- 1Department of Orthopedics, Xiangya Hospital, Central South University, Changsha, China
- 2National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Central South University, Changsha, China
- 3Xiangya School of Medicine, Central South University, Changsha, China
Background: Currently, there are many surgical options for patellar dislocation. The purpose of this study is to perform a network meta-analysis of the randomized controlled trials (RCTs) and cohort studies to determine the better treatment.
Method: We searched the Pubmed, Embase, Cochrane Central Register of Controlled Trials, Web of Science, clinicaltrials.gov and who.int/trialsearch. Clinical outcomes included Kujala score, Lysholm score, International Knee Documentation Committee (IKDC) score, redislocation or recurrent instability. We conducted pairwise meta-analysis and network meta-analysis respectively using the frequentist model to compare the clinical outcomes.
Results: There were 10 RCTs and 2 cohort studies with a total of 774 patients included in our study. In network meta-analysis, double-bundle medial patellofemoral ligament reconstruction (DB-MPFLR) achieved good results on functional scores. According to the surface under the cumulative ranking (SUCRA), DB-MPFLR had the highest probabilities of their protective effects on outcomes of Kujala score (SUCRA 96.5 %), IKDC score (SUCRA 100.0%) and redislocation (SUCRA 67.8%). However, DB-MPFLR (SUCRA 84.6%) comes second to SB-MPFLR (SUCRA 90.4%) in Lyshlom score. It is (SUCRA 70%) also inferior to vastus medialis plasty (VM-plasty) (SUCRA 81.9%) in preventing Recurrent instability. The results of subgroup analysis were similar.
Conclusion: Our study demonstrated that MPFLR showed better functional scores than other surgical options.
Introduction
Patellar dislocation is a serious injury, accounting for 3.3% of all knee injuries, and females aged 10–17 are at the highest risk (1, 2). Failure or suboptimal treatment may result in serious problems, such as recurrent instability, keen pain, and even osteoarthritis. Those with a history of dislocation were seven times more likely to have an unstable episode during follow-up than those with a first dislocation (3). Therefore, appropriate and effective treatments are urgently needed.
A meta-analysis has reported that conservative treatments can be used for patients with lower risk, while surgery should be considered for patients with higher risk (1). However, there are different surgical options, such as medial retinaculum plication (MR-plication), medial retinaculum plasty (MR-plasty), VM-plasty, medial capsule reefing (MC-reefing), medial patellofemoral ligament reconstruction (MPFLR) and so on. In addition, a study has shown that approximately from the femoral origination point, the medial patellofemoral ligament (MPFL) consists of two relatively concentrated fiber bundles: the inferior-straight bundle and the superior-oblique bundle (4). Thus, two different methods of reconstructing the medial patellar ligament were proposed, single-bundle MPFLR (SB-MPFLR) and DB-MPFLR respectively. However, there is no standard consensus on surgical options for the treatment of patellar dislocation.
This study aimed to perform a network meta-analysis of RCTs and cohort studies in the literature to clarify differences in surgical options and provide evidence for the better treatment. The hypothesis is that DB-MPFLR would repair the medial soft tissue structure better compared with other options.
Materials and methods
Study selection
This study was according to Cochrane Review methods, and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two reviewers independently performed a literature search, reviewing the titles and abstracts of all results, and then conducting a full-text review. We manually screened all references in the study and all literature reviews found in the search results to find articles that met the inclusion criteria. We used some combined text and MeSH terms (“patellar dislocation”, “medial patellofemoral ligament reconstruction”, “plication”, “plasty”, and “reefing”) to search the Cochrane Central Register of Controlled Trials, Pubmed, Embase, Web of Science, clinicaltrials.gov and who.int/trialsearch. The complete search used for electronic databases was listed in Supplementary Appendix A. This search was carried out in December 2021.
Inclusion criteria
(1) Human studies; (2) Studies that evaluated clinical outcomes of MPFLR or other soft tissue surgeries (plication, plasty, reefing etc.); (3) RCTs or cohort studies; (4) Published in English language; (5) Studies reporting at least one of the following data: Kujala score, Lysholm score, IKDC score, redislocation or recurrent instability.
Exclusion criteria
(1) Subjects with knee disease or previous knee surgery; (2) Studies that only reported preoperative or intraoperative outcomes.
Data collection and analysis
The studies were independently evaluated by two authors, followed by full-text readings of potentially eligible articles for eventual inclusion. The uncertainties included in the study were resolved through discussion and negotiation. Eligible data were extracted independently by one author into a pre-defined format and then extracted by another author for a second time to ensure accuracy. We collected information concerning (1) study characteristics including journal, authors, year of publication, study design, and level of evidence; (2) demographics of patients including the number of subjects, gender, age, surgical techniques, postoperative rehabilitation, and duration of follow-up. (3) the outcomes of studies including the Kujala score, Lysholm score, IKDC score, redislocation, or recurrent instability.
Assessment of risk of bias and quality of evidence
The assessment is done independently by two investigators using the Cochrane Risk of Bias Tool for RCTs, while the cohort studies were assessed using the modified Newcastle-Ottawa Scale (NOS) (5, 6). Any disagreement between the two authors was resolved through discussion and, if no agreement could be reached after discussion, it was left to the judgment of the third author.
