
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 13 October 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.991476
This article is part of the Research Topic Clinical Application of Medical Imaging for Functional Evaluation in Orthopaedics View all 21 articles
 Yichao Luan1
Yichao Luan1 Min Zhang1
Min Zhang1 Tianfei Ran2
Tianfei Ran2 Huizhi Wang3
Huizhi Wang3 Chaohua Fang3,4
Chaohua Fang3,4 Maodan Nie3
Maodan Nie3 Min Wang2*
Min Wang2* Cheng-Kung Cheng1,3*
Cheng-Kung Cheng1,3*
Objective: This study aimed to investigate the correlation between component alignment and short-term clinical outcomes after total knee arthroplasty (TKA).
Methods: 50 TKA patients from a regional hospital were enrolled in the study. The following component alignments were measured from radiological data acquired within 1 week after surgery: hip-knee-ankle angle (HKA), medial distal femoral angle (MDFA), medial proximal tibial angle (MPTA), femoral flexion-extension angle (FEA), tibial slope angle (TSA), femoral rotational angle (FRA) and tibial rotational angle (TRA). The Hospital for Special Surgery (HSS) knee scoring system was used to assess clinical outcomes after 1 year, with patients being divided into three groups (excellent, good and not good) according to the HSS scores. Difference analysis and linear correlation analysis were used for the statistical analysis.
Results: The results showed significant differences in MDFA (p = 0.050) and FEA (p = 0.001) among the three patient groups. It was also found that the total HSS had only a moderate correlation with FEA (r = 0.572, p < 0.001), but FEA had a positive linear correlation with pain scores (r = 0.347, p = 0.013), function scores (r = 0.535, p = 0.000), ROM scores (r = 0.368, p = 0.009), muscle scores (r = 0.354, p = 0.012) and stability scores (r = 0.312, p = 0.028). A larger MDFA was associated with lower FE deformity scores (r = −0.289, p = 0.042) and the TSA had a positive influence on the ROM (r = 0.436, p = 0.002). Also, changes in FRA produced a consequent change in the FE deformity score (r = 0.312, p = 0.027), and the muscle strength scores increased as TRA increased (r = 0.402, p = 0.004).
Conclusion: The results show that the FEA plays a significant role in clinical outcomes after TKA. Surgical techniques and tools may need to be improved to accurately adjust the FEA to improve joint functionality and patient satisfaction.
Total knee arthroplasty (TKA) is the most effective treatment for severe arthritis of the knee joint. However, about 20% of patients are reportedly dissatisfied with the outcome because of joint pain or restricted function (1, 2). Malalignment of the knee prosthesis, which possibly results from inadequate determination of anatomical landmarks, the thickness of the saw blade and surgeon experience (3–5) have been reported as some of the main reasons for dissatisfaction and even revision (6, 7). Previous studies found that malalignment of knee prostheses can cause patellofemoral mal-tracking and incongruence with the femoral-insert interface, which may cause postoperative complications such as anterior knee pain and patellar subluxation (8, 9). The alignment of the prosthesis also influences the biomechanics and kinematics of the knee joint, such as stress on the ligaments, anterior-posterior translation of the femoral component and polyethylene wear (10–14).
Mechanical alignment is considered to create a biomechanically friendly environment in the knee joint that aims to position both the femoral and tibial components perpendicular to the mechanical axis. This method of aligning the components has been proven to produce good clinical and functional outcomes as well as long survivorship (15, 16). Some surgeons have suggested that the “safe zone” for the hip-knee-ankle (HKA) angle is with tibiofemoral alignment on the coronal plane being 180° ± 3° (17, 18). Patients aligned in this zone have reported better clinical outcomes (19), but, in contrast, some studies found no difference in outcomes or survivorship regardless if the alignment is within the “safe zone” (20, 21). Moreover, it has been reported that the “safe zone” may not be applicable to modern personalized alignment strategies (22). Complicating the discussion, differences in component alignment on the sagittal and transverse planes can also have a considerable impact on the joint. Some studies have shown that maintaining component alignment within 3° on the sagittal or transverse planes will not significantly affect the clinical outcomes (23, 24). However, opposing results have also been reported in other literature (25, 26). Few studies have examined the correlation between clinical outcomes and the alignment of knee components on all three planes (transverse, frontal and sagittal) in the same cohort of patients.
Recent advances in navigation, patient-specific instrumentation and robotics have improved surgical precision, but many surgeons still prefer conventional techniques because of the longer surgical time, higher cost and lack of qualifiable improvements in clinical outcome with the more advanced methods (27–30), a possible reason might be the greater attention to coronal alignment rather than also considering the sagittal and transverse planes, as well as unclear correlations between planar alignment and clinical outcomes. Therefore, this study aimed to investigate the correlation between the clinical scores and component alignment on all three planes (transverse, frontal and sagittal) using radiological measurements and clinical follow-up. It was hypothesized that there was a linear correlation between the alignment and clinical scores.
