- 1The 2nd Clinical Medical College, Guangzhou University of Traditional Chinese Medicine, Guangzhou, China
- 2Department of Orthopaedic Surgery, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou University of Chinese Medicine, Guangzhou, China
Background: This study aimed to demonstrate that dual-mobility cup total hip arthroplasty (DMC-THA) can significantly improve the quality of life (QOL) of elderly femoral neck fracture patients with severe neuromuscular disease in unilateral lower extremities due to stroke hemiplegia compared to internal fixation (IF).
Methods: Fifty-eight cases of severe neuromuscular disease in the unilateral lower extremities with muscle strength < grade 3/5 due to stroke were retrospectively examined From January 2015 to December 2020. Then, patients were divided into DMC and IF groups. The QOL was examined using the EQ-5D and SF-36 outcome measures. The physical and mental statuses were assessed using the Barthel Index (BI) and e Fall Efficacy Scale-International (FES-I), respectively.
Results: Patients in the DMC group had higher BI scores than those in the IF group at different time point. Regarding mental status, the FES-I mean score was 42.1 ± 5.3 in the DMC group and 47.3 ± 5.6 in the IF group (p = 0.002). For the QOL, the mean SF-36 score was 46.1 ± 18.3 for the health component and 59.5 ± 15.0 for the mental component in the DMC group compared to 35.3 ± 16.2 (p = 0.035), and 46.6 ± 17.4 (p = 0.006) compared to the IF group. The mean EQ-5D-5L values were 0.733 ± 0.190 and 0.303 ± 0.227 in the DMC and IF groups (p = 0.035), respectively.
Conclusion: DMC-THA significantly improved postoperative QOL compared to IF in elderly patients with femoral neck fractures and severe neuromuscular dysfunction in the lower extremity after stroke. The improved outcomes were related to the enhanced early, rudimentary motor function of patients.
Introduction
Stroke is the second leading cause of disability and death worldwide, especially among the elderly, with projected mortality rates of 24.9% by 2030 (1). Up to 88% of stroke patients experience hemiplegia (2). Multiple studies have shown that people with hemiplegia after a stroke have lower bone mineral density and bone strength than the general elderly population (3, 4), thereby increasing the risk of femoral neck fracture (5).
Hip arthroplasty (HA) can substantially improve patients' function, quality of life (QOL), and survival, recognized as the primary therapeutic approach for femoral neck fractures. However, HA is restricted to individuals in good physical condition. Clinically, some elderly stroke patients have severe neuromuscular dysfunction with muscle strength < grade 3/5 (Lovett scale) in one lower extremity. The reduction of periprosthetic muscle and fascia tension increases the risk of prosthesis dislocation and loosening, resulting in poor QOL after surgery (6, 7). Consequently, most doctors believe that internal fixation (IF) is more appropriate than HA for these patients with severe neuromuscular illness in the unilateral lower extremity (muscle strength < grade 3/5) (8). However, for IF, patients should remain in bed long after surgery, which is not conducive to enhancing function and QOL (9, 10).
Currently, how to improve the QOL of people suffering from severe hemiplegia remains unclear. Dual-mobility cup total hip arthroplasty (DMC-THA) might be a viable option (11). Bousquet first presented the idea of dual-mobility hip articulations in 1974 (12). This unique artificial joint system adds a high molecular polyethylene liner between the acetabular cup and femoral head to create two mobility interfaces that can increase the hip joint's range of motion and decrease dislocation risk (13). DMC-THA has successfully treated femoral neck fractures in older patients with neuromuscular diseases. However, most studies were concentrated on patients more prone to recover quickly (14).
Therefore, this study aimed to show that DMC-THA, instead of IF, can significantly improve the QOL for senior femoral neck fracture patients with severe neuromuscular dysfunction in one lower extremity from hemiplegia caused by stroke.
Materials and methods
Herein, we retrospectively analyzed the clinical data of femoral neck fracture patients with severe stroke hemiplegia admitted to the Guangdong Hospital of Traditional Chinese Medicine in Guangzhou, China, between January 2015 and December 2020, with a minimum 1-year follow-up. The inclusion criteria were: femoral neck fracture and stroke hemiplegia, unilateral lower extremity muscular strength < grade 3/5 (Lovett scale) (15), and treatment at our institution. The exclusion criteria included bilateral lower extremity impairment, revision arthroplasty, pathological fractures, less than one year of follow-up, and lack of specific information. We retrieved 233 femoral neck fracture cases with stroke hemiplegia via the electronic medical record (EMR) system. Then, 163 patients who did not fit the inclusion criteria were excluded, seven patients were lost to follow-up or had insufficient data, and five patients passed away. Finally, 58 cases were included for analysis. All cases were separated into two groups based on the surgical technique. This study was authorized by the Investigational Ethics Review Board (Guangdong Hospital of Traditional Chinese Medicine). An exemption from informed consent was acquired from the board.
The patient data consisted of two sections: hospitalization and follow-up information. Hospitalization information comprised demographic characteristics, such as age, gender, and BMI. Clinical data included the kind of femoral neck fracture, activities of daily living (ADL) at admission and discharge, operative blood loss, and surgery time. The ADL was evaluated using the Barthel index (BI). Patients unable or unwilling to attend the hospital were contacted by telephone (16–18). Follow-up records included follow-up time, postoperative complications, reoperation, rehabilitation time, initial time to get off the ground, ADL follow-up assessment, fear of falling (FOF), and QOL. The mortality rate was excluded since most participants were elderly with a high risk of natural death (19). The FOF was assessed with the Fall Efficacy Scale-International (FES-I) to determine the psychological state of patients (20, 21). The QOL was determined with the SF-36 Health Survey and EQ-5D-5L score (22–24). EQ-5D-5L utility scores derived from the Chinese Time-Trade Off (TTO) were used for additional analysis (25). All patient data, including baseline characteristics, clinical data, and follow-up information, were compiled by a research assistant in training who was blind to the assignment.
