- 1Department of Dermatology, The First People’s Hospital of Foshan, Foshan, China
- 2Institute of Medical Biology, Chinese Academy of Medical Sciences and Peking Union Medical College, Yunnan Key Laboratory of Vaccine Research and Development on Severe Infectious Diseases, Kunming, China
- 3Department of Burn and Plastic Surgery, Guangzhou First People's Hospital, South China University of Technology, Guangzhou, China
Objective: Providing protection against aggregation and guiding hydrophobic precursors through the mitochondria’s intermembrane space, this protein functions as a chaperone-like protein. SLC25A12 is imported by TIMM8 as a result of its interaction with TIMM13. In spite of this, it is still unknown how TIMM13 interacts with skin cutaneous melanoma (SKCM) and tumor-infiltrating lymphocytes (TILs).
Methods: Aberrant expression of TIMM13 in SKCM and its clinical outcome was evaluated with the help of multiple databases, including the Xiantao tool (https://www.xiantao.love/), HPA, and UALCAN. TISIDB and Tumor Immune Estimation Resources (TIMER) databases were applied to explore the association between TIMM13 and tumor infiltration immune cells. OS nomogram was constructed, and model performance was examined. Finally, TIMM13 protein expression was validated by immunohistochemistry (IHC).
Results: TIMM13 expression was higher in SKCM samples than in peritumor samples. TIMM13 was strongly associated with sample type, subgroup, cancer stage, lymph node stage, and worse survival. Further, upregulation of TIMM13 was significantly associated with immunoregulators, and chemokines, as well as T cells, B cells, monocytes, neutrophils, macrophages, and T-cell regulators. An analysis of bioinformatic data uncovered that TIMM13 expression was strongly associated with PD1 (T-cell exhaustion marker). The nomogram showed good predictive performance based on calibration plot. TIMM13 was highly expressed in melanoma tissue samples than in normal samples.
Conclusion: In brief, TIMM13 may be a prognostic biomarker for SKCM. It might modulate the tumor immune microenvironment and lead to a poorer prognosis. In addition, it is necessary to study the targeted therapy of TIMM13.
Introduction
There are two main types of melanoma: cutaneous and uveal (1). Melanin-producing melanocytes in the skin are transformed into melanoma cells through malignant transformation (2). More than 75% of skin cancer deaths are caused by melanoma, even though it represents only 5% of all skin cancer cases (3). Cutaneous melanoma is considered the most aggressive type of skin cancer (4). There are approximately 232,100 (1.7%) new cases of cutaneous melanoma diagnosed worldwide (excluding nonmelanoma skin cancers), and the incidence of cutaneous melanoma is around 55,500 deaths per year (0.7% of all cancer deaths) (5). Before the FDA’s approved targeted and immunotherapy strategies in 2011 and 2014, metastatic melanoma was thought to be incurable and not treatable (6). These strategies are effective in treating some cases of melanoma, but not all, due to toxicity, intrinsic resistance to drugs, and other unidentified causes (7). It is necessary to perform surgery, radiotherapy, chemotherapy, and conduct clinical trials to cure resistant melanoma cells (8). With SKCM, the discovery of new immunotherapy targets and the detection of immune-related biomarkers are urgent tasks.
The TIMM13 gene encodes a chaperone protein that is part of the evolutionarily conserved TIMM (translocase of inner mitochondrial membrane) family that assists in the transport of proteins into mitochondria from the cytosol (9). The TIMM13 gene prevents hydrophobic precursors from aggregating and guides the proteins passing the mitochondrial intermembrane. SLC25A12/ARALAR1 and SLC25A13/ARALAR2 are imported by the TIMM8-TIMM13 complex (10). Timm13 is associated with Mohr-Tranebjaerg Syndrome and Visual Cortex Disease (11). It is related to the Peroxisomal lipid metabolism pathway (12). Studies have shown that TIMM13 was differently expressed in metastatic susceptibility (13), hepatocellular carcinoma (14), breast cancer (15) et al. These research proposed that TIMM13 may impact cancer profoundly, and it may be considered a new target for dealing with various malignant tumors. However, the possible mechanisms of TIMM13 in tumorigenesis and immune involvement in SKCM is still unclear.
In the study, the expression of TIMM13 and its connection with the clinical outcomes of SKCM were explored by various databases, including the Xiantao tool, HPA, and UALCAN databases. In addition, the Xiantao tool and TIMER database was conducted to explore the connection of TIMM13 with the infiltration of immune cells. The TISIDB database was used to study the relationship between TIMM13 and immunomodulators, immunostimulators, and chemokines. This research revealed the important function of TIMM13 in SKCM, and then the possible relationship and possibility of TIMM13 regulating tumor invasion of immune cells.
Materials and methods
Interaction analysis of gene expression profiling
The Xiantao tool online database (https://www.xiantao.love/) (16) is an integrated platform using R software (3.6.3) for obtaining analytical data from TCGA (https://portal.gdc.cancer.gov/) (17) and The Genotype–Tissue Expression (GTEx) (https://gtexportal.org/home/) (18). R packages used in the Xiantao tool were set as default. In the study, we evaluated TIMM13 expression in SKCM and normal tissues using the Xiantao data source.
UALCAN database analysis
The UALCAN website (http://ualcan.path.uab.edu/) contains massive bioinformatics and clinical data on 31 TCGA malignant tumors (19). It can be used to make a gene expression comparison between SKCM and normal samples, at different tumor stages, different subtypes, and other clinicopathological characteristics. In the research, the expression level of TIMM13 will be determined by the main clinicopathological characteristics, such as tissue category (healthy or tumor), SKCM stage (stages 1, 2, 3, 4), lymph node stage (N01 stage, 2, 3), cancer subgroup, etc. The clinicopathological features (tumor degree, stage) and TIMM13 expression distribution of patients were collected by the UALCAN database and Xiantao tool for correlation analysis.
Survival analysis for SKCM
Based on the median of the expression of TIMM13, patients were divided into a high TIMM13 expression group and a low TIMM13 expression group. The prognostic significance of TIMM13 in SKCM, including overall survival (OS), and progression-free interval (PFI), were explored using the Xiantao tool between the high TIMM13 expression group and low TIMM13 expression group. The hazard ratio (HR) with 95% confidence intervals and log-rank p-value was estimated. P < 0.05 was regarded as statistical significance.
Tumor immune infiltration analysis
ssSGSEA method was applied to explore the potential connection between TIMM13 mRNA expression and immune infiltration level in SKCM by TIMER 2.0 (http://timer.cistrome.org/) (20). In addition, TILs gene markers and TILs gene expression were analyzed by the Xiantao tool. Then we drew the expression dispersion maps between a pair of custom genes for SKCM and the statistical significance of the correlation was estimated by Spearman's method. log2 RSEM was applied to exhibit the levels of gene expression.
TISIDB database analysis
TISIDB (http://cis.hku.hk/TISIDB/) (21) is an online platform for studying tumor-immune system interaction, which combines various heterogeneous data sources. This database can assist us to know the interaction between tumors and immune cells, predict the responses of the body to immunotherapy, and find out novel immunotherapy targets. It will be a precious basis for tumor immunology studies and treatment. In this study, we used TISIDB to study the relationship between TIMM13 and 28 TILs, 45 immunopotentiators, 24 immunosuppressants, 41 chemokines, and 18 receptors in SKCM.
Building and validation of a nomogram
A nomogram is a statistical model of prognosis presented as a simple graph. In the nomogram, each sample is assigned a point for each of its variables and the resulting total score predicts 1-, 3-, and 5-year survival rates. We used independent prognostic factors to build a nomogram using the “rms” package. A calibration plot (by a bootstrap method with 500 resamples) was used to validate the nomogram and concordance index (C-index).
