- Department of Neurosurgery, University Medical Center, Johannes Gutenberg University Mainz, Mainz, Germany
Multiple myeloma (MM) is a hematological malignancy with characteristic clonal plasma cell proliferation and production of monoclonal immunoglobulins. Although it can often metastasize to the bony spine, completely extravertebral and extra-/intradural manifestations are exceedingly rare. In this case report, we describe a 51-year-old male patient with cervical extradural and intraforaminal MM who was surgically treated in our department. Clinical findings and radiological images were retrieved from medical records and an imaging system. This unusual localization of MM and similar cases in the literature are reviewed in detail. The patient underwent tumor resection via a ventral approach, and postoperative MRI demonstrated a sufficient decompression of neural structures. No new neurological deficits were observed at subsequent follow-ups. Although 7 cases of extramedullary extradural manifestations of multiple myeloma have been described in the literature so far, this is the first case of intraforaminal extramedullary multiple myeloma located in the cervical spine and treated by surgery.
Introduction
Multiple myeloma (MM) represents 10% of all hematologic cancers with an annual incidence of 6.6 cases per 100,000 (1). It is characterized by the proliferation of neoplastic plasma cells, producing excessive monoclonal immunoglobulin (Ig) or free light chains (2). Multiple myeloma occurs as an extramedullary disease caused by hematogenous or continuous growth via the bone cortex. The most common site of manifestation of MM is the lower thoracic spine, followed by the lumbar spine. Vertebral destruction is primarily responsible for neurological symptoms, while the most frequent symptoms are pain and radiculopathy (3).
Here, we present a case of a patient with previously diagnosed and treated MM who was diagnosed with an intraspinal extradural tumor with an extension to the neuroforamen, resembling a spinal schwannoma, which finally turned out to be a manifestation of MM. We review the literature for the clinical course and management of this important differential diagnosis.
Case description
A 51-year-old male patient presented to our department with pain in his left shoulder for approximately 9 months. The patient developed burning and piercing pain and dysesthesia in his left arm for 5 months, which corresponded to the C6 dermatome. His pain medication consisted of hydromorphone and dexamethasone. On admission, the patient was awake and cooperative. Cranial nerve status was normal. Except for the tingling paraesthesia of Dig 1, there were no sensory or motor deficits in the extremities. There were no pathological findings in the standing and gait tests.
The patient was diagnosed with multiple myeloma 18 months ago, with manifestation in the 11th thoracic vertebral body, and treated with vertebral body replacement and dorsal spondylodesis T10–12. The surgery was followed by radiotherapy of the T10–12 up to a total dose of 46 Gy and two cycles of adjuvant chemotherapy (bortezomib–cyclophosphamide–dexamethasone). In the subsequent course, autologous stem cell transplantation was performed without complications.
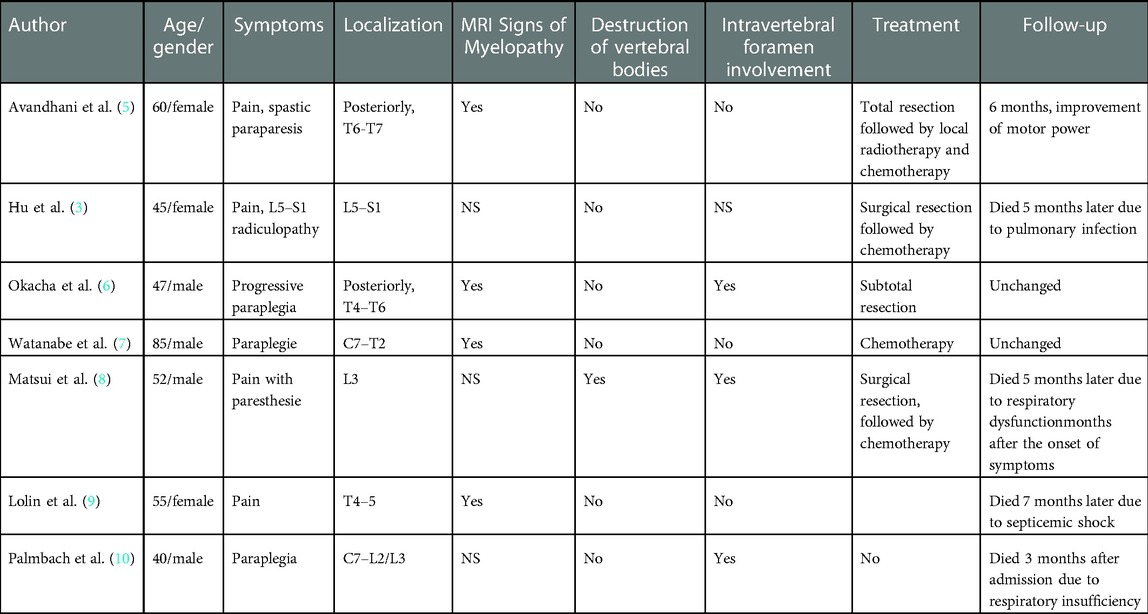
Associated with his new radicular symptoms, an MRI of his cervical spine demonstrated an intraspinal, extradural, and intraforaminal contrast-enhancing lesion adjacent to the left-sided C6 root, without evidence of bone destruction. MRI features were suggestive of a C6 schwannoma (Figure 1).
