
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 16 June 2023
Sec. Orthopedic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1095961
A correction has been applied to this article in:
Corrigendum: Prediction model for tibial plateau fracture combined with meniscus injury
Purpose: To investigate a prediction model of meniscus injury in patients with tibial plateau fracture.
Methods: This retrospective study enrolled patients with tibial plateau fractures who were treated in the Third Hospital of Hebei Medical University from January 1, 2015, to June 30, 2022. Patients were divided into a development cohort and a validation cohort based on the time-lapse validation method. Patients in each cohort were divided into a group with meniscus injury and a group without meniscus injury. Statistical analysis with Student’s t-test for continuous variables and chi square test for categorical variables was performed for patients with and without meniscus injury in the development cohort. Multivariate logistic regression analysis was used to screen the risk factors of tibial plateau combined with meniscal injury, and a clinical prediction model was constructed. Model performance was measured by examining discrimination (Harrell’s C-index), calibration (calibration plots), and utility [decision analysis curves (DCA)]. The model was validated internally using bootstrapping and externally by calculating their performance in a validation cohort.
Results: Five hundred patients (313 [62.6%] males, 187 [37.4%] females) with a mean age of 47.7 ± 13.8 years were eligible and were divided into development (n = 262) and validation (n = 238) cohorts. A total of 284 patients had meniscus injury, including 136 in the development cohort and 148 in the validation cohort We identified high-energy injuries as a risk factor (OR = 1.969, 95%CI 1.131–3.427). Compared with blood type A, patients with blood type B were more likely to experience tibial plateau fracture with meniscus injury (OR = 2.967, 95%CI 1.531–5.748), and office work was a protective factor (OR = 0.279, 95%CI 0.126–0.618). The C-index of the overall survival model was 0.687 (95% CI, 0.623–0.751). Similar C-indices were obtained for external validation [0.700(0.631–0.768)] and internal validation [0.639 (0.638–0.643)]. The model was adequately calibrated and its predictions correlated with the observed outcomes. The DCA curve showed that the model had the best clinical validity when the threshold probability was 0.40 and 0.82.
Conclusions: Patients with blood type B and high-energy injuries are more likely to have meniscal injury. This may help in clinical trial design and individual clinical decision-making.
The meniscus is an important fibrocartilage structure in the knee joint that functions as a lubricant and cushion, minimizing shock, and stress in the joint (1, 2). Tibial plateau fracture is a complex traumatic fracture caused by the stress of external or internal rotation of the tibia, combined with the axial force of knee flexion (3–5). Fractures are often accompanied by meniscal injury, with an incidence of 39%–99% (6). At present, resection is often used to treat meniscal injury, though this reduces the contact area between the meniscus and tibial femur, increases contact pressure, and reduces joint stability. This leads to pain and limitation of knee function, and can even cause articular cartilage degeneration and osteoarthritis (7, 8). Therefore, the integrity of the meniscus structure is important for the function and quality of life in patients with tibial plateau fractures. Therefore, it is crucial for clinical prevention to predict the high-risk population for tibial plateau fractures combined with meniscal injury.
The clinical prediction model, known as the clinical prediction rule or risk score, refers to the use of multifactorial models to predict the probability of having a certain disease or certain future outcome. Nomograms (also known as nomograms) are graphical descriptions of models that estimate the probability of an event occurring for an individual patient (9, 10). The precise prevention and control of diseases is important. In terms of predicting the risk factors of tibial plateau fracture combined with meniscal injury, previous studies have only analyzed the risk factors of tibial plateau fracture or meniscus injury alone (11–13). There are still no models that adequately predict meniscal injuries in patients with tibial plateau fractures.
Therefore, we designed this study to retrospectively collect the data of patients with tibial plateau fractures admitted to the Third Hospital of Hebei Medical University from January 2015 to June 2022. We aimed to describe and analyze the demographic characteristics and preoperative fracture-related factors and develop nomograms to predict the possibility of meniscal injury in these patients. This study provides a reference for clinical diagnosis, treatment, and disease prevention.
The study inclusion criteria were as follows: (i) closed tibial plateau fractures and (ii) complete medical records and imaging data. The exclusion criteria were as follows: (i) pathologic fractures, (ii) old or secondary tibial plateau fractures, (iii) open tibial plateau fractures, and (iv) incomplete data and imaging material.
The clinical data of patients with tibial plateau fractures admitted to the Third Hospital of Hebei Medical University from January 1, 2015, to June 30, 2022, was retrospectively analyzed. Fracture patients admitted between January 2019 and June 2022 were assigned as the development cohort to analyze risk factors for meniscus injury and built a nomogram, and patients admitted between January 2015 and December 2018 were assigned as the validation cohort to evaluate the transportability and generalizability of the model. This epidemiological study was approved by the Institutional Review Board of the Third Hospital of Hebei Medical University (section 2015-002-1) in compliance with the Helsinki Declaration. This was a retrospective study based on historical medical records, and no human participants were included. Written informed consent was not required for participation.