Immunohistochemistry (IHC) staining
Paraffin-embedded tissues were sectioned at 4 μm for IHC analysis. Antigens were retrieved by incubating the samples in citrate buffer (pH 6.0) for 15 min at 100 °C in a microwave oven and naturally cooled to room temperature. After blocking with a mixture of methanol and 0.75% hydrogen peroxide, sections were incubated overnight with appropriate dilatation of primary antibodies (TIMM13, Invitrogen, 1:150) followed by incubation with a secondary antibody conjugated with HRP (goat anti-rabbit, 1:500, Cell Signalling Technology). The sections were washed three times with PBS and incubated with AEC (ZSGB-BIO).
Statistical analysis
Statistical analyses were performed with the Student t test, the Mann-Whitney U test, or analysis of variance, as appropriate. For nonparametric (non-normally distributed) data, Mann–Whitney U test was used for statistical analysis. The survival curve was drawn by KM plot by log-rank test. We calculated Spearman's correlation coefficient to explore the relationship between TIMM13 expression and immune infiltration levels, immunomodulators, and chemokines. Statistically significant was regarded as p < 0.05.
Results
High expression of TIMM13 in SKCM tissue
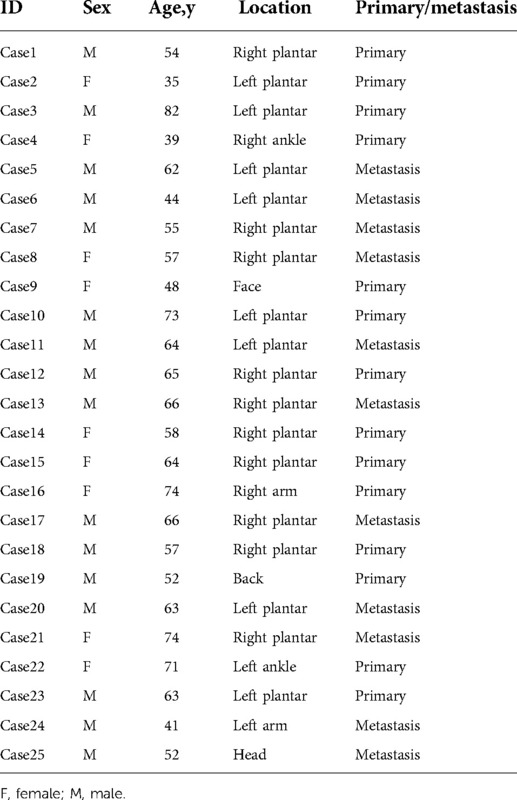
The differential expression of TIMM13 in tumor and normal tissues were studied by RNA-seq data of different types of cancer from TCGA. The conclusion was shown in Figure 1A. According to Xiantao tool, we found that the expression of TIMM13 upregulated in almost all cancer tissues such as ACC, BLCA and SKCM, but downregulated in KIRC, LAML and PCPG.
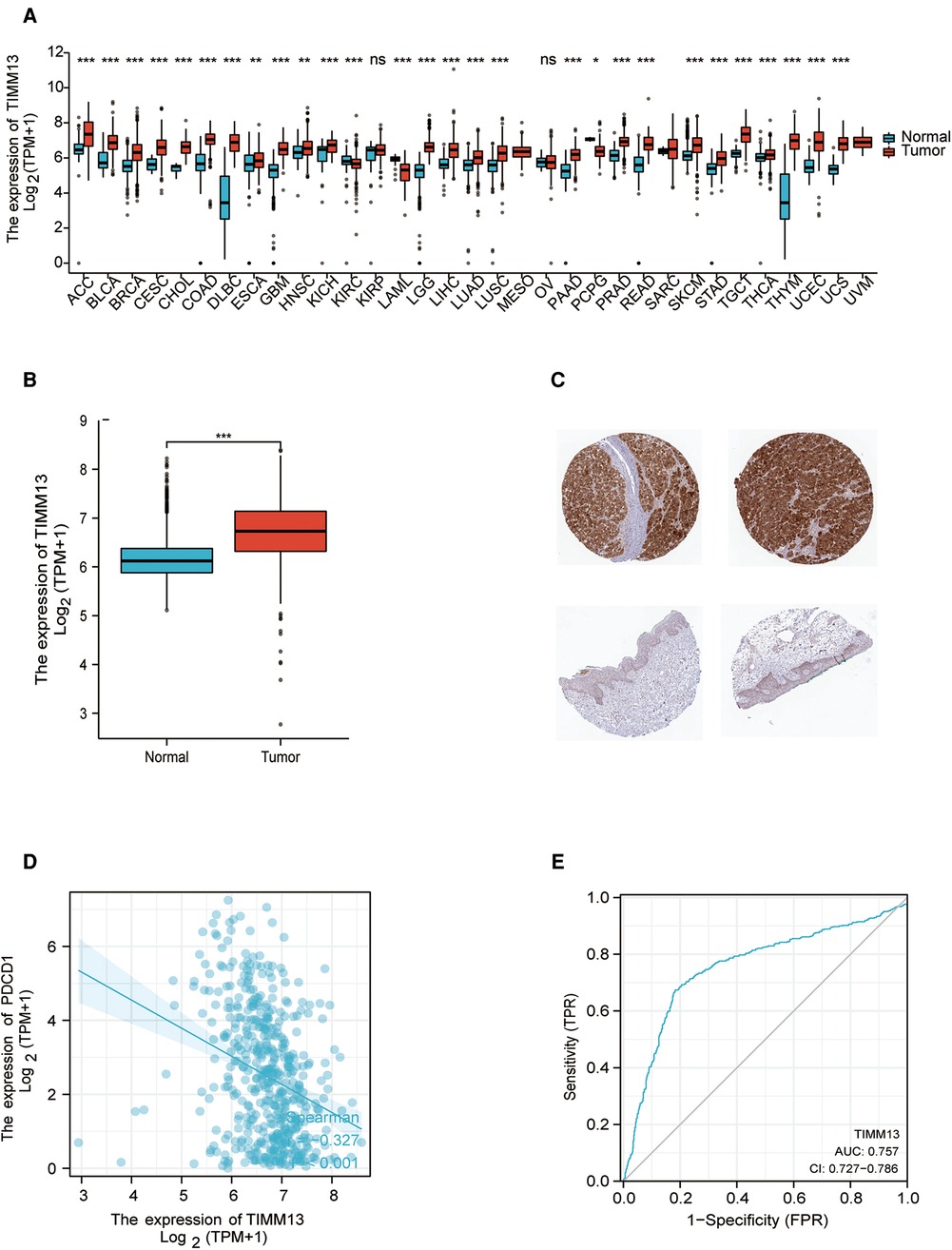
Figure 1. TIMM13 expression levels. (A) Increased or decreased TIMM13 in different tumor types from The Cancer Genome Atlas (TCGA) database were determined by Xiantao tool (*p < 0.05, **p < 0.01, ***p < 0.001). (B) Increased TIMM13 in SKCM tissues compared with normal tissues. (C) TIMM13 immunohistochemical staining levels in SKCM tissues (up) and normal tissues (down) by using HPA database. (D) The correlation analysis between TIMM13 and PD1 mRNA level. (E) The receiver-operating characteristic (ROC) curve analysis of TIMM13 in SKCM patients.
To validate these results in SKCM, cancer samples from the TCGA database and normal samples from GTEx database were tested by xiantao tool. As shown in Figure 1B, it was found that TIMM13 mRNA expression was significantly higher in SKCM samples (469 cases) than that in normal samples (813 cases) (p < 0.05) from GETx. Based on the HPA website, immunohistochemistry confirmed the TIMM13 protein expression pattern (Figure 1C). It is worth noting that the increased expression of TIMM13 mRNA was negatively correlated with PD1 (Figure 1D), where the AUC of TIMM13 in SKCM is 0.757 (95% CI is 0.727 to 0.786) (Figure 1E). It is suggested that TIMM13 was significantly elevated in SKCM tissues, which may be a potential biomarker for the diagnosis of SKCM.
