
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 29 March 2023
Sec. Orthopedic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1111024
This article is part of the Research Topic Advances in Research of Degenerative Orthopedic Conditions: from Basic to Clinical Research View all 32 articles
Objective: Pelvic incidence (PI) minus the lumbar lordosis (LL) angle (PI-LL) correlates with function and disability. It is associated with paravertebral muscle (PVM) degeneration and is a valuable tool for surgical planning of adult degenerative scoliosis (ADS). This study aims to explore the characteristics of PVM in ADS with PI-LL match or mismatch and to identify the risk factors for PI-LL mismatch.
Methods: A total of 67 patients with ADS were divided into PI-LL match and mismatch groups. The visual analog scale (VAS), symptom duration, and Oswestry disability index (ODI) were used to assess patients’ clinical symptoms and quality of life. The percentage of fat infiltration area (FIA%) of the multifidus muscle at the L1-S1 disc level was measured by using MRI with Image-J software. Sagittal vertical axis, LL, pelvic tilt (PT), PI, sacral slope, and the asymmetric and average degeneration degree of the multifidus were recorded. Logistic regression analysis was done to identify the risk factors for PI-LL mismatch.
Results: In the PI-LL match and mismatch groups, the average FIA% of the multifidus on the convex side was less than that on the concave side (P < 0.05). There was no statistical difference of asymmetric degeneration degree of the multifidus between the two groups (P > 0.05). In the PI-LL mismatch group, the average degeneration degree of the multifidus, VAS, symptom duration, and ODI were significantly higher than that in the PI-LL match group, respectively (32.22 ± 6.98 vs. 26.28 ± 6.23 (%), 4.33 ± 1.60 vs. 3.52 ± 1.46, 10.81 ± 4.83 vs. 6.58 ± 4.23 (month), 21.06 ± 12.58 vs. 12.97 ± 6.49, P < 0.05). The average degeneration degree of the multifidus muscle was positively correlated with the VAS, symptom duration, and ODI, respectively (r = 0.515, 0.614, and 0.548, P < 0.05). Sagittal plane balance, LL, PT, and the average degeneration degree of the multifidus were the risk factors for PI-LL mismatch (OR: 15.447, 95% CI: 1.274–187.269; OR: 0.001, 95% CI: 0.000–0.099; OR: 107.540, 95% CI: 5.195–2,225.975; OR: 52.531, 95% CI: 1.797–1,535.551, P < 0.05).
Conclusion: The PVM on the concave side was larger than that on the convex side in ADS irrespective of whether PI-LL matched or not. PI-LL mismatch could aggravate this abnormal change, which is an important cause of pain and disability in ADS. Sagittal plane imbalance, decreased LL, higher PT, and larger average degeneration degree of the multifidus were independent risk factors for PI-LL mismatch.
Adult degenerative scoliosis (ADS) is a three-dimensional deformity in skeletally mature individuals, defined as a coronal deviation of greater than 10° (1). It is a common condition and often causes significant low back pain (LBP) and disability in adults (2). It has been reported that the incidence rate of ADS is up to 68% in the older population (3). Given its prevalence in the expanding portion of the global population aged older than 65 years, the disorder is of growing interest in the field of healthcare (4). Furthermore, ADS is a complicated deformity and has always been a matter of concern, but its pathogenesis remains unclear.
The paravertebral muscle (PVM) is closely associated with spinal deformities (5–7) and health-related quality of life (HRQOL) (8). The signal intensities and degree of fatty change of the multifidus muscle are higher in people with degenerative lumbar kyphosis than in the healthy population (5). There is a significant imbalance between fatty infiltration and muscle volume in the deep PVM of adolescent idiopathic scoliosis (AIS) (6). Our previous study found that there exists an asymmetric degeneration of the PVM in ADS, and the asymmetric change is more often seen on the concave side (7). In addition, the lumbar PVM fatty infiltration area (FIA) is closely related to LBP and disability in adults (8).
Pelvic incidence (PI) minus the lumbar lordosis (LL) angle (PI-LL) can be used to study the relationship between the pelvic and the lumbar curve, and both of them correlate with PVM degeneration (7, 9, 10). In addition, PI-LL is considered a valuable tool for surgical planning in the treatment of adult patients with spinal deformities (11–13) and correlates with function and disability, both of which are associated with PVM degeneration (5–7). However, the direct relationship between PI-LL and PVM has not been reported to date.
This study aims to reveal the characteristics of the PVM in ADS with PI-LL match or mismatch and identify the risk factors for PI-LL mismatch.
This was a retrospective cross-sectional study. Data from patients with ADS who were diagnosed at the Third Hospital of Hebei Medical University during the period from July 2010 to October 2019 were evaluated. The inclusion criteria were as follows: (1) aged ≥50; (2) presence of ADS, defined by a coronal Cobb angle >10°; (3) presence of ADS with no radiculopathy and those who did not receive physical therapy, acupuncture, or brace treatment. The exclusion criteria were as follows: (1) presence of symptomatic spinal stenosis with neurogenic claudication and those who received physical therapy, acupuncture, or brace treatment; (2) a recent history of trauma; (3) a prior diagnosis of scoliosis or other spine deformities; (4) underlying diseases such as diabetes mellitus (DM) and sarcopenia; (5) data integrity. All patients in this study had only symptoms of LBP. The visual analog scale (VAS), symptom duration, and Oswestry disability index (ODI) were used to assess the patients’ clinical symptoms and quality of life.
