
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 08 February 2023
Sec. Reconstructive and Plastic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1109936
This article is part of the Research Topic Insights in Reconstructive and Plastic Surgery: 2022 View all 7 articles
 Hyeokjae Kwon1,2,†
Hyeokjae Kwon1,2,† Seokui Lee1,†
Seokui Lee1,† Sunje Kim1,†
Sunje Kim1,† Seung Han Song1,2,†
Seung Han Song1,2,† Sang-Ha Oh1,2,†
Sang-Ha Oh1,2,† Joo-hak Kim3,†
Joo-hak Kim3,† Hyunwoo Kyung2,3,†
Hyunwoo Kyung2,3,† Ho Jik Yang3
Ho Jik Yang3 Yooseok Ha1,2*†
Yooseok Ha1,2*†
A gastrocnemius muscle flap is a versatile option for covering the proximal one-third of the lower leg and around the knee. On the other hand, it is of limited use in patients with short gastrocnemius muscle or insufficient volume. The authors present a case in which a knee soft tissue defect occurred in a very thin patient and was reconstructed using a gastrocnemius myocutaneous flap and a distally based gracilis flap as a supplementary flap.
Skin and soft tissue defects around the knee are a challenge for reconstructive surgeons, and proper reconstruction is essential for patients to return to daily life (1). As the success rate of free tissue transfer increases, attempts to reconstruct knee defects using the procedure are increasing, but it is still difficult due to the deeply positioned recipient vessels (2). In general, knee defects can be covered by diverse muscle flaps, such as pedicled gastrocnemius muscle flap (3), distally pedicled gracilis flap (4), distal sartorius muscle flap (5), and distally based split vastus lateralis musculocutaneous flap (6). Among them, the medial gastrocnemius muscle flap is the “cornerstone” of the strategy for reconstructing defects around the knee and is considered to be a simple and safe method (7). However, the gastrocnemius muscle flap is often insufficient in volume and length, especially for the elderly with degenerated muscles or thin patients (8). The authors present a case in which a knee soft tissue defect occurred in a very thin patient and was reconstructed through a gastrocnemius myocutaneous flap and a distally based gracilis flap simultaneously.
An 80-year-old female patient with an underlying medical disease, hypertension, cerebral infarction, and heart failure was admitted to the hospital with a surgical site infection on the knee. She underwent total knee replacement arthroplasty four years ago to treat degenerative osteoarthritis. One year after surgery, a periprosthetic infection occurred, resulting in a soft tissue defect, and a free flap was performed to cover the defect.
The skin flap was fine, but the infection from the inside continued, causing soft tissue necrosis and dead space. Some openings on the skin occurred, with pus passing through it. The decision was to replace the artificial joint and capsule of knee reconstruction surgery after consulting with orthopedics.
The patient was very thin with a BMI of 15.81 (38 kg, 155 cm), and another free flap was recommended but declined due to previous surgical experience. Surgery for a capsule of knee reconstruction was decided with a gastrocnemius flap as the first choice. After replacing the artificial joint, the size of the capsule defect was confirmed as 11 cm × 6 cm. The capsule defect would be challenging to cover with only the gastrocnemius flap. Eventually, The flap volume was expected to be insufficient, so the following method was used (Figures 1, 2).
1. The gastrocnemius myocutaneous flap was elevated, and the distal halves were dissected and divided to cover the lower 50% defect. The skin island covering the gastrocnemius muscle was buried after deepithelization.
2. The gastrocnemius muscle fascia was scored to expand, and its origin was detached.
3. A distally based gracilis flap was used to cover the upper 50% defect.
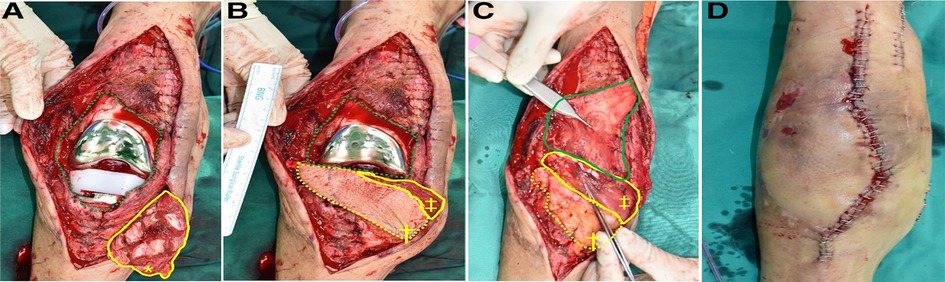
Figure 1. Intraoperative photographs. (A) 11 cm × 6 cm sized capsule defect (green dotted line), scored gastrocnemius muscle fascia (yellow bold line). (B) Gastrocnemius musculocutaneous flap covered the lower half. (C) Deepithelized skin island (yellow dotted line), the gastrocnemius muscle, and the distally based gracilis (green bold line) covered the defect was and sutured. (D) An immediate postoperative appearance after skin closure. (*, scored gastrocnemius muscle fascia; †, skin island overlying gastrocnemius muscle; ‡, gastrocnemius muscle).