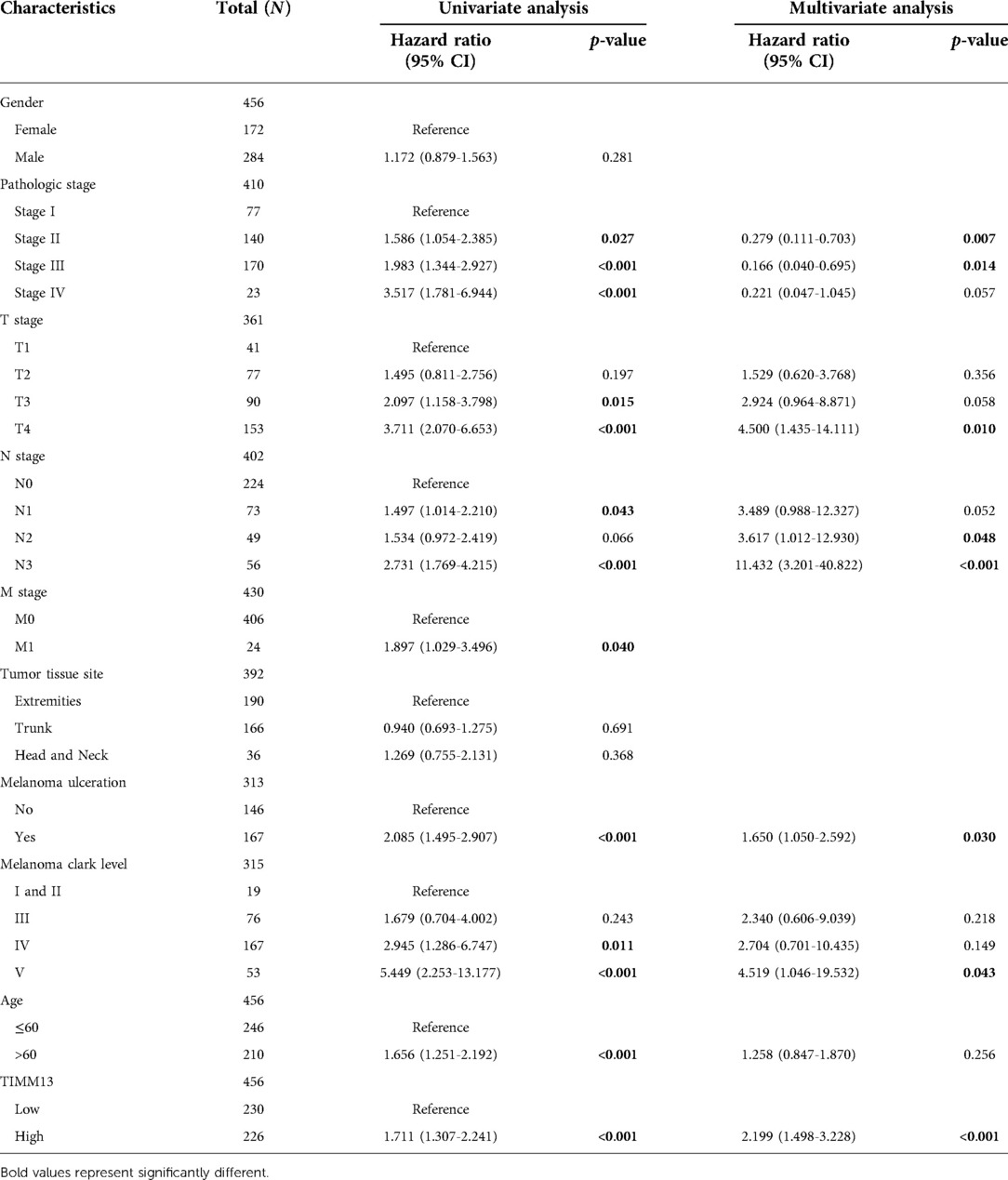
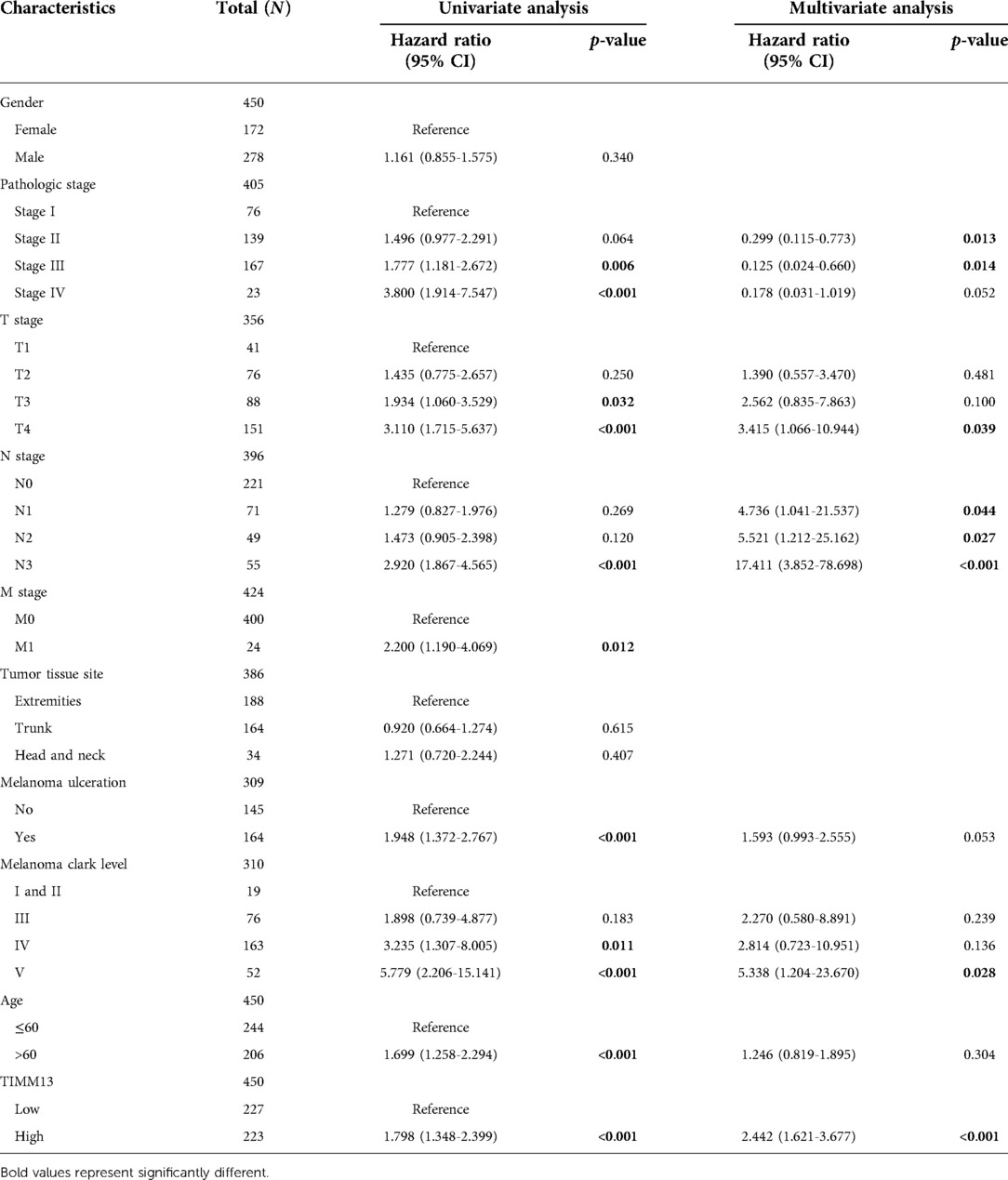
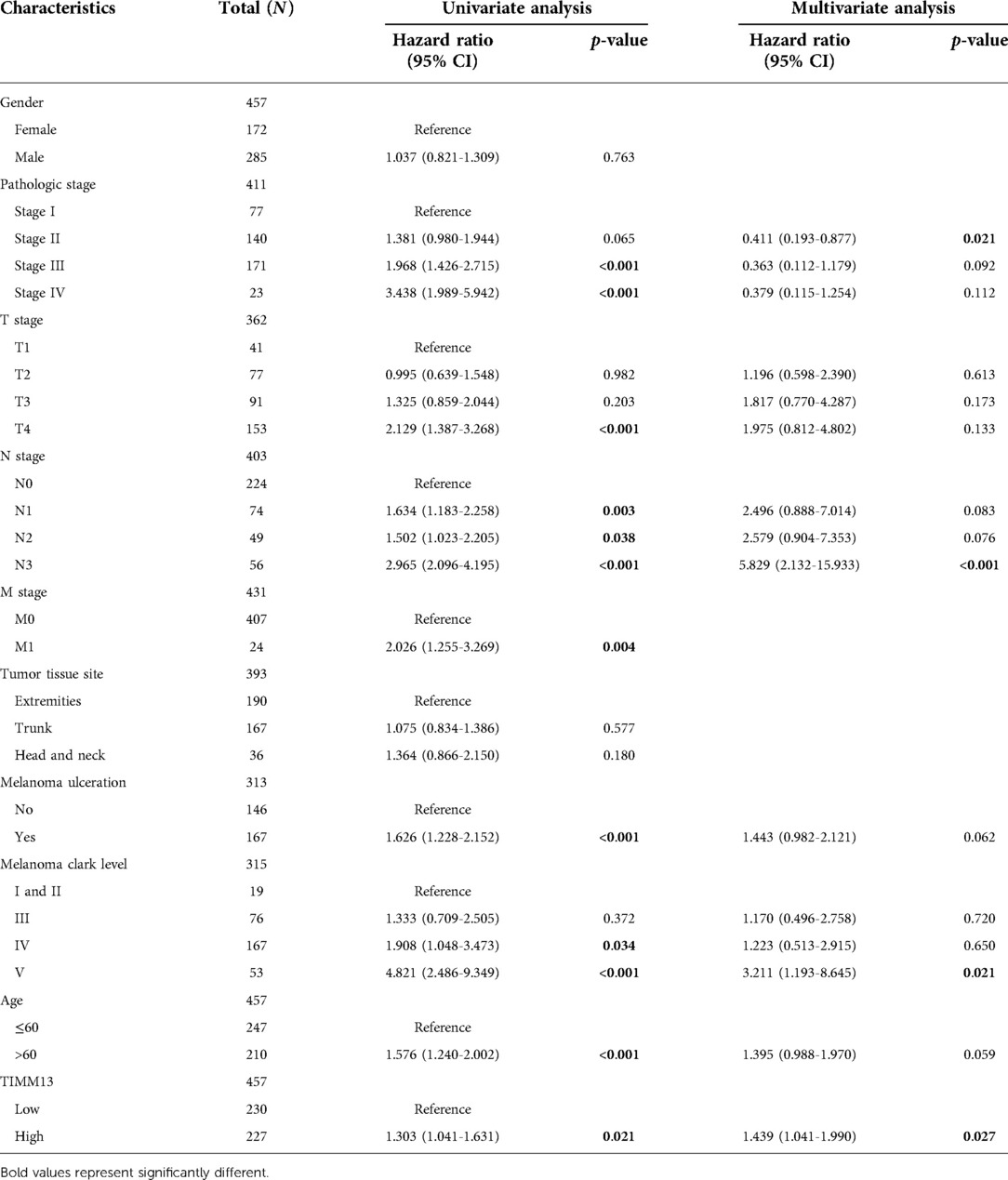
Relationship between TIMM13 expression and patient clinical pathology in SKCM
Using the UALCAN and the Xiantao tool, we investigated the relationship between TIMM13 expression and several clinicopathological features, such as tumor type, stage, lymph node stage, and TP53 mutation shown in Figure 2A, the expression of TIMM13 in SKCM metastatic cancer tissues was significantly higher than that in primary cancer tissues and normal cancer tissues (p = 0. 0018). There was no significant difference between different cancer stages (Figure 2B), different lymph nodes (Figure 2C) and TP53 mutation (Figure 2D). Secondly, in order to further understand the function and possible mechanism of TIMM13 in tumorigenesis, we used univariate and multivariate Cox regression analysis to observe the correlation between TIMM13 expression and clinicopathological features of SKCM. The up-regulation of TIMM13 expression was related to a poorer OS (HR = 2. 199, p < 0.001) (Table 1), DSS (Table 2) (HR = 2. 442, p < 0.001) and PFI (Table 3) (HR = 1. 439, p = 0. 