The medical records of enrolled patients were retrieved using a medical record inquiry system. The demographic characteristics of the patients and detailed information on the tibial plateau fractures were recorded. Specifically, collated information included (1) demographic characteristics: sex, age, marital status, occupation, ethnic origin, body mass index (BMI), medical payment method, urbanization, and blood type; (2) injury characteristics: season, holiday, injury mechanism, injury side, AO classification, Schatzker classification, ligament injury, and associated injuries; (3) preoperative complications and preoperative concomitant injuries.
Preoperative and postoperative imaging data were collected using a picture archiving and communication system. x-ray, computed tomography (CT) and magnetic resonance imaging (MRI) scans were performed on all patients with tibial plateau fracture meeting the inclusion and exclusion criteria after admission. X-ray films, CT and MRI scans, and arthroscopy of tibial plateau fractures were reviewed by two orthopaedic surgeons with more than 10 years of experience. Schatzker and AO fracture classification were used to assess the pattern of tibial plateau fractures. If there was any disagreement in the classification of tibial plateau fractures and the diagnosis of meniscus and ligament damage, a final decision was made through discussion, with consensus achieved by the two surgeons.
All 500 patients with tibial plateau fractures underwent surgical treatment. The patients with Schatzker type I split of the lateral tibial plateau was treated with prepatellar clamp reduction and plate screw fixation. Type Ⅱ and Ⅲ split of the lateral tibial plateau combined with collapse and simple collapse fracture were treated with Kirschner wire pry reduction, arthroscopic reduction and plate screw fixation, or balloon distraction and bone cement fixation. For type Ⅳ medial tibial plateau fracture, the anterior patellar clamp was used for reduction, Kirschner wire pry for reduction, and medial plate screw fixation. For type Ⅴ and Ⅵ bilateral tibial plateau fractures, the collapsed bone was reduced by incised Kirschner wire pry, the width of the tibial plateau was restored by prepatellar forceps, and bilateral plate screws were used for fixation. In addition to fracture reduction and fixation, we performed arthroscopy during the operation. On the one hand, we observed whether the reduction quality was satisfactory. At the same time, we explored whether the anterior and posterior cruciate ligaments and meniscus were damaged or torn. and intraoperative arthroscopy was performed to observe whether the reduction quality was satisfactory and whether there were anterior and posterior cruciate ligaments and meniscus injuries.
Statistical analyses were performed using R4.1.0 (R Foundation for Statistical Computing, Austria). Statistical significance was set at P < 0.05. Descriptive statistics were reported as frequencies and proportions, cause the collected factors were all categorical variable. Differences in the constituent ratios of baseline comparison of tibial plateau fractures between the development and validation cohorts were tested using the chi squared (χ2) test or Fisher’s exact probability method. Model building used univariate analysis to analyze the 53 variables. Variables with P < 0.05 were selected and included in multivariate logistic regression for further analysis to obtain the independent influencing factors related to tibial plateau fracture combined with meniscal injury and a nomogram plot were established. Logistic regression analyses were used to estimate the odds ratios (OR) and their 95% confidence intervals (CIs) or P-values. Model performance was evaluated by examining discrimination (C-index), calibration (calibration plots and H-L goodness of fit test), and utility [decision analysis curves (DCA)].
The model validation was performed in two steps. First, we performed an internal validation using a bootstrap resampling process to provide an unbiased estimate of model performance, using the C-index (validated package in R) and calibration plot (calibrate package in R). The original development cohort was resampled to obtain a dataset with the same size. Second, to assess external validity, the prediction accuracy of the model was determined in the validation cohort by computing the C-indices, calibration plots, and H-L goodness of fit test. The clinical effectiveness was evaluated in the validation cohort using the DCA curve, and the net clinical benefit of the model was obtained.