Statistical analysis
We conducted a pairwise meta-analysis and a network meta-analysis in a frequentist model (7). In addition, we performed a subgroup analysis of recurrent patellar dislocation in network meta-analysis. The relative effect sizes of continuous outcomes in data analysis were mean difference (MD) with confidence interval (CI) of 95% and odds ratios (ORs) and 95% CIs were calculated to evaluate the dichotomous outcomes. The level of statistical significance was set as p < 0.05. All statistical analyses were performed using R 4.1.1. The I-Squared (I2) test was used to estimate heterogeneity among studies for pairwise meta-analyse and network meta-analysis (8). According to the Cochrane Collaboration Handbook, only if I2 < 25%, the heterogeneity between studies is low. Therefore, in the heterogeneity test, if I2 < 25%, fixed-effects model was adopted; otherwise, we conducted the random-effects model. For the network meta-analysis, the analysis was performed in a frequentist model employing the “netmeta” packages. For each outcome, we used a trail network plot to show the comparison of all interventions. SUCRA was used to represent the overall ranking of an intervention; that was, the higher the value of SUCRA, the higher the probability of this surgical option being the best intervention (9). We calculated the value of SUCRA to rank each intervention. Publication bias of the studies was assessed by observing the symmetry of comparison-adjusted funnel plots.
CINeMA assessment
The confidence in network meta-analysis (CINeMA) framework was used to assessed the certainty of the evidence (10). The CINeMA evaluation consists of six evaluable items: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. There are four levels of evidence: high, medium, low, and very low. The grade of RCT is high and The grade of cohort studies is low before evaluation.
Results
Results of the search
A total of 208 articles were queried from the databases with additional 4 records identified through other sources. Of these, 102 were duplicates in the databases and were subsequently excluded. The remaining 110 papers were carefully screened for titles and abstracts, and only 22 remained, excluding all others as irrelevant to the purpose of the study. We reviewed the full text of the remaining 22 articles and subsequently excluded 10 due to the lack of necessary data. Ultimately, a total of 10 RCTs and 2 cohort studies were included for data extraction and meta-analysis. Figure 1 illustrates the process of systematic literature retrieval and research selection.
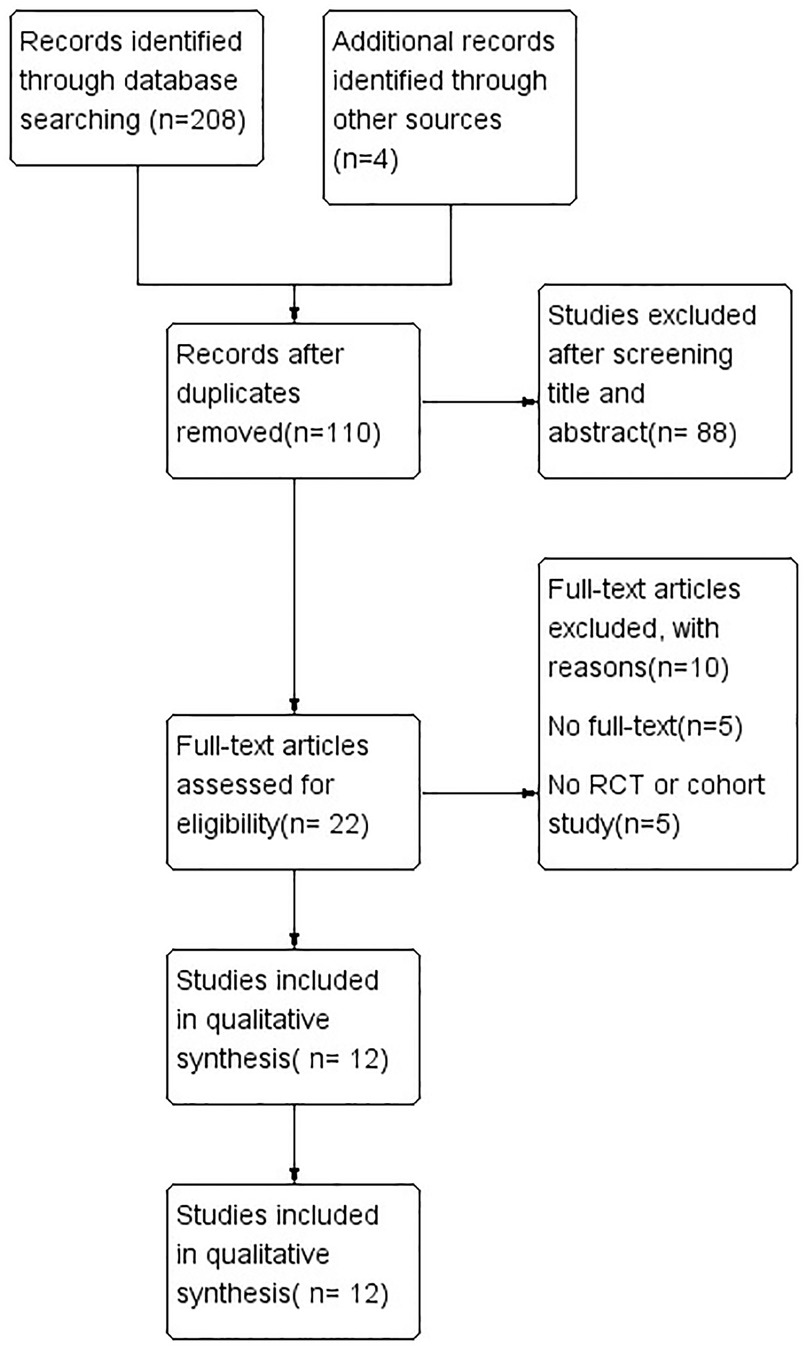
Figure 1. Search flow diagram. The search flow diagram summarizes the search, screening, retrieval, and appraisal of articles finally included in the network meta-analysis.
