
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 18 April 2023
Sec. Otorhinolaryngology - Head and Neck Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1118083
Background: The EBSLN is vulnerable to damage during thyroidectomy, results in voice related complications, negatively affect patient quality of life, routine identification of the EBSLN prior to surgical manipulation is necessary for a complication-free thyroidectomy. We aimed to validate a video-assisted procedure for identifying and preserving the external branch of the superior laryngeal nerve (EBSLN) during thyroidectomy and analyze the EBSLN Cernea classification and the localization of the nerve entry point (NEP) from the insertion of the sternothyroid muscle.
Methods: A prospective descriptive study was performed; 134 patients, who scheduled for lobectomy with an intraglandular tumor max diameter ≤ 4 cm and without extrathyroidal extension, were randomly divided into the video-assisted surgery (VAS) and conventional open surgery (COS) groups. We used the video-assisted surgical procedure for visually identifying the EBSLN directly, and compared the differences in the visual identification rate and total identification rate of the two groups. We also measured the localization of the NEP using the insertion of the sternothyroid muscle as a reference.
Results: There was no statistically significant difference in clinical characteristics between the two groups. The visual identification rate and total identification rate were significantly higher in the VAS group than the COS group (91.04% vs. 77.61%, 100% vs. 89.6%). The EBSLN injury rate was 0 in both groups. The mean vertical distance (VD) of the NEP from the sternal thyroid insertion was 1.18 mm (SD 1.12 mm, range, 0–5 mm), with approximately 88.97% of the results occurring within the 0–2 mm range. The mean horizontal distance (HD) was 9.33 mm (SD 5.03 mm, range, 0–30 mm), with over 92.13% of the results occurring within the 5–15 mm range.
Conclusion: Both the visual and total identification rates of the EBSLN were significantly higher in the VAS group. This method provided a good visual exposure rate of the EBSLN, aiding in identifying and protecting the EBSLN during thyroidectomy.
section-at-acceptanceOtorhinolaryngology - Head and Neck SurgeryThe external branch of the superior laryngeal nerve (EBSLN) is an important nerve tissue in thyroid surgery (1, 2), similar to the recurrent laryngeal nerve (RLN) and the parathyroid gland, and is responsible for motor innervation of the cricothyroid muscle (CTM), which acts to elongate and thin the true vocal folds during phonation, thereby elevating the pitch of the voice. Dysfunction of the CTM secondary to EBSLN injury results in hoarseness, a weak voice, vocal fatigue, or reduced vocal frequency; these consequences may be permanent and negatively affect patient quality of life, especially for professional voice users (3, 4).
Considering its high injury rate (up to 58%) and varying exposure rate (5, 6), routine identification of the EBSLN prior to surgical manipulation is necessary for a complication-free thyroidectomy (7, 8). The EBSLN descends posterior to the sternothyroid muscle towards the cricothyroid muscles, along and cross the STA. As described by Cernea classification, types 1, 2A and 2B means more than 1 cm above the upper pole of thyroid, within 1 cm of the upper pole, or below the upper pole respectively. While there are techniques to identify the RLN during thyroid surgery, there is no clear consensus or standard technique for the identification of the EBSLN. Due to its close anatomical relationship with the superior thyroid artery, its fine structure, and its highly variable anatomy (9), its susceptibility to injury and the difficulty in exposing the EBSLN during thyroidectomy are well recognized (10). Inadequate exposure of the upper polar region is the major factor affecting EBSLN identification and iatrogenic injury, which is mainly caused by occlusion of the sternalthyroid muscle, which is also assessed as a landmark for the nerve entry point (NEP) of the EBSLN on the inferior constrictor muscle (11, 12).
The aim of the present study was to validate a video-assisted method for visually identifying and preserving the EBSLN accurately and feasibly by expanding the scope and eliminating the dead angle of observation.
This was a descriptive study of a prospective case series of conventional open thyroidectomy performed from February 2021 to July 2022 in our department.