The radiography system used was a 500 mA Siemens DR System (Siemens Corporation, Germany) with an automatic exposure control system. The detailed parameters are as follows: the electric current was kept at 500 mA and the voltage at 75 kV on the anteroposterior position, and the current was kept at 500 mA and the voltage at 85 kV on the lateral position.
The MRI system was a 1.5 Tesla Imaging System (Siemens Magnetom Symphony, Germany). T1-weighted images (T1WI) and T2-weighted images (T2WI) of sagittal views of the lumbar intervertebral disc were obtained using a spin echo sequence system for T1WI and a fast spin echo sequence system for T2WI. A surface coil was used. The slice width was 4 mm and the interslice gap was 1 mm. The acquisition matrix was 512 × 256. The sequence parameter was repetition time (TR) 482 ms/echo time (TE) 10 ms for T1WI and TR 2,300 ms/TE 99 ms for T2WI.
X-ray and MRI were performed for all subjects and the data were recorded in detail.
Radiography was a useful tool to evaluate the bony structural parameters of ADS. The radiography consisted of a standing anteroposterior and lateral radiograph of the entire spine. In standard anteroposterior radiography, the lumbar scoliosis Cobb's angle, apical vertebral level, and curve direction of the main/compensatory curve were measured. A distance between the C7 plumb line (C7PL) and the center sacral vertical line (CSVL) of more than 2 cm represented coronal plane imbalance, and if this distance was less than 2 cm, it denoted coronal plane balance (14). In standard lateral radiography, the measurements were LL, and spinopelvic parameters included PI, pelvic tilt (PT), sacral slope (SS), and PI-LL. A sagittal vertical axis (SVA) <5 cm denoted sagittal plane balance, and if it was >5 cm, it represented sagittal plane imbalance. A total of 13 PI-LL < 10° were defined as the PI-LL match group and PI-LL ≧ 10° as the PI-LL mismatch group (15, 16).
MRI was a valuable tool to assess the changes in the PVM, and T2WI were taken at each L1-SI disc level. The center slice of the multifidus muscle was the primary research subject that included the cross-sectional area (CSA) and the percentage of fat infiltration area (FIA%). The CSA of the multifidus muscle was measured in the following steps. The first step was to set scale pixel/cm, converting pixels into cm measurement units by using the ruler present in the photographic image and converting each image into a grayscale 8-bit image. The second step was to measure the CSA of the multifidus muscle by outlining its region freehand using Image-J software. The measurement of FIA% was based on the above, using a threshold technique. The detailed operation steps were as follows: the value of the threshold was selected by the “default” and “dark background” method automatically and then image/adjust/ threshold/dark background and default/auto. Fat tissue in the 8-bit image was colored red using the threshold technique and the red area was measured as the FIA. FIA% was FIA divided by CSA.
Statistical analysis was conducted using IBM SPSS 20.0 software. Non-parametric tests were used to compare age and the ODI between PI-LL match and mismatch. The χ2 test was used to compare sex between PI-LL match and mismatch. The t-test was used to compare sex, the VAS score, and symptom duration, respectively, between PI-LL match and mismatch. The t-test was used to compare the asymmetric degeneration degree and average degeneration degree of the multifidus muscle between the two groups. The Pearson correlation coefficient was used to assess the correlation between the asymmetric and the average degeneration degree of the multifidus muscle and the VAS score and the symptom duration. Univariate and multivariate logistic regression analyses were used to identify the possible risk factors. For all statistical analysis, the level of significance was set at P < 0.05.
A total of 67 patients who met the above criteria were enrolled in this study, and they included 17 males and 50 females. The mean age was 63.1 ± 7.2 (years) and the mean body mass index (BMI) was 25.4 ± 1.8 (kg/m2). The subjects were divided into two groups: PI-LL match group (31 cases) and PI-LL mismatch group (36 cases). The mean age of the PI-LL mismatch group was more likely older than that of the PI-LL match group (65.0 ± 5.5 vs. 61.0 ± 8.4, P < 0.05, Table 1), but gender distribution and BMI were not statistically different between the two groups (P > 0.05, Table 1).
The VAS score in the PI-LL mismatch group was 4.33 ± 1.60, which was higher than that in the PI-LL match group, which was 3.52 ± 1.46 (P < 0.05, Table 1). The symptom duration (month) in the PI-LL mismatch group was 10.81 ± 4.83, which was higher than that in the PI-LL match group, which was 6.58 ± 4.23 (P < 0.05, Table 1). The ODI in the PI-LL mismatch group was 21.06 ± 12.58, which was higher than that in the PI-LL match group, which was 12.97 ± 6.49 (P < 0.05, Table 1).
In the PI-LL match group, the average FIA% of the multifidus muscle on the convex side was 22.41 ± 8.45 (%), 22.16 ± 8.70 (%), 25.82 ± 9.70 (%), 25.80 ± 7.10 (%), and 29.89 ± 8.61 (%), and on the concave side, it was 31.87 ± 9.05 (%), 35.18 ± 12.32 (%), 32.49 ± 9.89 (%), 33.32 ± 8.72 (%), and 37.77 ± 10.42 (%) at the L1-2, L2-3, L3-4, L4-5, and L5-S1 levels. The average FIA% of the multifidus muscle on the concave side was larger than that on the convex side at each level (P < 0.05, Table 2).
