findings furthermore provided additional support to the safety and efficacy of mRNA vaccines in the selected cohort of surgical COVID-19 patients (21).
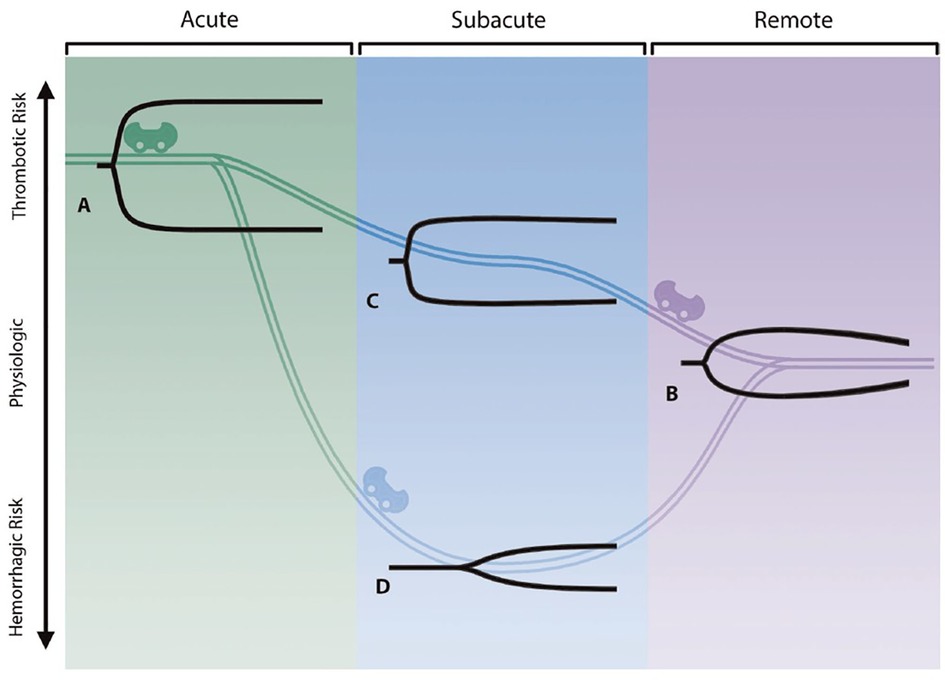
Figure 1. The three stages constituting the “rollercoaster” phenomenon of COVID-associated coagulopathy, as determined by thromboelastography (TEG). See original publication for detailed explanation of the content (21).
Another observational study from a tertiary referral center in Taiwan assessed patient-reported outcome measures (PROMs) after spine surgery and determined that patients had worse subjective postoperative outcomes during the COVID-19 pandemic Lin et al. While the root cause of the decrease in PROMs remains speculative, the authors recommend consideration for psychological support for surgical patients during the pandemic to improve postoperative outcomes Lin et al. A similar publication from Germany reported unchanged infectious complication rates after spinal surgery during the COVID-19 pandemic from April 2020 to June 2021, when compared to a historic pre-pandemic cohort of spine surgery patients managed at the same institution from January 2019 until March 2020 (22). The authors attributed the lack of decreased surgical site infections, in spite of the COVID-19 preventative measures, to higher rates of emergency surgical spine procedures during the pandemic (22). The special edition concludes with a case report on three patients with COVID-19 who sustained severe osteomyelitis of the jaw as a rare but severe infectious complication Kvolik Pavic et al. The authors hypothesized that the SARS-CoV-2-induced immune dysfunction and microvascular changes contributed to the increased vulnerability for severe infection in patients with COVID-19 Kvolik Pavic et al.
In summary, the profound immunological derangements induced by SARS-CoV-2 infection significantly increase the risk of perioperative complications and adverse outcomes in COVID-19 patients undergoing surgical procedures. Delaying elective surgery for 6 weeks after infection has been proposed by surgical societies as a strategy to prevent adverse outcomes. However, this conservative strategy represents a double-edged sword due to the risk associated with depriving patients from access to timely surgical care (23). There are currently multiple anti-inflammatory pharmacological agents available to attenuate the SARS-CoV-2-induced immune system derangements, including complement inhibitors (8, 24, 25) and monoclonal antibodies to pro-inflammatory cytokines, such as interleukin (IL)-1, IL-6, IL-22 or IL-33 (26–28). Now at three years into the pandemic, the lessons learned from the COVID-related immunopathology will allow for more specifically targeted treatment modalities to inhibit SARS-CoV-2-induced hyperinflammation and the related immuno-thrombotic sequelae responsible for the high complication rates and increased mortality in surgical COVID-19 patients.