The inclusion criteria included the following: (1) adult patients who were scheduled for lobectomy, according to the standard of the ATA Thyroid Guidelines (13); (2) patients with an intraglandular tumor max diameter ≤ 4 cm; and (3) patients without extrathyroidal extension. The exclusion criteria included (1) previous thyroid or neck surgery, (2) ipsilateral neck dissection, (3) neck irradiation, (4) pregnant woman, and (5) preoperative vocal fold palsy.
All surgeries were performed by the same surgical team. This study was approved by the ethics committee of our hospital, and written informed consent was obtained from all patients.
All patients underwent open thyroid lobectomy under general anesthesia by the same surgical team. To ensure the full return of muscular activity, a minimal single dose of a nondepolarizing muscle relaxant (rocuronium, approximately 0.5 mg/kg) was used, as previous described (14).
In the video-assisted surgery (VAS) group, a transverse low-collar skin incision was made, platysmal flaps were dissociated and raised, and the thyroid was exposed with a longitudinal incision in the linea alba cervicalis. The sternohyoid and sternothyroid muscles were retracted upward and laterally, while the superior pole of the thyroid lobe was retracted inferolaterally, and an avascular window was opened in the sternothyroid–laryngeal triangle, which constituted the sternothyroid muscle, the inferior constrictor muscle of the pharynx and the cricothyroid muscle, and the thyroid.
Through video assistance, combining blunt separation and meticulous dissection, we attempted to visually identify the EBSLN in this area (Figure 1) and confirmed it with a nerve stimulator. Contraction of the CTM under electrostimulation of 1 mA represents the functional integrity of the EBSLN during operation (14).
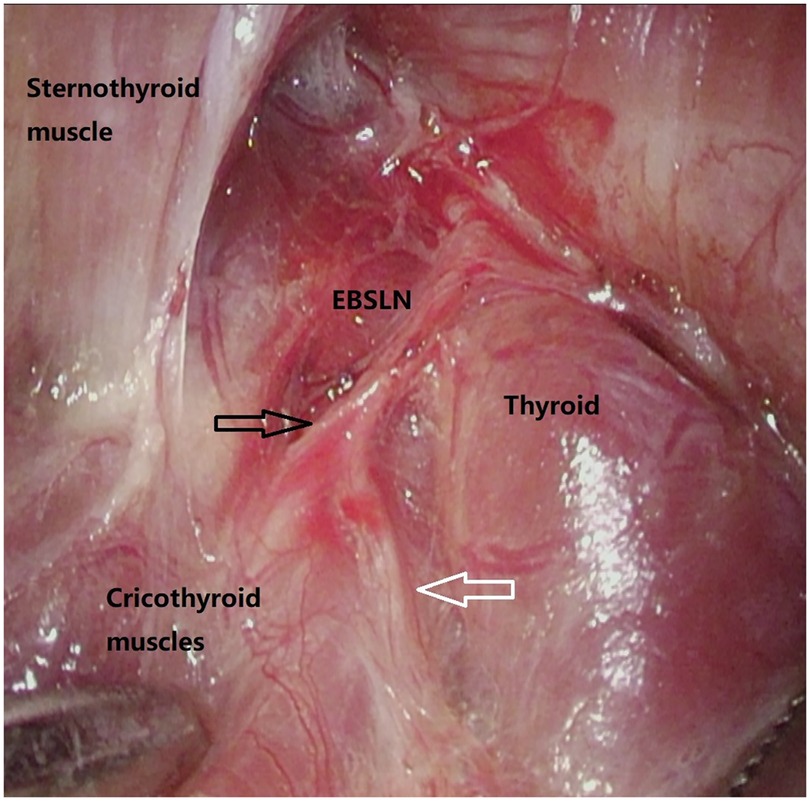
Figure 1. Visually expose of EBSLN by video-assisted view angle. Black arrow: EBSLN toward cricothyroid muscles, white arrow: communicating branch between EBSLN and RLN.