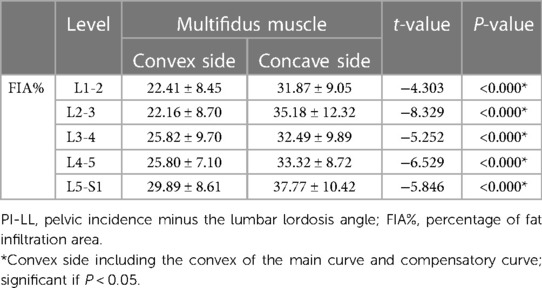
Table 2. The FIA% of the multifidus muscle on the concave and convex sides in the PI-LL match group.
In the PI-LL mismatch group, the average FIA% of the multifidus muscle on the convex side was 24.49 ± 7.98 (%), 25.02 ± 9.73 (%), 26.78 ± 9.31 (%), 27.18 ± 7.71 (%), and 31.76 ± 8.64 (%), and on the concave side, it was 36.05 ± 12.14 (%), 38.29 ± 11.85 (%), 35.57 ± 13.19 (%), 36.12 ± 9.60 (%), and 40.95 ± 9.91 (%) at the L1-2, L2-3, L3-4, L4-5, and L5-S1 levels. The average FIA% of the multifidus muscle on the concave side was larger than that on the convex side at each level (P < 0.05, Table 3) (Figures 1–3).
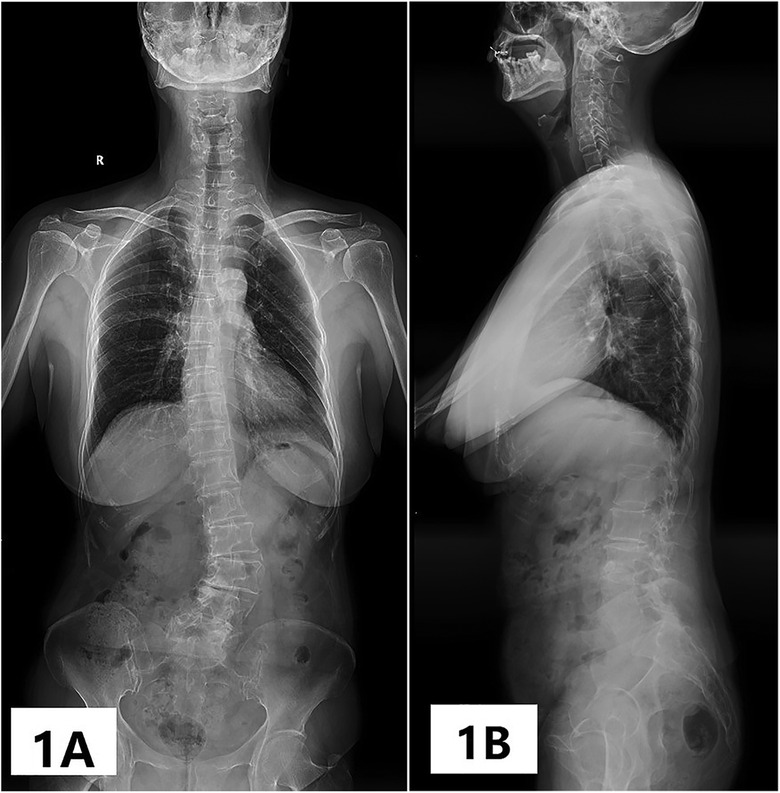
Figure 1. (A) Apical vertebrae was L3 vertebrae, the scoliosis Cobb's angle was 40°, and the coronal plane was imbalanced; the main curve was located on the lumbar segment with left scoliosis, and the compensatory curve whose orientation was opposite to the main curve was located on the lumbosacral segment. (B) LL = 41°, SS = 36°, PT = 32°, PI = 68°, PI-LL = 27° and the sagittal plane was imbalanced.