Means, ranges, and standard deviations were used for descriptive statistics. Categorical variables were compared using the χ2 test, continuous variables were compared using the independent samples t-test, and ranked data were compared using the rank sum test. Statistical analyses were performed with SPSS v. 26.0 (SPSS, Inc., Chicago, IL, United States), and significance levels were set as * p < 0.05; ** p < 0.01; *** p < 0.001.
Results
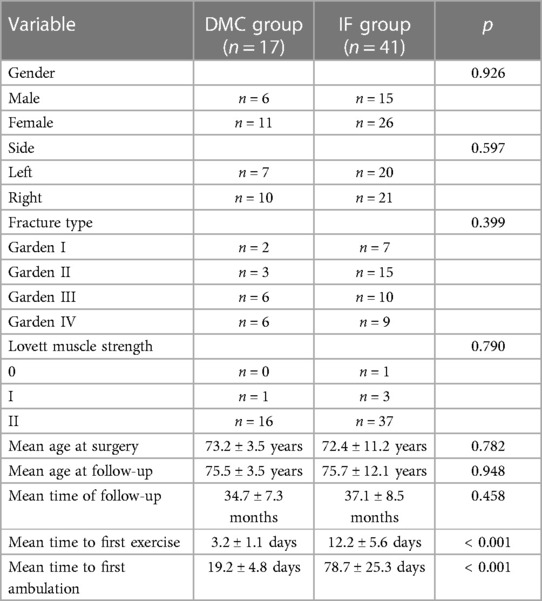
A total of 58 patients (21 men and 37 women; mean age: 75.2 ± 9.2 years) were included, then divided into two groups: dual-mobility cup total hip arthroplasty (DMC group, n = 17) and internal fixation (IF group, n = 41). Surgeons recommended that all patients avoid excessive hip flexion, internal rotation, and adduction and perform rehabilitation exercises as early as possible. Patients who could not ambulate were advised to do simple exercises on beds.
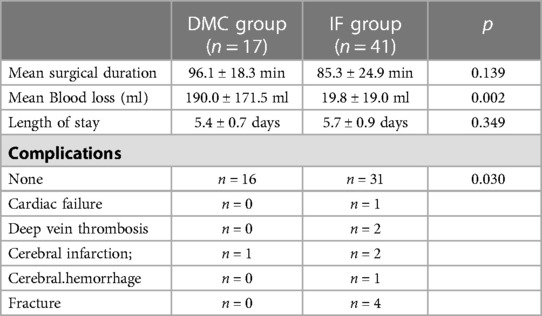
The mean follow-up time for all patients was 12.3 months (range: 12–14 months). The two groups did not differ in sex, age, injury side, fracture kind, or muscle strength (Table 1). The average surgery length was 96.1 ± 18.3 min in the DMC group and 85.3 ± 24.9 min in the IF group (p = 0.139). The mean blood loss was 190.0 ± 171.5 ml and 19.8 ± 19.0 ml in the DMC and IF groups (p = 0.002). After surgery, only one sign of complication was detected in the DMC group, while 10 patients in the IF group experienced complications (p = 0.030). Additionally, the IF group had a higher incidence of fractures (40%) and vascular-related disorders (60%) (Table 2). Patients in the DMC group began rehabilitation exercises and walking earlier than those in the IF group.
In the DMC group, patients had higher BI scores at admission, after surgery, and during follow-up than in the IF group (Figure 1). The BI scores significantly differed between preoperative, discharge and follow-up time in the DMC group (p1, p2 < 0.001). Meanwhile, preoperative and discharge scores significantly differed in the IF group (p1 = 0.001) but not discharge and follow-up (p2 = 0.187) (The p1 value represents the p-value of the BI score between preoperation and discharge, while the p2 value represents the p-value of the BI score between discharge and follow-up).
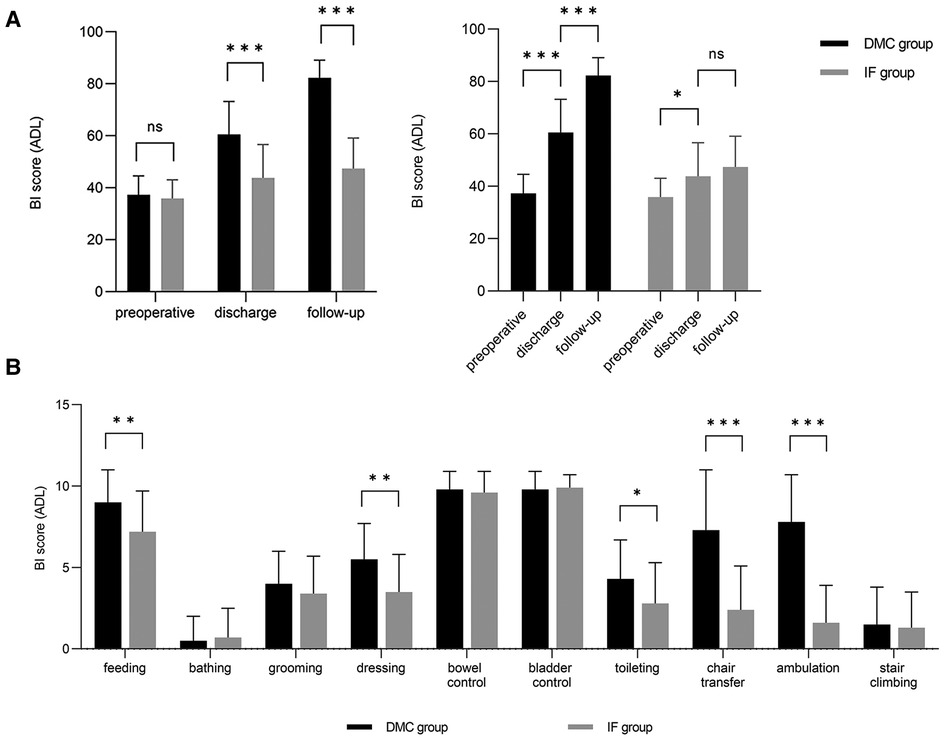
Figure 1. Scores for patient-related ADL assessed with the BI. The results of the DMC group cohort are shown in black and the IF group cohort are illustrated in grey. (A) Comparison and Change trend of ADL between DMC group and IF group at different time points. (B) Comparison between DMC group and IF group on subdimension scores of BI.
