
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 06 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.994795
 Jinchang Han1,2,†
Jinchang Han1,2,† Xiao-yu Zhang1,2,†
Xiao-yu Zhang1,2,† Shi-yin Mu3
Shi-yin Mu3 Shi-long Liu1,2
Shi-long Liu1,2 Qing-tong Cui1,2
Qing-tong Cui1,2 Chao Zhang1,2
Chao Zhang1,2 Ai-feng Liu1,2*‡
Ai-feng Liu1,2*‡
Objective: The aim of this study was to identify the influence of a tourniquet on the blood loss, transfusion requirement, swelling, pain, knee function, range of motion (ROM), operation time, bone cement mantle thickness, and complications in patients operated with total knee arthroplasty (TKA).
Methods: Two authors independently retrieved PubMed, Embase, and CENTRAL to identify eligible randomized controlled trials (RCTs) evaluating the effectiveness of a tourniquet in TKA. Fixed- (I2 < 50%) or random-effects (I2 > 50%) models were selected to perform meta-analysis according to the value of I2. Mean difference (MD) and risk ratio were selected as the effect sizes for continuous and dichotomous variables, respectively.
Results: A total of 29 RCTs, involving 2,512 operations (1,258 procedures with a tourniquet and 1,254 procedures without a tourniquet), were included, and 18 outcomes were compared. Tourniquet application could significantly decrease intraoperative blood loss (MD = −138.72 ml, p < 0.001), shorten operation duration (MD = −1.77 min, p < 0.001), and increase cement mantle thickness (MD = 0.17 mm, p < 0.001). However, it was significantly associated with increased postoperative pain intensity, decreased full ROM/flexion ROM/extension ROM, poorer knee function, increased knee swelling, and increased length of hospital stay (LOS) at several follow-up points (p < 0.050). No significant difference was found for postoperative draining volume, total blood loss, transfusion rate, change of Hb level, and risks of deep venous thrombosis and all complications.
Conclusions: Tourniquet application could only decrease the intraoperative blood loss but has no effectiveness on the total blood loss and transfusion requirement. On the contrary, it has a reverse effect on the pain score, knee function, ROM, swelling, and LOS.
Total knee arthroplasty (TKA) has been shown to be with a satisfaction rate of up to 91%, for patients with end-stage knee osteoarthritis (1, 2). A successful TKA procedure depends on multiple critical factors, among which the bloodless operation field is an important factor to guarantee a full visualization during operation, decrease blood loss and requirement of blood transfusion, and reduce operation time (3, 4). Various strategies have been deployed to reduce intraoperative blood loss in TKA, including iron therapy, administration of erythropoietin, controlled hypotension, local or systemic administration of tranexamic acid (TXA), and application of a tourniquet (4–6). The pneumatic tourniquet was first applied in surgery as described by Cushing et al. (3) in 1904. In the recent publications, over half of surgeons prefer to use a tourniquet during TKA (7, 8).
However, although the tourniquet is widely accepted by many orthopedic surgeons, results from clinical trials remain controversial (4, 9–12). There are a growing body of studies that have raised some concerns about the tourniquet application during TKA, mainly for the increased risks of postoperative pain, reperfusion injury, limb swelling, deep venous thrombosis (DVT), wound complication, and peripheral nerve injury (9–11). In a meta-analysis conducted by Cai et al. (4) in 2019, 11 primary randomized controlled trials (RCTs) involving 541 patients were included for analysis, showing that tourniquet application during TKA could only decrease the intraoperative blood loss and calculated blood loss, but has no effectiveness on postoperative blood loss, transfusion rate, total blood loss, and risk of DVT. Smith and Hing (12) conducted a meta-analysis based on 15 RCTs or non-RCTs, presenting that tourniquet-assisted TKA was associated with a significantly increased intraoperative blood loss compared to the non-tourniquet-assisted group. No significance was found for the total blood loss and overall transfusion rate. However, the application of a tourniquet was related with a trend of increased complications. In recent years, plenty of new studies have been published to discuss the effectiveness of tourniquet application in TKA, but no consensus has been reached until now.
Thus, in response to this confusion about the use of a tourniquet, this meta-analysis was aimed to identify the influence of a tourniquet on the blood loss, transfusion requirement, swelling, pain, knee function, range of motion (ROM), operation time, bone cement mantle thickness, and complications in patients operated with TKA. The working hypothesis of this review is that the application of a tourniquet could reduce blood loss and transfusion requirement but can have adverse effects on swelling, pain, knee function, ROM, operation time, bone cement mantle thickness, and complications in primary TKA.
The current review was conducted according to the PRISMA statement (13). Two authors searched the electronic databases of PubMed, Embase, and Cochrane Library independently to identify potentially related records. The key words include “total knee arthroplasty” and “tourniquet.” We conducted the search on the platforms using a method of combining the “subject term” and “free terms.” There was no restriction on the publication years (from inception of the databases to year of 2021) and publication countries.
The records retrieved from the electronic databases were screened for eligibility when fulfilling the following criteria: (1) participants: undergone TKA for knee osteoarthritis; (2) intervention and comparison: the TKA was assisted with or without a tourniquet during operation; (3) outcome: studies reported outcome data about blood loss, transfusion requirement, swelling, pain, knee function, ROM, operation time, bone cement mantle thickness, complications, and so on; (4) study: only RCTs with high quality were included.
Studies were excluded for the following reasons: (1) duplicated records; (2) studies published in non-English language; (3) studies for patients with diagnosis other than knee osteoarthritis; (4) non-RCTs, including cohort study, nonrandomized clinical trial, case–control study, case series, literature review, and meta-analysis.
