- 1The First Department of Urology, The First Affiliated Hospital of Kunming Medical University, Kunming, China
- 2Department of Obstetrics, The First Affiliated Hospital of Kunming Medical University, Kunming, China
Uterine leiomyomas, also known as uterine fibroids, are the most common benign tumors found in the female reproductive system. Transvaginal prolapsed submucosal leiomyomas are a rare complication of uterine fibroids during the postpartum period. Due to the lack of sufficient published evidence on these rare complications and their uncommon appearance, they often result in diagnostic and treatment difficulties for clinicians. This case report presents a primigravida with no special prenatal examination developed recurrent high fever and bacteremia following an emergency cesarean section. On the 20th day after delivery, a vaginal prolapsed mass was observed, which was initially misdiagnosed as bladder prolapse before being corrected to a diagnosis of vaginal prolapse of submucosal uterine leiomyoma. This patient was able to retain fertility by prompt use of powerful antibiotics and transvaginal myomectomy rather than undergoing a hysterectomy. For parturient women with hysteromyoma and recurrent fever after delivery where the source of infection cannot be found, the infection of the submucous leiomyoma of the uterus should be highly suspected. It can be helpful to perform an imaging examination to diagnose a disease, and transvaginal myomectomy should be the first choice for treating prolapsed leiomyoma in cases with no obvious blood supply or if pedicle can be achieved.
Introduction
Leiomyomas, or uterine fibroids, are commonly occurring benign tumors that can be found in the female reproductive system (1). Approximately 10%–30% of pregnant women experience fibroid-related complications (2), such as spontaneous abortion, preterm labor, soft tissue dystocia, uterine inertia, fetopelvic disproportion, fetal malposition, and postpartum hemorrhage (3). Transvaginal prolapsed submucosal leiomyoma, a rare complication among postpartum women, can be difficult for clinicians to diagnose and treat. This case report describes the successful treatment of a postpartum submucosal leiomyoma of the uterus with the vaginal prolapse of a Chinese puerpera (a woman who has recently given birth). It describes the detailed diagnosis and successful treatment process without a hysterectomy.
Case presentation
The patient, a 24-year-old woman, was referred to our hospital from a subordinate hospital with a persistent, recurrent high fever for 20 days and a prolapsed vaginal mass for 1 day after delivery. At admission, her body temperature was 38.7°C. She had filthy, smelly lochia and a soft, hyperemic, edematous, bag-like excrescence in her vulva (Figure 1), which could be self-repaired and had a diameter of approximately 4 cm.

Figure 1. Prolapse day 1. A soft, hyperemia, edema, and bag-like excrescence was observed in the patient’s vulva, which could be self-repaired with a diameter of approximately 4 cm.
History: The patient, a gravida 1, para 1, had no special findings during the prenatal examination, including ultrasonic examination. At 40 weeks + 5 days of gestation, she delivered a healthy baby boy weighing 3,300 g via emergency cesarean section in a local hospital due to persistent occipital posterior position. While delivering the child, difficulties were encountered in removing the fetal head by hand, resulting in a tear on the left side of the lower segment of the uterus to the external orifice of the cervix. An intramural leiomyoma with a diameter of about 1.5 cm was found around the incision on the anterior wall of the uterus, and a myomectomy was performed. Following the operation, the patient developed a recurrent fever, with the highest temperature of 39.8°C. Her white blood cell count was 21.56 × 109, and the percentage of neutrophils was 85%. Blood culture, urine culture, and vaginal discharge culture all indicated multiple drug resistance to Escherichia coli. Based on the drug sensitivity results, it was decided to replace the antibiotics with meropenem 1 g Q8H + metronidazole 0.5 g Q8H + azithromycin 0.5 g QD. During treatment, the patient's peak temperature decreased. At 20 days postpartum, a fleshy tissue emerged from the vagina as the patient was squatting. An ultrasound examination at the local hospital suggested that the tissue may be prolapsed bladder, and the patient was immediately transferred to our hospital. Upon admission, considering the patient's serious infection and the multiple drug resistance to E. coli, she was treated with the antibiotic solution of meropenem 1 g Q8H + doxycycline 0.1 g Q12H.