The mean FES-I score significantly differed between the two groups (DMC: 42.1 ± 5.3, IF: 47.3 ± 5.6; p = 0.002) (Figure 2A). In both groups, the mean score was > 3 for walking on a slippery surface (p = 0.013), going to a place with crowds, going up or down stairs, taking a bath or shower, and walking on an uneven surface. Besides, cleaning the house, getting dressed and undressed, and preparing simple meals were significantly different between groups (p < 0.001) (Figure 2B).
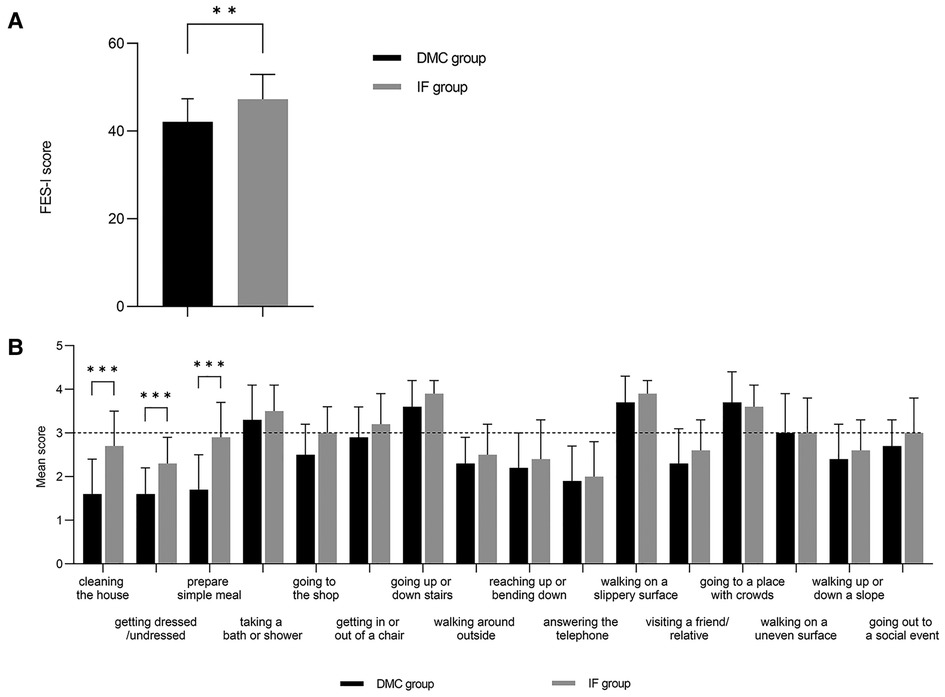
Figure 2. Scores for patient-related FOF assessed with the FES-I. The results of the DMC group cohort are shown in black and the IF group cohort are illustrated in grey. (A) Comparison of FES-I scores between DMC group and IF group. (B) Comparison between DMC group and IF group on subdimension scores of FES-I.
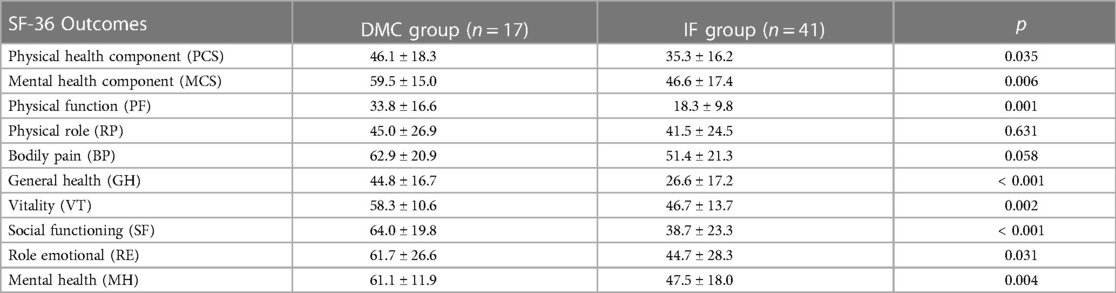
The mean SF-36 physical health component score (PCS) was 46.1 ± 18.3 for DMC and 35.3 ± 16.1 for IF. The SF-36 mental health component score (MCS) was 59.5 ± 15.0 in the DMC group and 46.6 ± 17.6 in the IF group (Figure 3A). Patients in the IF group had poorer scores on both SF-36 components (p = 0.035 and p = 0.006, respectively), with mental scores lower than physical ones. Additionally, patients in the IF group had lower SF-36 subdomain scores (Figure 3B, Table 3).