Two authors independently screened the records to identify eligible studies. First, all available records were checked to remove the duplicates. The remaining records were then evaluated for potential eligibility by screening the titles/abstracts and the full text, in turn.
Two reviewers extracted the related information independently. In case of diversity on the extracted data between two reviewers, a third senior author would participate in the discussion. The following data were extracted: (1) Study information: first author's name, year of publication, publication country, and study period; (2) Patients’ information: sample size, number of dropped patients, sex, average age, body mass index (BMI), and follow-up time; (3) Intervention information: tourniquet product, tourniquet pressure applied, prostheses types, type and volume of cement, postoperative thromboprophylaxis, and other management of intraoperative bleeding; (4) Clinical outcomes: data about the operation time, intraoperative blood loss, draining volume, total blood loss, change of hemoglobin (Hb) level, transfusion requirement, length of hospital stay (LOS), bone cement mantle thickness, visual analog scale (VAS)-pain score, ROM, Knee Society Score (KSS), Oxford knee score, knee swelling, and risks of DVT and all recorded complications.
The risk of bias of primary RCTs was evaluated using the Cochrane Collaboration tool (14), by two individual authors.
For those variables reported as mean ± standard deviation (SD), the mean difference (MD) as well as 95% confidence interval (95% CI) were selected as the effect size, while for those outcomes reported as percentage or dichotomous variable, risk ratio (RR) was selected as effect size. Random- (I2 > 50%) or fixed-effects (I2 < 50%) models would be selected according to the between-study heterogeneity test.
For the continuous variables, subgroup meta-analyses were performed at different follow-up points and were displayed in line charts. In each meta-analysis with significant heterogeneity, if three or more studies were included, sensitivity analysis was conducted to detect studies causing unstability. Publication bias tests, including Begg's test (p < 0.050) and Egger's test (p < 0.100), were performed, when five or more studies were included (15). When significant publication bias was detected, a nonparametric trim-and-fill method would be used to adjust the bias.
The above procedures were performed with R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided p value of <0.05 was defined as statistical significance.
The search and screening flowchart is presented in Figure 1. First, 1,499 records were identified through database retrieval and manual search. After excluding 323 duplicates, 1,069 titles/abstracts were excluded. The remaining 107 were assessed by reading the full text, 78 of which were excluded with various reasons. Finally, a total of 29 RCTs (9, 16–42) were eligible for final inclusion in qualitative synthesis and quantitative meta-analysis.
Table 1 presents the summary of the included studies. A total of 2,512 operations (2,393 patients, 119 patients conducted bilateral TKA) were included. With a tourniquet, 1,258 procedures were performed and 1,254 were performed without a tourniquet. The male percentages ranged from 14% to 70% in the tourniquet group and from 10.3% to 90% in the non-tourniquet group. The mean age at operation was available in all studies, ranging from 58.0 to 73.0 both in tourniquet and non-tourniquet groups. The BMI was available in 21 studies, ranging from 26.1 to 33.0 in the tourniquet group and from 25.3 to 33.0 in the non-tourniquet group. At the final follow-up, a total of 45 and 49 procedures were dropped out in the tourniquet and non-tourniquet groups, respectively.
Table 2 provides a list of detailed information about the operation, including tourniquet product, tourniquet pressure, prosthesis and bone cement used for TKA, postoperative thromboprophylaxis, and other management of intraoperative bleeding. The tourniquet pressure was reported in 24 trials. In general, they applied a higher pressure of 100–150 mmHg than systolic blood pressure (SBP) or an absolute pressure of 250–380 mmHg.
Figure 2 shows the results of assessment on the risk of bias. Generally, no obvious risk of bias was demonstrated in these trials. Only a few studies have high risk of bias, on the domains 2 (allocation concealment), 3 (blinding of participants), and 6 (selective reporting).
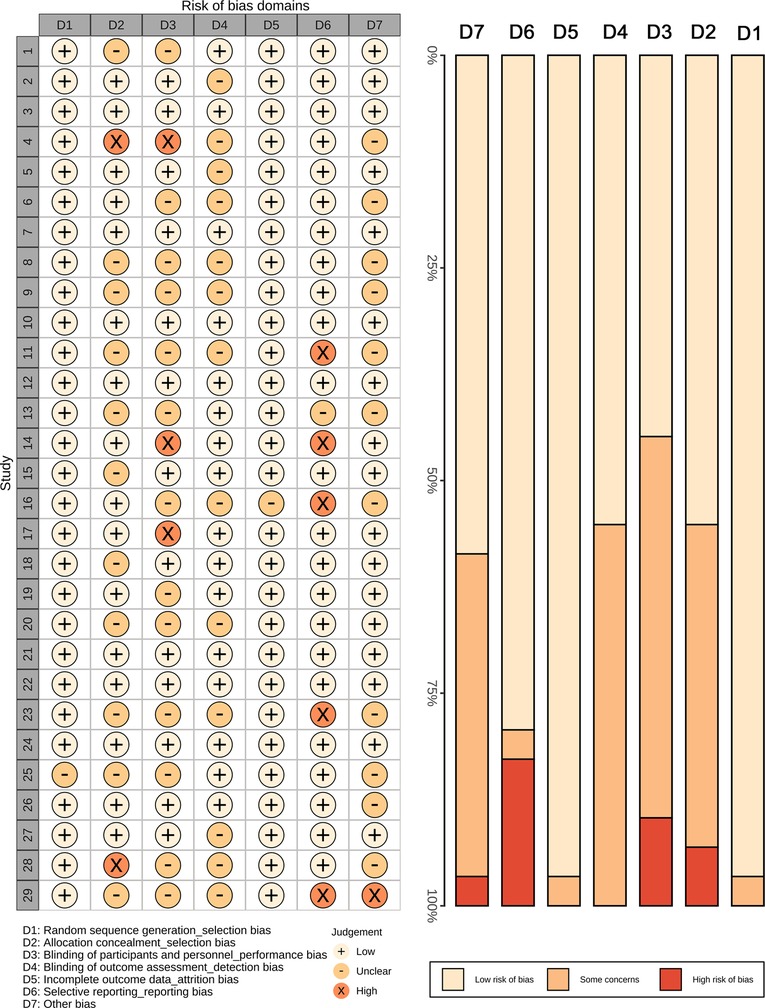
Figure 2. The risk of bias summary plot and bar chart for risk of bias assessment. A total of seven domains were assessed. A few studies have high risk of bias concerning the allocation concealment, blinding of participants, selective report, and other bias.