027) in SKCM patients. The increase of TIMM13 mRNA expression was related to a poorer OS in T4 stage (HR = 4. 500, p = 0. 010), N2 stage (HR = 3. 617, p = 0. 048), N3 stage (HR = 11. 432, p < 0.001), melanoma ulceration (HR = 1. 650, p = 0. 030), and Melanoma Clark V level (HR = 4. 519, p = 0.043) SKCM patients. Furthermore, we found that DSS and PFI in T4 stage (DSS HR = 3.415, p = 0.039), N1 stage (DSS HR = 4.736, p = 0.044), N2 stage (DSS HR = 5.521, p = 0.027), N3 stage (DSS HR = 17.411, p < 0.001; PFI HR = 5.829, p < 0.001), Melanoma Clark V level (DSS HR = 5.338, p = 0.028; PFI HR = 3.211, p = 0.021) were associated with TIMM13 expression. It was a hint that the prognostic effect of TIMM13 in SKCM might be influenced by their clinical characteristics.
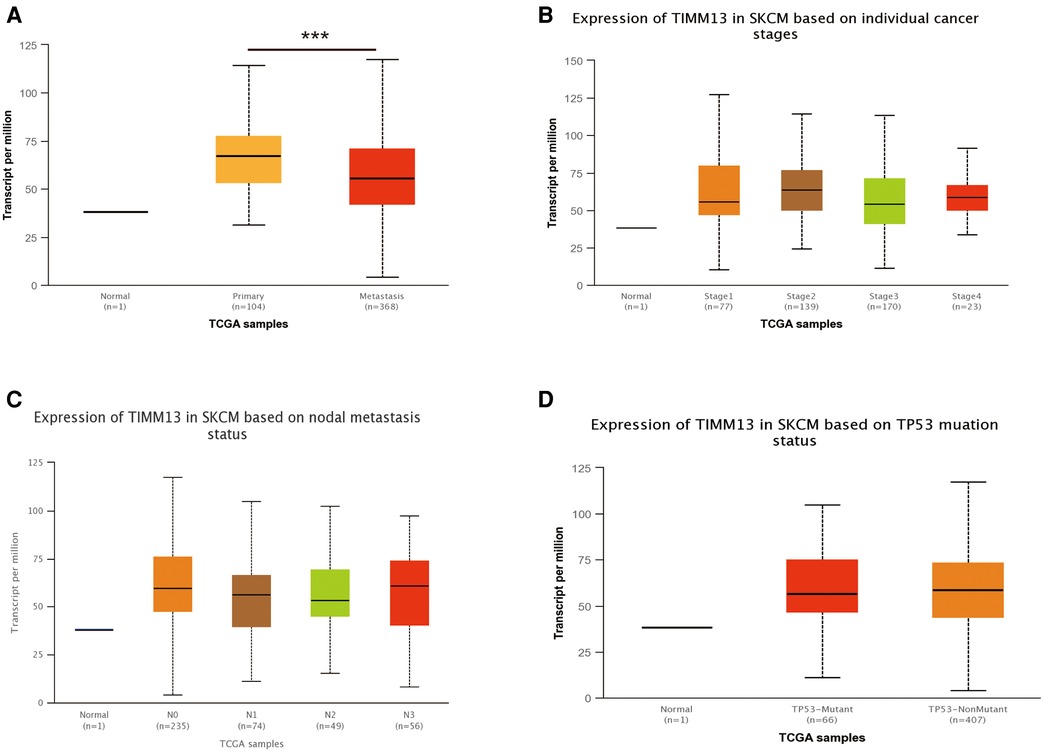
Figure 2. Correlation between TIMM13 mRNA expression level and clinicopathological parameters of SKCM through the UALCAN database. (A) Sample type (normal/primary tumor). (B) Cancer stage (stage 1, 2, 3, and 4). (C) Lymph node stage (N0 1, 2, and 3). (D) TP53 mutation subgroup. N, normal; P, primary tumor; S1, stage 1; S2, stage 2; S3, stage 3; S4, stage 4.