This retrospective research was approved by our institutional ethics committee and all patients provided informed consent before involvement. This study retrospectively assessed all primary TKA procedures performed in a regional hospital between June 2019 and December 2020. In total, 276 TKA procedures were considered. The exclusion criteria of this study were as follows: (1) patients preoperatively diagnosed with rheumatoid arthritis or traumatic arthritis; (2) patients with served extra-articular deformities, trauma or other joint diseases; (3) patients treated with bilateral TKA; (4) patients imaged more than 1 week after the procedure; (5) patients followed up less than 1 year after surgery. After exclusions, 50 patients (Female:Male = 42:8) were enrolled in this study including 24 left knees and 26 right knees. The age of these patients was 68.40 ± 8.73 years old.
All subjects were implanted with a posterior-stabilized (PS) knee system (Vanguard, Zimmer Biomet, USA) by an experienced senior knee surgeon following the approved guidelines for this prosthesis. The anteromedial incision and medial parapatellar approach were adopted for all TKA procedures and the prostheses were positioned using mechanical alignment. After cutting the distal femur, an intramedullary rod was placed into the femur along the anatomical axis. A valgus angle between the anatomical axis and mechanical axis was set according to pre-operative radiographs to ensure the cutting plane lay perpendicular to the mechanical axis. On the sagittal plane, the cutting line was perpendicular to the rod. The size of the femoral component was determined using the AP sizer and a 4-in-1 cutting block was placed when the slot was parallel to the trans-epicondylar axis (TEA). The location of the block was checked according to the anterior reference, and the distal femur was resected before the PS box was prepared following the surgical guidelines.
The extramedullary method was used for tibial resection. The cutting plane was perpendicular to the mechanical axis of the tibia on the coronal plane with a 5-degree slope on the sagittal plane. The size of the tibial component was confirmed following the best tibial coverage in both AP and medial-lateral (ML) directions. Rotational alignment of the tibial component was determined with the tibial trail under the knee flexion. The patella was repaired to an appropriate shape instead of the resurfacing.
Full leg weight-bearing anterior-posterior (AP) radiographs were taken preoperatively to measure the angle between the mechanical and anatomical axis, and lateral radiographs were used to estimate the required size of femoral component. The standard anteroposterior and lateral radiographs and the artifact-reducing CT images of the knee joint were taken routinely within 1 week after surgery. On the coronal plane, the hip-knee-ankle angle (HKA), medial distal femoral angle and medial proximal tibial angle were used to assess joint alignment (31). The femoral mechanical axis was defined as a line connecting the centers of the femoral head and knee joint, and the tibial mechanical axis was a line connecting the centers of the knee joint and ankle joint. The medial angle between the mechanical axis of the femur and tibia was taken as the HKA, the medial angle between the mechanical axis and condylar tangent line of the femoral component was MDFA, and the angle between the mechanical axis and the border of the tibial baseplate was the MPTA (Figure 1). The femoral flexion-extension angle (FEA) and tibial slope angle (TSA) were used to evaluate alignment on the sagittal plane (24), with the anatomical axis being the line that connected the midpoints of the outer cortical diameter at 5 and 15 cm proximal to the joint line on the femur and tibia (32). The anterior angle between the femoral anatomical axis and the distal cutting line was the FEA, and the posterior angle between the tibial anatomical axis and the border of the tibial baseplate was the TSA (Figure 2). On the transverse plane, the femoral rotational angle (FRA) and tibial rotation angle (TRA) were used to identify the alignments. The angle between TEA and the posterior condylar line (PCL) was FRA (Figure 3A). The TRA was determined by the tibial component axis (TCA) and tibial tuberosity axis (TTA) (Figure 3D). TCA was the mid-perpendicular line of the tibial posterior border (TPB) (Figure 3B). TTA was the line connecting the geometrical center (GC) (Figure 3C) of an ellipse of best fit around the proximal tibia just below the metal base plate and the center of the most prominent part of the tibial tuberosity (9). Neutral tibial rotational alignment was considered to be 18° internal rotation from TTA to TCA (33). Alignment errors were calculated as the difference between the preoperative surgical plan (HKA = 180°, MDFA = MPTA = FEA = 90°, TSA = 85°, FRA = 0°, TRA = 18°) and actual measurements from radiographs, and the outlier was considered as the errors more than 3° (17, 18). The outlier rate was the ratio of number of outlier cases to the total cases. The angles on the coronal (HKA, MDFA, MPTA) and sagittal (FEA, TSA) planes were measured by Picpick 5.0 (NGWIN, Korea) while the angles on the transverse plane (FRA, TRA) were measured by Mimics 21.0 (Materialise, Belgium). All measurements were recorded to an accuracy of 0.1°. Each angle was measured three times, with the average being considered the result for that angle.