Characteristics of the included studies
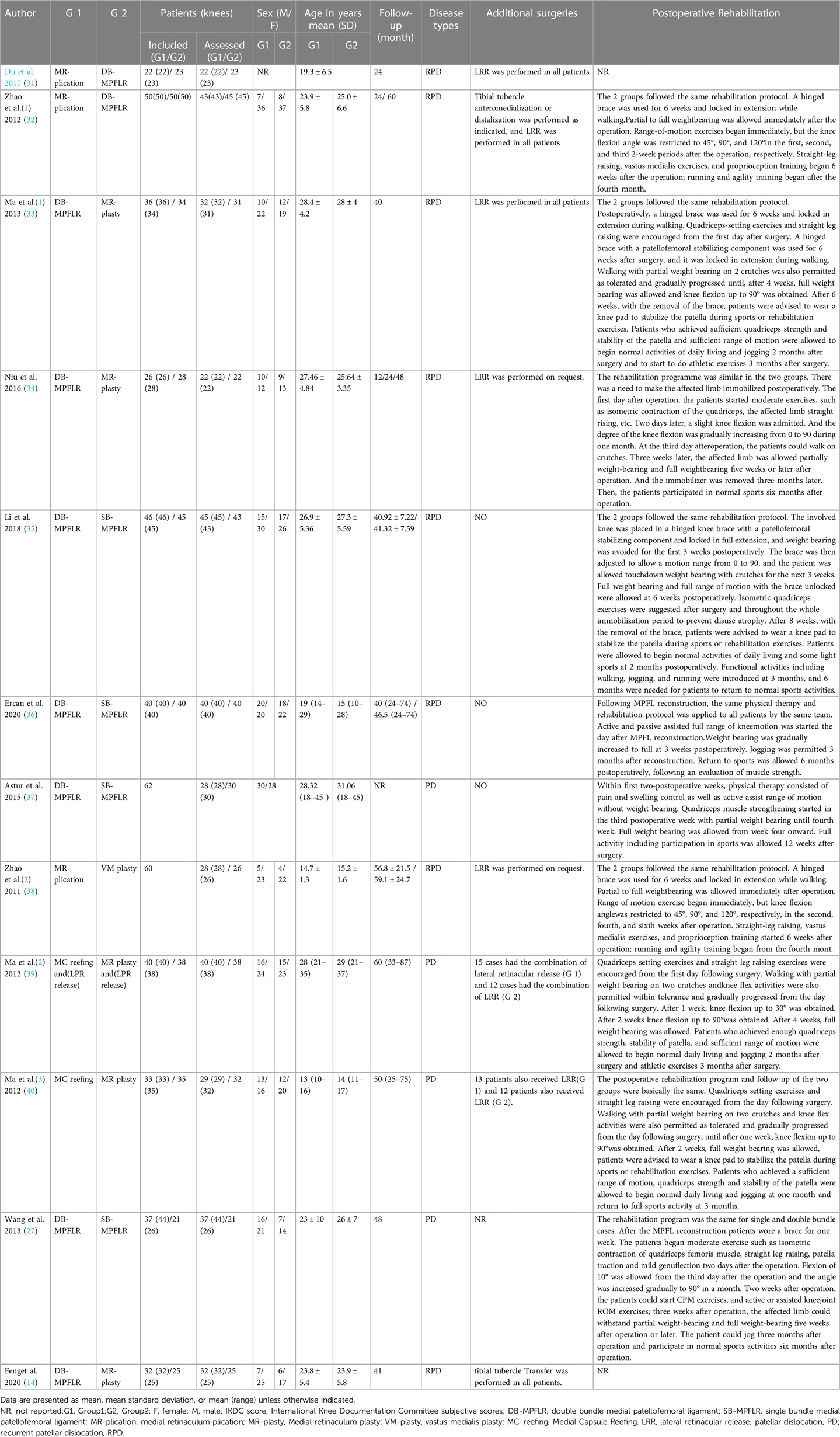
This review includes 12 trials involving 774 patients. These studies were published between 2011 and 2020. A total of 6 different surgical methods were introduced for the 10 RCTs and 2 cohort studies. Of the included 12 studies, 12 studies provided Kujala scores, 6 provided Lysholm scores, 5 provided IKDC scores and 9 provided redislocation and 8 provided recurrent instability respectively. The sample sizes of the included trials ranged from 45 to 88 patients, with the mean ages ranging from 13 to 29 years and the duration of follow-up ranging from 24 to 87 months. The basic characteristics of the included studies are summarized in Table 1.
Quality assessment of included studies
We adopted the Cochrane Risk of Bias Tool for RCTs (RoB2.0) (the score for each bias domain was graded as representing a low, high, or unclear risk of bias) and modified Newcastle-Ottawa Scale (NOS) for cohort studies (Studies with scores of 7, 5 to 7, 3 to 5, and 0 to 2 were considered of good, fair, poor-fair, and poor quality, respectively) for methodological quality evaluation. Among 10 RCTs, 6 studies utilized sufficient random sequence generation methods. Appropriate methods of allocation concealment were described in 3 studies. None of the studies applied blindness to patients and researchers because of practical and ethical issues, which resulted in a high risk of bias. In 3 studies, the outcome measures were blinded. Other bias of five included RCTs was unclear. NOS indicated that the two cohort studies were of good quality. The risk of bias assessment for RCTs is shown in Supplementary Appendix B(a-b), and the risk of bias assessment for cohort studies is shown in Supplementary Appendix B(C).