On the second day after the prolapse of the vaginal orifice, the tissue on the surface of the mass had necrotized and exfoliated, accompanied by a stench. To avoid worsening infection caused by ischemic necrosis of the prolapsed “bladder,” the mass was cleaned and disinfected daily before being lubricated with paraffin oil and gently inserted into the vagina. B-ultrasound indicated a strong echo with sound shadow in the intrauterine cavity (indicative of pus formation).
On the fifth day after the prolapse, the mass became flaky and gradually darkened due to ischemia (Figure 2). The validity of the bladder prolapse diagnosis was questioned, requiring a multidisciplinary consultation given the patient's absence of dysuria and urine retention. T2-weighted magnetic resonance imaging (MRI) images of the pelvis showed uneven signals in the myometrium of the uterus, moderately lower signal mass near the bottom of the posterior wall of the uterus, no diffusion limitation in diffusion-weighted imaging (DWI), marginally unbalanced lower signal in the intrauterine, scattered gas signal, and slightly uneven lower signal in the vagina connected with the intrauterine signal (Figure 3A). Dynamically enhanced sagittal T1-weighted images of the pelvis showed no enhancement of the intrauterine and vaginal signal (Figure 3B). At this stage, bladder prolapse had been ruled out, and the patient was first diagnosed with a prolapsed submucosal fibroid. Once the diagnosis was confirmed, transvaginal resection of the protuberant was performed with the assistance of an obstetrician.
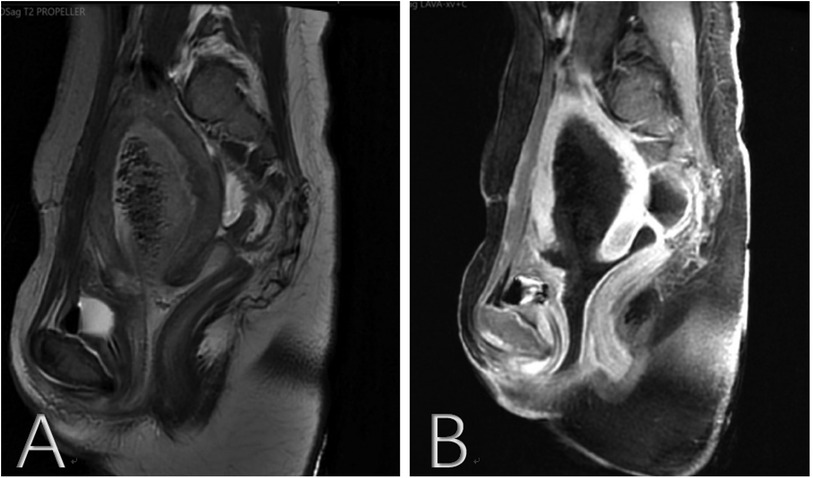
Figure 3. (A) T2-weighted MRI images of the pelvis found uneven signals in the myometrium of the uterus, slightly lower signal mass near the bottom of the posterior wall of the uterus, no diffusion limitation in DWI, slightly uneven lower signal in the intrauterine, scattered gas signal, and slightly uneven lower signal in the vagina connected with the intrauterine signal. (B) Dynamically enhanced sagittal T1-weighted images of the pelvis found no enhancement of the intrauterine and vaginal signals. MRI, magnetic resonance imaging; DWI, diffusion-weighted imaging.
Operation process: The patient had a 16F urethral catheter removed under general anesthesia. Upon examination, the uterus was observed to be intact and large, consistent with the size of the uterus 30 days after delivery. Exploration revealed an irregular, prolapsed vegetation, approximately 18 cm long, 10 cm wide, and 4 cm thick, originating from the uterine cavity. The cervical edge could be touched with careful palpation. The irregular vegetation was gripped and pulled hard by oval pliers using vaginal retractors to expose the field of vision, and the pedicle of the vegetation was found to be deep and strong. A transabdominal ultrasound showed the vegetation to be connected to the fundus uteri. The vegetation was excised completely as far as possible and divided into irregular tissue pieces during the operation (Figure 4). An old laceration up to the vaginal fornix on the right part of the cervix was sutured using 2-0 absorbable sutures.