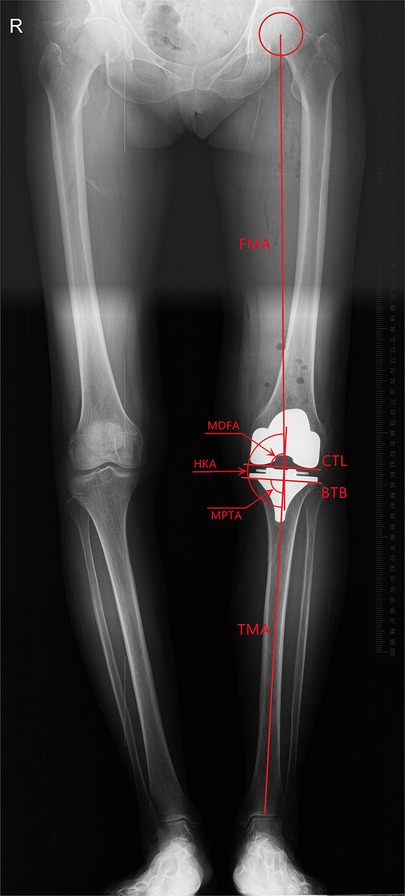
Figure 1. Measurement on the coronal plane (FMA, femoral mechanical axis: a line connecting the centers of the femoral head and knee joint; CTL, condylar tangent line; BTB, border of tibial baseplate; TMA, tibial mechanical axis: a line connecting the centers of the knee joint and ankle joint; MDFA, medical distal femoral angle; MPTA, medical proximal tibial angle; HKA, medical angle between FMA and TMA).
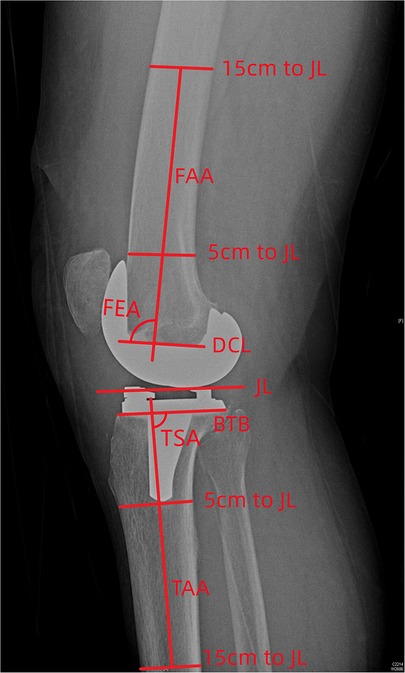
Figure 2. Measurement on the sagittal plane (JL, joint line; FAA, femoral anatomical axis; DCL, distal cutting line; BTB, border of tibial baseplate; TAA, tibial anatomical axis; FEA, femoral flexion-extension angle; TSA, tibial posterior slope angle).
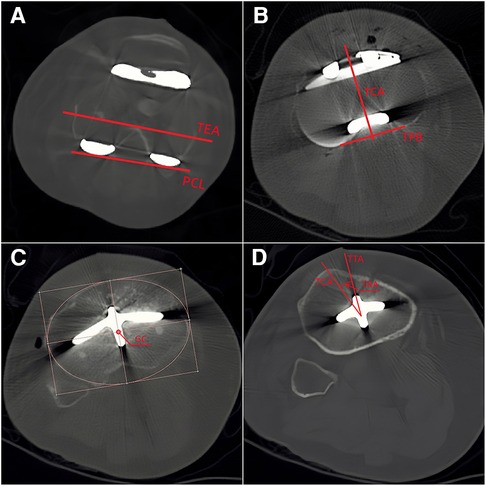
Figure 3. Measurement on the transverse plane (A: TEA, trans-epicondyle axis; PCL, posterior condylar line; B: TPB, tibial posterior border; TCA, tibial component axis: the mid-perpendicular line of the TPB; C: GC, geometrical center; D: TRA, tibial rotational angle).
All patients were followed up by physical examination in the outpatient department for at least 12 months after surgery. The Hospital for Special Surgery knee scoring system (HSS) was selected to assess the clinical outcome (34). The HSS score consisted of six sections, including pain (30 scores), function (22 scores), range of motion (18 scores), muscle force (10 scores), flexion-extension deformity (10 scores) and stability (10 scores). The maximum score achievable is 100 which is the sum of the six sections. The patients were divided into three groups according to their HSS scores. Scores between 85 and 100 were considered excellent (Group A), scores between 84 and 70 points were considered good (Group B), and scores less than 69 points were considered not good (Group C) (34).