Clinical outcomes: quantitative analysis
Pairwise meta-analysis
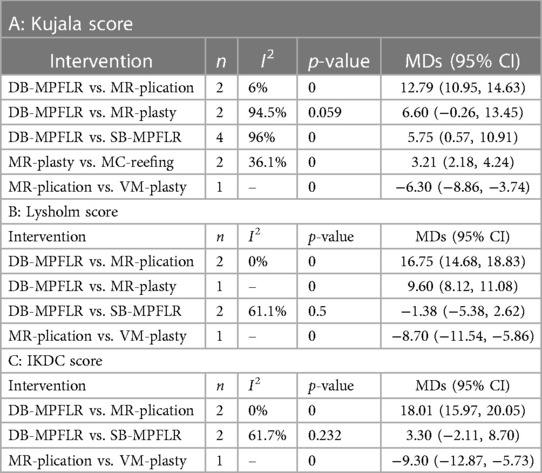
For redislocation and recurrent instability, no pairwise meta-analysis was performed because the number of events in many studies was 0. All detailed results of pair-wise meta-analysis are shown in Table 2A–C.
Network meta-analysis
Kujala score
Twelve included studies reported Kujala scores as one of the study outcomes. I2 = 94.1%, so we chosen the random effects model. Figure 2A shows the MD and 95% CI of each surgery compared with DB-MPFLR. MC-reefing (MD −10.12, 95% CI, −18.43, −1.81), MR-plasty (MD −6.63,95% CI, −18.43, −0.68), MR-plication (MD −12.66,95% CI, −18.67, −6.66), SB-MPFLR (MD −5.83,95% CI, −10.31, −1.34) and VM-plasty (MD −6.36,95% CI, −16.77, −4.04) were inferior to DB-MPFLR. The effects of all surgeries were ranked with SUCRA probabilities in Table 3, and DB-MPFLR had the greatest probability (SUCRA 96.5%) for being the best treatment option on Kujala score, followed by the SB-MPFLR (SUCRA 57.4%), VM-plasty(SUCRA 55.5%)and MR-plasty (SUCRA 42.0%), MC-reefing ranked in the sixth position (SUCRA 28.5%) and MR-plication ranked the last (SUCRA 9.9%).
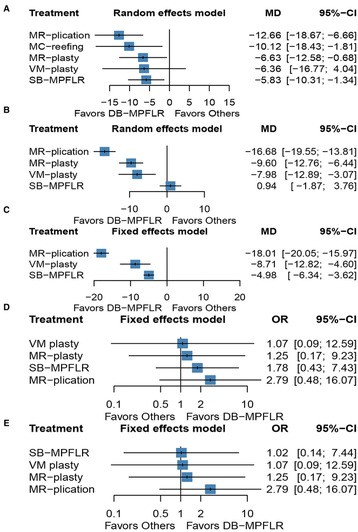
Figure 2. Forest plot of different surgeries: (A) kujala score; (B) lysholm score; (C) IKDC score; (D): redislocation; (E) recurrent instability.
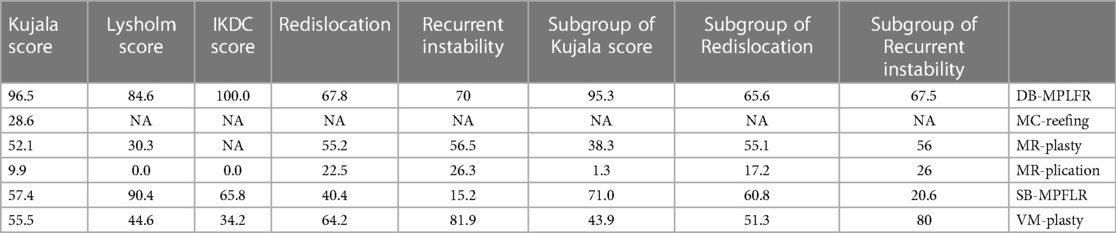
Table 3. Ranking of surgeries based on probability of their protective effects on all outcomes according to the SUCRA. Larger probability, stronger protective effects.
Lysholm score
Six studies reported Lysholm scores as one of the study outcomes. I2 = 42.1%, so we chosen the random effects model. Figure 2B shows the MD and 95% CI, of each surgery compared with DB-MPFLR. MR-plasty (MD −9.6,95% CI, −11.08, −8.12), MR-plication (MD −16.68,95% CI, −19.55, −13.81), and VM-plasty (MD −7.98,95% CI, −12.89, −3.07) were inferior to DB-MPFLR. DB-MPFLR was not superior to SB-MPFR (MD 0.94, 95% CI, −1.87, 3.76). As shown Table 3, SB-MPFLR had the highest probability of being the best treatment option (SUCRA 90.4%) followed by DB-MPFLR (SUCRA 84.6%). MR-plasty (SUCRA 30.3%) and MPR-plication(SUCRA 0.0%) ranked in the fourth and fifth positions behind the and VM-reefing(SUCRA 44.0%).