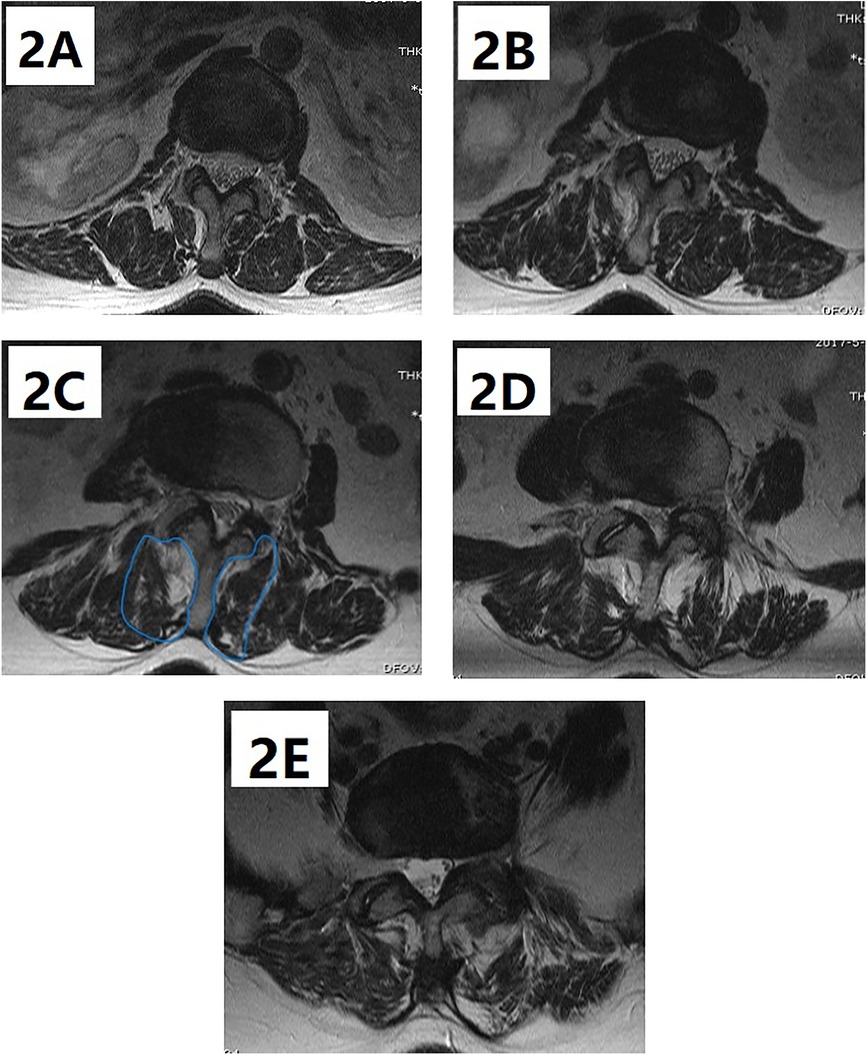
Figure 2. (A–E) Fat tissue on the MRI is colored in white; FIA% of the multifidus muscle on the convex side is 27.09%, 14.26%, 30.37%, 33.36%, and 30.69%, and on the concave side, it is 40.67%, 42.77%, 39.25%, 34.16%, and 43.02% at the L1-2, L2-3, L3-4, L4-5, and L5-S1 levels, respectively; the asymmetric degree of the multifidus muscle is 12.82% and the average degree of the multifidus muscle is 33.57%.
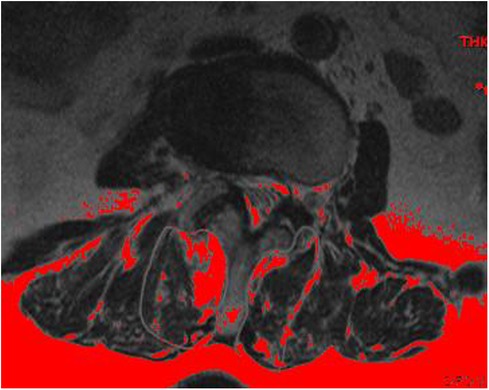
Figure 3. Fat tissue on the MRI is colored in red (a darker background in the red version) using the threshold technique.
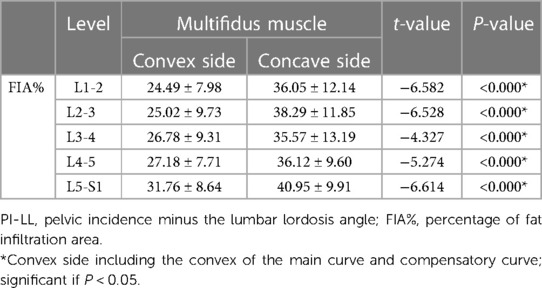
Table 3. The FIA% of the multifidus muscle on the concave and convex sides in the PI-LL mismatch group.
The asymmetric degeneration degree of the multifidus muscle in the PI-LL match group was 8.91 ± 4.61 (%), and in the PI-LL mismatch group, it was 10.35 ± 5.44 (%), and there was no statistical difference between the two groups (P > 0.05, see Table 4). The average degeneration degree of the multifidus muscle in the PI-LL mismatch group was 32.22 ± 6.98 (%), which was higher than that in the PI-LL match group, which was 26.28 ± 6.23 (%) (P < 0.05, Table 4).
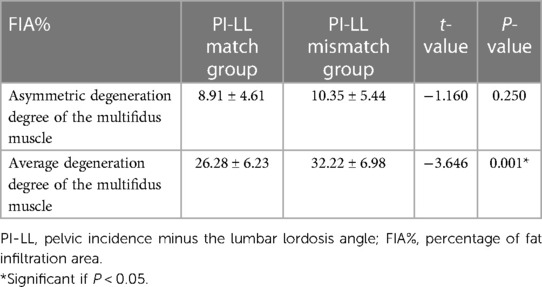
Table 4. Asymmetric and average degeneration degree of the multifidus muscle between PI-LL match and PI-LL mismatch groups.
In the 67 patients in this study, the asymmetric degree of the multifidus muscle was positively correlated with symptom duration (r = 0.403, P < 0.05, Table 5). There was no correlation between the asymmetric degree of the multifidus muscle and the VAS score or ODI (P > 0.05, Table 5). The average degeneration degree of the multifidus muscle was positively correlated with the VAS score, symptom duration, and ODI, respectively (r = 0.515, 0.614, 0.548, P < 0.05, Table 5).
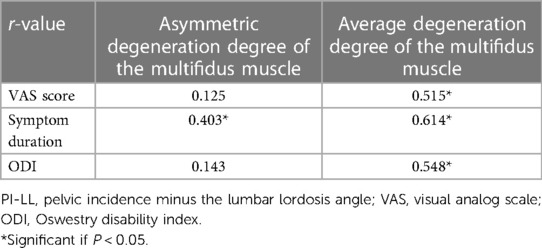
Table 5. Correlation between asymmetric and average degeneration degree of the multifidus muscle and the VAS score, symptom duration, and ODI.