Increased TIMM13 mRNA expression associated with poor overall survival in SKCM patients
It was suggested that the expression level of TIMM13 mRNA in SKCM patients is higher than that in the normal control group. Therefore, whether the expression of TIMM13 was related to tumor prognosis needs further study. In this study, the expression of TIMM13 and its relationship with prognosis were detected by the Kaplan–Meier survival curve to determine whether TIMM13 can be used as a biomarker for prognosis of SKCM. It was worth noting that the high expression of TIMM13 was associated with a poorer outcome of SKCM. High expression of TIMM13 was associated with poorer OS, and PFI (Figures 3A,B).
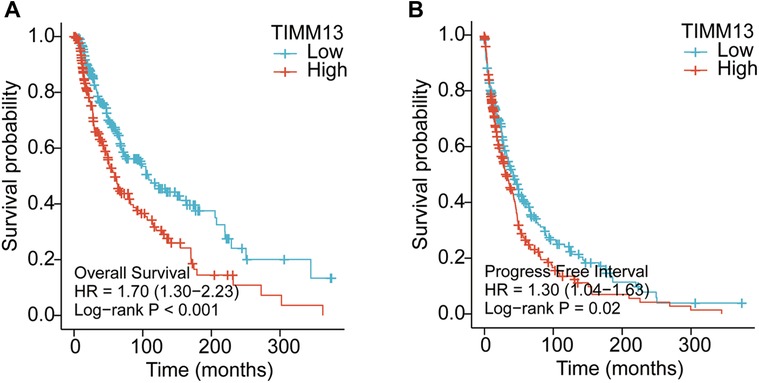
Figure 3. Kaplan–Meier survival curves comparing the high and low expression of TIMM13 in SKCM by using Xiantao tool. Survival curves of OS (A), FPI (B) in the SKCM patients. OS, overall survival; PFI, progression free interval.
Correlation between immune infiltration and TIMM13 expression in SKCM
Immune infiltration plays an important role in tumor progression. We observed whether the expression of TIMM13 affected the number of tumors infiltrating lymphocytes (TILs) in SKCM by using the Xiantao tool. As a result, the expression of TIMM13 was negatively correlated with StromalScore, ImmuneScore, and ESTIMATEScore of SKCM (rho = −0.307, p < 0.001; rho = −0.398, p < 0.001; rho = −0.393, p < 0.001, respectively) (Figure 4A). Our results also revealed a significant correlation between TIMM13 and TILs abundance (Figure 4B). The high expression of TIMM13 was negatively correlated with the infiltration of Th1 cells (rho = −0.416) (Figure 4C) and T lymphocytes (Rho = −0.415) (Figure 4D), aDC cells (rho = −0.338) (Figure 4E), TFH cells (rho = −0.366) (Figure 4F), B lymphocytes (Rho = −0.359) (Figure 4G) and T helper T cells (rho = −0.354) (Figure 4H). All the p-values above were <0.001. Similar results were obtained by detecting CD8 + T lymphocyte infiltration using the TIMER database, suggesting that TIMM13 could play a key role in inhibiting SKCM immune infiltration and was related to tumor microenvironment.
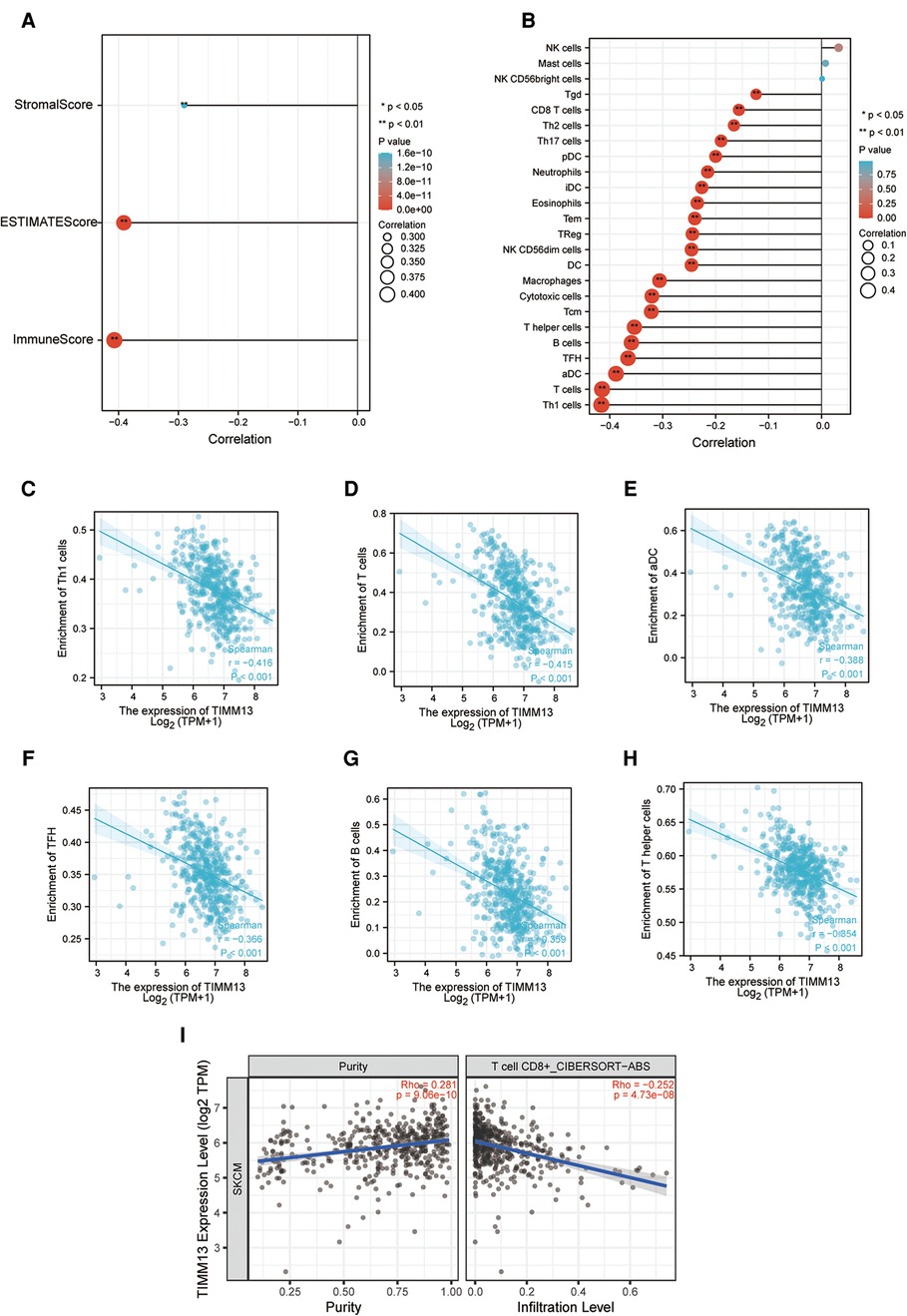
Figure 4. Correlation of TIMM13 expression with immune infiltration in SKCM. (A) Correlation of TIMM13 expression with infiltration levels of StomalScore, ESTIMATEScore, and ImmuneScore in SKCM available at Xiantao tool. (B) Correlation of TIMM13 expression with infiltration levels of immune cells in SKCM available at Xiantao tool. Correlation of ITGAL expression with infiltration levels of Th1 cells (C), T cells (D), aDC (E), TFH (F), B cells (G), and T helper in SKCM (H). (I) Correlation between the expression of TIMM13 and the abundance of TILs in SKCM validation at TIMER database.