A total of 500 patients diagnosed with tibial plateau fracture, 313 males (62.6%) and 187 females (37.4%) with an average age of 47.7 ± 13.8 years (range, 14–89 years) met the eligibility criteria (Figure 1). Before the age of 60 years, male patients accounted for the majority of tibial plateau fractures, with men aged 30–39 years old accounting for the largest proportion (86.0%). After 60 years of age, most tibial plateau fracture patients were female, and 66.3% of them were aged 60–69 years old (χ2 = 68.285, P < 0.01). There were 284 (56.8%) cases of tibial plateau fracture complicated by meniscal injury and 216 (43.2%) cases without meniscus injury. There were 84 cases (16.8%) with ligament injury, including 61 cases (72.6%) with anterior forks ligament injury, 21 cases (25.0%) with posterior forks ligament injury, and 2 cases (2.4%) with anterior forks ligament and posterior forks ligament injuries. According to the AO classification, 306 (61.8%) cases were type B fractures and 189 (38.2%) were type C fractures. According to the Schatzker classification, type II fractures were the most common (214 cases, 42.8%), followed by types VI (112, 22.4%), V (73, 14.6%), IV (56, 11.2%), III (40, 8.0%), and I (5, 1.0%). Among the 500 patients with tibial plateau fractures, the majority were overweight (266 cases, 53.2%), followed by obese (125 cases, 25.0%), normal weight (105 cases, 21.0%), and underweight (4 cases, 0.8%). The medical insurance group comprised the majority of patients (491 cases, 98.2%), and most patients were married (462 cases, 93.4%). Moreover, most of the patients were diagnosed in spring (150 cases, 30.0%), followed by winter (124 cases, 24.8%), autumn (120 cases, 24.0%), and summer (106 cases, 21.2%). Most patients were of Han nationality (488 cases, 97.6%), and from rural areas (306 cases, 61.2%). Blood type B was predominant (162 cases, 32.4%), followed by blood type A (142 cases, 28.4%), type O (139 cases, 27.8%), and type AB (57 cases, 11.4%). Hypertension was the most common preoperative complication (104 patients, 20.8%). The comparison results of the baseline data between the development and validation cohorts are shown in Table 1.
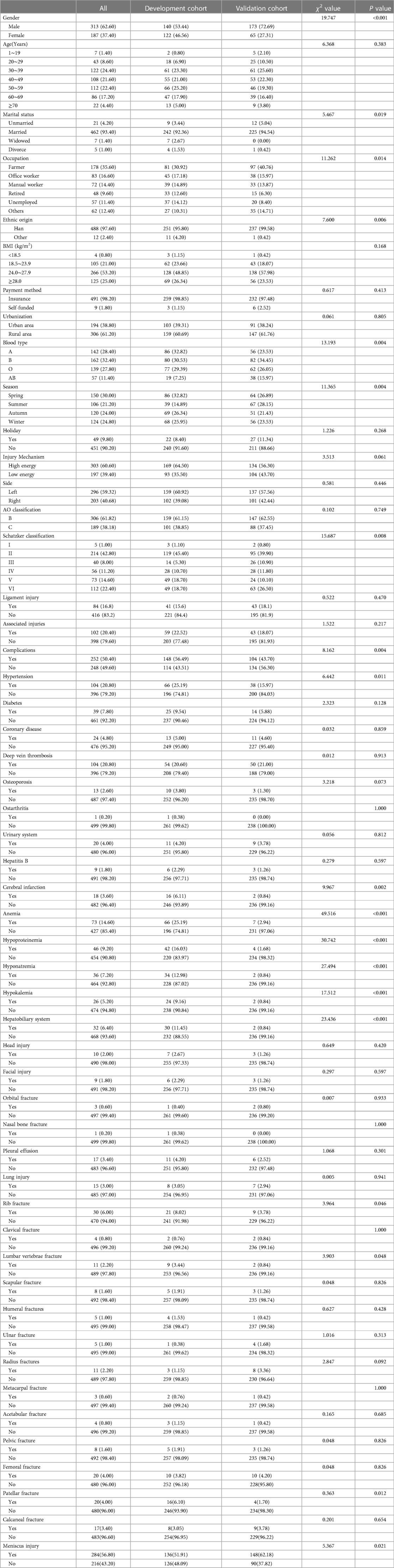
Table 1. Baseline comparison of tibial plateau fracture between development and validation cohort [n (%)].
Univariate analysis of the model building population showed that compared with the tibial plateau fracture patients without meniscus injury, the proportion of patients with meniscus injury who were farmers and workers, high-energy injury, and blood type B and blood type AB were higher (P < 0.05, Table 2). These factors were included in the multivariate logistic regression analysis.
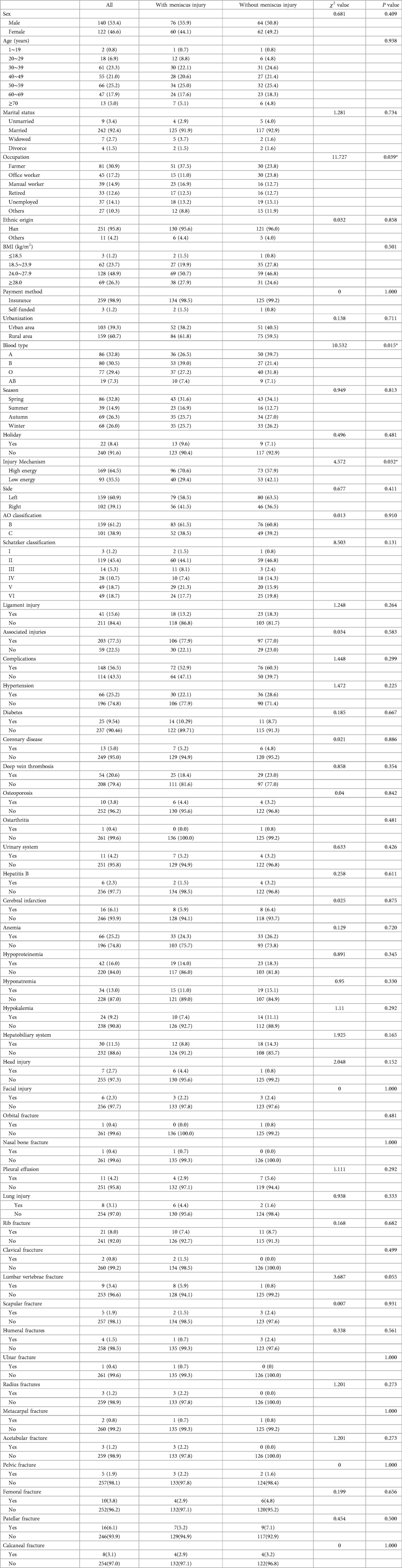
Table 2. Results of univariate analysis of tibial plateau fracture in development cohort [case (%)].