Author contributions
PFS wrote the first draft of the manuscript. VPS summarized the content of the published manuscripts included in the special edition. SW, MSH-L, and SRB contributed with critical revisions of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The first author (PFS) is employed by HCA Healthcare. The views expressed in this editorial exclusively represent the author’s personal perspective and do not necessarily represent official views of HCA Healthcare or any of its affiliated entities. The senior author (SRB) was employed by CNine Biosolutions, LLC, and declares the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All other authors declare no conflict of interest related to this editorial.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Abate SM, Mantefardo B, Basu B. Postoperative mortality among surgical patients with COVID-19: a systematic review and meta-analysis. Patient Saf Surg. (2020) 14:37. doi: 10.1186/s13037-020-00262-6
2. Egol KA, Konda SR, Bird ML, Dedhia N, Landes EK, Ranson RA, et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma. (2020) 34(8):395–402. doi: 10.1097/BOT.0000000000001845
3. Colosimo C, Bhuller S, Cornett B, Dziadkowiec O, Yon JR, Weaver J, et al. Perioperative mortality in SARS-CoV-2-positive surgical patients during the first wave of the novel coronavirus pandemic. Br J Surg. (2021) 108(5):e201–2. doi: 10.1093/bjs/znab058
4. Shrestha DB, Sedhai YR, Budhathoki P, Adhikari A, Pokharel N, Dhakal R, et al. Pulmonary barotrauma in COVID-19: a systematic review and meta-analysis. Ann Med Surg (Lond). (2022) 73:103221. doi: 10.1016/j.amsu.2021.103221
5. Diamond MS, Lambris JD, Ting JP, Tsang JS. Considering innate immune responses in SARS-CoV-2 infection and COVID-19. Nat Rev Immunol. (2022) 22(8):465–70. doi: 10.1038/s41577-022-00744-x
6. Auger N, Begin P, Kang H, Lo E, Brousseau E, Healy-Profitos J, et al. Multisystem inflammatory syndrome in adults: comparison with other inflammatory conditions during the COVID-19 pandemic. Respir Med. (2022) 206:107084. doi: 10.1016/j.rmed.2022.107084
7. Kashyap A, Sebastian SA, Krishnaiyer NarayanaSwamy SR, Raksha K, Krishnamurthy H, Krishna B, et al. Molecular markers for early stratification of disease severity and progression in COVID-19. Biol Methods Protoc. (2022) 7(1):bpac028. doi: 10.1093/biomethods/bpac028
8. Stahel PF, Barnum SR. Complement inhibition in coronavirus disease (COVID)-19: a neglected therapeutic option. Front Immunol. (2020) 11:1661. doi: 10.3389/fimmu.2020.01661
9. Thomas G, Frederick E, Hausburg M, Goldberg L, Hoke M, Roshon M, et al. The novel immunomodulatory biologic LMWF5A for pharmacological attenuation of the “cytokine storm” in COVID-19 patients: a hypothesis. Patient Saf Surg. (2020) 14:21. doi: 10.1186/s13037-020-00248-4
10. Mastellos DC, Skendros P, Calado RT, Risitano AM, Lambris JD. Efficacy matters: broadening complement inhibition in COVID-19. Lancet Rheumatol. (2021) 3(2):e95. doi: 10.1016/S2665-9913(20)30423-9
11. Sharma S, Tyagi T, Antoniak S. Platelet in thrombo-inflammation: unraveling new therapeutic targets. Front Immunol. (2022) 13:1039843. doi: 10.3389/fimmu.2022.1039843
12. Tierney AL, Alali WM, Scott T, Rees-Unwin KS, Collaboration CNBC, Clark SJ, et al. Levels of soluble complement regulators predict severity of COVID-19 symptoms. Front Immunol. (2022) 13:1032331. doi: 10.3389/fimmu.2022.1032331
13. Lage SL, Rocco JM, Laidlaw E, Rupert A, Galindo F, Kellogg A, et al. Activation of complement components on circulating blood monocytes from COVID-19 patients. Front Immunol. (2022) 13:815833. doi: 10.3389/fimmu.2022.815833
14. Niederreiter J, Eck C, Ries T, Hartmann A, Markl B, Buttner-Herold M, et al. Complement activation via the lectin and alternative pathway in patients with severe COVID-19. Front Immunol. (2022) 13:835156. doi: 10.3389/fimmu.2022.835156