The correlation between TIMM13 and different TILs' biomarkers in SKCM was studied by using the Xiantao tool. We found that TIMM13 was associated with most TILs' markers in SKCM. Several functional T lymphocytes, including Th1, Tregs and exhausted T lymphocytes, were also investigated. In particular, TIMM13 is significantly associated with most sets of TILs immunomarkers in SKCM (Table 4).
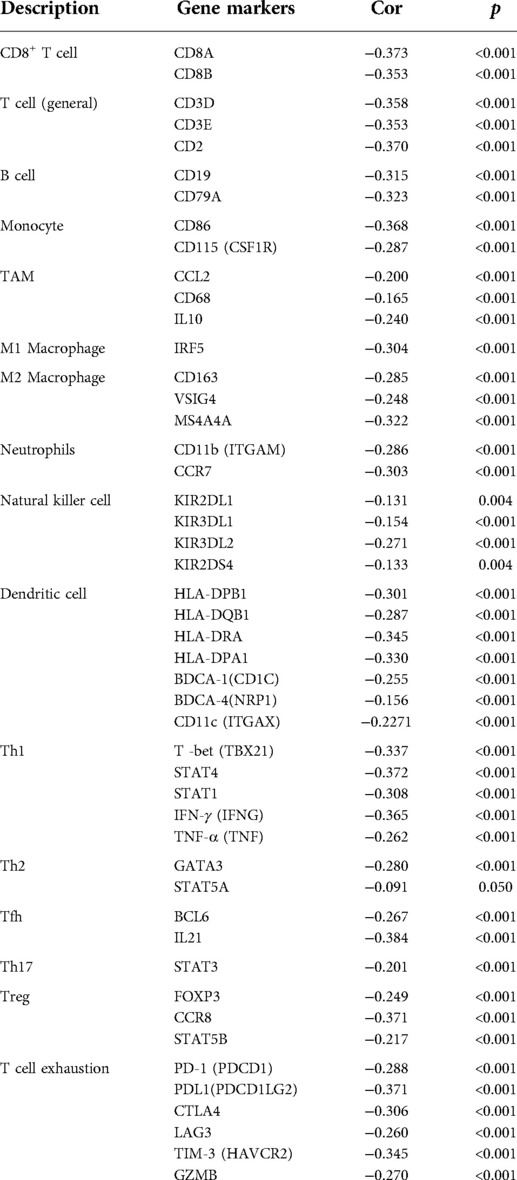
Table 4. Correlation analysis between ITGAL and related genes and markers of immune cells in Xiantao tool.
Furthermore, TIMM13 was significantly associated with most of monocytes, TAM, M2 macrophages and T cell exhaustion markers in SKCM (Table 4). As shown in the table, PD-1, PDL1, CTLA4, LAG3, TIM-3, GZMB of T-cell exhaustion, and CCL-2, CD68, IL10 of TAMs, IRF5 of M1 phenotype and CD163, VSIG4 and MS4A4A of M2 phenotype were almost negatively correlated with TIMM13 in SKCM (p < 0.0001). It was suggested that TIMM13 could regulate exhaustion, and macrophage polarization in SKCM.
The expression of TIMM13 is related to immunoinhibitors and immunostimulators in SKCM
Immunoinhibitors and immunostimulators are substances that influence the function of the immune system. This study showed that TIMM13 was significantly associated with immunoinhibitors (p < 0.001), such as BTLA (rho = −0.389), CD274 (rho = −0.476), CD96 (rho = −0.404), IL10 (rho = −0.328), PDCD1LG2 (rho = −0.458), and TIGIT (rho = −0.342) (Figure 5A). The expression of TIMM13 was also significantly associated with immunostimulators (p < 0.001), including CD28 (rho = −0.389), CD80 (rho = −0.44), IL2RA (rho = −0.434), TNFRSF9 (rho = −0.417), TNFSF13B (rho = −0.402), TNFSF4 (rho = −0.396) (Figure 5B). These results proposed that TIMM13 was intimately engaged in the regulation of the immune interaction and might modulate tumor immune escape.
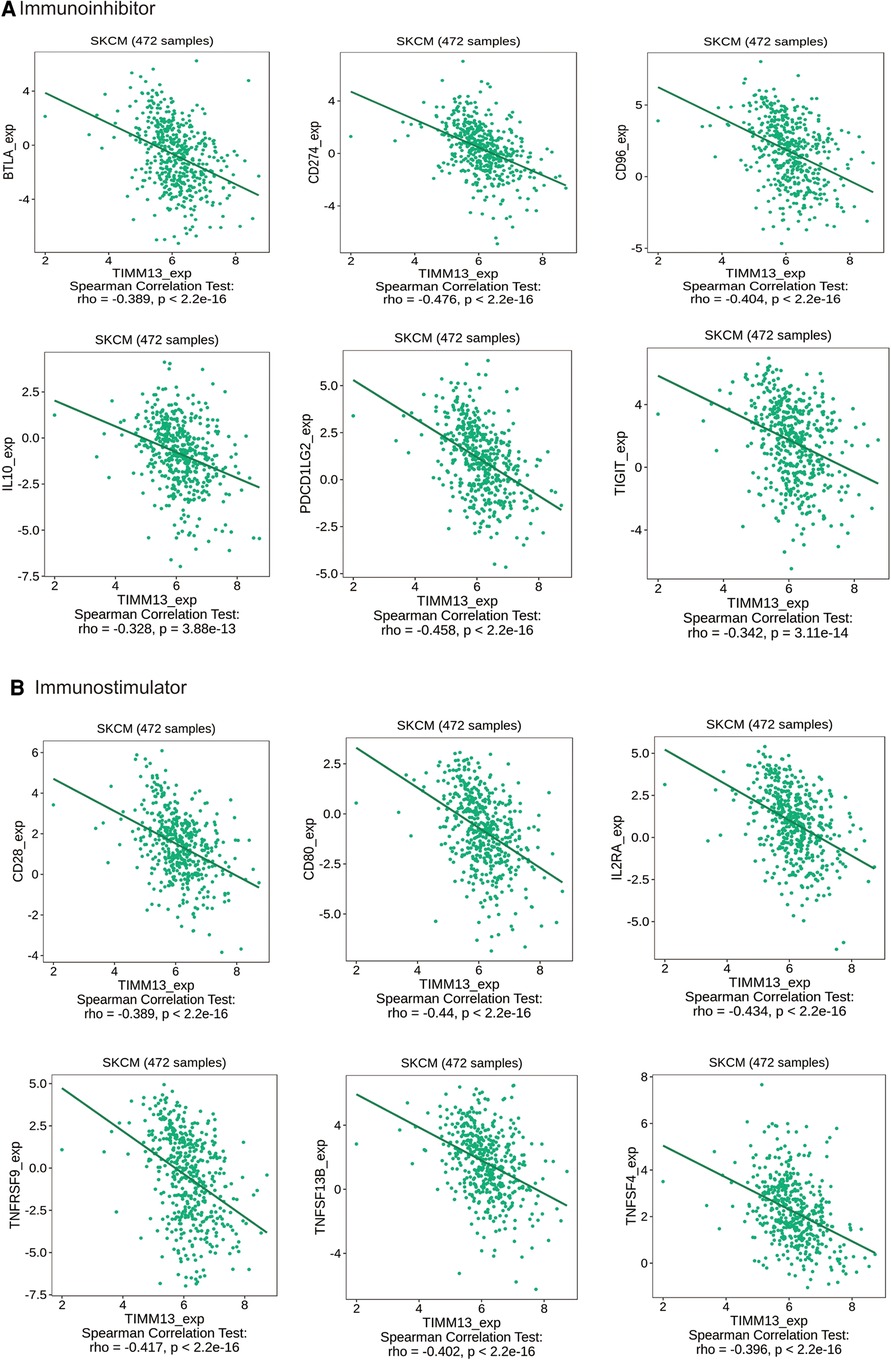
Figure 5. The expression of TIMM13 is associated with immunomodulators in SKCM. (A) Correlation between TIMM13 expression and immunoinhibitors in SKCM available at TISIDB database. (B) Correlation between TIMM13 expression and immunostimulators in SKCM available at TISIDB database. Color images are available online.