The univariate logistic regression analysis showed that age, scoliosis Cobb angle, sagittal plane balance, LL, PT, SS, and average degeneration degree of the multifidus muscle were independent risk factors for ADS with PI-LL mismatch (P < 0.05, Table 6). The binary multivariate logistic regression analysis revealed that sagittal plane balance, LL, PT, and average degeneration degree of the multifidus muscle were risk factors for ADS with PI-LL mismatch (OR: 15.447, 95% CI: 1.274–187.269, P = 0.032; OR: 0.001, 95% CI: 0.000–0.099, P = 0.004; OR: 107.540, 95% CI: 5.195–2,225.975, P = 0.002; OR: 52.531, 95% CI: 1.797–1,535.551, P = 0.021, Table 7).
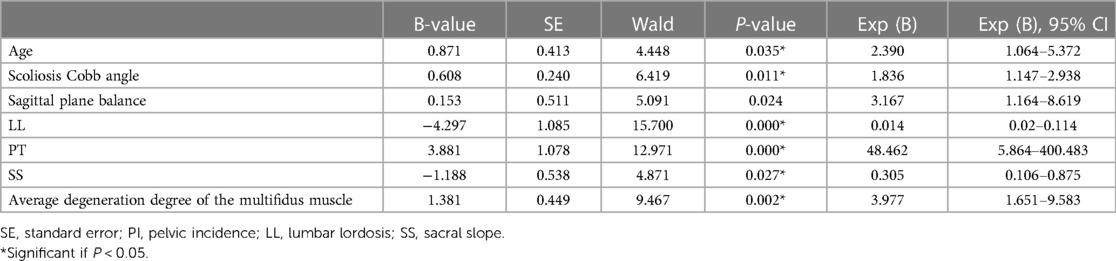
Table 6. Univariate logistic regression analysis of significantly different variables for the factors associated with PI-LL mismatch.
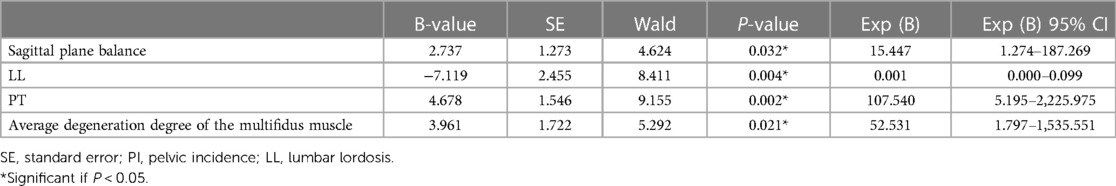
Table 7. Multivariate logistic regression analysis of significantly different variables for the factors associated with PI-LL mismatch.
The multifidus muscle, the most medial PVM, plays a key role in lumbar stability, and is often regarded as the subject of primary research for its sensitivity to pathologic change. In patients with unilateral lumbar disc herniation, there exist ipsilateral abnormal changes in the multifidus muscle (17). In addition, our team found that there existed asymmetric PVM changes in ADS and its asymmetric degree was associated with bony structural parameters such as apical vertebral rotation, lateral vertebral translation, LL, and lumbar scoliosis Cobb's angle (7). For further study, we investigated the relationship between multifidus and PI-LL, and we found that the latter was a novel spinopelvic parameter for surgical planning in the treatment of adult patients with spinal deformities.
Spinopelvic parameters form a part of the most important bony structural parameters and are closely related to disability and quality of life (8, 11, 18, 19). PI-LL mismatch is directly related to poor q;’lpuality of life in ASD patients (11). A higher PI-LL leads to worse LBP and PI-LL mismatch is correlated to postoperative residual symptoms (20). In this study, the VAS score, pain duration, and ODI of patients in the PI-LL mismatch group were found to be higher than in the PI-LL match group, and the results were consistent with those of previous studies. It is important to study PI-LL for understanding the clinical symptoms, progression, and surgical treatment of ADS. The purpose of this study was to reveal the characteristics of the PVM in ADS with PI-LL match or mismatch and identify the risk factors for PI-LL mismatch.
In the PI-LL match and mismatch groups, the FIA% of the multifidus muscle on the concave side was significantly larger than that on the convex side, and the characteristics of the PVM were similar. These results were consistent with those of previous studies on the correlation between PVM and scoliosis (7, 21–23). The FIA was greater on the concave side than on the convex side in AIS, and the multifidus muscle on the convex side was smaller than on the concave side at the apex in idiopathic scoliosis (IS) (21, 22). In ADS, the FIA of the multifidus muscle on the concave side was also significantly higher than on the convex side at the apical vertebral level (23). In our previous study, there existed asymmetric PVM changes in ADS and FIA% on the concave side was higher than on the convex side (7). The above results were consistent with those of this study and revealed that the pattern of PVM change was similar no matter what type of scoliosis it was. Different from former studies, we further divided ADS patients into two groups and found that the characteristics of PVM asymmetric change were the same and were not related to PI-LL match or mismatch. Therefore, it was considered that the asymmetric change resulted from the mechanical asymmetry of the spine in patients with scoliosis and that sagittal parameters had less effect on this asymmetry.