A total of 18 outcomes were compared in this study, and the results of meta-analyses as well as the additional analyses (heterogeneity analysis, sensitivity analysis, and publication bias test) are presented in Supplementary Table S1.
Several outcomes were reported at different follow-up points, including VAS-pain score, full ROM, flexion ROM, extension ROM, KSS, percentage of hematocrit (HCT), Oxford knee score, and knee circumference. Thus, subgroup meta-analyses were performed for these outcomes according to the follow-up period (Figure 3). As a result, application of a tourniquet was significantly associated with higher VAS-pain score, at the 1st day, 2nd day, 3rd day, 4th day, 5th day, 1st week, and 3rd week, compared to that of the non-tourniquet group (Figure 3A). Concerning the postoperative ROM, the tourniquet group was associated with significantly decreased full ROM (at the 1st day, 3rd day, and 6th week, Figure 3B), flexion ROM (at the 3rd day, Figure 3C), and extension ROM (at the 6th week and 8th month, Figure 3D). The application of a tourniquet was also related with poorer knee outcome according to KSS at the 3rd week, 6th week, and 3rd month (Figure 3E). The percentage of HCT was significantly lower at the 3rd day postoperatively in the tourniquet group (Figure 3F). The Oxford knee score was higher in the tourniquet group only at the 6th month postoperatively (Figure 3G). Increased swelling was demonstrated for application of tourniquet at the 3rd day and 6th month according to knee circumference (Figure 3H).
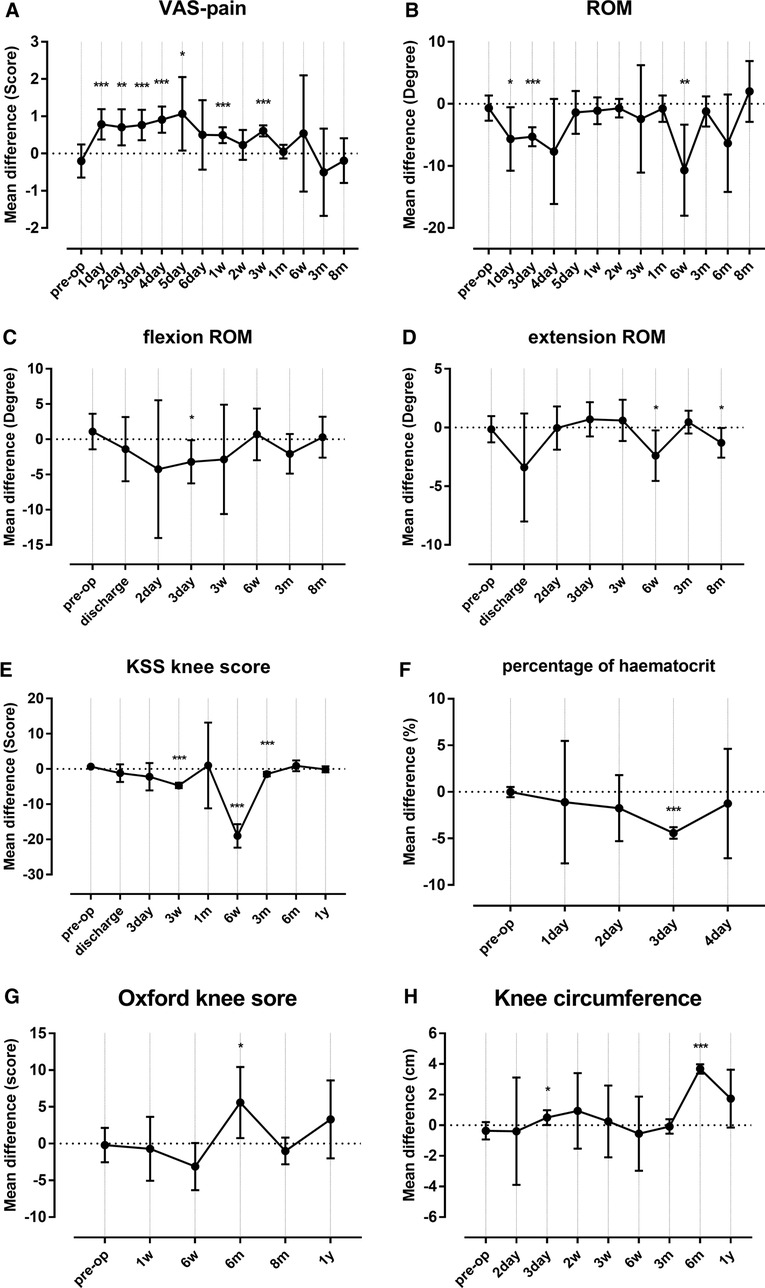
Figure 3. Results for subgroup meta-analyses for outcomes including VAS-pain score (A), ROM (B), flexion ROM (C), extension ROM (D), KSS (E), percentage of HCT (F), Oxford knee score (G), and knee circumference (H). The error bars in the plot represent mean ± 95%CI. *P < 0.050, **P < 0.010, ***P < 0.001. VAS, visual analog scale; ROM, range of motion; KSS, Knee Society Score; HCT, hematocrit.