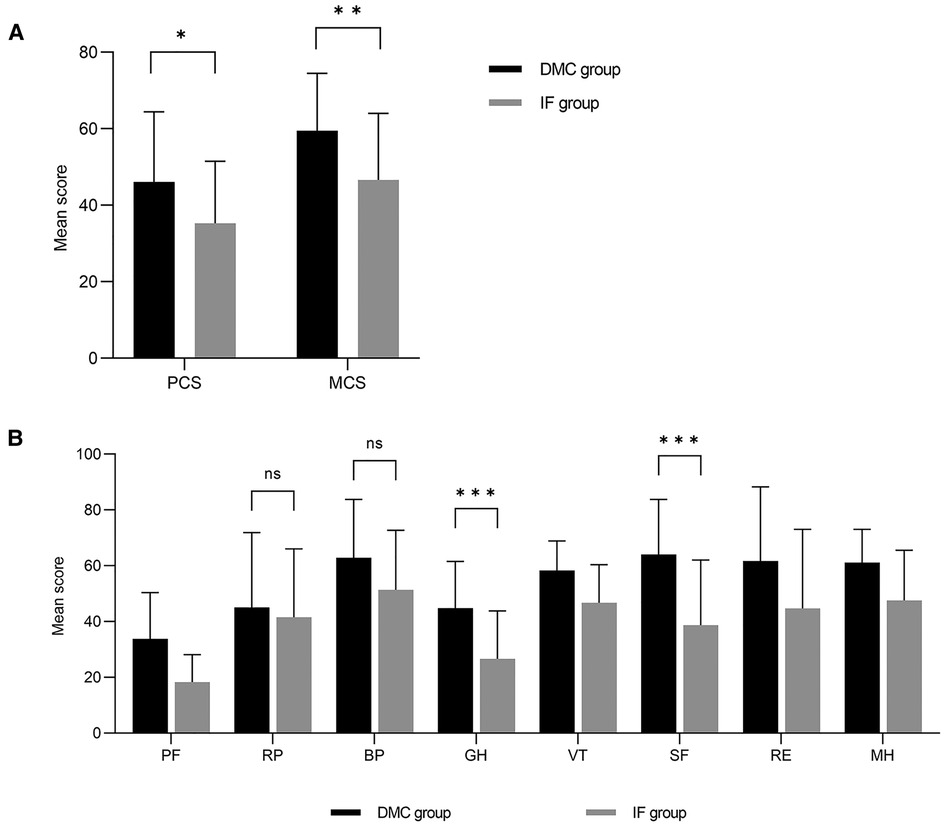
Figure 3. Scores for patient-related QOL assessed with the SF-36. The results of the DMC group cohort are shown in black and the IF group cohort are illustrated in grey. (A) Mean physical health component score (PCS) and mean mental health component score (MCS) assessed with the SF-36. (B) Comparison between DMC group and IF group on subdimension scores of SF-36.
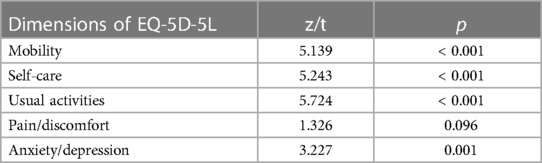
The mean EQ-5D-5L utility index was 0.737 ± 0.190 and 0.303 ± 0.227 for the DMC and IF groups (p = 0.035) (Figure 4A). At follow-up, The patients in the IF group had significantly worse walking, daily activities, and self-care capacity than those in the DMC group. A minimal difference was detected between the two groups for pain, and the DMC group had a much better psychological status than the IF group (Table 4, Figure 4B).
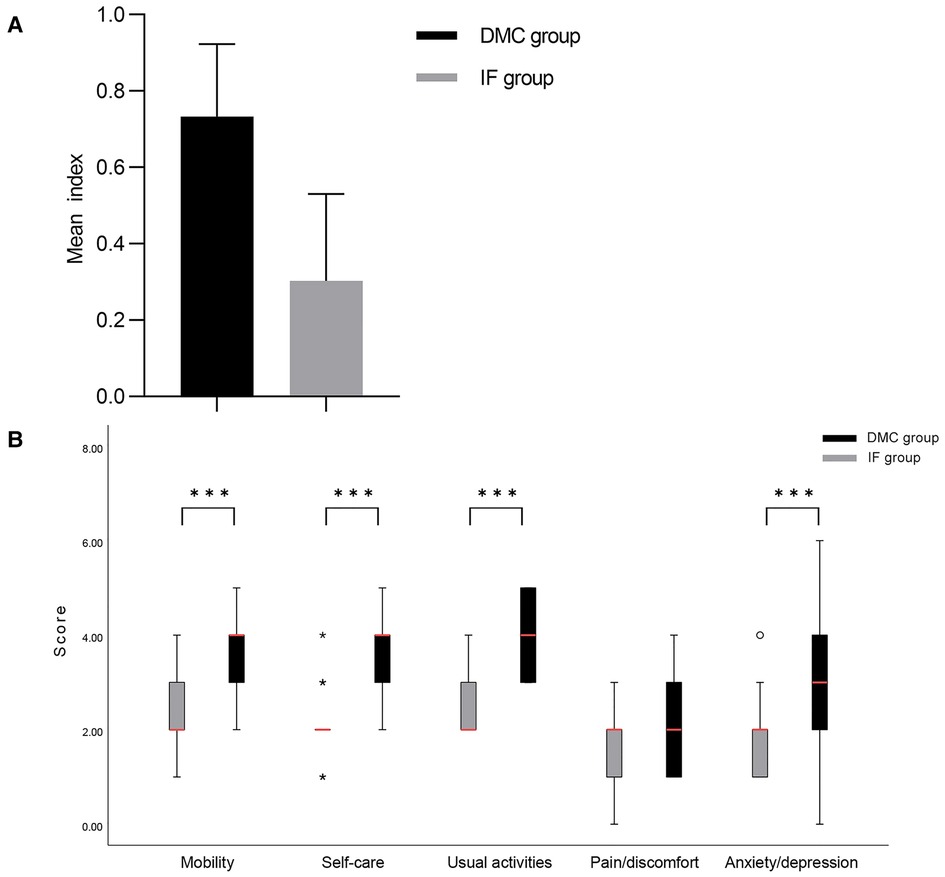
Figure 4. Scores for patient-related QOL assessed with the EQ-5D-5L. The results of the DMC group cohort are shown in black and the IF group cohort are illustrated in grey. (A) Comparison of EQ-5D-5L utility index between DMC group and IF group. (B) Comparison between DMC group and IF group on subdimension scores of EQ-5D-5L.