Multivariate analysis showed that high-energy injury (OR = 1.969, 95%CI:1.131–3.427) was a risk factor for tibial plateau fracture combined with meniscal injury. Compared with blood type A, blood type B was a risk factor (OR = 2.967, 95%CI:1.531–5.748). Compared to farmers, office staff occupation was a protective factor (OR = 0.279, 95%CI:0.126–0.618) (Table 3).
According to the ROC curve, the C-index of the model was 0.687 (95%CI:0.623–0.751), and the best cut-off value was 0.572. The specificity and sensitivity were 0.794 and 0.522, respectively (Figure 2). The C-index of the external validation cohort was 0.700 (95%CI:0.631–0.768), and the optimal cut-off value was 0.528. The specificity and sensitivity were 0.667 and 0.669, respectively (Figure 3), and the C-index of the internal validation cohort was 0.639 (0.638–0.643).
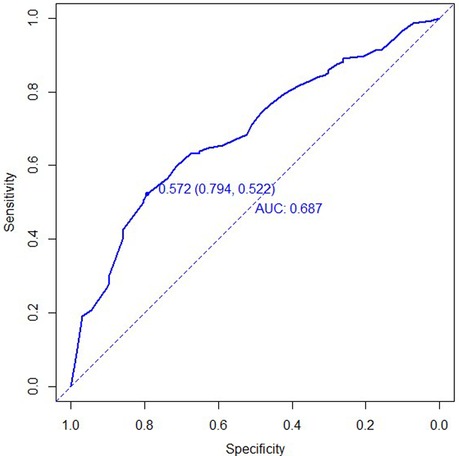
Figure 2. ROC curve for development cohort of tibial plateau fracture combined with meniscus injury.
In the calibration figures for the modeling, internal validation, and external validation groups, the prediction curve fitted the reference line well, indicating that the risk predicted by the model was consistent with the actual risk of meniscal injury. The H-L test results of the development and validation cohorts were P = 0.120 (χ2 = 14.074) and P = 0.216 (χ2 = 11.961), respectively, indicating that the model had good predictive ability and a high level of calibration (Figures 4–6).
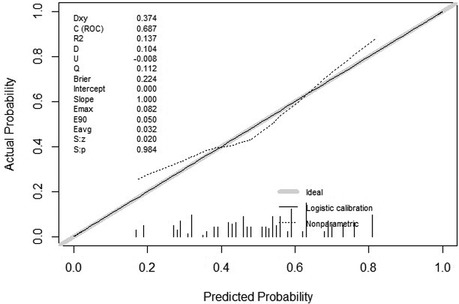
Figure 4. Calibration curve for development cohort of tibial plateau fracture combined with meniscus injury.
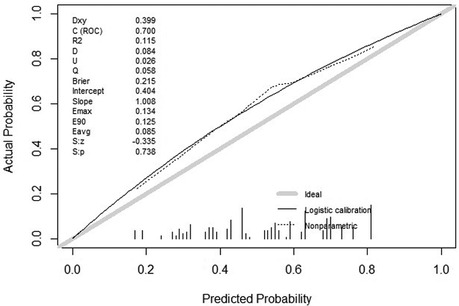
Figure 5. Calibration curve for external validation cohort of tibial plateau fracture combined with meniscus injury.
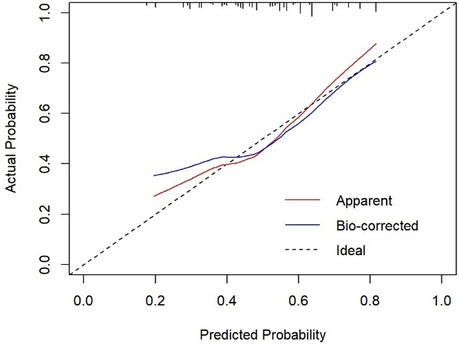
Figure 6. Calibration curve for internal validation cohort of tibial plateau fracture combined with meniscus injury.