15. Amikishiyev S, Gunver MG, Bektas M, Aghamuradov S, Ince B, Koca N, et al. Criteria for hyperinflammation developing in coronavirus disease-19: analysis of two cohorts from different periods of the pandemic. Arthritis Rheumatol. (2022). doi: 10.1002/art.42417. [Epub ahead of print]36508470
16. Wright EV, Musbahi O, Singh A, Somashekar N, Huber CP, Wiik AV. Increased perioperative mortality for femoral neck fractures in patients with coronavirus disease 2019 (COVID-19): experience from the United Kingdom during the first wave of the pandemic. Patient Saf Surg. (2021) 15:8. doi: 10.1186/s13037-020-00279-x
17. Stahel VP, Blum SD, Anand P. The impact of immune dysfunction on perioperative complications in surgical COVID-19 patients: an imperative for early immunonutrition. Patient Saf Surg. (2022) 16:14. doi: 10.1186/s13037-022-00323-y
18. Ferraro JJ, Reynolds A, Edoigiawerie S, Seu MY, Horen SR, Aminzada A, et al. Associations between SARS-CoV-2 infections and thrombotic complications necessitating surgical intervention: a systematic review. World J Methodol. (2022) 12(6):476–87. doi: 10.5662/wjm.v12.i6.476
19. Koutalos AA, Ntalouka MP, Angelis FA, Hantes M, Arnaoutoglou E. Venous thromboembolism and major adverse cardiovascular events in patients with hip fractures suffering from SARS-CoV-2 infection: a systematic review. Hip Int. (2022):11207000221132489. doi: 10.1177/11207000221132489. [Epub ahead of print]36285337
20. Karna ST, Gouroumourty R, Ahmad Z, Trivedi S, Thaware P, Singh P. Performance of prognostic scores in prediction of 30-day postoperative mortality in COVID-19 patients after emergency surgery: a retrospective cohort study. J Postgrad Med. (2022) 68(4):199–206. doi: 10.4103/jpgm.jpgm_1197_21
21. Anand P, Stahel VP. The safety of COVID-19 mRNA vaccines: a review. Patient Saf Surg. (2021) 15:20. doi: 10.1186/s13037-021-00291-9
22. Jankovic D, Krenzlin H, Keric N, Ottenhausen M. The impact of SARS-CoV-2 measures on patient samples and complication rates in spine surgery: a single center analysis. Front Surg. (2023):9. doi: 10.3389/fsurg.2022.1086960
23. Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. (2020) 14:8. doi: 10.1186/s13037-020-00235-9
24. Mastellos DC, Pires da Silva BGP, Fonseca BAL, Fonseca NP, Auxiliadora-Martins M, Mastaglio S, et al. Complement C3 vs C5 inhibition in severe COVID-19: early clinical findings reveal differential biological efficacy. Clin Immunol. (2020) 220:108598. doi: 10.1016/j.clim.2020.108598
25. Skendros P, Germanidis G, Mastellos DC, Antoniadou C, Gavriilidis E, Kalopitas G, et al. Complement C3 inhibition in severe COVID-19 using compstatin AMY-101. Sci Adv. (2022) 8(33):eabo2341. doi: 10.1126/sciadv.abo2341. [Epub ahead of print]35977025
26. Davidson M, Menon S, Chaimani A, Evrenoglou T, Ghosn L, Grana C, et al. Interleukin-1 blocking agents for treating COVID-19. Cochrane Database Syst Rev. (2022) 1:CD015308. doi: 10.1002/14651858.cd015308
27. Haibel H, Poddubnyy D, Angermair S, Allers K, Vahldiek JL, Schumann M, et al. Successful treatment of severe COVID-19 pneumonia, a case series with simultaneous interleukin-1 and interleukin-6 blockade with 1-month follow-up. Ther Adv Musculoskelet Dis. (2022) 14:1759720X221116405. doi: 10.1177/1759720X221116405
Keywords: COVID-associated coagulopathy, fibrinolytic shutdown, hyperinflammation, innate immunity, surgical complications
Citation: Stahel PF, Weckbach S, Huber-Lang MS, Stahel VP and Barnum SR (2023) Editorial: The impact of COVID-19 on immune system-related complications in surgical patients. Front. Surg. 10:1132752. doi: 10.3389/fsurg.2023.1132752
Received: 27 December 2022; Accepted: 6 January 2023;
Published: 30 January 2023.
Edited and Reviewed by: Jaimo Ahn, University of Michigan, United States
© 2023 Stahel, Weckbach, Huber-Lang, Stahel and Barnum. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip F. Stahel cGhpbGlwLnN0YWhlbEBnbWFpbC5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Philip F. Stahel
Philip F. Stahel Sebastian Weckbach
Sebastian Weckbach Markus S. Huber-Lang
Markus S. Huber-Lang Vincent P. Stahel
Vincent P. Stahel Scott R. Barnum
Scott R. Barnum