All statistical analyses were performed using IBM SPSS Statistics 26 (SPSS Inc, Chicago, USA). Power analysis was used to calculate the sample size. The power level was set as 80% with a 0.05 significance level, and the effect size was set as 0.44 (35). The analysis indicated that 43 participants were needed to provide a statistical power of 80%. The Kolmogorov-Smirnov test was used to test the normality of all data and data was regarded as a normal distribution when the significance was greater than 0.05. Quantitative data was expressed as a mean ± standard deviation. The linear correlation between joint alignments (HKA, MDFA, MPTA, FEA, TSA, FRA, TRA) and HSS scores, both the total score and section scores, was analyzed by Pearson analysis when the variable was distributed normally, and by Spearman analysis when the variable was not normally distributed. The correlation coefficient (r) assumes any value from −1 to 1, with an |r| value of less than 0.4 being considered a weak correlation, moderate correlations when |r| is between 0.4 and 0.7, and strong correlations when |r| is more than 0.7. Difference in alignment among the groups were assessed using a Kruskal-Wallis test. A p-value less than 0.05 was considered significant.
The pre-operative HKA for the patient cohort was 174.10° ± 8.66° and the follow-up time was 16.94 ± 3.61 months. Joint alignment on the three measurement planes is shown in Table 1. On the coronal plane, the post-operative HKA was 179.46° ± 3.36° and presented as varus alignment, which was defined as an angle of less than 180°. The MDFA and MPTA were 89.08° ± 2.59° and 89.78° ± 1.68° respectively, which were similarly considered to be in varus alignment if the angle was less than 90°. On the sagittal plane, the FEA was 91.67° ± 2.18°, with an angle of more than 90° being considered extension. The TSA was 86.20° ± 1.77°, which represents a posterior slope when the angle is less than 90°. On the transverse plane, the FRA and TRA were 1.58° ± 2.83° and 3.32° ± 4.92° respectively, with positive values representing external alignment. The total HSS score and the score from each section are shown in Table 2.
The outlier rates for all the post-operative alignments were calculated. The results showed that FEA had the highest rate (42%) in all alignments (Table 3).
The correlation coefficients (r) and associated p-values are shown in Table 4. The results show that the FEA had a positive linear correlation with the total HSS score (Figure 4, r = 0.572, p = 0.000), pain score (r = 0.347, p = 0.013), function score (r = 0.535, p = 0.000), ROM score (r = 0.368, p = 0.009), muscle score (r = 0.354, p = 0.012) and stability score (r = 0.312, p = 0.028). Larger values for MDFA were associated with lower FE deformity scores (r = −0.289, p = 0.042) and the TSA had a positive influence on the ROM scores (r = 0.436, p = 0.002). Also, it was found that different FRA would result in the different FE deformity scores (r = 0.312, p = 0.027), and the muscle strength score increased as the TRA increased (r = 0.402, p = 0.004). Positive correlations between results were confirmed when the r-value was greater than 0.
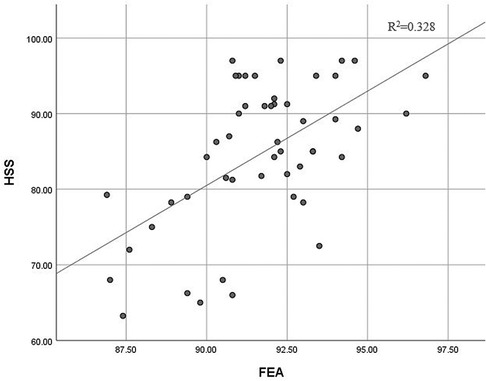
Figure 4. Correlation between HSS and FEA (HSS, hospital for special surgery knee scores; FEA, femoral flexion-extension angle).
The patients were divided into different groups according to the total HSS score. There were 28 patients in Group A, 16 patients in Group B, 6 patients in Group C. Patient age, pre-operative HKA, alignments on the three planes for the three groups were assessed using a Kruskal Wallis test. The results revealed significant differences in MDFA (p = 0.050) and FEA (p = 0.001) between the groups. Except for the parameters mentioned, no significant differences were detected between other measurements (p > 0.050). All results are detailed in Table 5.
The main finding of this study was that there were significant differences in MDFA and FEA between the three groups with excellent, good and not good scores. It was also found that the total HSS only had a moderate correlation with FEA. Meanwhile, the outlier rate of FEA was the highest among all alignments within the same patient cohort.