According to the DCA curve in the development group, the clinical effectiveness is best and the treatment has a higher net benefit, when the threshold probability is in the range of 0.40 to 0.82 (Figures 7, 8).
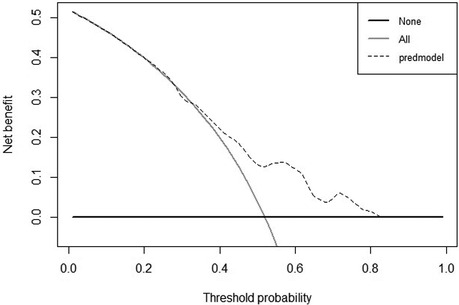
Figure 7. DCA curve for development cohort of tibial plateau fracture combined with meniscus injury.
The “lrm” function in the Rms package of R language was used to establish the Logistic regression model with the above three factors. The “Plot” function was used to further draw the nomogram, and the results of the clinical prediction model were visualized (Figure 9). A nomogram can be used to determine the risk of tibial plateau fracture combined with meniscal injury, according to the relevant variables of individuals in practice.
For example, a worker with blood type B suffered a tibial plateau fracture in the spring when he fell from a scaffolding that was 3 m high. The corresponding score was obtained on the nomogram based on the values of each factor. When the scores for each factor were summed, the risk of meniscal injury in this patient was 0.765.
Tibial plateau fracture combined with meniscal injury can cause serious damage to knee joint function. At present, meniscal injury is usually judged by knee MRI, which has a certain false-positive rate (14). Therefore, it is critical to take preventive measures against risk factors and high-risk groups that may develop meniscal injury. In this study, we developed and validated a clinical model to predict the risk of meniscal injury in patients with tibial plateau fractures. Through univariate and multivariate analyses, we included the selected variables in the model, and the model evaluation showed good discrimination, calibration, and clinical validity. According to the nomogram, occupation was the most important predictor, followed by blood type and injury mechanism.
In the current study, when compared with farmers, being office workers was a protective factor for tibial plateau fracture combined with meniscus injury. This may be related to the lower daily exercise and lower activity levels of office workers. This finding is similar to those of previous studies that showed that excess exercise is a known risk factor for meniscal injury (15, 16). Repeated bending and crouching can cause frequent compression and friction of the meniscus, resulting in minor trauma. When the long-term injury accumulation exceeds the physiological capacity, the meniscus will undergo pathological changes in tissue composition and structure, and even tears, which will affect function (17, 18). Office workers work does not involve heavy physical strength and endurance activities, as such there is less joint wear, and a lower incidence of meniscus injury. Conversely, farmers work involves heavy physical labor, endurance activities, and often the need to carry out activities which strain the knee joint such as squatting or weightlifting. Such activities can easily cause acute or chronic meniscus injury. Some studies have found that compared with the general population, the activity levels of farmers, professional athletes, and soldiers are significantly higher, and the incidence of meniscus injury is also markedly increased (19, 20). In addition to the lower level of activity, the higher level of education and income of the office workers may be another factor. Education level is closely related to health literacy. Typically, the higher the education level, the better the economic condition, higher the health literacy, and healthier the lifestyle and behavior (21, 22). The average education level and per capita disposable income of office workers was higher than those of farmers. Moreover, office workers are more likely to perform reasonable exercises in their daily life and pay attention to the protection of the knee joints, thus lowering the incidence of meniscal injury. These findings are similar to those of previous studies. Lee (23) found that the incidence of knee osteoarthritis was higher in people with low income, low education level, non-management jobs or unemployed. Moreover, the study showed the correlation between low education level and knee osteoarthritis was the strongest.
The findings from this study showed that tibial plateau fracture patients with blood type B were more likely to have meniscal injury complications than those with blood type A. The relationship between blood type and the prognosis of cardiovascular disease and cancer has been well established (24–28). However, a direct link between blood type and meniscal injury has not been proven. These findings are similar to those of previous studies that showed that ABO blood type is associated with personality characteristics. People with blood type B tend to be enthusiastic, active and explorative (29, 30). Daily activities are frequent, and they prefer short-range, medium-high-intensity exercise, which results in repeated flexion and extension of the knee joint over a prolonged time, frequent stimulation, and excessive load on the meniscus. Therefore, blood type may affect individual behavior by influencing personality which subsequently affects tibial plateau fracture combined with meniscal injury, this is consistent with the results of this study.
Another issue elucidated in this study was that patients with tibial plateau fractures with high-energy injuries are more likely to have meniscal injuries than those with low-energy injuries. High energy injury refers to the injury caused by falling from a height >1 m, the strong impact and extrusion of electric vehicles or motor vehicles, etc (31). When the human body is impacted, the cushioning effect of the meniscus can reduce the impact force on the articular surface and subsequent body injury. When falling from a height, in order to share the pressure on the femur, the meniscus bares a huge load, resulting in serious deformation of the meniscus and easily causing a crush injury. When there is a traffic accident, the knee joint often experiences excessive flexion or joint torsion, resulting in meniscal tear injury (4). Chen (32) reported that traffic accidents were the main cause of posterior cruciate ligament injuries, particularly motorcycle accidents. Ligament injuries are also associated with meniscal tears. However, Shamrock (33) found that the mechanism of high-energy injury was associated with increased cartilage injury rates, but not with meniscal injury rate.