Between the PI-LL match group and the mismatch group, there was no statistical difference in asymmetric degeneration of the multifidus muscle. PI was an anatomical parameter that was relatively fixed and reflected spinopelvic morphotypes (13). LL could reveal the lumbar sagittal plane condition and could be influenced by factors such as age, sex, and disc degeneration (24). Based on this thesis, we considered that LL was a key factor influencing the value of PI-LL. In our previous study, we found that the asymmetric degree was negatively correlated with LL, but the correlation was weak (7). A possible reason was that there existed a negative correlation between LL and scoliosis Cobb's angle and the latter directly influenced the PVM change (7, 25–27). When the LL increased by 10°, the lumbar scoliosis Cobb's angle reduced at least by 5° (25). In this study, a tendency towards increase in PI-LL mismatch could be discerned, although the asymmetry degree was not statistically different between the two groups. Moreover, the asymmetric degree of the multifidus muscle was positively correlated with pain duration, but there was no correlation between the asymmetric degree of the multifidus muscle, VAS score and ODI. We considered that pain could lead to an abnormal posture. The longer the pain duration, the greater asymmetric pressure on the PVM and, finally, the asymmetric degree of the multifidus muscle is aggravated.
In the PI-LL mismatch group, the average degeneration degree of the multifidus muscle was higher than in the PI-LL match group, and the VAS score, pain duration, and ODI were more severe than in the latter group. This result was consistent with the trend of the average degeneration degree of the multifidus muscle. Furthermore, we found that the average degeneration degree of the multifidus muscle was positively correlated with the VAS score, symptom duration, and ODI, respectively. It could be inferred that the possible mechanism was that PI-LL mismatch could aggravate the degeneration of the PVM, and the latter was an important source of pain (8, 28, 29), disability (28), and lumbar instability (30, 31). Wu et al. reported that the VAS score and ODI were significantly positively correlated with the tone and stiffness of the PVM on the painful side (32). Protopsaltis concluded that PI-LL correlated with the ODI and Short Form-36 physical component score scoliosis research society (SRS) correlated with all (33). Skeletal malalignment might result in a greater recruitment in muscular effort and a greater energy expenditure to maintain the erect posture as well as the use of compensatory mechanisms (13). Several studies supported the idea that the appropriate sagittal alignment determined the outcome of spinal deformity surgery and that it is a better determinant of HRQOL and pain in patients (13, 34, 35). A better correction of PI-LL mismatch could result in good clinical outcomes in patients with degenerative flat back deformity and ASD (36). In this study, we clarified the importance of PI-LL and the possible mechanism of pain and disability resulting from PI-LL mismatch and inferred that PI-LL mismatch could aggravate PVM degeneration which was possibly associated with pain and disability in ADS patients.
The present study showed that sagittal plane imbalance, decreased LL, higher PT, and larger average degeneration degree of the multifidus muscle were the independent risk factors for ADS with PI-LL mismatch. There existed a chain of interconnected parameters including SVA, PT, SS, and LL (37, 38). ASD could perturb regional alignment, which might result in a chain of modification along the standing axis. In severe ADS, the consequences were decreased LL, larger PT, and SVA, leading to a “spinopelvic mismatch” radiographically and a resultant loss of function and disability (13). The results of this study were consistent with those of previous studies (13, 15, 16, 37, 38). In addition, the degenerative PVM was less effective in maintaining spinal stability and restoring sagittal plane alignment. We first confirmed that a larger average degeneration degree of the multifidus muscle was an important risk factor for PI-LL mismatch. Lee et al. supported the idea that volume loss of lumbar PVM and ectopic FIA into the PVM may cause spinopelvic deformity (39). Menezes-Reis reported that there was significant correlation between spinopelvic parameters and lumbar PVM volumes (40).
There are also limitations in this study. First, the number of patients with ADS was relatively small. Second, there is a lack of studies on CT, electromyography (EMG), histochemistry, cytology, and pathology to support the findings. In the future, we need to collect more imaging data of patients with ADS through multicenter recruitment and employ more methods of investigation.
The PVM on the concave side was larger than on the convex side in ADS irrespective of PI-LL was matched or mismatched. PI-LL mismatch could aggravate this abnormal change, which was an important reason for pain and disability in ADS patients. Sagittal plane imbalance, decreased LL, higher PT, and larger average degeneration degree of the multifidus muscle were independent risk factors for PI-LL mismatch. Strengthening of the PVM may be beneficial in preventing PI-LL mismatch in ADS patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
WD, JG, and DX contributed to the conception and design of the study. BZ organized the database. JZ performed the statistical analysis. JG wrote the first draft of the manuscript. DX, YH, and ZL wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
We would like to thank the experts in the Imaging Department in the Third Hospital of Hebei Medical University for rendering their invaluable help and support for this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1111024/full#supplementary-material.