After identification, the exposed nerve was followed downstream until it entered the inferior constrictor or cricothyroid muscle at the nerve entry point (NEP) and traced upstream until it crossed over the STA. If the nerve was not clearly visualized, then the nerve tract on the constrictor muscle was indirectly stimulated to create and observe the physiological response of the CTM. If the nerve was still not identified, the search for the nerve was discontinued to avoid excessive damage caused by excessive dissociation, and the superior thyroid vessels were adequately dissected for safe ligation and division.
In the conventional open surgery (COS) group, the main step was similar but involved only the use of the naked eye without the assistance of a laparoscope.
We studied the following aspects: (1) the rate of EBSLN identification wherein the total identification rate included both the visual identification rate of the EBSLN confirmed by intraoperative nerve monitoring (IONM) and the functional identification rate of nonvisualized EBSLNs confirmed by IONM; (2) the rate of EBSLN injury for which we evaluated EBSLN injury by (1) anatomical or functional integrity damage during the operation, (2). positive findings on postoperative laryngoscopy, including posterior glottis rotation toward the affected side, inferior vocal fold positioning on the paralyzed side, and epiglottic petiole deviation toward the affected side (15, 16), and (3) voice assessment, including maximum phonation time (MPT, sec), voice level (VL, dB), and fundamental frequency (Fo, Hz), which were measured as previously described (17), and the quality of voice, which was measured using the VoiSS questionnaire focused on patient perspectives (18); (3) the percentage distribution of the Cernea classification, which describes the anatomic variations in the EBSLN in relation to the intersection of the superior thyroid artery and superior thyroid pole (19); (4) the localization of the NEP, which is defined by two distances (11), namely, the vertical distance (VD), which is the perpendicular distance from the NEP to the sternothyroid insertion onto the oblique line of the thyroid cartilage, and the horizontal distance (HD), which is the distance from the NEP to the anterior border of the sternothyroid muscle; and (5) the operative time from the incision of the skin to dissection of the upper pole of the thyroid area.
Data are expressed as the mean ± standard deviation (SD) and were analyzed with SPSS 22.0 statistical software (SPSS Inc., Chicago, IL, USA). The statistical significance of categorical variables was evaluated by the chi-square (χ2) test or Fisher's exact test. P < 0.05 was considered to indicate significance.
A total of 134 patients qualified for inclusion in the study. All operations were completed smoothly. A total of 67 patients were enrolled in the VAS group, and their mean age was 45.37 ± 9.792 years (range, 20–68). A total of 67 patients were enrolled in the COS group, and their mean age was 43.96 ± 9.516 years (range, 24–62). The general distribution of the patients is shown in Table 1.
We first tried to visually identify the EBSLN during upper pole dissection. Visual identification rates were 91.04% (61 in 67 cases) and 77.61% (52 in 67 cases) in the VAS group and the COS group, respectively (P < 0.05). Electrophysiological stimulation of all visually identified nerve branches generated CTM contractions that showed functional integrity. In addition to visual identification, nonvisualized nerve branches were functionally discovered in 6 and 8 nerves by IONM in the VAS group and the COS group, respectively. In total, in the VAS group, 67 (100%) EBSLNs were identified, and in the COS group, 60 (89.6%) EBSLNs were identified (P < 0.05) (Table 2).
The injury rate of the EBSLN was 0 in both groups, with no significant differences. All EBSLNs identified during the operation were confirmed to have anatomical and functional integrity before the end of the operation. All patients underwent postoperative stroboscopic laryngoscopy, and we did not find any signs of EBSLN injury. On functional voice assessment, a 10% or higher decrease in phonation parameters (MPT, VL, and Fo) was not found in any patients in the two groups. The postoperative VoiSS questionnaire scores of all patients were within the normal range, and there was no significant difference between the two groups (Table 3).