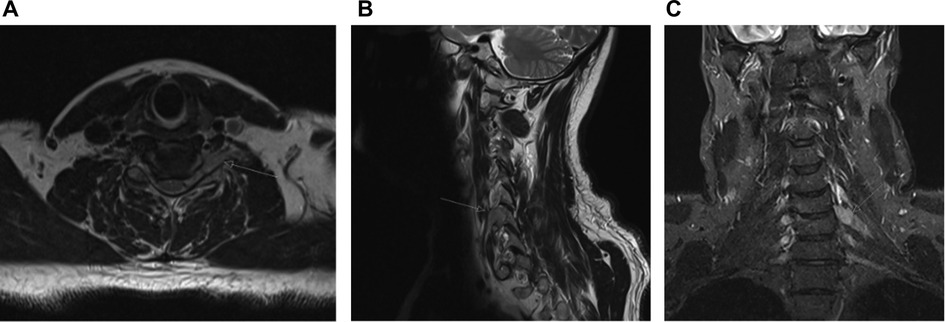
Figure 1. Axial (A), sagittal (B), and coronal (C) post-contrast T1 MRI showing extensive intraspinal, extradural tumor, including extension into the left C5/6 neural exit foramen.
A blood test showed normal values of hemoglobin (14.4 g/dl, reference range: 13.5–17.5 g/dl) and red cell count (4.72/pl; reference range: 4.2–5.6/pl). Serum LDH value was 275 U/I (reference range: <245 U/I). Tumor resection and decompression of the nerve root were scheduled via a ventral approach. A direct route to the lesion without retraction of the spinal cord was significantly more advantageous with a ventral approach.
As the intraoperative frozen section unexpectedly demonstrated a small blue cell tumor and the tumor diffusely infiltrated the nerve root, the decision was made to perform a partial resection and debulking of the tumor mass. A complete tumor resection could be taken into consideration after the completion of the histological analysis. The patient recovered well from the operation and reported significant pain relief. There were no new neurological deficits. Histologic analysis demonstrated cells with a narrow, poorly demarcated cytoplasm and relatively small, round, and hyperchromatic nuclei with numerous mitoses. The Ki67 proliferation index was >50%. Tumor cells were negative for CD45, CD3, CD20, CD138, synaptophysin, and S10. Positive immunoreactivity was observed only for vimentin antibodies. The final histological analysis revealed a manifestation of MM.
Postoperative MRI demonstrated a sufficient decompression of neural structures with a tumor remnant lateral to the nerve root (Figure 2). After an interdisciplinary case discussion, local ablative radiotherapy with a total dose of 45.0 Gy and adjuvant chemotherapy were performed. The patient has been followed for 9 months with no new neurological deficits and no tumor recurrence.