Figure 4. Complete excision of the vegetation was removed as far as possible and divided into several pieces of irregular tissue during the operation.
Histopathologic examination found a braided arrangement of muscular tissue with complete coagulation necrosis, which confirmed the diagnosis of leiomyoma with coagulation necrosis.
Literature review
The PubMed database was searched using MeSH terms including “submucosal fibroids,” “submucosal leiomyoma,” “submucous leiomyoma,” “submucous myoma,” “postpartum,” “after delivery,” or “caesarean” from January 1945 to November 2021. Each article abstract was evaluated, and the relevant original English language articles were read. Relevant articles were cross-referenced to identify related studies or publications on the subject, and cases of transvaginal prolapse of uterine submucous myoma or cervical myoma after delivery since 1949 were summarized (1, 3–13) (Table 1). The literature review found that transvaginal prolapse of postpartum submucosal fibroids occurred from immediate postpartum to seven weeks postpartum, with 7 of the 14 cases occurring at 4–5 weeks postpartum. Regarding symptoms, 12 of the 14 cases had a postpartum fever or spasmodic abdominal pain. Additionally, some patients experienced vaginal bleeding and malodorous vaginal secretions, and a few experienced urinary retention and urethrovaginal fistulas. The prolapsed fibroids were mostly pedicled, soft, and irregular. The location of their pedicles was found to be distributed in all uterine walls, but most were around the cervical canal and fundus. Transvaginal myomectomy was the most common surgical method, but some patients had to undergo transvaginal/transabdominal hysterectomy as a result of incomplete resections or serious complications. In both patients and infants, postoperative outcomes were positive, with no deaths reported.
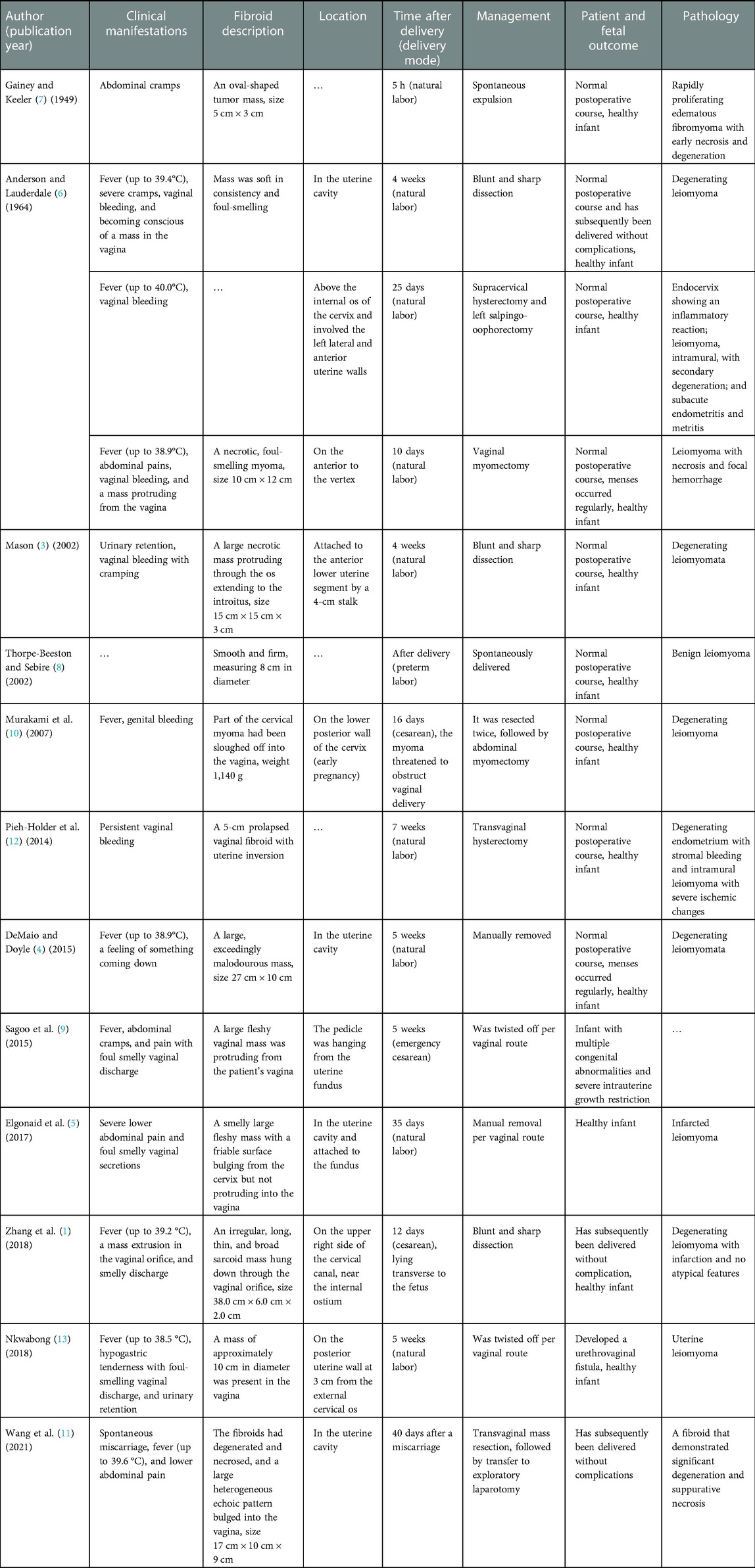
Table 1. Summary of the cases with transvaginal prolapse of uterine submucous myoma or cervical myoma after delivery since 1949.
Discussion