This study found similar correlations between alignments and clinical outcomes as previous studies. Kastner et al. demonstrated that the sagittal alignment of femoral components is significantly correlated with the range of motion (36), which supports the associated between FEA and the ROM scores in this present study. Scott et al. found that the alignment of the femoral component on the sagittal plane was associated with anterior knee pain, and femoral component extension was a major risk factor (37). Similarly, this study found a significant correlation between FEA and pain score. Meanwhile, the functional scores had a moderate correlation with FEA, which is somewhat supported by Okamoto's study that good femoral sagittal alignment leads to better joint function (38). In this study, the FEA was also correlated with muscle strength and stability. Koh et al. reported that the quadriceps force, collateral ligament force and patella-femoral contact stress decreased as the angle between the axis of the femoral component and anterior cortex became smaller (39). This indicates that changes in the biomechanical environment around the knee may affect muscle strength and joint stability. Also, the significant correlation between FE-deformity scores and MDFA and FRA is supported by a study by Matziolis et al. detailing that distal femoral resection influences the flexion deformity of knee joint (40).
In this study, the FEA had the highest outlier rate, which is similar to findings from previous studies (Table 6). It is common for surgeons to attempt to align the femoral component when the cutting line is perpendicular to the anatomical axis on the sagittal plane and avoid the notch of the anterior cortical bone (48). However, it is not easy to identify the anatomical axis during conventional operations. When an intramedullary rod is used to represent the anatomical axis of the femur, errors with positioning of the entry point and insertion direction might lead to the rod being offset from the true axis. Such differences may also contribute to malalignment on the coronal plane. While variations in radiographic assessments could also influence the results, when using the anatomical axis and anterior cortical axis to evaluate femoral alignment on the sagittal plane, Jenny et al. reported little difference between the two axes and any variation in readings will likely have little clinical relevance (32). Tibial rotational alignment is considered one of the most controversial alignment methods in TKA because of the different reference landmarks used for the tibia and difference methods of alignment (4). This study performed a tibial trial during rotational alignment of the tibial component to confirm proper positioning, but this led to an unclear target of TRA value, and hence the outlier rate of TRA was not calculated.
The results showed a correlation between femoral component alignment on the sagittal plane (FEA) and complications after TKA, including pain, flexion contracture, and a restricted range of motion. A 10-year follow-up study by Scott et al. found sagittal plane positioning of the femoral component to be associated with long-term anterior knee pain, and it was suggested that femoral component extension might be a major risk factor for knee pain (37). Okamoto et al. found that FEA was significantly different between groups with differing degrees of flexion contracture, and they reported that FEA and body height were independent predictive risk factors for residual flexion contracture of more than 10° (38). Changes in the mechanical and kinematic environment in the knee joint resulting from different FEA were a likely reason for these complications.
The sagittal positioning of the femoral component is recognized as an important factor in knee joint mechanics and kinematics. It was reported that the femoral flexion-extension angle influenced the femorotibial contact position in the knee flexion which changed the arm of the quadriceps force and patellofemoral (PF) contact force (49). Using finite element models, Koh et al. investigated how variations in the FEA impacted knee mechanics and kinematics, and found the femorotibial contact points were positioned more posteriorly with larger FEA angles, and the quadriceps force, as well as the PF contact force, was reduced because of the decreased lever arm. It was suggested that placing the prosthesis in slight flexion could be an effective alternative technique to enable positive biomechanical effects with TKA (39, 50). Besides, the discrepancy of medial and lateral collateral ligaments between different femoral flexion-extension angles, the collateral ligament force decreased as the femoral component flexed during the knee bending. Large amounts of sagittal femoral component extension may be harmful to the collateral ligament. Errors in femoral component sagittal alignment contribute to imbalanced soft tissue that leads to instability and a limited range of motion (51). However, while these factors may improve clinical outcomes, they must also be considered when evaluating differences between studies and patient satisfaction.
Although digital techniques such as navigation, custom instrumentation and robotics have been commercially available and widely used for a number of years, conventional surgical techniques are still common because of the additional surgical time and costs associated with more advanced methods (27, 29, 30, 52). Moreover, mechanical alignment is regarded as one of the best approaches to TKA, with many studies demonstrating acceptable joint kinematics when the error of coronal alignment is less than 3°. However, contrasting studies have also reported that coronal alignment is not an accurate predictor of clinical outcomes and maintaining alignment within 0 ± 3° is not a “safe zone” when using more modern personalized alignment strategies (22, 53). The sagittal alignment for TKA, especially for the femoral component needs more consideration, and the surgical procedures and tools need to be improved to allow for more precise alignment.
There are also some limitations in this study. First, 50 TKA patients were enrolled in the study because of the considerable time and cost associated with patient examination. However, the sample size was sufficient according to the power analysis to assess the correlations between alignments and clinical scores. Moreover, the minimum follow-up time was 12 months. Future studies may consider longer-term follow-up.