Discussion
Although MM is the most common malignant tumor in the vertebrae, spinal cord compression occurs in only 5% of cases, usually due to extramedullary epidural tumor growth or a vertebral fracture (4) We searched the PubMed/MEDLINE databases using the following keywords: “multiple myeloma” AND extraosseous AND spinal cord compression. A literature search revealed only 7 cases of extradural manifestation of multiple myeloma (Table 1) (3, 5–10). To our knowledge, this is the first case of intraforaminal extramedullary multiple myeloma located in the cervical spine and treated by surgery. It is postulated that extramedullary hematopoietic (EMH) multiple myeloma arises from hematogenous spread or contiguous seeding from local lytic bone lesions (11). In this case, the manifestation of MM was localized extradural in the lateral spinal canal and neural foramen, without the affection of the adjacent vertebra. The tumor compressed the nerve root, which led to pain, motor, and sensory deficits.
It is known that multiple myeloma can be associated with chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) (12). However, several studies have shown that idiopatic CIDP cannot be distinguished from CIDP related to monoclonal gammopathies (13, 14).
Given that pararoteinemia-neuropathy cannot be distinguished from CIDP, their work-up is still a debate. In addition to protein electrophoresis, some authors suggested that nerve biopsy could explain the etiology of neuropathy (15). Peripheral nerve ultrasound has been proposed to differentiate neuropathies associated with antimyelin, CIDP, and M-protein (16). However, due to variable neurotoxic patterns, ultrasound cannot provide relevant results in multiple myeloma.
The primary diagnostic tool for intraspinal tumors is MRI. MM manifests as a contrast-enhancing lesion. These lesions can be diffuse, spreading across multiple spinal levels (17).
The differential diagnoses for intraforaminal and spinal cord lesions usually include schwannoma, neurofibroma, hemangioblastoma, malignant peripheral nerve sheath tumor, spinal metastasis, solitary amyloidoma, and epidural abscess (5). However, the differentiation of intraforaminal lesions based on morphology and intensity may present a challenge for neuroradiologists. As a result, based on MRI features such as T1 iso- to hypointensity and T2 hyperintensity, as well as the configuration, a working diagnosis of schwannoma was made.
The median survival with MM is 2.5 years, while younger patients have a better prognosis. Some studies have reported that the median survival of a patient with EMH MM is 1–11 months (18–20) If the spine is affected, 75% of patients die within 1 year of diagnosis (21). Given the small number of papers published so far, MM's overall survival with extradural localization is unknown. In the cases of epidural extramedullary multiple myeloma reported so far, the cause of death was an infection or respiratory failure.
There are no guidelines for the management of treatment for intraspinal extradural multiple myeloma. In a longitudinal study of 1,003 patients by Varettoni et al., patients with an extramedullary manifestation of multiple myeloma had significantly lower hemoglobin and increased LDH levels (22). Similar findings were reported by studies of Barlogie et al. and Dimopoulus et al., confirming the association between LDH values and a more aggressive course and shorter survival of the patient with MM (23, 24). In our case, the serum LDH value on the day of admission was 275 U/I, which, with a Ki67 finding of >50%, confirms the aggressiveness of the tumor. Due to the extremely high proliferation activity, we hypothesized that MM has an aggressive phenotype, i.e., that there has been a plasmablastic transformation of MM.
An increased incidence of extramedullary relapse has been reported in patients undergoing allogeneic stem cell transplantation. In their retrospective study, Vincent et al. found that the number of previous therapies and age were associated with a higher risk of extramedullary relapse (25). Chemotherapy of extramedullary localizations of MM has so far not yielded satisfactory results (26).