Furthermore, the QOL of patients in the DMC group was superior to the IF group at follow-up. The main differences were detected for the ability to perform daily activities, mental health, and function, while the pain did not differ.
Discussion
HA and IF might not be the optimal therapeutic options for femoral neck fracture patients with grades < 3/5 lower limb muscular strength due to stroke. These patients are susceptible to dislocation after HA surgery due to a lack of muscle power in the lower extremities, and doctors usually choose IF (26–29). However, there are also shortcomings to IF, namely that patients must remain in bed for an extended period after surgery, which greatly affects their mobility and QOL. The DMC-THA may be a better solution. Some studies have shown that patients with neuromuscular diseases who undergo DMC-THA can quickly engage in rehabilitation training like individuals who have undergone HA, thereby achieving a lower risk of dislocation and complications, as well as a better quality of life (12, 30). However, for patients with severe lower limb weakness, postoperative rehabilitation is more difficult, and it is still unknown whether DMC-THA can maintain its advantages over IF. We found that DMC-THA improved the QOL by enhancing patients' physical and mental conditions.
Physical sickness and mobility are connected with QOL in older individuals (31, 32). THA has a higher surgical risk for patients with a history of cerebrovascular illness, resulting in a high risk of complications (33–35). However, we found no significant difference between the two groups regarding complications. Additionally, the proportion of postoperative problems was much lower in the DMC group (5.9%) than in the IF group (24.4%), which might be connected with early rehabilitation. In the short period after surgery, patients in the DMC group performed much better than those in the IF group regarding the BI score for dressing, toileting, flat ground transfer, and other low-intensity easy activities (Figure 1.3), indicating that low-intensity postoperative activity helps to lower complication risk (9, 36). We also demonstrated that the benefit of DMC-THA in enhancing mobility increased after discharge. At follow-up, BI scores were higher in the DMC group than in the IF group. Besides, the amplitude of the BI scores increased more in the DMC group relative to discharge than in the IF group, indicating that DMC-THA was more successful in recovering mobility and that its effects lasted longer. Despite receiving rehabilitation training, the patients in the IF group missed the “golden” early postoperative period. Consequently, continuous, early, uncomplicated home activities are essential for enhancing the postoperative QOL of femoral neck fracture patients with severe neuromuscular illness (10, 37).
The mental condition is a component of QOL evaluations (31). Previous research has shown that anxiety after surgery can decrease the QOL, consistent with our findings (38). The patient's anxiety remained for extended periods after surgery, mostly due to constraints in home-based activities. The FOF can confirm this idea, a psychological trauma after falls that can provoke further falls, anxiety, sadness, diminished physical activity, decreased QOL, and alterations in psychosocial function, impacting the rehabilitation of patients (39, 40). The FES-I results revealed significant differences in the mental status of indoor activities between the two groups: DMC was superior to IF, confirming our hypothesis that DMC-THA improves the QOL of patients with severe neuromuscular illness by enhancing home activities. In the FES-I outdoor activity section, no significant differences were detected, indicating that, even with DMC-THA, patients were still unable to cope with the complicated outdoor environment. Nevertheless, this did not influence the patients' general mental status. Therefore, by completing the reconstruction of indoor mental function, the QOL of older patients with impaired lower limb function can be considerably enhanced (41).
The SF-36 and EQ-5D-5L results demonstrated that patients' physical and mental health affect their QOL. In the SF-36 scale, the PCS and MCS indicate physical and mental status, respectively. Kimiko et al. (42) examined 8,333 patients and found that the MCS was an independent predictor of old age, whereas the PCS was not. We also found that mental status might be the primary reason for disparities in QOL between patients treated with DMC or IF. In the SF-36, significant differences were observed in the GH and SF subscales but not for RP and BP (Figure 3.2). Sim et al. (43) showed that GH, associated with the patient's self-perception level, was an independent factor influencing rehabilitation outcomes after hip fracture surgery. Patients with low GH scores feel gloomy about their situation, negatively affecting their attitude toward rehabilitation. Busija (44) found that changes in GH might not be noticeable in patients with minimal variation in health conditions before and after treatment, a phenomenon known as the GH ceiling effect. Consequently, GH differences indicated that DMC-THA could significantly improve patients' health status and confidence compared to IF, increasing patients' motivation to engage in rehabilitation exercises. SF is the social-relational dimension connected with physical and mental health. A previous study has shown that psychotherapy might greatly improve SF. Another study suggested the relevance of social ties in rehabilitating hip fracture patients (45–47). Our results supported these notions and revealed that optimism from early functional recovery might directly influence social connections in the elderly with significant mobility impairment. Therefore, psychological interventions during bed rest might improve the postoperative QOL of patients receiving IF. However, this topic should be further explored.