It is estimated that uterine leiomyomas occur in 20%–40% of women during their reproductive years (14). During pregnancy, women with uterine fibroids have a higher risk of preterm delivery, placenta previa, postpartum hemorrhage, and cesarean section compared to those without uterine fibroids (15). Furthermore, due to the rarity of the complication of myoma transvaginal prolapse, diagnostic difficulties or misdiagnosis can occur if an insufficient auxiliary examination is performed. In this case, large uterine fibroids were not discovered by B-ultrasonography during regular labor examination, which could be related to edema and the softening of fibroids.
There are four major reasons for the initial misdiagnosis of bladder prolapse in this case. First, the clinical manifestations of the patient—the prolapsed mass being slightly smooth and pouch-like—make it difficult to distinguish from a prolapsed bladder based on appearance. Second, this disease is rare and clinicians had not previously encountered similar cases, resulting in misdiagnosis. Third, as the ultrasound examination of the patient during pregnancy did not reveal the presence of uterine fibroids, the sonographer at the subordinate hospital offered a misdiagnosis of bladder prolapse. Fourth, due to the serious condition of the patient upon admission, the relevant examination was not completed in a timely manner.
The specific mechanism of uterine leiomyoma prolapse is unclear; however, according to the case analysis, factors such as treatment with uterine artery embolization (UAE), laparoscopic-assisted uterine depletion (LAUD), and gonadotropin-releasing hormone adjuvant therapy (GnRH-a) may play a role (10). Additionally, following delivery, the uterus returns to its pre-pregnancy size within approximately 4 weeks. Strong postpartum uterine contractions are also believed to be a factor that promotes fibroid discharge (10). In addition, Demirci et al. (16) discovered that when submucosal myomas have a pedicle in the uterine cavity, the natural tendency for the uterus is to attempt to expel the soft myomas through the cervical canal, ultimately leading to cervix dilation. Myomas are generally necrotic and can sometimes become infected when emerging from the gradually expanding cervix since they have difficulty maintaining an adequate blood supply through the long pedicle (5). In this case, it is possible for a quite large submucosal pedunculated myoma to be delivered gradually through a visibly dilated cervix, resulting in gradual ischemic necrosis.