Other factors for tibial plateau fracture combined with meniscal injury were also identified in the different subgroups during the current study. Many studies have shown that a high BMI is a known risk factor for degenerative meniscal injury, and most of the people in this study had high-energy injuries. Therefore, it was concluded that BMI is not a risk factor for tibial plateau combined with meniscal injury. Furthermore, in this study it was found that tibial plateau fracture classification is not related to meniscal injury, a finding that is consistent with other investigations showing that there was no difference in the distribution of meniscal injuries among different types of tibial plateau fractures (34–36). Moreover, results showed age was not a risk factor for tibial plateau combined with meniscal injury, and with increasing age, the meniscus undergoes degenerative changes, which can be damaged by a slight impact (37–39). On the other hand, young people engage in more vigorous sports which include bouncing, twisting, and collision motions, thus increasing the risk of meniscus injury (40, 41). This study concluded that sex and ligament injury were not risk factors for tibial plateau combined with meniscal injury, which is consistent with the results of many existing studies (42–44).
There are some limitations in this study. Firstly, it is a retrospective study with certain information bias. Secondly, fracture data from one hospital is unrepresentative, Thirdly, the data of fracture patients in 2022 in the development cohort only included patient data from January to June, resulting in a difference between the time range and the validation cohort. The relationship between time factors and complications of meniscal injury may be biased. As such, further large-sample, multicenter prospective studies are needed to increase the time and space range of data acquisition to obtain a more comprehensive and accurate data basis.
Farmer occupation, blood type B and high-energy injuries are independent risk factors for tibial plateau fracture complicated with meniscal injury. Based on this, a clinical prediction model was established and evaluated. This model can be used to predict the menisci of patients with tibial plateau fractures. This can provide guidance for orthopaedic surgeons to make targeted preoperative examinations and surgical plans.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
YZ and JW designed this study. HL, WL, YW and WC prepared the manuscript. Data were collected by XY and WY Data was analyzed and interpreted by HL, WL and YW. The revision of the article was done by ZH. All authors contributed to the article and approved the submitted version.
This study was supported by the Key R&D project of Hebei Province (20377780D), Hebei Province Medical Science Research Project (20210552), and Natural Science Foundation of Hebei Province (H2021206317).
The authors wish to thank ZZ and XL, Orthopedic surgeons, XZ, epidemiologist, for their assistance and cooperation in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. (1975) 109:184–92. doi: 10.1097/00003086-197506000-00027
2. Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. (1980) 149:283–90. doi: 10.1097/00003086-198006000-00039
3. Deng X, Hu H, Wang Y, Shao D, Zhang Y. Arthroscopically assisted evaluation of frequency and patterns of meniscal tears in operative tibial plateau fractures: a retrospective study. J Orthop Surg Res. 2021;16(1):117. doi: 10.1186/s13018-021-02265-0
4. McDermott ID. (Ii) meniscal tears. Curr Orthop. (2006) 20(2):85–94. doi: 10.1016/j.cuor.2006.02.010
5. Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S, et al. Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res. (2019) 105(1):107–11. doi: 10.1016/j.otsr.2018.10.001
6. Chang H, Zheng Z, Shao D, Yu Y, Hou Z, Zhang Y. Incidence and radiological predictors of concomitant meniscal and cruciate ligament injuries in operative tibial plateau fractures: a prospective diagnostic study. Sci Rep. 2018;8(1):13317. doi: 10.1038/s41598-018-31705-x
7. Koh JL, Zimmerman TA, Patel S, Ren Y, Xu D, Zhang LQ. Tibiofemoral contact mechanics with horizontal cleavage tears and treatment of the lateral Meniscus in the human knee: an in vitro cadaver study. Clin Orthop Relat Res. (2018) 476(11):2262–70. doi: 10.1097/CORR.0000000000000464