In the VAS group, all 67 EBSLNs were identified, among these, 9 (13.43%) were Cernea type 1, 26 (38.81%) were type 2A, and 32 (47.76%) were type 2B. while in the VAS group, 60 EBSLNs were identified, 5 (8.33%) were Cernea type 1, 24 (40.0%) were type 2A, and 31 (51.67%) were type 2B. There is no statistical difference in the distribution of Cernea type between the two groups (Table 4).
Among the total of 127 EBSLNs identified in the two groups, 14 (11.02%) were Cernea type 1, 50 (39.37%) were type 2A, and 63 (49.61%) were type 2B.
We also analyzed the localization of the NEP based on the distances from the sternothyroid insertion. The mean vertical distance (VD) was 1.18 mm (SD 1.12 mm, range, 0–5 mm), with approximately 88.97% occurring within the 0–2 mm range, and the mean horizontal distance (HD) was 9.33 mm (SD 5.03 mm, range, 0–30 mm), with over 92.13% occurring within the 5–15 mm range.
The average time from skin incision to the dissection of the upper pole was 15.90 ± 3.802 min and 16.36 ± 4.191 min in the VAS group and the COS group, respectively, and there were no significant differences between the two groups.
The fine size, variable course and label of “the neglected nerve” make the EBSLN at potential risk during thyroidectomy (20, 21). Injury to the EBSLN can occur by transection, traction, ligation, thermal damage, and disrupted blood supply (22), and identification though proper and sufficient exposure is important to avoid this (8). The laryngeal head of the sternothyroid muscle is assessed as a landmark for the course of the EBSLN on the inferior constrictor, but it also obstructs the surgeon's observation of the superior pole of the thyroid region and affects the exposure of the EBSLN (11, 23).
Some surgeons used to cut off part of the laryngeal head of the sternothyroid muscle to better expose the EBSLN (24). This process not only increases muscle damage but also increases the chance of unintentional EBSLN injury. To avoid this, a strap intermuscular approach has been described for exposing and protecting the EBSLN (25). Considering that the main factor affecting the exposure of the upper polar region is the angle of view, not the sternal thyroid muscle itself, we tried to change the visual angle and afford sufficient visualization of the superior thyroid region by means of endoscopic assistance, without sacrificing the integrity of the sternothyroid muscle or an extra expanded separation area.
Compared to COS, the new video-assisted method does not require amputation of the sternothyroid muscle, provides a better visual field to expose the EBSLN, and makes it more easily protected intraoperatively. Additionally, the new video-assisted method does not increase the time from cutting the skin to exposing the upper thyroid region. This method not only uses the magnifying effect of the endoscope to expand the observation field but also reduces surgical injury through precise and directional operation.
Currently, IONM has gained extensive acceptance as an adjunct to the gold standard of EBSLN identification (26). For the nerves that cannot be identified accurately and those that run inside the pharyngeal constrictor muscle (Friedman's classification type 3 (27), IONM plays an important role in EBSLN protection (2, 28). Moreover, visual exposure and protection can confirm the anatomical integrity of nerves, but functional integrity cannot be confirmed. Before the end of the operation, while anatomical integrity is confirmed, neural monitoring is required to exclude the elimination of thermal damage and strain injury and verify neural function. Electrostimulation causes simultaneous contraction of the cricothyroid muscle in both the straight and oblique abdomen as the standard of neurological integrity (3, 14, 29).
Nevertheless, IONM does not completely eliminate the risk of nerve injury caused by unintentional injuries (30, 31), and the surgeon's experience and full understanding of anatomy and possible variations are more important than the aid of high-tech instruments during thyroid surgery (32). Therefore, our strategy mainly depends on visual confirmation of the nerve during surgery, and electrical nerve stimulation is used for confirmation after exposure and functional examination before the end of the surgery.
In the present study, we achieved a 91% EBSLN exposure rate (61 in 67 nerves) based on visual exposure and confirmed that nerve function was good through the contraction of the cricothyroid muscle. This rate is satisfactory compared with those reported in previous studies with IONM (33–35).