Clinical diagnosis of vaginal prolapse of the submucosal myoma can be challenging due to its occult nature and rarity. However, radiology can help make a diagnosis. Computed tomography (CT) scans can reveal a qualitative echo of a pelvic mass, linking solid and cystic components to degeneration and infarcted areas, which can lead to an early and definite diagnosis (11). MRI can provide significantly accurate and useful information related to myoma survival, vascular supply, and myometrial involvement and also plays an important role in selecting the appropriate surgical procedure (17). In this case, an enhanced MRI revealed that there was no blood supply to the prolapsed fibroid and its pedicle, and thus, a transvaginal myomectomy was chosen.
There are currently no clinical guidelines for treating a pedunculated submucosal myoma during pregnancy or postpartum, as this type of myoma is rare, and there have only been 14 cases reported since 1945, all of which have been accompanied by an occult development of suppuration (1–13). Sirha et al. (18) have found that surgical intervention combined with more effective antibiotics is the most appropriate treatment. Golan et al. (19) found that the success rate of vaginal myomectomy was 95.6% in 46 patients with prolapsed submucosal myomas over a 10-year period and the recurrence rate was incredibly low. Therefore, it is recommended that transvaginal myomectomy should be the first choice of surgical treatment. Surgically preserving fertility may be possible if the surgeon reaches the uterine pedicle (16).
In summary, the infection of submucous leiomyoma of the uterus should be highly suspected in parturient women with hysteromyoma and recurrent fever after delivery, where the source of infection cannot be identified. MRI can provide incredibly accurate and useful information related to myoma survival, vascular supply, and myometrial involvement and plays a crucial role in selecting surgical procedures. Transvaginal myomectomy may be the preferred treatment for prolapsed myoma in situations where the pedicle can be achieved.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University prior to the commencement of the study. The study was conducted according to the principles of the Declaration of Helsinki and its amendments. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LL, XW, and ZG provided and drafted the manuscript. DM Tian, XY, and HZ completed the literature review and preliminary revision. BL and D Tang assisted with the operation and provided surgical records. JS and QZ provided critical revisions of the report for important intellectual content. All authors participated in the care of the patient. All authors contributed to the article and approved the submitted version.
Funding
This case report was supported by the National Natural Science Foundation of China (No. 82260297), Yunnan University Science and Technology Innovation Team (No. K1322112), and Yunnan Province Clinical Research Center for Chronic Kidney Disease (No. 202102AA100060).
Acknowledgments
The authors thank Yin Mo and Yizhen Zeng for their help in the imaging diagnosis of the patient.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
E. coli, Escherichia coli; MRI, magnetic resonance imaging; DWI, diffusion-weighted imaging; UAE, uterine artery embolization; LAUD, laparoscopic-assisted uterine depletion; GnRH-a, gonadotropin-releasing hormone adjuvant therapy; CT, computed tomography.
References
1. Zhang J, Zou B, Wang K. Spontaneous expulsion of a huge cervical leiomyoma from the vagina after cesarean: a case report with literature review. Medicine (Baltimore). (2018) 97:e11766. doi: 10.1097/MD.0000000000011766
2. Coronado GD, Marshall LM, Schwartz SM. Complications in pregnancy, labor, and delivery with uterine leiomyomas: a population-based study. Obstet Gynecol. (2000) 95:764–9. doi: 10.1016/s0029-7844(99)00605-5