Correlation between the TIMM13 expression and chemokines/receptors in SKCM
Chemokines played a great function in controlling the infiltration degree of immune cell. This research implicated a significant association between TIMM13 expression and chemokines. For instance, the expression of TIMM13 was significantly associated with CCL8 (rho = −0.293), CXCL9 (rho = −0.359), CXCL10 (rho = −0.347), CXCL10 (rho = −0.347), CXCL11 (rho = −0.375), CXCL12 (rho = −0.33), and CXCL13 (rho = −0.372) (Figure 6A). All the values of p were < 0.001. At the same time, we found that the expression of TIMM13 was also significantly related with chemokine receptors (p < 0.001), including CCR1 (rho = −0.375), CCR2 (rho = −0.429), CCR4 (rho = −0.441), CCR5 (rho = −0.362), CCR8 (rho = −0.432), XCR1 (rho = −0.385) (Figure 6B). These results further suggested that TIMM13 may be an immunoregulatory factor in SKCM.
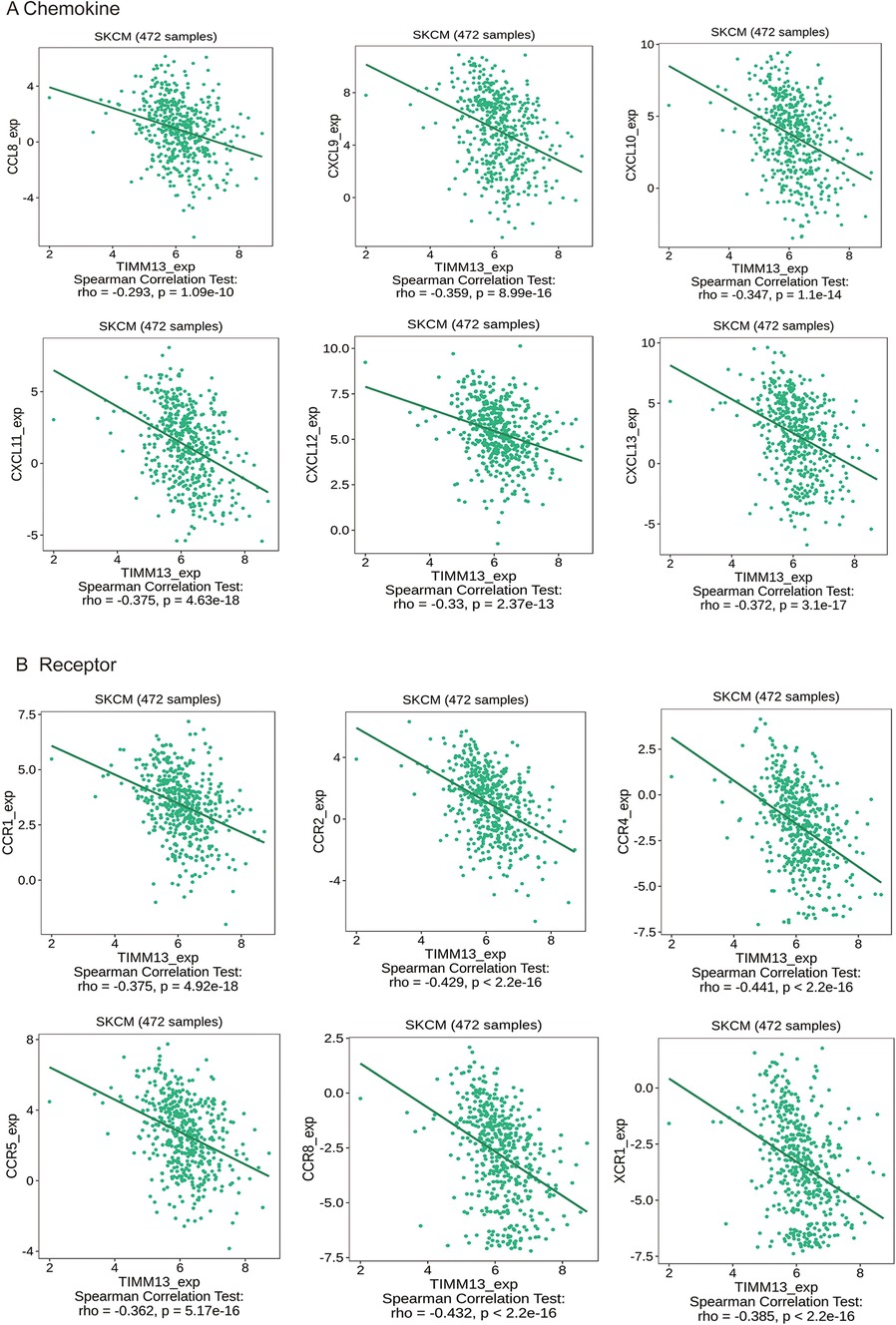
Figure 6. Correlation between the expression of TIMM13 and chemokines in SKCM. (A) Correlation between TIMM13 expression and chemokines in SKCM available at TISIDB database. (B) Correlation between TIMM13 expression and chemokine receptors in SKCM available at TISIDB database. Color images are available online.
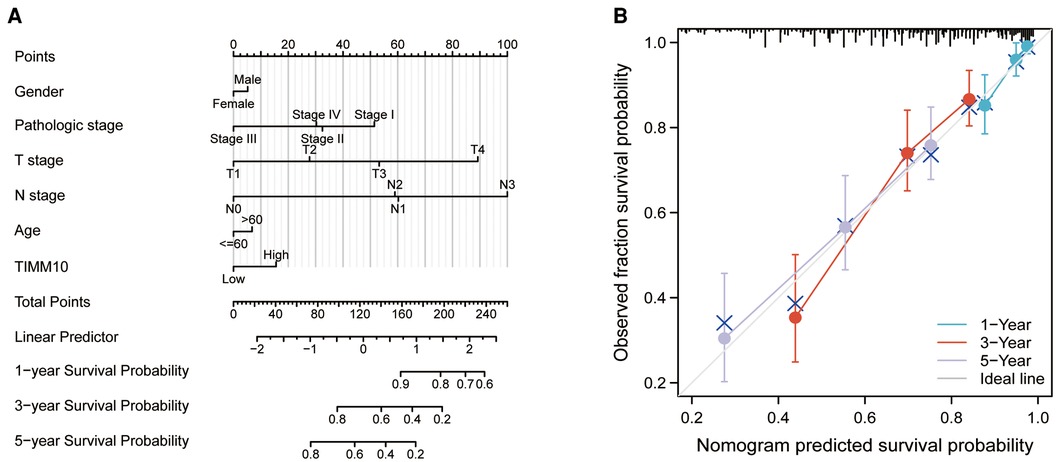
Construction and validation of a nomogram
A nomogram was built for the training set based on the gender, pathologic stage, TNM stage, age, and TIMM13 expression (Figure 7A). The C-index of the nomogram was 0.715(0.693–0.736). The calibration plots for the 1-, 3-, and 5-year survivals indicated good agreement between the actual observations and the predictions (Figure 7B). These results indicated that the prediction performance of the nomogram was good.
Histologic analysis
We next explored the protein expression levels of TIMM13 between melanoma and normal skin tissues. The IHC staining results showed that TIMM13 showed higher expression levels in melanoma tissues (n = 25) than in normal skin tissues (n = 15) (Figures 8A,B). The patients' characteristics were shown in Table 5.