The forest plot for comparison of operation time is shown in Supplementary Figure S1. A total of 19 studies were included, presenting that a significantly shorter period was required in TKA with assistance of a tourniquet than TKA without a tourniquet (MD = −1.77 min, 95% CI: −2.61 to −0.93, p < 0.001). The forest plot for LOS is presented in Figure 4A, showing increased LOS after application of a tourniquet (MD = 0.59 days, 95% CI: 0.29–0.90, p < 0.001).
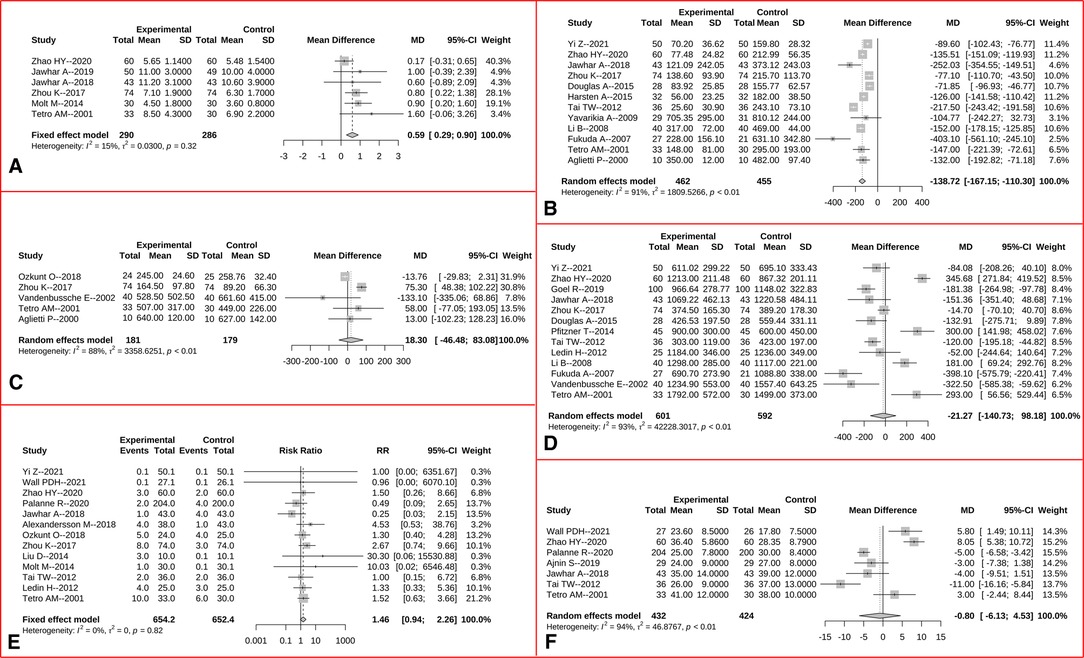
Figure 4. Forest plots for comparisons of length of hospital stay (A), intraoperative blood loss (B), draining volume (C), total blood loss (D), transfusion rate (E), and hemoglobin change (F) between the tourniquet (experimental) and non-tourniquet (control) groups. The I2 were 15%, 91%, 88%, 93%, 0%, and 94% for the fixed-effects, random-effects, random-effects, random-effects, fixed-effects, and random-effect models, respectively.
The intraoperative blood loss was significantly decreased after tourniquet application (MD = −138.72 ml, 95% CI: −167.12 to −110.30, p < 0.001, Figure 4B). However, no significant difference was found between two groups for postoperative draining volume (MD = 18.30 ml, 95% CI: −46.48 to 83.08, p = 0.580, Figure 4C), total blood loss (MD = −21.27 ml, 95% CI: −140.73 to 98.18, p = 0.727, Figure 4D), rate of blood transfusion (RR = 1.46, 95% CI: 0.94–2.26, p = 0.095, Figure 4E), and change of the lowest level of Hb compared to baseline level (MD = −0.80 g/L, 95%CI: −6.13 to 4.53, p = 0.769, Figure 4F).
Data about bone cement mantle thickness were available in five studies, and the corresponding forest plot is presented in Figure 5. As a result, tourniquet application during TKA was related with a significantly increased thickness of bone cement (MD = 0.17 mm, 95% CI: 0.11–0.23, p < 0.001, Figure 5).
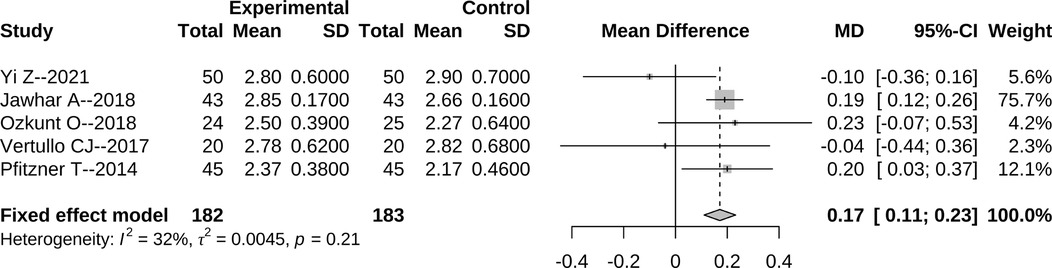
Figure 5. Forest plot for comparison of bone cement mantle thickness between the tourniquet (experimental) and non-tourniquet (control) groups. The I2 was 32%, and the fixed-effect model was selected.