IKDC score
Five studies reported IKDC scores as one of the study outcomes. I2 = 24.4%, so we chosen the fixed effects model. Figure 2C show the MD and 95% CI of each surgery compared with DB-MPFLR. MR-plication (MD −18.01,95% CI, −20.05, −15.97), SB-MPFLR (MD −4.98, 95% CI, −6.34, −3.62) and VM-plasty (MD −8.71,95% CI, −12.82, −4.60) were inferior to DB-MPFLR. DB-MPFLR was at the top-ranking position (SUCRA 100.0%) shown in Table 3 followed by SB-MPFLR (SUCRA 65.8%). Two of the least effective treatments for IKDC Score were VM-plasty (SUCRA 34.2%) and MPR-plication (SUCRA 0.0%).
Redislocation
Nine studies reported redislocation as one of the study outcomes. I2 = 0.0%, so we chosen the fixed effects model. Figure 2D shows the OR and 95% CI of each surgery compared with DB-MPFLR. DB-MPFLR has no significant advantage over other surgical procedures in preventing redislocation, although it is the most likely intervention to be the best (SUCRA 67.8% shown in Table 3).
Recurrent instability
Eight studies reported recurrent instability as one of the study outcomes. I2 = 0.0%, so we chosen the fixed effects model. Figure 2E shows the OR and 95% CI of each surgery compared with DB-MPFLR. All the methods are not obviously inferior to DB-MPFLR. Even DB-MPFLR(SUCRA 70%) is less likely than VM-plasty(SUCRA 81.9%) to be the best intervention shown in shown in Table 3.
Subgroup
Since the clinical studies which reported Lyshlom and IKDC scores were all about recurrent patellar dislocation, we only conducted a subgroup analysis of Kujala score, redislocation, and recurrent instability. The results of the subgroup analysis were similar to those of the previous analysis. Detailed results are shown in Supplementary Appendix C and Table 3.
Publication bias
The comparison-adjusted funnel plots are displayed in Figures 3A–E. For the funnel plot of Kujala score, the outcomes showed obvious asymmetry, indicating a certain publication bias. The existence of points at the bottom of all funnel plots indicates that these outcomes all have small-study effects in the included studies.
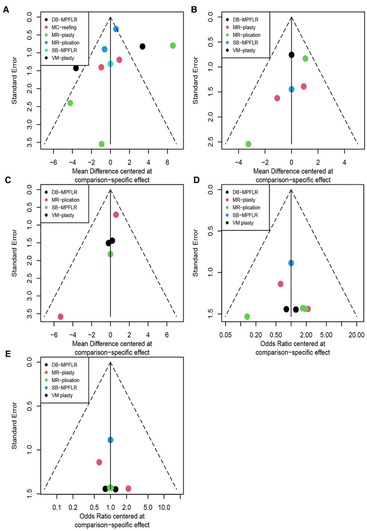
Figure 3. Adjusted funnel plot of different surgeries: (A) kujala score; (B) lysholm score; (C) IKDC score; (D) redislocation; (E) recurrent instability.
Network plots
Trial network plots are shown in Figures 4A–E. The width of the line indicates the number of studies in which the two interventions are connected, and the size of the node indicates the number of patients receiving the intervention. Since there is no closed loop in each trial network plot, there is no inconsistency in NMA, and we only choose the consistency model.
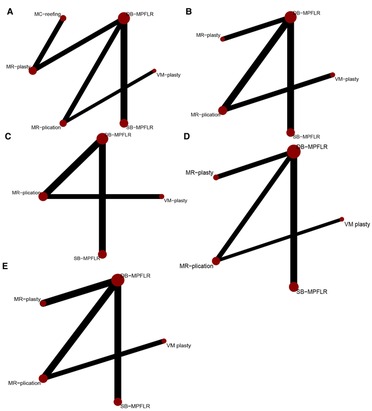
Figure 4. Network plot of treatment comparisons: (A) kujala score; (B) lysholm score; (C) IKDC score; (D) redislocation; (E) recurrent instability.
CINeMA assessment
For the vast majority of interventions, the quality of evidence was “low” across the five outcome indicators. The comparisons of MC-reefing with DB-MPFLR and MR-plasty achieved very low
quality of evidence for the outcome of Kujala scores; the comparison of MR-plication with VM plasty achieved very low quality of evidence for the outcome of Recurrent instability (details were shown in Supplementary Appendix D).
Comparison of pair-wise meta-analysis and network meta-analysis
The comparison of pair-wise meta-analysis and network meta-analysis revealed that the results were generally consistent. This comparison between pair-wise meta-analysis and network meta-analysis confirmed the accuracy of the results.
Discussion
The most important finding of this study was that DB-MPFLR is a fairly good method, which greatly improves function scores. In pairwise meta-analysis, DB-MPFLR shows great advantages in three outcomes. However, this conclusion requires careful consideration as it is highly heterogeneous, which may lead to the serious risk of bias. Also, we found the source of heterogeneity through meta-analysis: studies that compare DB-MPFLR and MR-plasty. For network meta-analysis, DB-MPFLR achieves the highest SURCA not only for patellar dislocation but also in recurrent patellar dislocation subgroup, except Lysholm score and recurrent instability. DB-MPFLR ranked second only to SB-MPFLR In Lysholm score and VM-plasty in recurrent instability. However, no significant difference was achieved in the prevention of dislocation and recurrent instability compared with other treatments.