The RP and BP are unique subscales in the SF-36 and did not differ between the two groups. Changes in RP can persist over six months to two years with a single intervention under normal conditions (48). However, the effects of alternative interventions or more time on RP progression remain unknown. We believe that the lack of significant differences in RP was related to the limited sensitivity of the RP program to individual changes in patients, consistent with Busija et al. (39). Pain (BP) is one of the most significant elements in the QOL of patients, and postoperative pain might increase anxiety risk. For example, patients with femoral neck fractures tend to experience prolonged discomfort after IF, whereas those receiving arthroplasty do not, comprehending one of the most crucial reasons for choosing arthroplasty (38). However, the pain-related SF-36 and EQ-5D-5L subscales did not differ between the two groups, indicating that postoperative anxiety was not associated with pain in this study. These results might be partially related to old age and not operation type, which relevant studies have not previously demonstrated since healthy people have a decline in bone mass and are more susceptible to systemic discomfort as they age.
The EQ-5D-5L results demonstrated that the mean utility index of both groups did not meet the mean standard for the elderly in China (49), indicating that neither DMC-THA nor IF could fully restore the QOL, which was associated with the history of cerebrovascular disease. Nevertheless, the DMC group had a higher QOL than the IF group due to a greater recovery of daily activities and mental status, supported by additional scales. We found that the QOL might be associated with socioeconomic position, education, and the cost of in-home care during follow-up, influencing utility values (49).
However, our current study also has some limitations: (1) This was a retrospective analysis with a restricted number of eligible patients and various surgical procedures. In the future, high-quality research with larger samples and longer follow-up periods is required to corroborate our findings. (2) Although previous studies have established that the scales used here are equally powered, we cannot rule out variances in the results due to the telephone follow-up data collection for some patients. (3) Due to the history of cerebrovascular disease, we did not fully analyze the patient's postoperative problems in other aspects, which could have affected the QOL results. Thus, future studies should evaluate the impacts of other diseases on the QOL of these individuals.
Conclusion
In summary, DMC-THA significantly improved postoperative QOL compared to IF in elderly stroke patients with severe neuromuscular dysfunction of the lower extremity. DMC-THA improved both physical and mental well-being. Enhancing patients' early, rudimentary motor performance improved physical and mental outcomes. Moreover, patients with complex illnesses tend to have low expectations for surgery. Early daily physiological function recovery increases their excitement for postoperative rehabilitation and enhances the treatment's efficacy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
This work was supported by Natural Science Foundation of Guangdong Province (grant number: 2018A030313643). We thank XL for writing assistance and language help; BC and ZH for clinical data collating; and YH for experimental design. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chavda V, Madhwani K. Coding and non-coding nucleotides’: the future of stroke gene therapeutics. Genomics. (2021) 113(3):1291–307. doi: 10.1016/j.ygeno.2021.03.003
2. Cho KH, Pyo S, Shin GS, Hong SD, Lee SH, Lee D, et al. A novel one arm motorized walker for hemiplegic stroke survivors: a feasibility study. Biomed Eng Online. (2018) 17(1):14. doi: 10.1186/s12938-018-0446-z
3. Yang FZ, Jehu D, Ouyang H, Lam F, Pang M. The impact of stroke on bone properties and muscle-bone relationship: a systematic review and meta-analysis. Osteoporos Int. (2020) 31(2):211–24. doi: 10.1007/s00198-019-05175-4
4. Potin P, Degboé Y, Couture G, Marque P, De Boissezon X, Laroche M. Loss of bone mineral density in hemiplegic patients after stroke: prospective single-center study. Rev Neurol (Paris). (2022) 178(8):808–11. doi: 10.1016/j.neurol.2022.01.012
5. Wang Y, Wang Z, Tian S, Tan Z, Zhu Y, Chen W, et al. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in patients with neuromuscular diseases: a minimum of 2 years’ follow-up study. J Orthop Surg Res. (2021) 16(1):418. doi: 10.1186/s13018-021-02572-6
6. Konan S, Duncan CP. Total hip arthroplasty in patients with neuromuscular imbalance. Bone Joint J. (2018) 100-B(1 Supple A):17–21. doi: 10.1302/0301-620X.100B1.BJJ-2017-0571.R1
7. Gausden EB, Parhar HS, Popper JE, Sculco PK, Rush B. Risk factors for early dislocation following primary elective total hip arthroplasty. J Arthroplasty. (2018) 33(5):1567–1571.e2. doi: 10.1016/j.arth.2017.12.034
8. Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand. (2000) 71(6):597–602. doi: 10.1080/000164700317362235
9. Zidén L, Kreuter M, Frändin K. Long-term effects of home rehabilitation after hip fracture—1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disabil Rehabil. (2010) 32(1):18–32. doi: 10.3109/09638280902980910