The risk of DVT was reported in 12 trials, and an overall similar rate of DVT was found between two groups (RR = 1.22, 95% CI: 0.86–1.72, p = 0.261, Figure 6A). The frequency of all recorded complications were reported in 16 studies, and no significant difference between two group was demonstrated (RR = 1.19, 95% CI: 0.96–1.49, p = 0.118, Figure 6B).
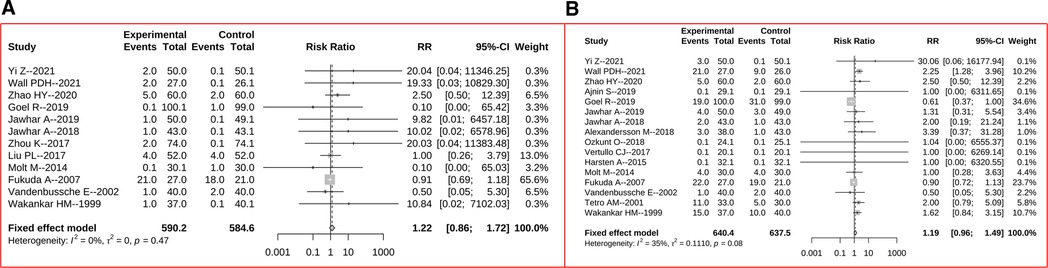
Figure 6. Forest plots for comparisons of risk of DVT (A) and risk of all complications (B) between the tourniquet (experimental) and non-tourniquet (control) groups. The I2 were 0% and 35%, and fixed-effect models were selected, respectively.
When significant heterogeneity was detected in a meta-analysis with more than three studies, sensitivity analysis was performed. As a result, two, one, and three studies were detected to cause significant nonstability to the pooling results, for outcomes of operation time, draining volume, and LOS, respectively (Supplementary Table S1). Thus, these studies were excluded from the final forest plots.
Significant publication bias was found for risk of DVT, according to Egger's test (p = 0.088 < 0.100, Supplementary Table S1). The nonparametric trim-and-fill method adjusted the publication bias, and the adjusted effect size was RR = 0.929 (95% CI: 0.720–1.197, p = 0.568, I2 = 0.0%, fixed-effect model) after adding four studies. The funnel plot of the trim-and-fill process is available in Supplementary Figure S2.
The use of a tourniquet in TKA is controversial, with proponents of tourniquet use claiming possible benefits such as less blood loss, shorter operation time, and thicker cement penetration, while the opponents were concerned about the potential disadvantages of tourniquet application such as increased postoperative pain intensity, increased knee swelling, higher risk of thromboembolic events, and poorer knee function (43). Thus, the exact effectiveness of a tourniquet is not clear now, with conflicting evidence available in recent literature. The main results of the current study include the following: (1) tourniquet application could decrease intraoperative blood loss, shorten operation duration, and increase cement mantle thickness significantly; (2) tourniquet application was significantly associated with increased postoperative pain intensity, decreased full ROM/flexion ROM/extension ROM, poorer knee function, increased knee welling, and increased LOS; (3) no significant difference was found for postoperative draining volume, total blood loss, transfusion rate, change of Hb level, and risks of DVT and all complications.
Extensive blood loss is a major concerning during TKA for orthopedic surgeons, which may cause poor vision during operation and increase the difficulty of operation and risk of injury to some important structures. Thus, various blood-saving techniques have been applied for reducing the intraoperative blood loss. In our study, we confirmed that tourniquet could effectively reduce the intraoperative blood loss, with a mean volume of 138.72 ml, during TKA. Additionally, the operation time was shorter after applying the tourniquet, which may be due to the better intraoperative visualization. It is easy to speculate that tourniquet application is associated with more clear surgical field and can help the surgeons more easily distinguish the anatomical structures, which is great importance for shortening the operation time. However, considering from clinical perspective, the magnitude of the decreased operation time was of no practical significance, as only an average period of 1.77 (95% CI: 0.93–2.61) min was saved. In the meta-analysis of Cai et al. (4), they also showed a similar value of operation time saved in TKA with the assistance of tourniquet (average: 1.08 min, 95% CI: 0.66–1.50 min).
Although many studies have shown decreased intraoperative blood loss with the use of a tourniquet, mixed results have been reported for postoperative and total blood loss. Smith and Hing (12) reported an average of 269 ml increased intraoperative blood loss when no tourniquet was used, while no significant difference was found on the total blood loss and transfusion requirements. Li et al. (44) compared the clinical outcomes of patients who had undergone TKA with or without tourniquet, showing that the tourniquet application was related to decreased intraoperative blood loss, with similar draining volume, total blood loss, and transfusion requirement. In our results, regarding the postoperative draining volume, total blood loss, transfusion rate, and change of Hb level, no significant difference was demonstrated between two groups. On the other hand, some other studies have pointed out that tourniquet application would increase the postoperative hidden blood loss or draining volume (27, 44, 45). Thus, tourniquet application has no influence on the total blood loss and has no effectiveness on reducing transfusion requirement, but only reduces intraoperative bleeding.