1. Wong E, Altaf F, Oh LJ, Gray RJ. Adult degenerative lumbar scoliosis. Orthopedics. (2017) 40(6):e930–9. doi: 10.3928/01477447-20170606-02
2. Jin LY, Wang K, Lv ZD, Su XJ, Liu HY, Shen HX, et al. Therapeutic strategy of percutaneous transforaminal endoscopic decompression for stenosis associated with adult degenerative scoliosis. Global Spine J. (2022) 12(4):579–87. doi: 10.1177/2192568220959036
3. Schwab F, Dubey A, Gamez L, EI Fegoun AB, Hwang K, Pagala M, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. (2005) 30(9):1082–85. doi: 10.1097/01.brs.0000160842.43482.cd
4. Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, et al. Adult spinal deformity. Lancet. (2019) 394(10193):160–72. doi: 10.1016/S0140-6736(19)31125-0
5. Hyun SJ, Bae CW, Lee SH, Rhim SC. Fatty degeneration of the paraspinal muscle in patients with degenerative lumbar kyphosis: a new evaluation method of quantitative digital analysis using MRI and CT scan. Clin Spine Surg. (2016) 29(10):441–7. doi: 10.1097/BSD.0b013e3182aa28b0
6. Jiang J, Meng Y, Jin X, Zhang C, Zhao J, Wang C, et al. Volumetric and fatty infiltration imbalance of deep paravertebral muscles in adolescent idiopathic scoliosis. Med Sci Monit. (2017) 23:2089–95. doi: 10.12659/msm.902455
7. Xie D, Zhang J, Ding W, Yang S, Yang D, Ma L, et al. Abnormal change of paravertebral muscle in adult degenerative scoliosis and its association with bony structural parameters. Eur Spine J. (2019) 28(7):1626–37. doi: 10.1007/s00586-019-05958-7
8. Crawford RJ, Volken T, Ni Mhuiris Á, Bow CC, Elliott JM, Hoggarth MA, et al. Geography of lumbar paravertebral muscle fatty infiltration: the influence of demographics, low back pain, and disability. Spine. (2019) 44(18):1294–302. doi: 10.1097/brs.0000000000003060
9. Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V. Sagittal alignment of the spine: what do you need to know? Clin Neuro Neurosurg. (2015) 139:295–301. doi: 10.1016/j.clineuro.2015.10.024
10. Thakar S, Sivaraju L, Aryan S, Mohan D, Sai Kiran NA, Hegde AS. Lumbar paraspinal muscle morphometry and its correlations with demographic and radiological factors in adult isthmic spondylolisthesis: a retrospective review of 120 surgically managed cases. J Neurosurg Spine. (2016) 24(5):679–85. doi: 10.3171/2015.9.spine.15705
11. Bourret S, Cerpa M, Kelly MP, Hasegawa K, Hey HWD, Wong HK, et al. Correlation analysis of the PI-LL mismatch according to the pelvic incidence from a database of 468 asymptomatic volunteers. Eur Spine J. (2022) 31(6):1413–20. doi: 10.1007/s00586-021-07087-6
12. Passias PG, Bortz CA, Segreto FA, Horn SR, Pierce KE, Manning J, et al. Pelvic incidence affects age-adjusted alignment outcomes in a population of adult spinal deformity. Clin Spine Surg. (2021) 34(1):E51–6. doi: 10.1097/BSD.0000000000001025
13. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine. (2010) 35(25):2224–31. doi: 10.1097/BRS.0b013e3181ee6bd4
14. Zhang RF, Liu K, Wang X, Liu Q, He JW, Wang XY, et al. Reliability of a new method for measuring coronal trunk imbalance, the axis-line-angle technique. Spine J. (2015) 15(12):2459–65. doi: 10.1016/j.spinee.2015.08.022
15. Bai H, Li Y, Liu C, Zhao Y, Lei W, Feng Y, et al. Surgical management of degenerative lumbar scoliosis associated with spinal stenosis: does the PI-LL matter? Spine. (2020) 45(15):1047–54. doi: 10.1097/brs.0000000000003465
16. Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, et al. Scoliosis research society—schwab adult spinal deformity classification: a validation study. Spine. (2012) 37(12):1077–82. doi: 10.1097/BRS.0b013e31823e15e2
17. Stevens S, Agten A, Timmermans A, Vandenabeele F. Unilateral changes of the multifidus in persons with lumbar disc herniation: a systematic review and meta-analysis. Spine J. (2020) 20(10):1573–85. doi: 10.1016/j.spinee.2020.04.007
18. Uehara M, Lkgami S, Horiuchi H, Takahashi J, Kato H. Prevalence and related factors of low back pain in the general elderly population: a Japanese cross-sectional study randomly sampled from a basic resident registry. J Clin Med. (2021) 10(18):4213. doi: 10.3390/jcm10184213
19. Li J, Zhang D, Shen Y, Qi X. Lumbar degenerative disease after oblique lateral interbody fusion: sagittal spinopelvic alignment and its impact on low back pain. J Orthop Surg Res. (2020) 15(1):326. doi: 10.1186/s13018-020-01837-w
20. Aoki Y, Nakajima A, Takahashi H, Sonobe M, Terajima F, Saito M, et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord. (2015) 16:213. doi: 10.1186/s12891-015-0676-1
21. Wajchenberg M, Astur N, Fernandes EA, Paredes-Gamero EJ, Luciano RP, Schmidt B, et al. Assessment of fatty infiltration of the multifidus muscle in patients with adolescent idiopathic scoliosis through evaluation by magnetic resonance imaging compared with histological analysis: a diagnostic accuracy study. J Pediatr Orthop B. (2019) 28(4):362–7. doi: 10.1097/bpb.0000000000000578