A study has shown elevated TT-TG distance, trochlear dysplasia, patella alta and so that 92% of 175 patients had MPFL injury after a first time acute patellar dislocation (11). Injured sites include the femoral attachment and the patellar attachment (12). Moreover, a biomechanical study showed that MPFL provides approximately 60% of the inward binding resistance against lateral patella displacement (13). There is good reason to suspect that MPFLR, which can directly repair the medial patellar ligament, may yield higher functional outcomes. Based on this, there are many clinical studies of MPFLR for patellar dislocation to verify whether this is an appropriate method. In many studies, some have found that MPFLR is not superior to other soft tissue surgeries, but others have concluded that MPFLR does result in better functional scores than other surgeries (14–16). Therefore, our study collected high-quality RCTs and finally confirmed that MPFLR can obtain higher functional scores.
In adults, MPFLR has shown promising results, however, alternative MPFLR techniques are urgently needed for the treatment of recurrent patellar dislocation in children and adolescents with open growth plates. Several studies have developed a minimally invasive reconstruction of the MPFL through the insertion of the medial patellofemoral growth plate (17, 18).
For recurrent patellar dislocation, MPFL also achieved good results compared to other procedures in this study. However, other studies have found that risk factors for recurrent patellar dislocation include many bony structural abnormalities, such as elevated TT-TG distance, trochlear dysplasia, patella alta and so on (19). This means that simply repairing the inner soft tissue may not be enough. A clinical study reported that MPFLR combined with Tibial Tubercle Osteotomy obtained patellar kinematics and better functional scores compared with isolated MPFLR in the surgical treatment of recurrent patellar instability in patients with a TT-TG distance of 17–20 mm (20). Another study reported that the use of arthroscopic deepening tracheoplasty combined with MPFLR is a safe, reliable and reproducible surgical option, considering the stability of surgical results, knee function scores and patient satisfaction (21). However, a study showed that MPFLR combined with tuberosities transposition is not superior to isolated MPFLR on Kujala score and KOOS score (22). Moreover, A SurveyMonkey survey of 50 active surgeons in the International Patella Femur Study Group (IPSG) revealed inconsistent results on whether to perform bone surgeries for patients with recurrent patellar dislocation with bone abnormalities (23). So the jury is still out on whether bony surgery is needed.
The type of bundle reconstructed (SB or DB) is also a critical issue worth considering when surgeons conduct MPFLR on patients with patellar dislocation to restore normal patellar function. As previously mentioned, the MPFL is located in the second layer of soft tissue on the medial side of the knee joint and consists of two bundles, the inferior-straight bundle and the superior-oblique bundle respectively (4). A cadaver study reported that the attachment point of the patellofemoral ligament on the side of the patella is flexible and extends from the upper pole of the patella to the midpoint of the patella in a fan shape (24). As mentioned in the literature, the static constraint of medial soft tissue mainly depends on the inferior-straight bundle, while the dynamic constraint mainly depends on the superior-oblique bundle (4). SB-MPFLR which is reconstructed with only one bundle lost the normal patella-femoral ligament anatomy shape and thus lost binding to a larger area, while DB-MPFLR which is reconstructed with two bundles maximally mimicked the fan-shaped structure of the original patellofemoral ligament and thus gaining better constraint on the patella and being able to produce better clinical results. There have been many clinical trials of DB-MPFLR or SB-MPFLR, and the result is that DB-MPFLR is superior to SB-MPFLR on function scores or complications (25–27). This is exactly consistent with the results of our meta-analysis. A RCT of DB-MPFLR was conducted for graft morphology (28). One group was Y-shaped graft, and the other group was C-shaped graft (28). The result is that Y-graft technique was superior to C-graft technique in knee function scores for double bundle anatomic MPFL reconstruction, at a follow-up of at least 2 years (28). Although we have addressed many issues regarding MPFLR, including indications and bundle selection. But there are also many problems left for us, such as graft selection, fixation selection and so on. Therefore, more, larger scale and higher quality clinical studies are needed to find a better way to conduct DB-MPFLR.
Patella dislocation is not only a problem with the medial ligament, but also with the lateral ligament. Many studies have explored DBMPFLR in combination with other procedures. Chang Liu et al. compared the efficacy of different lateral ligament treatments combined with DB-MPFLR, and concluded that lateral retinaculum plasty would achieve better efficacy than lateral retinacular release (29).
The included clinical studies compared the outcomes of different types of surgeries for patellar dislocation (30). We also performed a subgroup analysis of recurrent patellar dislocation. There have been previous meta-analyses comparing MPFLR with other soft tissue surgeries, but either the quality of the included studies was low or there were few studies included. Of course, there are also studies comparing DB-MPFLR and SB-MPFLR, but they are only qualitative analyses. Therefore, this study conducted a meta-analysis of RCTs and provided high-quality evidence for the selection of the most effective methods of surgery.
There are some limitations. The validity of meta-analysis is closely related to the quality of the included studies and the number of studies between each direct comparison. In our study, the number of original studies between each comparison is small, and a comparison between MR-plication and VM-plasty contains only one original study. Many studies also had few outcome measures, with only the kujala score reported in all studies. Although RCTs are all included in our studies, the randomization methods and whether to allocate hidden are not described in some studies. And the level of evidence in this study is low or very low. In this study, we only discussed soft tissue surgery for patellar dislocation, while bone surgery was not included, which reduced the source of heterogeneity to a certain extent but also reduced the clinical applicability of this study.