Although extremely rare, a manifestation of multiple myeloma should be included in the differential diagnosis of extradural and intraforaminal tumors in patients with a known MM. Early detection of the lesion is essential, especially if neurological symptoms appear. CSF cytology might be helpful in the diagnosis of intradural lesions, while tumor decompression can prevent neurological deterioration and improve the patient's quality of life. Given that it is difficult to distinguish multiple myeloma from other intraspinal pathology based on signal intensity and morphology on MRI scans, a rapid intraoperative tissue analysis should be considered to avoid unnecessary extensive tumor resections.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
The authors that contributed to the conception and design of the study were DJ, DK, and NK. Data acquisition and interpretation were performed by DJ and DK. The first draft of the manuscript was written by DJ. DK, NK, and MO reviewed the manuscript. FR supervised and approved the final version of the report. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Becker N. Epidemiology of multiple myeloma. Recent Results Cancer Res. (2011) 183:25–35. doi: 10.1007/978-3-540-85772-3_2
2. Rafae A, Malik MN, Abu Zar M, Durer S, Durer C. An overview of light chain multiple myeloma: clinical characteristics and rarities, management strategies, and disease monitoring. Cureus. (2018) 10(8):e3148, doi: 10.7759/cureus.3148
3. Hu KC, Lin J, Chuang YC, Cheng SJ, Chang KM. Multiple myeloma associated with extramedullary plasmacytoma causing nerve root compression: a case report. J Formos Med Assoc. (2001) 100(4):277–80.11393129
4. Dispenzieri A, Kyle RA. Neurological aspects of multiple myeloma and related disorders. Best Pract Res Clin Haematol. (2005) 18(4):673–88. doi: 10.1016/j.beha.2005.01.024
5. Avadhani A, Shetty AP, Rajasekaran S. Isolated extraosseous epidural myeloma presenting with thoracic compressive myelopathy. Spine J. (2010) 10(4):e7–e10. doi: 10.1016/j.spinee.2010.01.007
6. Okacha N, Chrif E, Brahim E, Ali A, Abderrahman E, Gazzaz M, et al. Extraosseous epidural multiple myeloma presenting with thoracic spine compression. Joint Bone Spine. (2008) 75(1):70–2. doi: 10.1016/j.jbspin.2007.01.044
7. Watanabe Y, Endou A, Ooi S, Matsushima E, Shimisu Y, Nakashima K. Extraosseous epidural IgD myeloma presenting with compression myelopathy. Psychiatry Clin Neurosci. (2000) 54(6):665–7. doi: 10.1046/j.1440-1819.2000.00767.x
8. Matsui H, Fujie H, Tsuji H. Extraosseous epidural tumor of immunoglobulin D myeloma. J Spinal Disord. (1992) 5(3):366–9. doi: 10.1097/00002517-199209000-00017
9. Lolin YI, Lam CW, Lo WH, Au KL, Masarei JR. IgD multiple myeloma with thoracic spine compression due to epidural extra-osseous tumour spread. J Clin Pathol. (1994) 47(7):669–71. doi: 10.1136/jcp.47.7.669
10. Palmbach M, Hoffmann W, Grodd W, Postler E, Voigt K. Extraosseous, epidural tumour spread of multiple myeloma. Eur J Radiol. (1996) 22(2):146–8. doi: 10.1016/0720-048x(96)00754-1
11. Gozzetti A, Cerase A, Lotti F, Rossi D, Palumbo A, Petrucci MT, et al. Extramedullary intracranial localization of multiple myeloma and treatment with novel agents: a retrospective survey of 50 patients. Cancer. (2012) 118(6):1574–84. doi: 10.1002/cncr.26447
12. Fasanya AA, Loncharich MF, Gandhi V, Rana S, Balaan M. Multiple myeloma associated chronic inflammatory demyelinating polyradiculoneuropathy: the importance of continued surveillance. Cureus. (2016) 8(11):e899. doi: 10.7759/cureus.899
13. Rajabally YA. Neuropathy and paraproteins: review of a complex association. Eur J Neurol. (2011) 18(11):1291–8. doi: 10.1111/j.1468-1331.2011.03380.x
14. Simmons Z, Albers JW, Bromberg MB, Feldman EL. Long-term follow-up of patients with chronic inflammatory demyelinating polyradiculoneuropathy, without and with monoclonal gammopathy. Brain. (1995) 118(Pt 2):359–68. doi: 10.1093/brain/118.2.359