8. Logan CA, Aman ZS, Kemler BR, Storaci HW, Dornan GJ, LaPrade RF. Influence of medial meniscus bucket-handle repair in setting of anterior cruciate ligament reconstruction on tibiofemoral contact mechanics: a biomechanical study. Arthroscopy. (2019) 35(8):2412–20. doi: 10.1016/j.arthro
9. Moons KG, Altman DG, Reitsma JB, Ioannidis JP, Macaskill P, Steyerberg EW, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. (2015) 162(1):W1–73. doi: 10.7326/M14-0698
10. Ranstam J, Cook JA, Collins GS. Clinical prediction models. Br J Surg. (2016) 103(13):1886. doi: 10.1002/bjs.10242
11. Chen G, Tang X, Li Q, Zheng G, Yang T, Li J. The evaluation of patient-specific factors associated with meniscal and chondral injuries accompanying ACL rupture in young adult patients. Knee Surg Sports Traumatol Arthrosc. (2015) 23(3):792–8. doi: 10.1007/s00167-013-2718-2
12. Tomihara T, Hashimoto Y, Takahashi S, Taniuchi M, Takigami J, Okazaki S, et al. Risk factors related to the presence of meniscal injury and irreparable meniscal tear at primary anterior cruciate ligament reconstruction. Orthop J Sports Med. (2021) 9(3):2325967121989036. doi: 10.1177/2325967121989036
13. Li W, Liang J, Zeng F, Lin B, Liu C, Huang S, et al. Anatomic characteristics of the knee influence the risk of suffering an isolated meniscal injury and the risk factors differ between women and men. Knee Surg Sports Traumatol Arthrosc. (2021) 29(11):3751–62. doi: 10.1007/s00167-020-06396-5
14. Khan K, Azzopardi E, Camilleri L, Azzopardi EA, Bragg TH. Value of clinical, ultrasonographic and MRI signs as diagnostic differentiators of non-benign lipomatous tumours. Sci Rep. (2020) 10(1):20756. doi: 10.1038/s41598-020-77244-2
15. Logerstedt DS, Ebert JR, MacLeod TD, Heiderscheit BC, Gabbett TJ, Eckenrode BJ. Effects of and response to mechanical loading on the knee. Sports Med. (2022) 52(2):201–35. doi: 10.1007/s40279-021-01579-7
16. Thorlund JB, Juhl CB, Ingelsrud LH, Skou ST. Risk factors, diagnosis and non-surgical treatment for meniscal tears: evidence and recommendations: a statement paper commissioned by the danish society of sports physical therapy (DSSF). Br J Sports Med. (2018) 52(9):557–65. doi: 10.1136/bjsports-2017-098429
17. Sherman SL, DiPaolo ZJ, Ray TE, Sachs BM, Oladeji LO. Meniscus injuries: a review of rehabilitation and return to play. Clin Sports Med. (2020) 39(1):165–83. doi: 10.1016/j.csm.2019.08.004.3
18. Zhou T. Analysis of the biomechanical characteristics of the knee joint with a meniscus injury. Healthc Technol Lett. (2018);5(6):247–9. doi: 10.1049/htl.2018.5048
19. Adams BG, Houston MN, Cameron KL. The epidemiology of Meniscus injury. Sports Med Arthrosc Rev. (2021) 29(3):e24–33. doi: 10.1097/JSA.0000000000000329
20. Donohue MA, Zhou L, Haley CA. Meniscus injuries in the military athlete. J Knee Surg. (2019) 32(2):123–6. doi: 10.1055/s-0038-1676959
21. Pigeyre M, Rousseaux J, Trouiller P, Dumont J, Goumidi L, Bonte D, et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes (Lond). 2016;40(11):1794–801. doi: 10.1038/ijo.2016.109
22. Delley M, Brunner TA. Breakfast eating patterns and drivers of a healthy breakfast composition. Appetite. (2019) 137:90–8. doi: 10.1016/j.appet.2019.02.006
23. Lee JY, Han K, Park YG, Park SH. Effects of education, income, and occupation on prevalence and symptoms of knee osteoarthritis. Sci Rep. 2021;11(1):13983. doi: 10.1038/s41598-021-93394-3
24. Groot HE, Villegas Sierra LE, Said MA, Lipsic E, Karper JC, van der Harst P. Genetically determined ABO blood group and its associations with health and disease. Arterioscler Thromb Vasc Biol. (2020) 40(3):830–8. doi: 10.1161/ATVBAHA.119.313658
25. Zakai NA, Judd SE, Alexander K, McClure LA, Kissela BM, Howard G, et al. ABO Blood type and stroke risk: the reasons for geographic and racial differences in stroke study. J Thromb Haemost. (2014) 12(4):564–70. doi: 10.1111/jth.12507
26. Huang JY, Wang R, Gao YT, Yuan JM. ABO Blood type and the risk of cancer—findings from the Shanghai cohort study. PLoS One. 2017;12(9):e0184295. doi: 10.1371/journal.pone.0184295
27. Tanaka Y, Kumagi T, Terao T, Kuroda T, Yokota T, Azemoto N, et al. ABO blood type and the long-term outcomes of pancreatic cancer. Intern Med. (2020) 59(6):761–8. doi: 10.2169/internalmedicine.3748-19