Conclusions
Our study demonstrates that MPFLR results in better functional scores than other soft tissue surgeries. Compared with SB-MPFLR, DB-MPFLR achieved higher scores in Kujala score and IKDC score, and lower scores only in Lysholm score.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MF: design and manuscript writing. ZC: provision of study material, data analysis, and provision of relevant references. YD, YZ and SC were responsible for revising the article and for data acquisition. YW, JG and LP: data analysis and interpretation. WX: conception, financial support, administrative support. YL: conception, financial support, administrative support. All authors approved the final version for publication.
Funding
This work was supported by the National Clinical Research Center for Geriatric Disorders (Xiangya Hospital, Grant No. 2021KFJJ02 and 2021LNJJ05), National Clinical Research Center for Orthopedics, Sports Medicine and Rehabilitation (2021-NCRC-CXJJ-PY-40), Science and Technology Innovation Program of Hunan Province (No. 2021RC3025), Innovation-Driven Project of Central University South (No. 2020CX045), the Independent Exploration, Innovation Project for Postgraduate Students of Central South University (No. 2021zzts1030), Exploration and Innovation Project for Undergraduate Students South University of Central (No. XCX2021046).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1003796/full#supplementary-material.
References
1. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. (2006) 13(3):184–8. doi: 10.1016/j.knee.2006.01.005
2. Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW. High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc. (2018) 26(4):1204–9. doi: 10.1007/s00167-017-4594-7
3. Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. (2004) 32(5):1114–21. doi: 10.1177/0363546503260788
4. Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. (2010) 18(11):1511–6. doi: 10.1007/s00167-010-1090-8
5. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ (Clinical research ed). (2019) 366:l4898. doi: 10.1136/bmj.l4898
6. Zhang Y, Huang L, Wang D, Ren P, Hong Q, Kang D. The Robins-I and the Nos Had Similar Reliability but Differed in Applicability: A Random Sampling Observational Studies of Systematic Reviews/Meta-Analysis. Journal of Evidence-Based Medicine. (2021) 14(2):112–22. doi: 10.1111/jebm.12427
7. Efthimiou O, Debray TP, van Valkenhoef G, Trelle S, Panayidou K, Moons KG, et al. Getreal in network meta-analysis: a review of the methodology. Res Synth Methods. (2016) 7(3):236–63. doi: 10.1002/jrsm.1195
8. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21(11):1539–58. doi: 10.1002/sim.1186
9. Salanti G, Ades A, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64(2):163–71. doi: 10.1016/j.jclinepi.2010.03.016
10. Nikolakopoulou A, Higgins JP, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. Cinema: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. (2020) 17(4):e1003082. doi: 10.1371/journal.pmed.1003082
11. Migliorini F, Pilone M, Eschweiler J, Marsilio E, Hildebrand F, Maffulli N. High Rates of Damage to the Medial Patellofemoral Ligament, Lateral Trochlea, and Patellar Crest after Acute Patellar Dislocation: Magnetic Resonance Imaging Analysis. Arthroscopy: the Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association. (2022) 38(8):2472–9. doi: 10.1016/j.arthro.2022.01.044
12. Jiang B, Qiao C, Shi Y, Ren Y, Han C, Zhu Y, et al. Evaluation of risk correlation between recurrence of patellar dislocation and damage to the medial patellofemoral ligament in different sites caused by primary patellar dislocation by mri: a meta-analysis. J Orthop Surg Res. (2020) 15(1):461. doi: 10.1186/s13018-020-01984-0
13. Desio SM, Burks RT, Bachus KN. Soft Tissue Restraints to Lateral Patellar Translation in the Human Knee. The American Journal of Sports Medicine (1998) 26(1):59–65. doi: 10.1177/03635465980260012701
14. Feng X, Wang F. Clinical outcomes of medial retinaculum plasty versus mpfl reconstruction with concomitant tibial tubercle transfer: a retrospective study. Arch Orthop Trauma Surg. (2020) 140(11):1759–66. doi: 10.1007/s00402-020-03556-7
15. Wang XL, Wang XL, Peng C, Yang JJ, Hua GJ, Liu YP. Comparative study of three different combination surgical methods for recurrent Patella dislocation. J Orthop Sci. (2020) 25(6):1067–71. doi: 10.1016/j.jos.2020.01.008
16. Yeung M, Leblanc MC, Ayeni OR, Khan M, Hiemstra LA, Kerslake S, et al. Indications for Medial Patellofemoral Ligament Reconstruction: A Systematic Review. The Journal of Knee Surgery (2016) 29(7):543–54. doi: 10.1055/s-0035-1564730
17. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. (2013) 41(1):58–63. doi: 10.1177/0363546512463683
18. Nelitz M, Dreyhaupt J, Williams SRM. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents using a pedicled quadriceps tendon graft shows favourable results at a Minimum of 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. (2018) 26(4):1210–5. doi: 10.1007/s00167-017-4597-4
19. Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. (2017) 45(9):2105–10. doi: 10.1177/0363546517704178
20. Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, Granata GSM Jr., Kubota MS, et al. Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy. (2019) 35(2):566–74. doi: 10.1016/j.arthro.2018.10.109