15. Van den Bergh PY, Rajabally YA. Chronic inflammatory demyelinating polyradiculoneuropathy. Presse Med. (2013) 42(6 Pt 2):e203–15. doi: 10.1016/j.lpm.2013.01.056
16. Athanasopoulou IM, Rasenack M, Grimm C, Axer H, Sinnreich M, Decard BF, et al. Ultrasound of the nerves—an appropriate addition to nerve conduction studies to differentiate paraproteinemic neuropathies. J Neurol Sci. (2016) 362:188–95. doi: 10.1016/j.jns.2016.01.055
17. Di L, Huang K, Kesayan T, Kroll D, Baz RC, Macaulay RJ, et al. Multiple myeloma presenting as an intramedullary spinal cord tumor: a case report and review of the literature. J Med Case Rep. (2020) 14(1):189. doi: 10.1186/s13256-020-02496-5
18. Dias A, Higashi F, Peres ALM, Cury P, Crusoe EQ, Hungria VTM. Multiple myeloma and central nervous system involvement: experience of a Brazilian center. Rev Bras Hematol Hemoter. (2018) 40(1):30–6. doi: 10.1016/j.bjhh.2017.09.004
19. Paludo J, Painuly U, Kumar S, Gonsalves WI, Rajkumar V, Buadi F, et al. Myelomatous involvement of the central nervous system. Clin Lymphoma Myeloma Leuk. (2016) 16(11):644–54. doi: 10.1016/j.clml.2016.08.010
20. Jurczyszyn A, Grzasko N, Gozzetti A, Czepiel J, Cerase A, Hungria V, et al. Central nervous system involvement by multiple myeloma: a multi-institutional retrospective study of 172 patients in daily clinical practice. Am J Hematol. (2016) 91(6):575–80. doi: 10.1002/ajh.24351
21. Bladé J, Kyle RA. Multiple myeloma in young patients: clinical presentation and treatment approach. Leuk Lymphoma. (1998) 30(5–6):493–501. doi: 10.3109/10428199809057562
22. Varettoni M, Corso A, Pica G, Mangiacavalli S, Pascutto C, Lazzarino M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol. (2010) 21(2):325–30. doi: 10.1093/annonc/mdp329
23. Barlogie B, Smallwood L, Smith T, Alexanian R. High serum levels of lactic dehydrogenase identify a high-grade lymphoma-like myeloma. Ann Intern Med. (1989) 110(7):521–5. doi: 10.7326/0003-4819-110-7-521
24. Dimopoulos MA, Barlogie B, Smith TL, Alexanian R. High serum lactate dehydrogenase level as a marker for drug resistance and short survival in multiple myeloma. Ann Intern Med. (1991) 115(12):931–5. doi: 10.7326/0003-4819-115-12-931
25. Vincent L, Ceballos P, Plassot C, Méniane JC, Quittet P, Navarro R, et al. Factors influencing extramedullary relapse after allogeneic transplantation for multiple myeloma. Blood Cancer J. (2015) 5(8):e341. doi: 10.1038/bcj.2015.48
26. Damaj G, Mohty M, Vey N, Dincan E, Bouabdallah R, Faucher C, et al. Features of extramedullary and extraosseous multiple myeloma: a report of 19 patients from a single center. Eur J Haematol. (2004) 73(6):402–6, tumour spread. J. Clin. Pathol. 1994; 47: 669–671. doi: 10.1111/j.1600-0609.2004.00331.x
Keywords: case report, multiple myeloma, outcome, spine, surgery
Citation: Jankovic D, Kalasauskas D, Keric N, Ottenhausen M and Ringel F (2023) Multiple myeloma presenting as a cervical intraforaminal tumor: A case report and review of literature. Front. Surg. 10:1011152. doi: 10.3389/fsurg.2023.1011152
Received: 3 August 2022; Accepted: 2 January 2023;
Published: 30 January 2023.
Edited by:
Riccardo Bertolo, Hospital San Carlo di Nancy, ItalyReviewed by:
Lukas Rasulić, University of Belgrade, SerbiaRana Moshref, King Faisal Specialist Hospital and Research Centre, Saudi Arabia
© 2023 Jankovic, Kalasauskas, Keric, Ottenhausen and Ringel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dragan Jankovic ZHJhZ2FuLm1lZGljaW5lQGdtYWlsLmNvbQ==
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
 Dragan Jankovic
Dragan Jankovic Darius Kalasauskas
Darius Kalasauskas Naureen Keric
Naureen Keric Malte Ottenhausen
Malte Ottenhausen Florian Ringel
Florian Ringel