22. Fidler MW, Jowett RL. Muscle imbalance in the aetiology of scoliosis. J Bone Joint Surg Br. (1976) 58(2):200–1. doi: 10.1302/0301-620x.58b2.932082
23. Tang Y, Yang S, Chen C, Luo K, Chen Y, Wang D, et al. Assessment of the association between paraspinal muscle degeneration and quality of life in patients with degenerative lumbar scoliosis. Exp Ther Med. (2020) 20(1):505–11. doi: 10.3892/etm.2020.8682
24. Chun SW, Lim CY, Kim K, Hwang J, Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J. (2017) 17(8):1180–91. doi: 10.1016/j.spinee.2017.04.034
25. Murata Y, Takahashi K, Hanaoka E, Utsumi T, Yamagata M, Moriya H. Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine. (2002) 27(20):2268–73. doi: 10.1097/00007632-200210150-00016
26. Sun XY, Kong C, Zhang TT, Lu SB, Wang W, Sun SY, et al. Correlation between multifidus muscle atrophy, spinopelvic parameters, and severity of deformity in patients with adult degenerative scoliosis: the parallelogram effect of LMA on the diagonal through the apical vertebra. J Orthop Surg Res. (2019) 14(1):276. doi: 10.1186/s13018-019-1323-6
27. Yagi M, Hosogane N, Watanabe K, Asazuma T, Matsumoto M. The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J. (2016) 16(4):451–8. doi: 10.1016/j.spinee.2015.07.001
28. Suh JH, Kim H, Jung GP, Ko JY, Ryu JS. The effect of lumbar stabilization and walking exercises on chronic low back pain: a randomized controlled trial. Medicine. (2019) 98(26):e16173. doi: 10.1097/md.0000000000016173
29. Janssens L, McConnell AK, Pijnenburg M, Claeys K, Goossens N, Lysens R, et al. Inspiratory muscle training affects proprioceptive use and low back pain. Med Sci Sports Exerc. (2015) 47(1):12–9. doi: 10.1249/mss.0000000000000385
30. Zhou Z, Zhang Y, Chen W, Wang J. Massage manipulation vs. low back muscle exercise for lumbar intervertebral instability: a preliminary randomized clinical trial. J Pak Med Assoc. (2020) 70(2):324–36. doi: 10.5455/jpma.302076
31. Wattananon P, Prasertkul W, Sakulsriprasert P, Laskin JJ. Effect of increased relative stiffness of the lumbar spine on hamstring muscle stretching in individuals with a history of low back pain suspected to have a clinical lumbar instability: a randomized crossover design. Clin Biomech. (2020) 75:104996. doi: 10.1016/j.clinbiomech.2020.104996
32. Wu ZG, Ye XL, Ye ZX, Hong KH, Chen ZH, Wang Y, et al. Asymmetric biomechanical properties of the paravertebral muscle in elderly patients with unilateral chronic low back pain: a preliminary study. Front Bioeng Biotechnol. (2022) 10:814099. doi: 10.3389/fbioe.2022.814099
33. Protopsaltis TS, Lafage R, Smith JS, Passias PG, Shaffrey CI, Kim HJ, et al. The lumbar pelvic angle, the lumbar component of the T1 pelvic angle, correlates with HRQOL, PI-LL mismatch, and it predicts global alignment. Spine. (2018) 43(10):681–7. doi: 10.1097/brs.0000000000002346
34. Sun XY, Zhang XN, Hai Y. Optimum pelvic incidence minus lumbar lordosis value after operation for patients with adult degenerative scoliosis. Spine J. (2017) 17(7):983–9. doi: 10.1016/j.spinee.2017.03.008
35. Makino T, Kaito T, Sakai Y, Takenaka S, Yoshikawa H. Health-related quality of life and postural changes of spinal alignment in female adolescents associated with back pain in adolescent idiopathic scoliosis: a prospective cross-sectional study. Spine. (2019) 44(14):E833–40. doi: 10.1097/BRS.0000000000002996
36. Kim KT, Lee SH, Huh DS, Kim HJ, Kim JY, Lee JH. Restoration of lumbar lordosis in flat back deformity: optimal degree of correction. Asian Spine J. (2015) 9(3):352–60. doi: 10.4184/asj.2015.9.3.352
37. Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. (2006) 31(25):E959–67. doi: 10.1097/01.brs.0000248126.96737.0f
38. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. (2005) 87(2):260–7. doi: 10.2106/jbjs.d.02043
39. Lee D, Kuroki T, Nagai T, Kawano K, Higa K, Kurogi S, et al. Sarcopenia, ectopic fat infiltration into the lumbar paravertebral muscles, and lumbo-pelvic deformity in older adults undergoing lumbar surgery. Spine. (2022) 47(2):E46–57. doi: 10.1097/brs.0000000000004175
Keywords: adult degenerative scoliosis, paravertebral muscle, fat infiltration area, PI-LL mismatch, risk factor
Citation: Guo J, Xie D, Zhang J, Ding W, Zhao B, Li Z and Huo Y (2023) Characteristics of the paravertebral muscle in adult degenerative scoliosis with PI-LL match or mismatch and risk factors for PI-LL mismatch. Front. Surg. 10:1111024. doi: 10.3389/fsurg.2023.1111024
Received: 29 November 2022; Accepted: 7 March 2023;
Published: 29 March 2023.
Edited by:
Jaimo Ahn, University of Michigan, United StatesReviewed by:
Paul Porensky, US Navy, United States© 2023 Guo, Xie, Zhang, Ding, Zhao, Li and Huo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenyuan Ding ZGluZ3dlbnl1YW4yMDEyQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.