28. Qiu MZ, Zhang DS, Ruan DY, Luo HY, Wang ZQ, Zhou ZW, et al. A relationship between ABO blood groups and clinicopathologic characteristics of patients with gastric adenocarcinoma in China. Med Oncol. (2011) 28(Suppl 1):S268–73. doi: 10.1007/s12032-010-9735-5
29. Tsuchimine S, Saruwatari J, Kaneda A, Yasui-Furukori N. ABO Blood type and personality traits in healthy Japanese subjects. PLoS One. 2015;10(5):e0126983. doi: 10.1371/journal.pone.0126983
30. Furukawa T. A study of temperament by means of human blood groups. Jpn J Psychol. (1927) 2:612–34. doi: 10.4992/jjpsy.2.612
31. Lv H, Zhang Q, Yin Y, Zhu Y, Wang J, Hou Z, et al. Epidemiologic characteristics of traumatic fractures during the outbreak of coronavirus disease 2019 (COVID-19) in China: a retrospective & comparative multi-center study. Injury. (2020) 51(8):1698–704. doi: 10.1016/j.injury.2020.06.022
32. Chen G, Fu WL, Tang X, Li Q, Li J. Clinical epidemiological analysis on posterior cruciate ligament injuries. Zhongguo Gu Shang. (2015) 28(7):638–42. Chinese. https://europepmc.org/article/MED/2639910726399107
33. Shamrock AG, Hall JR, Hajewski CJ, An Q, Duchman KR. Cartilage and Meniscus injuries are more common in patients undergoing delayed multiligament reconstruction. J Knee Surg. (2022) 35(5):560–5. doi: 10.1055/s-0040-1716378
34. Deng X, Hu H, Wang Y, Shao D, Zhang Y. Arthroscopically assisted evaluation of frequency and patterns of meniscal tears in operative tibial plateau fractures: a retrospective study. J Orthop Surg Res. (2021) 16(1):117. doi: 10.1186/s13018-021-02265-0
35. Mustonen AO, Koivikko MP, Lindahl J, Koskinen SK. MRI Of acute meniscal injury associated with tibial plateau fractures: prevalence, type, and location. AJR Am J Roentgenol. (2008) 191(4):1002–9. doi: 10.2214/AJR.07.3811
36. Yan B, Sun J, Yin W. The prevalence of soft tissue injuries in operative schatzker type IV tibial plateau fractures. Arch Orthop Trauma Surg. (2021) 141(8):1269–75. doi: 10.1007/s00402-020-03533-0
37. Park DY, Min BH, Choi BH, Kim YJ, Kim M, Suh-Kim H, et al. The degeneration of Meniscus roots is accompanied by fibrocartilage formation, which may precede Meniscus root tears in osteoarthritic knees. Am J Sports Med. (2015) 43(12):3034–44. doi: 10.1177/0363546515605086
38. Levillain A, Boulocher C, Kaderli S, Viguier E, Hannouche D, Hoc T, et al. Meniscal biomechanical alterations in an ACLT rabbit model of early osteoarthritis. Osteoarthritis Cartilage. (2015) 23(7):1186–93. doi: 10.1016/j.joca.2015.02.022
39. Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. (2013) 43(6):352–67. doi: 10.2519/jospt.2013.4295
40. Jackson T, Fabricant PD, Beck N, Storey E, Patel NM, Ganley TJ. Epidemiology, injury patterns, and treatment of meniscal tears in pediatric patients: a 16-year experience of a single center. Orthop J Sports Med. (2019) 7(12):2325967119890325. doi: 10.1177/2325967119890325
41. Jr EH, Wise K, LaMont L, Copley L, Wilson P. Prevalence of discoid Meniscus during arthroscopy for isolated lateral meniscal pathology in the pediatric population. J Pediatr Orthop. (2017) 37(4):285–92. doi: 10.1097/BPO.0000000000000630
42. Chang H, Zheng Z, Shao D, Yu Y, Hou Z, Zhang Y. Incidence and radiological predictors of concomitant meniscal and cruciate ligament injuries in operative tibial plateau fractures: a prospective diagnostic Study. Sci Rep. (2018) 8(1):13317. doi: 10.1038/s41598-018-31705-x.30190502
43. Kontio T, Heliövaara M, Rissanen H, Knekt P, Aromaa A, Solovieva S. Risk factors for first hospitalization due to meniscal lesions—a population-based cohort study with 30 years of follow-up. BMC Musculoskelet Disord. (2017) 18(1):528. doi: 10.1186/s12891-017-1886-5.29237499
Keywords: tibial plateau fracture, meniscus injury, risk factors, prediction model, nomogram
Citation: Lv H, Li W, Wang Y, Chen W, Yan X, Yuwen P, Hou Z, Wang J and Zhang Y (2023) Prediction model for tibial plateau fracture combined with meniscus injury. Front. Surg. 10:1095961. doi: 10.3389/fsurg.2023.1095961
Received: 11 November 2022; Accepted: 5 June 2023;
Published: 16 June 2023.
Edited by:
Raffaele Vitiello, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Lu Jun, Southeast University, China© 2023 Lv, Li, Wang, Chen, Yan, Yuwen, Hou, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingze Zhang, ZHJ5enpoYW5nQDEyNi5jb20=; Juan Wang, ODQxMzM3MTlAcXEuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.