The reconstruction operation took approximately two hours. The deepithelized skin and both muscle flaps showed bright red bleeding after the suture, indicating a healthy state. Primary closure of the skin envelope was possible owing to the previous free flap. The wound healing was uneventful and was well maintained two months after surgery.
The medial gastrocnemius muscle flap is considered a simple and safe method and is commonly used to reconstruct defects around the knee and proximal leg (9). Typically, the reach of the muscle is restricted to just below the knee, so the release of the medial femoral condyle and scoring of the deep fascia is used to increase the reach (10). In addition, the volume of the distal part of the muscle for defect coverage is small (11), and is even smaller when accompanied by disuse atrophy or aging, as in this case.
A chimeric gastrocnemius muscle and sural artery perforator flap were used to overcome this (12, 13). Because each component can be inset independently in a chimeric flap, it is highly preferable for 3-dimensional defects. On the other hand, the perforator needs to be mobilized carefully to prevent venous compromise, and according to its location, a sophisticated design suitable for the defect is required.
In this case, instead of completely separating the muscle component and the skin flap, only 1/3 of the distal area was separated and spread like a fan to increase the coverage area. As the patient had undergone a free flap before, she had relatively redundant skin. Hence, the skin flap covering the gastrocnemius muscle was used only to cover the capsule after deepithelization.
Even after covering with a deepithelized skin flap and gastrocnemius flap, a defect still occurred in the upper third; a distally pedicled gracilis flap was used to cover the rest (4, 14). A distally pedicled gracilis flap has been used for soft tissue defects around the knee, where a pedicled gastrocnemius muscle is inadequate or has already been used.
The gracilis muscle, based on the minor pedicles, would appear to run counter to the current appreciation of the vascular anatomy of this type II flap. In type II flaps, it is generally believed that such a flap cannot survive in its entirety on the minor vascular pedicle(s) unless delayed for 10–14 days (3). On the other hand, recent cadaveric and CT angiogram work has suggested that these minor pedicles may be sufficient to sustain the muscle without a delay procedure and was used successfully in three cases.
One of the most significant advantages of the gracilis flap, distally based on minor pedicles, is the short operative time. There are a few choices available to cover the superior medial defect of the knee. One of the choices is a free flap, but a gracilis flap takes a shorter operative time. Therefore, it is more suitable for elderly patients who are reluctant to receive a free flap.
A distally based gracilis flap has a locational advantage. If a gastrocnemius flap is insufficient to cover the defect, the remaining defect would be the upper part of the defect. The pivot point of the gracilis muscle is the superior medial part of the knee compared to the inferior pivot point of the gastrocnemius flap.
Finally, in the gastrocnemius flap, the volume of the distal part of the muscle for defect coverage is small because the muscle is cut near the tendon. On the other hand, in a distally based gracilis flap which was cut in the proximal muscular part. The end of this flap can be spread like fan, so can be used for wider defect. Therefore, the distal part of the flap is not narrow and can cover wide defects.
Despite the many advantages of a distally based gracilis flap, not many knee reconstructions have been performed using it. This is because a two-stage operation is considered necessary. Nevertheless, the technique should be considered by reconstructive surgeons or regarded as a useful supplementary flap that can be used when a gastrocnemius flap alone is insufficient.
Many knee reconstructions are possible through the gastrocnemius muscle flap alone, but its role is limited in patients with insufficient volume. In this case, a free flap can be a better option, but there are cases where it is impossible. The author reconstructed the defect in a short time using the gastrocnemius muscle and skin island separately and using a supplementary flap in a patient who could not perform the free flap. The method shown in this case could be considered a way to reconstruct the knee in limited circumstances.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Institutional Review Board of Chungnam National University Hospital. The patients/participants provided their written informed consent to participate in this study.
HK: Writing; SL: Writing; SK: Formal analysis; SHS: Writing; S-HO: Manuscript Review; JK: Conception; HK: Conception; HJY: Manuscript Review; YH: Correspondence. All authors contributed to the article and approved the submitted version.
This work was supported by Chungnam National University Hospital Research Fund, 2021. This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2021R1G1A101369411).