A significant and moderate correlation was found between FEA and the HSS score, and the FEA had the highest outlier rate. This suggests that FEA should be carefully considered when planning TKA and implant positioning. Surgical techniques and tools, especially for conventional surgery, need to be enhanced, to improve surgical accuracy and patient satisfaction.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of the Second Affiliated Hospital of PLA Army Military Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CKC: conceptualization, methodology, project administration, supervision, writing-review and editing. MW: conceptualization, resources, supervision, writing-review and editing. YL: formal analysis, investigation, data curation, writing-original draft preparation, writing-review and editing. MZ: formal analysis, data curation, writing-original draft preparation, writing-review and editing. TR: data curation. HW, MN and CF: investigation, review and editing. All authors have agreed to be personally accountable for their own contributions and ensure that questions related to the accuracy and integrity of any part of the work have been appropriately investigated and resolved with reference to the literature when needed. All authors contributed to the article and approved the submitted version.
This research was supported by the Science and Technology Innovation and Application Development Project of Chongqing (2021MSXM197) and Ningbo Public Welfare Science and Technology project (2022S064).
We would like to thank Colin McClean for his assistance with editing this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
TKA, total knee arthroplasty; HKA, hip-knee-ankle angle; MDFA, medial distal femoral angle; MPTA, medial proximal tibial angle; FEA, femoral flexion-extension angle; TSA, tibial slope angle; FRA, femoral rotational angle; TRA, tibial rotational angle; HSS, Hospital for Special Surgery knee scoring system; PS, posterior-stabilized; TEA, trans-epicondylar axis; AP, anterior-posterior; PCL, posterior condylar line; TCA, tibial component axis; TTA, tibial tuberosity axis; GC, geometrical center; FMA, femoral mechanical axis; CTL, condylar tangent line; BTB, border of tibial baseplate; TMA, tibial mechanical axis; JL, joint line; FAA, femoral anatomical axis; DCL, distal cutting line; TAA, tibial anatomical axis
1. Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. (2008) 168(13):1430–40. doi: 10.1001/archinte.168.13.1430
2. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. (2010) 468(1):57–63. doi: 10.1007/s11999-009-1119-9
3. Peltola M, Malmivaara A, Paavola M. Learning curve for new technology? A nationwide register-based study of 46,363 total knee arthroplasties. J Bone Joint Surg Am. (2013) 95(23):2097–103. doi: 10.2106/jbjs.L.01296
4. Saffarini M, Nover L, Tandogan R, Becker R, Moser LB, Hirschmann MT, et al. The original akagi line is the most reliable: a systematic review of landmarks for rotational alignment of the tibial component in Tka. Knee Surg Sports Traumatol Arthrosc. (2019) 27(4):1018–27. doi: 10.1007/s00167-018-5131-z.
5. Yau WP, Chiu KY. Cutting errors in total knee replacement: assessment by computer assisted surgery. Knee Surg Sports Traumatol Arthrosc. (2008) 16(7):670–3. doi: 10.1007/s00167-008-0550-x
6. Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. (2015) 97(9):715–20. doi: 10.2106/jbjs.M.01534
7. Ben-Shlomo Y, Blom A, Boulton C, Brittain R, Clark E, Craig R, et al. National joint registry annual reports. The National Joint Registry 17th Annual Report 2020. London: National Joint Registry © National Joint Registry (2020).
8. Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. (1998) 356:144–53. doi: 10.1097/00003086-199811000-00021
9. Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br. (2010) 92(9):1238–44. doi: 10.1302/0301-620x.92b9.23516
10. Liau JJ, Cheng CK, Huang CH, Lo WH. The effect of malalignment on stresses in polyethylene component of total knee prostheses–a finite element analysis. Clin Biomech. (2002) 17(2):140–6. doi: 10.1016/s0268-0033(01)00109-7
11. Johnston H, Abdelgaied A, Pandit H, Fisher J, Jennings LM. The effect of surgical alignment and soft tissue conditions on the kinematics and wear of a fixed bearing total knee replacement. J Mech Behav Biomed Mater. (2019) 100:103386. doi: 10.1016/j.jmbbm.2019.103386
12. Wang ZW, Wen L, Luan YC, Ma DS, Dong X, Cheng CK, et al. Restoration of joint inclination in total knee arthroplasty offers little improvement in joint kinematics in neutrally aligned extremities. Front Bioeng Biotechnol. (2021) 9:673275. doi: 10.3389/fbioe.2021.673275