We found pain intensity was significantly lower in the non-tourniquet group especially within 3 weeks postoperatively. This may be due to the application of tourniquet that squeezes the thigh and restricts blood flow during operation (7, 46, 47). On the same time, the damage of tourniquet during operation may also cause risk of DVT and knee swelling. This study found a significant increase in knee circumference in the tourniquet group at several follow-ups. However, we did not detect significant difference on frequencies of DVT between the two groups. It could be speculated that the power to detect the difference was insufficient due to low incidences of DVT in both groups. Additionally, an average increase of 0.59 days was calculated for the LOS in the tourniquet group, due to increased pain, delayed rehabilitation, and other reverse effects of the tourniquet. For instance, patients operated with tourniquet assistance were found to be with decreased ROM, and KSS, which could be explained by comparatively more swelling and pain in the postoperative period. This is similar with other previous studies (35, 37, 39), which reported that ROM was reduced in the tourniquet group, even at a period as long as 2 years after TKA.
The bone cement mantle thickness is important for the stability of prostheses following primary TKA (48, 49). Increased thickness of the bone cement has been reported to improve the survival and stability of the prosthesis (50, 51). The cement thickness of 3–4 mm between the tibial component and the trabecular bone is considered to be the best status to avoid osteolysis of the surrounding bone and loosening of the prosthesis (52). Previous studies have presented inconsistent results regarding the effect of tourniquet application on the bone cement thickness (16, 24, 26, 29, 32). Yao et al. (53) evaluated the effect of tourniquet application on cement penetration in primary TKA, and they found that there was no influence on cement penetration; the tourniquet application has no effect on reducing blood loss, easing knee pain and improving knee function. In the results of our study, we found a thicker bone cement mantle in the tourniquet group (mean value: 0.17 mm).
Another strategy selected by many surgeons is to inflate the tourniquet during the cementation process of prosthesis, with the aim of decreasing the tourniquet time (54, 55). In the network meta-analysis published by Cao et al. (54), the efficacy and safety of different tourniquet protocols in TKA were compared, showing that a tourniquet during the entire operation process can effectively reduce blood loss but also may cause many safety problems, including DVTs, wound oozing, delayed healing, and serious wound complications, while tourniquet inflation before osteotomy and then deflation after wound closure can effectively shorten the operation time, reduce perioperative bleeding, and reduce postoperative complications.
This study, however, has some limitations that we need to point out. First, as several outcomes were reported at many follow-up periods, we must perform subgroup meta-analyses according to different follow-ups. As a result, the number of primary trials included in each meta-analysis was quite small. Second, some differences on the operation procedure, such as tourniquet products, tourniquet pressure, and type of prosthesis and cement, existed as presented in Table 2. Thus, we could only calculate an overall effect of size difference between the tourniquet and non-tourniquet groups. These may cause inevitable risk of bias to the results.
Basing on the available high-quality evidence, the current study demonstrated that tourniquet application could significantly decrease intraoperative blood loss, shorten operation duration, and increase cement mantle thickness. However, tourniquet application was significantly associated with increased postoperative pain intensity, decreased full ROM/flexion ROM/extension ROM, poorer knee function, increased knee welling, and increased LOS. No significant difference was found for postoperative draining volume, total blood loss, transfusion rate, change of Hb level, and risks of DVT and all complications. As a result, we recommend that the tourniquet should not be routinely applied during TKA, or surgeons could inflate the tourniquet only during the cementation process.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
JH, X-yZ, and S-yM: methodology, validation, formal analysis, investigation, data curation, writing-original draft, writing-reviewing and editing, and project administration. S-lL and Q-tC: investigation and data processing. CZ: validation and writing-reviewing and editing. A-fL: project administration. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the “Tuoxin Project” Funding of the first Affiliated Hospital of the Tianjin University of Traditional Chinese Medicine (No. YB202119). The sponsors or funders had no involvement in any parts of this study. All authors confirmed the independence of researchers from funding sources.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.994795/full#supplementary-material.
1. Themistoklis T, Theodosia V, Konstantinos K, Georgios DI. Perioperative blood management strategies for patients undergoing total knee replacement: where do we stand now? World J Orthop. (2017) 8:441–54. doi: 10.5312/wjo.v8.i6.441
2. Lange JK, Lee YY, Spiro SK, Haas SB. Satisfaction rates and quality of life changes following total knee arthroplasty in age-differentiated cohorts. J Arthroplasty. (2018) 33(5):1373–8. doi: 10.1016/j.arth.2017.12.031