We used IONM to further increase the exposure rate by 9% (6 in 67 nerves), and the total exposure rate of the EBSLN reached 100%. This result revealed that the EBSLN could be visually identified in the majority of cases, with or without IONM. For hospitals without neural monitoring equipment or the economic ability to purchase neural monitoring equipment, medical insurance limits expenses, and this method is conducive to the identification and isolation of the nerve, thereby minimizing iatrogenic injury and postoperative complications.
In the present study, we also calculated the distribution of Cernea groupings of the EBSLNs. Among the total of 127 EBSLNs identified in the two groups, we found a high prevalence of Cernea type 2 nerves (88.98%), with 49.61% being type 2B. These data are similar to those reported in previous studies (11, 36, 37). Moreover, notably, traction of the upper pole of the thyroid may change the position and classification of the EBSLN, increasing the proportion of type 2b. Due to the close proximity of the EBSLN to the STA, the high proportion of type 2 EBSLNs also indicates that it is meaningful to identify the EBSLN by routine exposure to reduce the risk of injury.
It was our experience that the STA was unsuitable as a landmark to find the EBSLN intraoperatively, and there were many variations both in the EBSLN and STA (38). Different from cadaveric anatomy, the position of the sternal thyroid muscle and superior posterior thyroid EBSLN and their relationship with the superior artery change during surgery, especially when the thyroid lobe is pulled. This also explains why the intraoperative exposure rate of the EBSLN is generally lower than that of cadaveric studies (39). Moreover, the possible small branches of the superior thyroid artery may bleed and affect the exposure.
According to a previous study (11), we used the insertion of the sternothyroid muscle as a reliable landmark to localize the NEP of the EBSLN. The NEP consistently lies close to the sternothyroid muscle insertion onto the oblique line and does not vary with the direction of pull on the lobe; there is not a bothersome ligament or vessel nearby. We look for the EBSLN in this area visually with the video assistance of a wide field of vision and magnification. In our study, the NEP was approximately 1.18 mm from the sternothyroid insertion and 5–15 mm from the anterior border of the muscle.
After finding the NEP, the nerve was readily traced superiorly to the intersection with the STA. With identification of the EBSLN, the superior thyroid vessels were adequately dissected for safe ligation and division. Our strategy greatly improved the exposure and ease of dissection of the EBSLN, thus reducing the chance of postoperative voice problems. For experienced surgeons with an understanding of local anatomy, this process can be accurate and fast.
The present study has some limitations. First, the sample size of a single institution was not sufficient. For the purpose of controlling postoperative sound function and operation time, we only included patients with unilateral lobectomy, and a large-scale multicenter study with a wider range of patients is needed to further compare the clinical effects. Second, we performed intraoperative visualization, IONM, voice assessments and laryngoscope evaluation to analyze the rates of exposure and injury but did not conduct CTM electroneuromyography (EMG), which is the most accurate tool for diagnosing abnormal EBSLN conductivity. For IONM, we only used cricothyroid muscle contraction to evaluate neural integrity. Due to the limitation of medical insurance costs, we cannot use the intratracheal electrode and cricothyroid electrode to quantitatively measure the EMG signal, which makes us unable to predict postoperative nerve function according to the change in signal strength. Third, the present study did not involve patients with large goiters, short necks or obesity. We also excluded patients with ETE of the upper pole; thus, the 100% exposure rate in the VAS group and 0% injury rate in this study may not accurately reflect the real status of clinical practice. We will conduct further research on these topics in follow-up studies.
In this study, we used a video-assisted method to fully expose the upper pole of the thyroid. Without increasing muscle injury or increasing the extent of surgery, a good visual exposure rate of the EBSLN was obtained, which was helpful for identifying and protecting the EBSLN during thyroidectomy. This method also represents a new strategy for exposing the EBSLN in patients when IONM cannot be applied. We showed that the EBSLN entry point was localized within 2 mm from the sternothyroid muscle insertion and 5–15 mm from the anterior border of the sternothyroid muscle. A detailed understanding of the anatomical variation in the EBSLN is helpful for finding the EBSLN in the cricothyroid space to avoid the chance of EBSLN injury. In the future, we intend to make the operation simpler and more feasible by using a smaller wireless lens that can be magnetically attached to the hook.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Committee of Harbin Medical University, Cancer Hospital, Harbin Medical University. The patients/participants provided their written informed consent to participate in this study.