21. Blønd L, Haugegaard M. Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent Patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. (2014) 22(10):2484–90. doi: 10.1007/s00167-013-2422-2
22. Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J. Clinical outcome in mpfl reconstruction with and without tuberositas transposition. Knee Surg Sports Traumatol Arthrosc. (2017) 25(9):2708–14. doi: 10.1007/s00167-015-3654-0
23. Liu JN, Steinhaus ME, Kalbian IL, Post WR, Green DW, Strickland SM, et al. Patellar instability management: a survey of the international patellofemoral study group. Am J Sports Med. (2018) 46(13):3299–306. doi: 10.1177/0363546517732045
24. Steensen RN, Dopirak RM, McDonald WG 3rd. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. (2004) 32(6):1509–13. doi: 10.1177/0363546503261505
25. Marteau E, Burdin P, Brilhault JM. Gracilis tendon transfer associated with distal alignment for Patella Alta with recurrent dislocations: an original surgical technique. Orthop Traumatol Surg Res. (2011) 97(4Suppl):S5–S11. doi: 10.1016/j.otsr.2011.03.013
26. Steensen RN, Dopirak RM, Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy. (2005) 21(3):365–70. doi: 10.1016/j.arthro.2004.10.007
27. Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, et al. Double-Bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. (2013) 37(4):617–24. doi: 10.1007/s00264-013-1788-6
28. Kang H, Cao J, Yu D, Zheng Z, Wang F. Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: a prospective randomized study. Am J Sports Med. (2013) 41(5):1013–21. doi: 10.1177/0363546513480468
29. Liu C, Duan G, Niu Y, Cao P, Fu K, Niu J, et al. Lateral retinaculum plasty instead of lateral retinacular release with concomitant medial patellofemoral ligament reconstruction can achieve better results for patellar dislocation. Knee Surg Sports Traumatol Arthrosc. (2018) 26:2899–905. doi: 10.1007/s00167-017-4798-x
30. Malatray M, Magnussen R, Lustig S, Servien E. Lateral retinacular release is not recommended in association to mpfl reconstruction in recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. (2019) 27:2659–64. doi: 10.1007/s00167-018-5294-7
31. Du H, Tian XX, Guo FQ, Li XM, Ji TT, Li B, et al. Evaluation of different surgical methods in treating recurrent patella dislocation after three-dimensional reconstruction. Int Orthop. (2017) 41(12):2517–24. doi: 10.1007/s00264-017-3552-9
32. Zhao J, Huangfu X, He Y. The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med. (2012) 40(6):1355–64. doi: 10.1177/0363546512439193
33. Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy. (2013) 29(5):891–7. doi: 10.1016/j.arthro.2013.01.030
34. Niu Y, Wang X, Liu C, Wang X, Dong Z, Niu J, et al. Double-Bundle Anatomical Medial Patellofemoral Ligament Reconstruction with Lateral Retinaculum Plasty Can Lead to Good Outcomes in Patients with Patellar Dislocation. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal of the ESSKA (2018) 26(9):2743–9. doi: 10.1007/s00167-017-4720-6
35. Li J, Li Z, Wang K, Liu C, Wang Y, Wang H. Medial patellofemoral ligament reconstruction: a comparison of single-bundle transpatellar tunnel and double-anchor anatomic techniques for the treatment of recurrent lateral patellar dislocation in adults. Arthroscopy. (2019) 35(3):845–54. doi: 10.1016/j.arthro.2018.08.050
36. Ercan N, Akmese R, Ulusoy B. Single-tunnel and double-tunnel medial patellofemoral ligament reconstructions have similar clinical. Radiological and Functional Results. Knee Surg Sports Traumatol Arthrosc. (2021) 29(6):1904–12. doi: 10.1007/s00167-020-06260-6
37. Astur DC, Gouveia GB, Borges JH, Astur N, Arliani GG, Kaleka CC, et al. Medial patellofemoral ligament reconstruction: a longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J. (2015) 9:198–203. doi: 10.2174/1874325001509010198
38. Zhao J, Huangfu X, He Y, Liu W. Recurrent patellar dislocation in adolescents: medial retinaculum plication versus Vastus Medialis plasty. Am J Sports Med. (2012) 40(1):123–32. doi: 10.1177/0363546511420551
39. Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Ji G, et al. Medial patellar retinaculum plasty versus medial capsule reefing for patellar subluxation in adult. Orthop Surg. (2012) 4(2):83–8. doi: 10.1111/j.1757-7861.2012.00178.x
Keywords: network meta-analysis, medial patellofemoral ligament reconstruction, medial soft tissue surgery, single bundle, double bundle, patellar dislocation
Citation: Fang M, Cai Z, Pan L, Ding Y, Zhang Y, Cheng S, Wang Y, Gao J, Li Y and Xiao W (2023) Surgical treatment of patellar dislocation: A network meta-analysis of randomized control trials and cohort studies. Front. Surg. 10:1003796. doi: 10.3389/fsurg.2023.1003796
Received: 26 July 2022; Accepted: 15 March 2023;
Published: 30 March 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
Lin Guo, Army Medical University, ChinaZiji Zhang, The First Affiliated Hospital of Sun Yat-sen University, China
© 2023 Fang, Cai, Pan, Ding, Zhang, Cheng, Wang, Gao, Li and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yusheng Li bGl5dXNoZW5nQGNzdS5lZHUuY24= Wenfeng Xiao eGlhb3dlbmZlbmdAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Mingqing Fang
Mingqing Fang Zijun Cai
Zijun Cai Linyuan Pan
Linyuan Pan Yilan Ding
Yilan Ding Yueyao Zhang3
Yueyao Zhang3 Yusheng Li
Yusheng Li Wenfeng Xiao
Wenfeng Xiao