This work was supported by research fund of Chungnam National University Hospital. This work was supported by Chungnam National University Hospital Research Fund, 2021. This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, & Future Planning (NRF-2021R1G1A1013694).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Gravvanis A, Kyriakopoulos A, Kateros K, Tsoutsos D. Flap reconstruction of the knee: a review of current concepts and a proposed algorithm. World J Orthop. (2014) 5(5):603. doi: 10.5312/wjo.v5.i5.603
2. Fang T, Zhang EW, Lineaweaver WC, Zhang F. Recipient vessels in the free flap reconstruction around the knee. Ann Plast Surg. (2013) 71(4):429–33. doi: 10.1097/SAP.0b013e31824e5e6e
3. Daigeler A, Drücke D, Tatar K, Homann HH, Goertz O, Tilkorn D, et al. The pedicled gastrocnemius muscle flap: a review of 218 cases. Plast Reconstr Surg. (2009) 123(1):250–7. doi: 10.1097/PRS.0b013e3181904e2e
4. Mitsala G, Varey AH, O’Neill JK, Chapman TW, Khan U. The distally pedicled gracilis flap for salvage of complex knee wounds. Injury. (2014) 45(11):1776–81. doi: 10.1016/j.injury.2014.06.019
5. Clavert P, Cognet J, Baley S, Stussi D, Prevost P, Babin SR, et al. Anatomical basis for distal sartorius muscle flap for reconstructive surgery below the knee. Anatomical study and case report. J Plast Reconstr Aesthet Surg. (2008) 61(1):50–4. doi: 10.1016/j.bjps.2006.01.059
6. Sahasrabudhe P, Panse N, Baheti B, Jadhav A, Joshi N, Chandanwale A. Reconstruction of complex soft-tissue defects around the knee joint with distally based split vastus lateralis musculocutaneous flap: a new technique. J Plast Reconstr Aesthet Surg. (2015) 68(1):35–9. doi: 10.1016/j.bjps.2014.09.034
7. Masquelet A-C, Sassu P. Gastrocnemius flap. In: Cook L, Bassett A, editors. Flaps and reconstructive surgery E-book. Taipei, Taiwan: Chang Gung Memorial Hospital (2009). p. 409.
8. Hyodo I, Nakayama B, Takahashi M, Toriyama K, Kamei Y, Torii S. The gastrocnemius with soleus bi-muscle flap. Br J Plast Surg. (2004) 57(1):77–82. doi: 10.1016/j.bjps.2003.10.008
9. Lamaris GA, Carlisle MP, Durand P, Couto RA, Hendrickson MF. Maximizing the reach of the pedicled gastrocnemius muscle flap: a comparison of 2 surgical approaches. Ann Plast Surg. (2017) 78(3):342–6. doi: 10.1097/SAP.0000000000000796
10. Bibbo C. The gastrocnemius flap for lower extremity reconstruction. Clin Podiatr Med Surg. (2020) 37(4):609–19. doi: 10.1016/j.cpm.2020.07.002
11. Chung YJ, Kim G, Sohn BK. Reconstruction of a lower extremity soft-tissue defect using the gastrocnemius musculoadipofascial flap. Ann Plast Surg. (2002) 49(1):91–5. doi: 10.1097/00000637-200207000-00014
12. Lee C-H, Chang N-JT, Hsiao J-C, Chu Y-Y, Lin C-H, Kao H-K, et al. Extended use of chimeric medial sural artery perforator flap for 3-dimensional defect reconstruction. Ann Plast Surg. (2019) 82(1S):S86–94. doi: 10.1097/SAP.0000000000001697
13. Hallock GG. Chimeric gastrocnemius muscle and sural artery perforator local flap. Ann Plast Surg. (2008) 61(3):306–9. doi: 10.1097/SAP.0b013e31815b2792
Keywords: case reports, plastic surgery procedures, surgical flaps, lower extremity, knee
Citation: Kwon H, Lee S, Kim S, Song SH, Oh S, Kim J, Kyung H, Yang HJ and Ha Y (2023) Reconstruction of complex knee wounds with a distally based gracilis flap and gastrocnemius myocutaneous flap: A case report. Front. Surg. 10:1109936. doi: 10.3389/fsurg.2023.1109936
Received: 28 November 2022; Accepted: 16 January 2023;
Published: 8 February 2023.
Edited by:
Rami Kantar, New York University, United StatesReviewed by:
Andrew Lindford, Helsinki University Central Hospital, Finland© 2023 Kwon, Lee, Kim, Song, Oh, Kim, Kyung, Yang and Ha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yooseok Ha dXNlb2s0dUBuYXZlci5jb20=
†ORCID Hyeokjae Kwon orcid.org/0000-0002-1418-3448 Seokui Lee orcid.org/0000-0002-3319-2286 Sunje Kim orcid.org/0000-0001-7887-7521 Seung Han Song orcid.org/0000-0001-5996-3408 Sang-Ha Oh orcid.org/0000-0003-3734-5005 Joo-hak Kim orcid.org/0000-0001-9244-0940 Hyunwoo Kyung orcid.org/0000-0002-6137-7958 Yooseok Ha orcid.org/0000-0001-7843-5790
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.