10. Liu HY, Yang CT, Cheng HS, Wu CC, Chen CY, Shyu YL. Family caregivers’ mental health is associated with postoperative recovery of elderly patients with hip fracture: a sample in Taiwan. J Psychosom Res. (2015) 78(5):452–8. doi: 10.1016/j.jpsychores.2015.02.002
11. Young JR, O'Connor CM, Anoushiravani AA, DiCaprio MR. The use of dual mobility implants in patients who are at high risk for dislocation after primary total hip arthroplasty. JBJS Rev. (2020) 8(8):e20.00028. doi: 10.2106/JBJS.RVW.20.00028
12. Almeida RFC. Dual mobility cup in total hip arthroplasty. The experiense of the university hospital. Rev Bras Ortop. (2020) 55(6):708–14. doi: 10.1055/s-0040-1702951
13. Lamo-Espinosa JM, Gómez-Álvarez J, Gatica J, Suárez Á, Moreno V, Díaz de Rada P, et al. Cemented dual mobility cup for primary total hip arthroplasty in elder patients with high-risk instability. Geriatrics (Basel, Switzerland). (2021) 6(1):23. doi: 10.3390/geriatrics6010023
14. Ryu HG, Roh YJ, Oh KJ, Hwang JH, Kim Y, Cho HW, et al. Dual mobility articulation total hip arthroplasty for displaced neck fracture in elderly with neuromuscular disorder. Injury. (2021) 52(6):1480–6. doi: 10.1016/j.injury.2021.01.005
15. Huber J, Kaczmarek K, Leszczyńska K, Daroszewski P. Post-Stroke treatment with neuromuscular functional electrostimulation of antagonistic muscles and kinesiotherapy evaluated with electromyography and clinical studies in a two-month follow-up. Int J Environ Res Public Health. (2022) 19(2):964. doi: 10.3390/ijerph19020964
16. Walter N, Rupp M, Hierl K, Koch M, Kerschbaum M, Worlicek M, et al. Long-Term patient-related quality of life after knee periprosthetic joint infection. J Clin Med. (2021) 10(5):907. doi: 10.3390/jcm10050907
17. Barclay R, Miller PA, Pooyania S, Stratford P. Development of a telephone interview version of the chedoke-McMaster stroke assessment activity inventory. Physiotherapy Canada. (2016) 68(3):216–22. doi: 10.3138/ptc.2015-44
18. Wu Z, Xu J, Yue C, Li Y, Liang Y. Collaborative care model based telerehabilitation exercise training program for acute stroke patients in China: a randomized controlled trial. J Stroke Cerebrovasc Dis. (2020) 29(12):105328. doi: 10.1016/j.jstrokecerebrovasdis.2020.105328
19. Ye CY, Liu A, Xu MY, Nonso NS, He RX. Arthroplasty versus internal fixation for displaced intracapsular femoral neck fracture in the elderly: systematic review and meta-analysis of short- and long-term effectiveness. Chin Med J. (2016) 129(21):2630–8. doi: 10.4103/0366-6999.192788
20. Schmid AA, Van Puymbroeck M, Knies K, Spangler-Morris C, Watts K, Damush T, et al. Fear of falling among people who have sustained a stroke: a 6-month longitudinal pilot study. Am J Occup Ther. (2011) 65(2):125–32. doi: 10.5014/ajot.2011.000737
21. Kwan MM, Tsang WW, Close JC, Lord SR. Development and validation of a Chinese version of the falls efficacy scale international. Arch Gerontol Geriatr. (2013) 56(1):169–74. doi: 10.1016/j.archger.2012.10.007
22. Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging. (2018) 13:143–50. doi: 10.2147/CIA.S150067
23. Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J. Quality of life after hip fracture in the elderly: a systematic literature review. Injury. (2016) 47(7):1369–82. doi: 10.1016/j.injury.2016.04.018
24. Tidermark J, Bergström G, Svensson O, Törnkvist H, Ponzer S. Responsiveness of the EuroQol (EQ 5-D) and the SF-36 in elderly patients with displaced femoral neck fractures. Qual Life Res. (2003) 12(8):1069–79. doi: 10.1023/a:1026193812514
25. Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5l value set for China. Value Health. (2017) 20(4):662–9. doi: 10.1016/j.jval.2016.11.016
26. Lee HY, Park JH, Lee H, Kim TW, Yoo SD. Does hip bone density differ between paretic and non-paretic sides in hemiplegic stroke patients? And its relationship with physical impairment. J Bone Metab. (2020) 27(4):237–46. doi: 10.11005/jbm.2020.27.4.237
27. Wang Y, Deng X, Wang Z, Zhu Y, Chen W, Zhang Y. Total hip arthroplasty or hemiarthroplasty for femoral neck fractures in elderly patients with neuromuscular imbalance. Aging Clin Exp Res. (2021) 34:2825–33. doi: 10.1007/s40520-021-01976-y Advance online publication.34506006
28. Bhandari M, Devereaux PJ, Tornetta P III, Swiontkowski MF, Berry DJ, Haidukewych G, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone and Joint Surg. (2005) 87(9):2122–30. doi: 10.2106/JBJS.E.00535
29. Barışhan FC, Akesen B, Atıcı T, Durak K, Bilgen MS. Comparison of hemiarthroplasty and total hip arthroplasty in elderly patients with displaced femoral neck fractures. J Int Med Res. (2018) 46(7):2717–30. doi: 10.1177/0300060518770354
30. Yang J, Bryan AJ, Drabchuk R, Tetreault MW, Calkins TE, Della Valle CJ. Use of a monoblock dual-mobility acetabular component in primary total hip arthroplasty in patients at high risk of dislocation. Hip Int. (2022) 32(5):648–55. doi: 10.1177/1120700020988469
31. Grassi L, Caruso R, Da Ronch C, Härter M, Schulz H, Volkert J, et al. Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: results from the MentDis_ICF65 + study. Health Qual Life Outcomes. (2020) 18(1):61. doi: 10.1186/s12955-020-01310-6