ZD-Design, writing and submission; RS-Data collection, writing; LZ-Data collection, writing; JH-Image edit; literature review; WB-Literature review; XZ-Literature review; JZ-Administrative support; CN-Design. All authors contributed to the article and approved the submitted version.
Haiyan Research Fund of the Harbin Medical University Cancer Hospital (Grant No. JJQN2023-07).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Stojadinovic A, Shaha AR, Orlikoff RF, Nissan A, Kornak MF, Singh B, et al. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg. (2002) 236(6):823–32. doi: 10.1097/00000658-200212000-00015
2. Dionigi G, Kim HY, Wu CW, Lavazza M, Materazzi G, Lombardi CP, et al. Neuromonitoring in endoscopic and robotic thyroidectomy. Updates Surg. (2017) 69(2):171–9. doi: 10.1007/s13304-017-0442-z
3. Gurleyik E, Gurleyik G. Intraoperative monitoring of external branch of the superior laryngeal nerve: functional identification, motor integrity, and its role on vocal cord function. J Invest Surg. (2018) 31(6):509–14. doi: 10.1080/08941939.2017.1362489
4. Sakorafas GH, Kokoropoulos P, Lappas C, Sampanis D, Smyrniotis V. External branch of the superior laryngeal nerve: applied surgical anatomy and implications in thyroid surgery. Am Surg. (2012) 78(9):986–91. doi: 10.1177/000313481207800940
5. Jansson S, Tisell LE, Hagne I, Sanner E, Stenborg R, Svensson P. Partial superior laryngeal nerve (SLN) lesions before and after thyroid surgery. World J Surg. (1988) 12(4):522–7. doi: 10.1007/BF01655439
6. Zhao Y, Zhao Z, Zhang D, Han Y, Dionigi G, Sun H. Improving classification of the external branch of the superior laryngeal nerve with neural monitoring: a research appraisal and narrative review. Gland Surg. (2021) 10(9):2847–60. doi: 10.21037/gs-21-518
7. Barczyński M, Randolph GW, Cernea C, International Neural Monitoring Study Group in Thyroid and Parathyroid Surgery. International survey on the identification and neural monitoring of the EBSLN during thyroidectomy. Laryngoscope. (2016) 126(1):285–91. doi: 10.1002/lary.25548
8. Hurtado-Lopez LM, Pacheco-Alvarez MI, Montes-Castillo Mde L, Zaldivar-Ramirez FR. Importance of the intraoperative identification of the external branch of the superior laryngeal nerve during thyroidectomy: electromyographic evaluation. Thyroid. (2005) 15(5):449–54. doi: 10.1089/thy.2005.15.449
9. Furlan JC, Brandão LG, Ferraz AR, Rodrigues AJ Jr. Surgical anatomy of the extralaryngeal aspect of the superior laryngeal nerve. Arch Otolaryngol Head Neck Surg. (2003) 129(1):79–82. doi: 10.1001/archotol.129.1.79
10. Wang K, Cai H, Kong D, Cui Q, Zhang D, Wu G. The identification, preservation and classification of the external branch of the superior laryngeal nerve in thyroidectomy. World J Surg. (2017) 41(10):2521–9. doi: 10.1007/s00268-017-4046-z
11. Ng SK, Li HN, Chan JY, Wong EWY, Vlantis AC. A useful landmark to locate the external branch of the superior laryngeal nerve during thyroidectomy. Gland Surg. (2020) 9(3):647–52. doi: 10.21037/gs.2020.03.25
12. Potenza AS, Phelan EA, Cernea CR, Slough CM, Kamani DV, Darr A, et al. Normative intra-operative electrophysiologic waveform analysis of superior laryngeal nerve external branch and recurrent laryngeal nerve in patients undergoing thyroid surgery. World J Surg. (2013) 37(10):2336–42. doi: 10.1007/s00268-013-2148-9
13. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. (2016) 26(1):1–133. doi: 10.1089/thy.2015.0020
14. Sung ES, Chang JH, Kim J, Cha W. Is cricothyroid muscle twitch predictive of the integrity of the EBSLN in thyroid surgery? Laryngoscope. (2018) 128(11):2654–61. doi: 10.1002/lary.27158
15. Tsai V, Celmer A, Berke GS, Chhetri DK. Videostroboscopic findings in unilateral superior laryngeal nerve paralysis and paresis. Otolaryngol Head Neck Surg. (2007) 136(4):660–2. doi: 10.1016/j.otohns.2006.11.024
16. Darr EA, Tufano RP, Ozdemir S, Kamani D, Hurwitz S, Randolph G. Superior laryngeal nerve quantitative intraoperative monitoring is possible in all thyroid surgeries. Laryngoscope. (2014) 124(4):1035–41. doi: 10.1002/lary.24446
17. Barczyński M, Konturek A, Stopa M, Honowska A, Nowak W. Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg. (2012) 36(6):1340–7. doi: 10.1007/s00268-012-1547-7
18. Tedla M, Chakrabarti S, Suchankova M, Weickert MO. Voice outcomes after thyroidectomy without superior and recurrent laryngeal nerve injury: VoiSS questionnaire and GRBAS tool assessment. Eur Arch Otorhinolaryngol. (2016) 273(12):4543–7. doi: 10.1007/s00405-016-4163-6
19. Cernea CR, Ferraz AR, Nishio S, Dutra A Jr, Hojaij FC, dos Santos LR. Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck. (1992) 14(5):380–3. doi: 10.1002/hed.2880140507
20. Dekhou AS, Morrison RJ, Gemechu JM. The superior laryngeal nerve and its vulnerability in surgeries of the neck. Diagnostics. (2021) 11(7):1243. doi: 10.3390/diagnostics11071243
21. Delbridge L. The ‘neglected’ nerve in thyroid surgery: the case for routine identification of the external laryngeal nerve. ANZ J Surg. (2001) 71(4):199. doi: 10.1046/j.1440-1622.2001.02120.x
22. Potenza AS, Araujo Filho VJF, Cernea CR. Injury of the external branch of the superior laryngeal nerve in thyroid surgery. Gland Surg. (2017) 6(5):552–62. doi: 10.21037/gs.2017.06.15
23. Iwata AJ, Liddy W, Barczyński M, Wu CW, Huang TY, Van Slycke S, et al. Superior laryngeal nerve signal attenuation influences voice outcomes in thyroid surgery. Laryngoscope. (2021) 131(6):1436–42. doi: 10.1002/lary.29413
24. Henry LR, Solomon NP, Howard R, Gurevich-Uvena J, Horst LB, Coppit G, et al. The functional impact on voice of sternothyroid muscle division during thyroidectomy. Ann Surg Oncol. (2008) 15(7):2027–33. doi: 10.1245/s10434-008-9936-8
25. Zhou B, Zhai Y, Hei H, Zhang S, Li C, Wang C, et al. The strap intermuscular approach can significantly increase the exposure rate of the external branch of the superior laryngeal nerve during thyroid surgery. Surg Oncol. (2020) 35:56–61. doi: 10.1016/j.suronc.2020.08.004
26. Uludag M, Aygun N, Kartal K, Besler E, Isgor A. Is intraoperative neural monitoring necessary for exploration of the superior laryngeal nerve? Surgery. (2017) 161(4):1129–38. doi: 10.1016/j.surg.2016.10.026
27. Friedman M, LoSavio P, Ibrahim H. Superior laryngeal nerve identification and preservation in thyroidectomy. Arch Otolaryngol Head Neck Surg. (2002) 128(3):296–303. doi: 10.1001/archotol.128.3.296
28. Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. (2013) 148(6 Suppl):S1–37. doi: 10.1177/0194599813487301
29. Aleksova L, Ali MM, Chakarov DI, Yozgyur ZM. Identification of the external branch of the superior laryngeal nerve during thyroid surgery. Folia Med. (2018) 60(1):154–7. doi: 10.1515/folmed-2017-0083
30. Hei H, Zhou B, Qin J, Song Y. Intermittent intraoperative nerve monitoring in thyroid reoperations: preliminary results of a randomized, single-surgeon study. Head Neck. (2016) 38(Suppl 1):E1993–7. doi: 10.1002/hed.24365
31. Sengul D, Sengul I, Ozturk T. Sutureless thyroidectomy with intraoperative neuromonitoring and energy-based device without sternotomy for symptomatic substernal goiter harboring thyroiditis of gland parenchyma. Cureus. (2021) 13(7):e16258. doi: 10.7759/cureus.16258
32. Gavid M, Dubois MD, Larivé E, Prades JM. Superior laryngeal nerve in thyroid surgery: anatomical identification and monitoring. Eur Arch Otorhinolaryngol. (2017) 274(9):3519–26. doi: 10.1007/s00405-017-4666-9
33. Ravikumar K, Sadacharan D, Muthukumar S, Mohanpriya G, Hussain Z, Suresh RV. EBSLN And factors influencing its identification and its safety in patients undergoing total thyroidectomy: a study of 456 cases. World J Surg. (2016) 40(3):545–50. doi: 10.1007/s00268-015-3383-z
34. Gurleyik E, Dogan S, Cetin F, Gurleyik G. Visual and electrophysiological identification of the external branch of superior laryngeal nerve in redo thyroid surgery compared with primary thyroid surgery. Ann Surg Treat Res. (2019) 96(6):269–74. doi: 10.4174/astr.2019.96.6.269
35. Engelsman AF, Warhurst S, Fraser S, Novakovic D, Sidhu SB. Influence of neural monitoring during thyroid surgery on nerve integrity and postoperative vocal function. BJS Open. (2018) 2(3):135–41. doi: 10.1002/bjs5.50
36. Chuang FJ, Chen JY, Shyu JF, Su CH, Shyr YM, Wu CW, et al. Surgical anatomy of the external branch of the superior laryngeal nerve in Chinese adults and its clinical applications. Head Neck. (2010) 32(1):53–7. doi: 10.1002/hed.21139
37. Aina EN, Hisham AN. External laryngeal nerve in thyroid surgery: recognition and surgical implications. ANZ J Surg. (2001) 71(4):212–4. doi: 10.1046/j.1440-1622.2001.02078.x
38. Cha YH, Moon SY, Jehoon O, Tansatit T, Yang HM. Anatomy of the external branch of the superior laryngeal nerve in Asian population. Sci Rep. (2017) 7(1):14952. doi: 10.1038/s41598-017-15070-9
Keywords: EBSLN, thyroidectomy, neuroanatomy, anatomical variations, cernea classification, surgical techniques
Citation: Ding Z, Sheng R, Zhang L, Han J, Chen M, Bi W, Zhao X, Zhang J and Nie C (2023) Utility of video-assisted method for identifying and preserving the external branch of the superior laryngeal nerve during thyroidectomy. Front. Surg. 10:1118083. doi: 10.3389/fsurg.2023.1118083
Received: 7 December 2022; Accepted: 3 April 2023;
Published: 18 April 2023.
Edited by:
Fabio Medas, University of Cagliari, ItalyReviewed by:
Ilker Sengul, Giresun University, Türkiye© 2023 Ding, Sheng, Zhang, Han, Chen, Bi, Zhao, Zhang and Nie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunlei Nie Y2h1bmxlaW5pZUBocmJtdS5lZHUuY24=
Specialty Section: This article was submitted to Otorhinolaryngology-Head and Neck Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.