3. Mason TC. Red degeneration of a leiomyoma masquerading as retained products of conception. J Natl Med Assoc. (2002) 94:124–6. PMID: 11853046. PMCID: 2594119.11853046
4. DeMaio A, Doyle M. Pyomyoma as a rare source of postpartum sepsis. Case Rep Obstet Gynecol. (2015) 2015:1–2. doi: 10.1155/2015/263518
5. Elgonaid W, Belkhir R, Boama V. Transvaginal postpartum manual removal of a prolapsed submucous leiomyoma, initially diagnosed hybrid predominantly intramural. BMJ Case Rep. (2017) 2017:1–5. doi: 10.1136/bcr-2016-218712
6. Anderson WR, Lauderdale JM. Submucous myoma in term pregnancy: report of a case. Obstet Gynecol. (1964) 24:455–7. doi: 10.1097/00006250-196409000-00024
7. Gainey HL, Keeler JE. Submucous myoma in term pregnancy. Am J Obstet Gynecol. (1949) 58:727–37. doi: 10.1016/S0002-9378(16)39228-6
8. Thorpe-Beeston JG, Sebire NJ. Spontaneous expulsion of submucous fibroid after preterm labour. BJOG. (2002) 109:726–7. doi: 10.1111/j.1471-0528.2002.01084.x
9. Sagoo B, Ng KY, Ghaleb G, Brown H. Spontaneous expulsion of intramural fibroid six weeks after emergency caesarean section. Case Rep Obstet Gynecol. (2015) 2015:640570. doi: 10.1155/2015/640570
10. Murakami T, Niikura H, Shima Y, Terada Y, Okamura K. Sloughing off of a cervical myoma after cesarean section: a case report. J Reprod Med. (2007) 52:962–4. PMID: 17977176
11. Wang J, Li Z, Sun Y. Prolapsed submucosal pyomyoma postpartum, a rare complication of fibroids. BMC Pregnancy Childbirth. (2021) 21:132. doi: 10.1186/s12884-021-03619-6
12. Pieh-Holder KL, Bell H, Hall T, DeVente JE. Postpartum prolapsed leiomyoma with uterine inversion managed by vaginal hysterectomy. Case Rep Obstet Gynecol. (2014) 2014:435101. doi: 10.1155/2014/435101
13. Nkwabong E. An intramural uterine fibroid became submucosal in the puerperium—proposed probable mechanism: a case report. J Med Case Rep. (2018) 12:88. doi: 10.1186/s13256-018-1624-0
14. Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. (2008) 198:357–66. doi: 10.1016/j.ajog.2007.12.039
15. Zaima A, Ash A. Fibroid in pregnancy: characteristics, complications, and management. Postgrad Med J. (2011) 87:819–28. doi: 10.1136/postgradmedj-2011-130319
16. Demirci F, Somunkiran A, Safak AA, Ozdemir I, Demirci E. Vaginal removal of prolapsed pedunculated submucosal myoma during pregnancy. Adv Ther. (2007) 24:903–6. doi: 10.1007/BF02849983
17. Torrance SM, Muhn N, Ellis S, Rebello R, Ramanna R. Role of dynamic MRI in surgical decision-making for a postpartum woman with a prolapsed degenerating uterine leiomyoma. J Obstet Gynaecol Can. (2009) 31:446–51. doi: 10.1016/S1701-2163(16)34176-7
18. Sirha R, Miskin A, Abdelmagied A. Postnatal pyomyoma: a diagnostic dilemma. BMJ Case Rep. (2013) 2013:1–4. doi: 10.1136/bcr-2013-201137
Keywords: submucosal leiomyoma, prolapse, bladder prolapse, postpartum, transvaginal
Citation: Li L, Shen J, Gao Z, Wang X, Tian D, Yang X, Zhou H, Li B, Tang D and Zhang Q (2023) Transvaginal prolapsed submucosal leiomyoma after cesarean section misdiagnosed as bladder prolapse: A case report with literature review. Front. Surg. 10:1071247. doi: 10.3389/fsurg.2023.1071247
Received: 16 October 2022; Accepted: 23 January 2023;
Published: 13 February 2023.
Edited by:
Zaleha Abdullah Mahdy, National University of Malaysia, MalaysiaReviewed by:
Huri Güvey, Private Parkhayat Hospital, TürkiyeKah Teik Chew, Universiti Kebangsaan Malaysia Medical Center (UKMMC), Malaysia
© 2023 Li, Shen, Gao, Wang, Tian, Yang, Zhou, Li, Tang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Quan Zhang MTU1MDA1NjY1N0BxcS5jb20=
Specialty Section: This article was submitted to Obstetrics and Gynecological Surgery, a section of the journal Frontiers in Surgery
 Ling Li
Ling Li Jihong Shen
Jihong Shen Zhenhua Gao1
Zhenhua Gao1 Xingqi Wang
Xingqi Wang Quan Zhang
Quan Zhang