3. Arthur JR, Spangehl MJ. Tourniquet use in total knee arthroplasty. J Knee Surg. (2019) 32(8):719–29. doi: 10.1055/s-0039-1681035
4. Cai DF, Fan QH, Zhong HH, Peng S, Song H. The effects of tourniquet use on blood loss in primary total knee arthroplasty for patients with osteoarthritis: a meta-analysis. J Orthop Surg Res. (2018) 14(1):348. doi: 10.1186/s13018-019-1422-4
5. Liu D, Dan M, Martinez Martos S, Beller E. Blood management strategies in total knee arthroplasty. Knee Surg Relat Res. (2016) 28:179–87. doi: 10.5792/ksrr.2016.28.3.179
6. Lu Q, Peng H, Zhou GJ, Yin D. Perioperative blood management strategies for total knee arthroplasty. Orthop Surg. (2018) 10:8–16. doi: 10.1111/os.12361
7. Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. (2014) 9:13. doi: 10.1186/1749-799X-9-13
8. National Joint Registry for England and Wales. National Joint Registry for England and Wales 1st annual report. (2004). Available at: https://nanopdf.com/download/1st-annual-report-national-joint-registry_pdf
9. Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE. Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res. (2016) 474(1):69–77. doi: 10.1007/s11999-015-4393-8
10. Tsubosaka M, Ishida K, Sasaki H, Shibanuma N, Kuroda R, Matsumoto T. Effects of suture and tourniquet on intraoperative kinematics in navigated total knee arthroplasty. J Arthroplasty. (2017) 32(6):1824–8. doi: 10.1016/j.arth.2017.01.033
11. Rathod P, Deshmukh A, Robinson J, Greiz M, Ranawat A, Rodriguez J. Does tourniquet time in primary total knee arthroplasty influence clinical recovery? J Knee Surg. (2015) 28(4):335–42. doi: 10.1055/s-0034-1388654
12. Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. (2010) 17(2):141–7. doi: 10.1016/j.knee.2009.06.007
13. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. (2009) 339:b2535. doi: 10.1136/bmj.b2535
14. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's Tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
15. Harsten A, Bandholm T, Kehlet H, Toksvig-Larsen S. Tourniquet versus no tourniquet on knee-extension strength early after fast-track total knee arthroplasty; a randomized controlled trial. Knee. (2015) 22(2):126–30. doi: 10.1016/j.knee.2014.12.010
16. Yi Z, Yan L, Haibo S, Yuangang W, Mingyang L, Yuan L, et al. Effects of tourniquet use on clinical outcomes and cement penetration in TKA when tranexamic acid administrated: a randomized controlled trial. BMC Musculoskelet Disord. (2021) 22(1):126. doi: 10.1186/s12891-021-03968-5
17. Wall PDH, Ahmed I, Edwin C, Farhan-Alanie MM, Parsons H, Price AJ, et al. Tourniquet use in total knee replacement surgery: a feasibility study and pilot randomised controlled trial (SAFE-TKR study). BMJ Open. (2021) 11(1):e043564. doi: 10.1136/bmjopen-2020-043564
18. Zhao HY, Yeersheng R, Kang XW, Xia YY, Kang PD, Wang WJ. The effect of tourniquet uses on total blood loss, early function, and pain after primary total knee arthroplasty: a prospective, randomized controlled trial. Bone Joint Res. (2020) 9(6):322–32. doi: 10.1302/2046-3758.96.BJR-2019-0180.R3
19. Palanne R, Rantasalo M, Vakkuri A, Madanat R, Olkkola KT, Lahtinen K, et al. Effects of anaesthesia method and tourniquet use on recovery following total knee arthroplasty: a randomised controlled study. Br J Anaesth. (2020) 125(5):762–72. doi: 10.1016/j.bja.2020.03.036
20. Ayik O, Demirel M, Birisik F, Ersen A, Balci HI, Sahinkaya T, et al. The effects of tourniquet application in total knee arthroplasty on the recovery of thigh muscle strength and clinical outcomes. J Knee Surg. (2020) 34(10):1057–63. doi: 10.1055/s-0040-1701454
21. Ajnin S, Fernandes R. Reduced length of stay and faster recovery after total knee arthroplasty without the use of tourniquet. J Clin Orthop Trauma. (2020) 11(1):129–32. doi: 10.1016/j.jcot.2019.08.016
22. Goel R, Rondon AJ, Sydnor K, Blevins K, O'Malley M, Purtill JJ, et al. Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: a prospective, double-blinded, randomized controlled trial. J Bone Joint Surg Am. (2019) 101(20):1821–8. doi: 10.2106/JBJS.19.00146
23. Jawhar A, Skeirek D, Stetzelberger V, Kollowa K, Obertacke U. No effect of tourniquet in primary total knee arthroplasty on muscle strength, functional outcome, patient satisfaction and health status: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. (2020) 28(4):1045–54. doi: 10.1007/s00167-019-05646-5
24. Jawhar A, Stetzelberger V, Kollowa K, Obertacke U. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2019) 27(7):2071–81. doi: 10.1007/s00167-018-5330-7
25. Alexandersson M, Wang EY, Eriksson S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the first 3 months after surgery: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. (2019) 27(4):1035–42. doi: 10.1007/s00167-018-5196-8
26. Ozkunt O, Sariyilmaz K, Gemalmaz HC, Dikici F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Medicine (Baltimore). (2018) 97(4):e9668. doi: 10.1097/MD.0000000000009668
27. Zhou K, Ling T, Wang H, Zhou Z, Shen B, Yang J, et al. Influence of tourniquet use in primary total knee arthroplasty with drainage: a prospective randomised controlled trial. J Orthop Surg Res. (2017) 12(1):172. doi: 10.1186/s13018-017-0683-z
28. Liu PL, Li DQ, Zhang YK, Lu QS, Ma L, Bao XZ, et al. Effects of unilateral tourniquet used in patients undergoing simultaneous bilateral total knee arthroplasty. Orthop Surg. (2017) 9(2):180–5. doi: 10.1111/os.12329
29. Vertullo CJ, Nagarajan M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg (Hong Kong). (2017) 25(1):2309499016684323. doi: 10.1177/2309499016684323