32. Lin CC, Li CI, Chang CK, Liu CS, Lin CH, Meng NH, et al. Reduced health-related quality of life in elders with frailty: a cross-sectional study of community-dwelling elders in Taiwan. PloS one. (2011) 6(7):e21841. doi: 10.1371/journal.pone.0021841
33. Wahlsten LR, Zareini B, Smedegaard L, Gislason GH, Palm H, Brorson S. A medical history of arterial thrombosis is a strong predictor of post-operative myocardial infarction and stroke in patients with hip fractures-a nationwide cohort study. Age Ageing. (2021) 50(4):1252–60. doi: 10.1093/ageing/afaa279
34. Haynes MS, Alder KD, Bellamkonda K, Kuzomunhu L, Grauer JN. Incidence, predictors, and timing of post-operative stroke following elective total hip arthroplasty and total knee arthroplasty. PloS one. (2020) 15(9):e0239239. doi: 10.1371/journal.pone.0239239
35. Yao DH, Keswani A, Shah CK, Sher A, Koenig KM, Moucha CS. Home discharge after primary elective total joint arthroplasty: postdischarge complication timing and risk factor analysis. J Arthroplasty. (2017) 32(2):375–80. doi: 10.1016/j.arth.2016.08.004
36. Pan XL. Efficacy of early rehabilitation therapy on movement ability of hemiplegic lower extremity in patients with acute cerebrovascular accident. Medicine (Baltimore). (2018) 97(2):e9544. doi: 10.1097/MD.0000000000009544
37. Shyu YI, Chen MC, Liang J, Tseng MY. Trends in health outcomes for family caregivers of hip-fractured elders during the first 12 months after discharge. J Adv Nurs. (2012) 68(3):658–66. doi: 10.1111/j.1365-2648.2011.05778.x
38. Cristancho P, Lenze EJ, Avidan MS, Rawson KS. Trajectories of depressive symptoms after hip fracture. Psychol Med. (2016) 46(7):1413–25. doi: 10.1017/S0033291715002974
39. Kovács É, Rozs F, Petridisz A, Erdős R, Majercsik E. Cross-cultural validation of the falls efficacy scale-international to assess concerns about falls among Hungarian community-living older people. Disabil Rehabil. (2018) 40(25):3070–5. doi: 10.1080/09638288.2017.1366555
40. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the falls efficacy scale-international (FES-I). Age Ageing. (2005) 34(6):614–9. doi: 10.1093/ageing/afi196
41. Campenfeldt P, Ekström W, Al-Ani AN, Weibust E, Greve K, Hedström M. Health related quality of life and mortality 10 years after a femoral neck fracture in patients younger than 70 years. Injury. (2020) 51(10):2283–8. doi: 10.1016/j.injury.2020.06.029
42. Tomioka K, Shima M, Saeki K. Mental component of health-related quality of life is an independent predictor of incident functional disability among community-dwelling older people: a prospective cohort study. Qual Life Res. (2021) 30(7):1853–62. doi: 10.1007/s11136-021-02780-x
43. Sim C, Sultana R, Tay K, Howe CY, Howe TS, Koh J. SF-36 physical function and general health domains are independent predictors of acute hospital length of stay after hip fracture surgery. Musculoskelet Surg. (2022) 32:s303–4. doi: 10.1007/s12306-022-00753-y Advance online publication.
44. Busija L, Osborne RH, Nilsdotter A, Buchbinder R, Roos EM. Magnitude and meaningfulness of change in SF-36 scores in four types of orthopedic surgery. Health Qual Life Outcomes. (2008) 6:55. doi: 10.1186/1477-7525-6-55
45. Tai YH, Wu HL, Lin SP, Tsou MY, Chang KY. An investigation of the effect of patient-controlled analgesia on long-term quality of life after major surgery: a prospective cohort study. J Chin Med Association: JCMA. (2020) 83(2):194–201. doi: 10.1097/JCMA.0000000000000241
46. Kalter J, Verdonck-de Leeuw IM, Sweegers MG, Aaronson NK, Jacobsen PB, Newton RU, et al. Effects and moderators of psychosocial interventions on quality of life, and emotional and social function in patients with cancer: an individual patient data meta-analysis of 22 RCTs. Psychooncology. (2018) 27(4):1150–61. doi: 10.1002/pon.4648
47. Swayambunathan J, Dasgupta A, Bhattacharyya T. The pronounced impact of hip fractures on psychosocial well-being. J Am Acad Orthop Surg. (2021) 29(1):e22–30. doi: 10.5435/JAAOS-D-19-00530
48. Tarakji BA, Wynkoop AT, Srivastava AK, O'Connor EG, Atkinson TS. Improvement in depression and physical health following total joint arthroplasty. J Arthroplasty. (2018) 33(8):2423–7. doi: 10.1016/j.arth.2018.03.051
Keywords: dual-mobility cup total hip arthroplasty, internal fixation, quality of life, stroke, severe neuromuscular dysfunction
Citation: Liang C, Chen B, Hu Z, Li X and Huang Y (2023) Dual-mobility cup total hip arthroplasty improves the quality of life compared to internal fixation in femoral neck fractures patients with severe neuromuscular disease in the lower extremity after stroke: a retrospective study. Front. Surg. 10:1120273. doi: 10.3389/fsurg.2023.1120273
Received: 9 December 2022; Accepted: 30 March 2023;
Published: 17 April 2023.
Edited by:
Jaimo Ahn, Michigan Medicine, University of Michigan, United StatesReviewed by:
Biagio Zampogna, Campus Bio-Medico University Hospital, ItalyYuanqiao Wu, Boston University, United States
© 2023 Liang, Chen, Hu, Li and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongming Huang aHVhbmcxNjNodWFuZ0AxNjMuY29t
†These authors share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Chaolun Liang
Chaolun Liang Bojian Chen2,†
Bojian Chen2,† Xing Li
Xing Li