13. Fang C, Luan Y, Wang Z, Shao L, Qu T, Cheng CK. Moderate external rotation of tibial component generates more natural kinematics than internal rotation after total knee arthroplasty. Front Bioeng Biotechnol. (2022) 10:910311. doi: 10.3389/fbioe.2022.910311
14. Ro J, Ro DH, Kang Y, Han HS, Shin CS. Biomechanical effect of coronal alignment and ligament laxity in total knee arthroplasty: a simulation study. Front Bioeng Biotechnol. (2022) 10:851495. doi: 10.3389/fbioe.2022.851495
15. Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. (2009) 24(4):560–9. doi: 10.1016/j.arth.2008.02.018
16. Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, anatomical, and kinematic axis in Tka: concepts and practical applications. Curr Rev Musculoskelet Med. (2014) 7(2):89–95. doi: 10.1007/s12178-014-9218-y
17. Bonner TJ, Eardley WG, Patterson P, Gregg PJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br. (2011) 93(9):1217–22. doi: 10.1302/0301-620x.93b9.26573
18. Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J. (2014) 96-b(7):857–62. doi: 10.1302/0301-620x.96b7.33946
19. Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT. Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc. (2018) 26(6):1602–9. doi: 10.1007/s00167-017-4744-y
20. Mugnai R, Zambianchi F, Digennaro V, Marcovigi A, Tarallo L, Del Giovane C, et al. Clinical outcome is not affected by total knee arthroplasty alignment. Knee Surg Sports Traumatol Arthrosc. (2016) 24(10):3339–45. doi: 10.1007/s00167-016-4094-1
21. Abdel MP, Ollivier M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J Bone Joint Surg Am. (2018) 100(6):472–8. doi: 10.2106/jbjs.16.01587
22. Schelker BL, Nowakowski AM, Hirschmann MT. What is the “safe zone” for transition of coronal alignment from systematic to a more personalised one in total knee arthroplasty? A systematic review. Knee Surg Sports Traumatol Arthrosc. (2022) 30(2):419–27. doi: 10.1007/s00167-021-06811-5
23. Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. (2014) 38(2):379–85. doi: 10.1007/s00264-013-2097-9
24. Ahmed I, Paraoan V, Bhatt D, Mishra B, Khatri C, Griffin D, et al. Tibial component sizing and alignment of tkr components does not significantly affect patient reported outcome measures at six months. A case series of 474 participants. Int J Surg. (2018) 52:67–73. doi: 10.1016/j.ijsu.2018.02.039
25. Thielemann FW, Konstantinids L, Herget GW, Knothe D, Helwig P, Sudkamp NP, et al. Effect of rotational component alignment on clinical outcome 5 to 7 years after tka with the Columbus knee system. Orthopedics. (2016) 39(3 Suppl):S50-5. doi: 10.3928/01477447-20160509-17
26. Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, et al. Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. (2018) 26(6):1636–44. doi: 10.1007/s00167-017-4823-0
27. Yang JH, Dahuja A, Kim JK, Yun SH, Yoon JR. Alignment in knee flexion position during navigation-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2016) 24(8):2422–9. doi: 10.1007/s00167-015-3589-5
28. Giannotti S, Sacchetti F, Citarelli C, Bottai V, Bianchi N, Agostini G, et al. Single-use, patient-specific instrumentation technology in knee arthroplasty: a comparative study between standard instrumentation and psi efficiency system. Musculoskelet Surg. (2020) 104(2):195–200. doi: 10.1007/s12306-019-00612-3
29. Onggo JR, Onggo JD, De Steiger R, Hau R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg. (2020) 140(10):1533–49. doi: 10.1007/s00402-020-03512-5
30. Batailler C, Fernandez A, Swan J, Servien E, Haddad FS, Catani F, et al. Mako CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. (2021) 29(11):3585–98. doi: 10.1007/s00167-020-06283-z
31. Abane L, Zaoui A, Anract P, Lefevre N, Herman S, Hamadouche M. Can a single-use and patient-specific instrumentation be reliably used in primary total knee arthroplasty? A multicenter controlled study. J Arthroplasty. (2018) 33(7):2111–8. doi: 10.1016/j.arth.2018.02.038
32. Jenny JY, Barbe B. Small differences between anatomical and mechanical sagittal femur axes: a radiological and navigated study of 50 patients. Arch Orthop Trauma Surg. (2012) 132(7):1053–7. doi: 10.1007/s00402-012-1500-0
33. Berger RA, Crossett LS. Determining the rotation of thefemoral and tibial components in total knee arthroplasty: a computer tomography technique. Oper Tech Orthop. (1998) 8(3):128–33. doi: 10.1016/S1048-6666(98)80022-0
34. Alicea J. Knee scores in total knee arthroplasty. In: Scuderi GR, Tria AJ, editors. Surgical techniques in total knee arthroplasty. New York, NY: Springer New York (2002). p. 31–8.
35. Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC. Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop. (2015) 86(4):432–9. doi: 10.3109/17453674.2015.1022438
36. Kastner N, Sternbauer S, Friesenbichler J, Vielgut I, Wolf M, Glehr M, et al. Impact of the tibial slope on range of motion after low-contact-stress, mobile-bearing, total knee arthroplasty. Int Orthop. (2014) 38(2):291–5. doi: 10.1007/s00264-013-2242-5
37. Scott CEH, Clement ND, Yapp LZ, MacDonald DJ, Patton JT, Burnett R. Association between femoral component sagittal positioning and anterior knee pain in total knee arthroplasty: a 10-year case-control follow-up study of a cruciate-retaining single-radius design. J Bone Joint Surg Am. (2019) 101(17):1575–85. doi: 10.2106/jbjs.18.01096
38. Okamoto Y, Otsuki S, Nakajima M, Jotoku T, Wakama H, Neo M. Sagittal alignment of the femoral component and patient height are associated with persisting flexion contracture after primary total knee arthroplasty. J Arthroplasty. (2019) 34(7):1476–82. doi: 10.1016/j.arth.2019.02.051
39. Koh YG, Hong HT, Lee HY, Kim HJ, Kang KT. Influence of variation in sagittal placement of the femoral component after cruciate-retaining total knee arthroplasty. J Knee Surg. (2021) 34(4):444–51. doi: 10.1055/s-0039-1696958
40. Matziolis G, Loos M, Böhle S, Schwerdt C, Roehner E, Heinecke M. Effect of additional distal femoral resection on flexion deformity in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2020) 28(9):2924–9. doi: 10.1007/s00167-019-05675-0
41. Ueyama H, Matsui Y, Minoda Y, Matsuura M, Nakamura H. Using accelerometer-based portable navigation to perform accurate total knee arthroplasty bone resection in Asian patients. Orthopedics. (2017) 40(3):e465–e72. doi: 10.3928/01477447-20170223-01
42. Huang TW, Peng KT, Huang KC, Lee MS, Hsu RW. Differences in component and limb alignment between computer-assisted and conventional surgery total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2014) 22(12):2954–61. doi: 10.1007/s00167-014-3331-8
43. Chen X, Wang H, Cai Y, Zhu Q, Zhu J. Sagittal component alignment is less reliable than coronal component alignment in a Chinese population undergoing navigated tka. J Orthop Surg Res. (2014) 9:51. doi: 10.1186/s13018-014-0051-1
44. Kotela A, Kotela I. Patient-specific computed tomography based instrumentation in total knee arthroplasty: a prospective randomized controlled study. Int Orthop. (2014) 38(10):2099–107. doi: 10.1007/s00264-014-2399-6
45. Yan CH, Chiu KY, Ng FY, Chan PK, Fang CX. Comparison between patient-specific instruments and conventional instruments and computer navigation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. (2015) 23(12):3637–45. doi: 10.1007/s00167-014-3264-2
46. Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res. (2014) 472(1):263–71. doi: 10.1007/s11999-013-2997-4
47. Boonen B, Schotanus MG, Kerens B, van der Weegen W, van Drumpt RA, Kort NP. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. (2013) 21(10):2206–12. doi: 10.1007/s00167-013-2620-y
48. Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop. (2014) 85(5):480–7. doi: 10.3109/17453674.2014.940573
49. Browne C, Hermida JC, Bergula A, Colwell CW Jr., D'Lima DD. Patellofemoral forces after total knee arthroplasty: effect of extensor moment arm. Knee. (2005) 12(2):81–8. doi: 10.1016/j.knee.2004.05.006
50. Kang KT, Koh YG, Son J, Kwon OR, Park KK. Flexed femoral component improves kinematics and biomechanical effect in posterior stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2019) 27(4):1174–81. doi: 10.1007/s00167-018-5093-1
51. Koh YG, Lee JA, Lee HY, Suh DS, Park JH, Kang KT. Finite element analysis of femoral component sagittal alignment in mobile-bearing total knee arthroplasty. Bio-Med Mater Eng. (2022) 33(3):195–207. doi: 10.3233/bme-211280
52. Zheng G, Nolte LP. Computer-assisted orthopedic surgery: current state and future perspective. Front Surg. (2015) 2:66. doi: 10.3389/fsurg.2015.00066
Keywords: total knee arthroplasty, component alignment, clinical outcomes, outlier rate, linear correlation
Citation: Luan Y, Zhang M, Ran T, Wang H, Fang C, Nie M, Wang M and Cheng C-K (2022) Correlation between component alignment and short-term clinical outcomes after total knee arthroplasty. Front. Surg. 9:991476. doi: 10.3389/fsurg.2022.991476
Received: 11 July 2022; Accepted: 26 September 2022;
Published: 13 October 2022.
Edited by:
Huiwu Li, Shanghai Ninth People's Hospital, ChinaReviewed by:
Jia Hua, University College London, United Kingdom© 2022 Luan, Zhang, Ran, Wang, Fang, Nie, Wang and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min Wang d2FuZ21pbkB0bW11LmVkdS5jbg== Cheng-Kung Cheng Y2tjaGVuZzIwMDlAZ21haWwuY29t
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.