30. Kumar N, Yadav C, Singh S, Kumar A, Vaithlingam A, Yadav S. Evaluation of pain in bilateral total knee replacement with and without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. (2015) 6(2):85–8. doi: 10.1016/j.jcot.2015.01.095
31. Liu D, Graham D, Gillies K, Gillies RM. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res. (2014) 26(4):207–13. doi: 10.5792/ksrr.2014.26.4.207
32. Pfitzner T, von Roth P, Voerkelius N, Mayr H, Perka C, Hube R. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2016) 24(1):96–101. doi: 10.1007/s00167-014-3341-6
33. Molt M, Harsten A, Toksvig-Larsen S. The effect of tourniquet use on fixation quality in cemented total knee arthroplasty a prospective randomized clinical controlled RSA trial. Knee. (2014) 21(2):396–401. doi: 10.1016/j.knee.2013.10.008
34. Tai TW, Chang CW, Lai KA, Lin CJ, Yang CY. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. (2012) 94(24):2209–15. doi: 10.2106/JBJS.K.00813
35. Ledin H, Aspenberg P, Good L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. (2012) 83(5):499–503. doi: 10.3109/17453674.2012.727078
36. Yavarikia A, Amjad GG, Davoudpour K. The influence of tourniquet use and timing of its release on blood loss in total knee arthroplasty. Pak J Biol Sci. (2010) 13(5):249–52. doi: 10.3923/pjbs.2010.249.252
37. Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. (2009) 33(5):1263–8. doi: 10.1007/s00264-008-0647-3
38. Fukuda A, Hasegawa M, Kato K, Shi D, Sudo A, Uchida A. Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. (2007) 127(8):671–5. doi: 10.1007/s00402-006-0244-0
39. Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. (2002) 26(5):306–9. doi: 10.1007/s00264-002-0360-6
40. Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg. (2001) 44(1):33–8.11220796
41. Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. (2000) 371:169–77. doi: 10.1097/00003086-200002000-00021
42. Wakankar HM, Nicholl JE, Koka R, D'Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. (1999) 81(1):30–3. doi: 10.1302/0301-620X.81B1.0810030
43. Touzopoulos P, Ververidis A, Mpogiatzis C, Chatzigiannakis A, Drosos GI. The use of tourniquet may influence the cement mantle thickness under the tibial implant during total knee arthroplasty. Eur J Orthop Surg Traumatol. (2019) 29:869e75. doi: 10.1007/s00590-019-02369-8
44. Li Z, Liu D, Long G, Ke G, Xiao A, Tang P, et al. Association of tourniquet utilization with blood loss, rehabilitation, and complications in Chinese obese patients undergoing total knee arthroplasty: a retrospective study. Medicine (Baltimore). (2017) 96(49):e9030. doi: 10.1097/MD.0000000000009030
45. Mutlu S, Guler O, Mutlu H, Karaman O, Duymus TM, Parmaksizoglu AS. Tourniquet use during total knee arthroplasty does not offer significant benefit: a retrospective cohort study. Int J Surg. (2015) 18:123–7. doi: 10.1016/j.ijsu.2015.04.054
46. Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. (2011) 19:1121–30. doi: 10.1007/s00167-010-1342-7
47. Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Fismer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. (2012) 27:331–40. doi: 10.1016/j.arth.2011.04.046
48. Argenson JN, Parratte S, Ashour A, Saintmard B, Aubaniac JM. The outcome of rotating-platform total knee arthroplasty with cement at a minimum of ten years of follow-up. J Bone Joint Surg Am. (2012) 94:638–44. doi: 10.2106/JBJS.K.00263
49. Feng B, Weng X, Lin J, Jin J, Wang W, Qiu G. Long-term follow-up of cemented fixed-bearing total knee arthroplasty in a Chinese population: a survival analysis of more than 10 years. J Arthroplast. (2013) 28:1701–6. doi: 10.1016/j.arth.2013.03.009
50. Arsoy D, Pagnano MW, Lewallen DG, Hanssen AD, Sierra RJ. Aseptic tibial debonding as a cause of early failure in a modern total knee arthroplasty design. Clin Orthop Relat Res. (2013) 471:94–101. doi: 10.1007/s11999-012-2467-4
51. Wang K, Ni S, Li Z, Zhong Q, Li R, Li H, et al. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. (2017) 25:2849–57. doi: 10.1007/s00167-015-3964-2
52. Bauze AJ, Costi JJ, Stavrou P, Rankin WA, Hearn TC, Krishnan J, et al. Cement penetration and stiffness of the cement-bone composite in the proximal tibia in a porcine model. J Orthop Surg (Hong Kong. (2004) 12:194–8. doi: 10.1177/230949900401200211
53. Yao S, Zhang W, Ma J, Wang J. Effect of tourniquet application on cement penetration in primary total knee arthroplasty: a meta-analysis. Arthroplasty. (2021) 3:29. doi: 10.1186/s42836-021-00083-7
54. Cao Z, Guo J, Li Q, Wu J, Li Y. Comparison of efficacy and safety of different tourniquet applications in total knee arthroplasty: a network meta-analysis of randomized controlled trials. Ann Med. (2021) 53:1816–26. doi: 10.1080/07853890.2021.1991588
Keywords: total knee arthroplasty, tourniquet, blood loss, meta-analysis, transfusion requirement
Citation: Han J, Zhang X, Mu S, Liu S, Cui Q, Zhang C and Liu A (2023) Tourniquet application in primary total knee arthroplasty for osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Front. Surg. 9:994795. doi: 10.3389/fsurg.2022.994795
Received: 15 July 2022; Accepted: 3 November 2022;
Published: 6 January 2023.
Edited by:
Panayiotis D. Megaloikonomos, McGill University, CanadaReviewed by:
Huiyin Tu, University of Nebraska Medical Center, United States© 2023 Han, Zhang, Mu, Liu, Cui, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ai-feng Liu bGl1YWlmZW5nMjAyMkB5ZWFoLm5ldA==
†These authors have contributed equally to this work
‡ORCID Ai-feng Liu orcid.org/0000-0003-2183-3565
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.