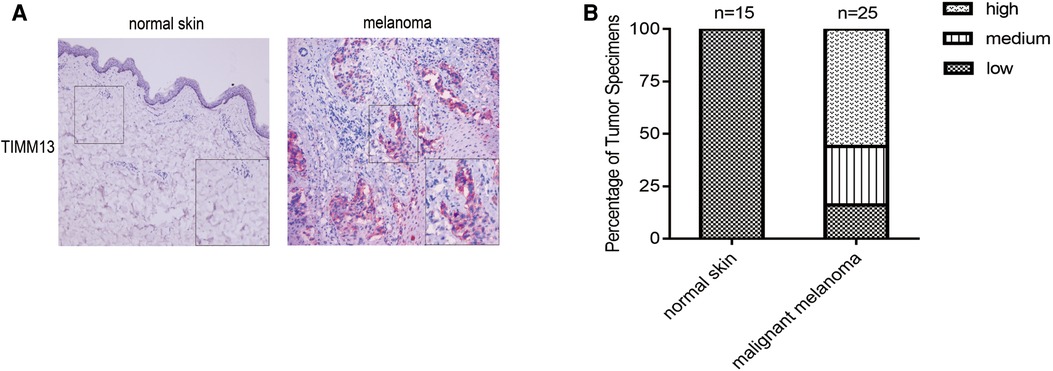
Figure 8. Gene expression of TIMM13 in melanoma tissue and normal skin specimens. Using IHC staining, TIMM13 was expressed at higher levels in the melanoma tissue (n = 25) when compared to normal skin (n = 15). (A) IHC staining. (B) Quantification of the TIMM13 levels. IHC: Immunohistochemistry. IHC stain, AEC, original magnification: 100× (inset, IHC stain, AEC, original magnification: 400×).
Discussion
In this study, the expression level of TIMM13 in SKCM and its clinical significance were comprehensively studied by bioinformatics. Our results showed that poor prognosis was in accordance with high expression of TIMM13 in SKCM. The expression of TIMM13 is closely related to the infiltration of various immune cells, immunomodulators, chemokines and receptors in SKCM. Therefore, our study provided new insights into the key functions of TIMM13, which might be a prognostic biomarker related to immune infiltration of SKCM.
TIMM13 partners with TIMM8a in the mitochondrial intermembrane space to form a 70 kDa complex and facilitates the import of the inner membrane substrate TIMM23 (9). Kim SH et al. reported that TIMM13 functions as a target gene of miRNA-1273g-3p to contribute to Alzheimer's Disease pathogenesis by regulating expression of mitochondrial genes (22). Roesch K et al. reported that human deafness dystonia syndrome was caused by a defect in assembly of the DDP1/TIMM8a-TIMM13 complex. Timm13 is related to Mohr-Tranebjaerg Syndrome and Visual Cortex Disease. Among its related pathways are Peroxisomal lipid metabolism. Several studies have shown that TIMM13 was differently expressed in metastatic susceptibility (13), hepatocellular carcinoma (14), breast cancer (15) et al. These researchers suggested that TIMM13 might have a significant influence on cancer, and may be a novel target in treating a variety of malignancies. However, the possible function of TIMM13 in regulating tumor immunity and its clinical significance in SKCM are still unknown.
Therefore, we computed the TIMM13 expression for SKCM using the Xiantao tool and the UALCAN database. We found that TIMM13 was abnormally expressed in the tissues of various malignant tumors. TIMM13 in SKCM was significantly higher than that in adjacent tissues. Using the HPA database, we also found that TIMM13mRNA and protein levels in most SKCM samples were higher than those in matched paracancer samples. It was suggested that the expression level of TIMM13 could be used as a diagnostic indicator of SKCM with the AUC is 0.757. In addition, in order to determine whether TIMM13 could be used as a biomarker for prognosis, we analyzed the correlation between TIMM13 expression and OS, and FPI in SKCM patients with the Xiantao tool. Furthermore, to confirm whether TIMM13 can be used as a prognostic biomarker, we used the xiantao tool to analyze the correlation between the TIMM13 expression and OS, DSS, and FPI in SKCM patients. Notably, analysis of this database indicated that the higher TIMM13 expression correlated with HR for worse OS DSS, and poorer PPS of SKCM. In addition, upregulated TIMM13 expression had a significant correlation with a worse prognosis of SKCM in T4 stage, N1 stage, N2 stage, N3 stage. Taken together, these observations supported our hypothesis that TIMM13 was a prognostic biomarker in SKCM.
Additionally, this study found that TIMM13 was correlated with the degree of immune infiltration of SKCM. In the cancer microenvironment, immune cell infiltration had been proved to play a key role in the development and progression of cancer (23, 24). TIMM13 is a chaperone protein, which plays a key role in transporting cytoplasmic proteins into the mitochondrial inner membrane. At present, it is not clear whether the expression of TIMM13 is related to the immune infiltration of SKCM. Therefore, we systematically discussed the relationship between TIMM13 expression and immune infiltration degree of SKCM. Based on our results, it was found for the first time that TIMM13 modulates immune infiltration through SKCM.
The expression of TIMM13 was closely related to the expression of TILs in CD8 + T cells, CD4 + T cells, Treg cells, and TAM cells. Meanwhile, the increase of TIMM13 expression was related to immunoregulators, chemokines and receptors. Additionally, the study proposed the relationship between TIMM13 expression and TILs’ marker genes of SKCM. The expression of TIMM13 was associated with M2 macrophage markers CD163, VSIG4, and MS4A4A, while M1 macrophage markers NOS2 and IRF5 were slightly associated with the expression of TIMM13. Macrophages played an important role in tumor proliferation (25), angiogenesis (26), invasion (27), metastasis (27) and tumor immunity (28). These results demonstrated that TIMM13 had the potential function of regulating TAMs polarization. The up-regulation of TIMM13 was closely related to Tregs markers (FOXP3, CCR8) and T lymphocyte depletion markers (PD1, CTLA4, LAG3). Blocking immune checkpoints is the main strategy of immunotherapy (29). The most important thing is to enhance the response of tumor cells to immune checkpoint inhibitors and cytokines (30, 31). According to TISIDB, TIMER and Xiantao tool, our results showed that the up-regulation of TIMM13 expression was not only related to PD1 and CTLA4, but also significantly related to cell response to chemokines. These results suggested that targeting TIMM13 may be a strategy to improve the efficacy of immunotherapy. It was also suggested that TIMM13 played an important role in the recruitment and regulation of TILs in SKCM, and its molecular mechanism and role in the regulation of tumor microenvironment deserve further study.
However, there are also some limitations in our research. One limitation is that most of the data is based on online platforms, which are constantly updated and extended; So, the research results may be influenced. Secondly, our study did not include any information about complications and therapy options. Thirdly, in vivo and in vitro experiments are not to verify the role of TIMM13 in SKCM. However, in future research, we are committed to paying more attention to the background information of patients and conducting experiments to further verify the expected results.
Conclusions
The increased expression of TIMM13 was closely related to poor prognosis of SKCM and increased immune infiltration of CD8 + T lymphocytes, C4 + T lymphocytes, and myeloid dendritic cells. The expression of TIMM13 might be involved in the regulation of M2, Treg, and T -cell exhaustion. So, this study suggested that TIMM13 might have a new potential function in the regulation of immune cell infiltration in SKCM patients.
Data availability statement
The original contributions presented in the study are included in the article/Suplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
RHY, XBP, and JHL designed the study. STZ and YYH conducted most of the experiments, data analysis, and wrote the manuscript. RHY, XBP, and JHL had full access to all of the data in the manuscript and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (82002913), Guangdong Basic and Applied Basic Research Foundation (2021A1515011453, 2022A1515012160, 2021B1515120036, and 2022A1515012245), the Medical Scientific Research Foundation of Guangdong Province (A2022293), Foshan 14th - fifth high-level key specialty construction project, Yunnan Fundamental Research Projects (grant NO. 202001AT070145, 202101AT070288).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Elder DE, Bastian BC, Cree IA, Massi D, Scolyer RA. The 2018 world health organization classification of cutaneous, mucosal, and uveal melanoma: detailed analysis of 9 distinct subtypes defined by their evolutionary pathway. Arch Pathol Lab Med. (2020) 144(4):500–22. doi: 10.5858/arpa.2019-0561-RA
2. Timar J, Ladanyi A. Molecular pathology of skin melanoma: epidemiology, differential diagnostics, prognosis and therapy prediction. Int J Mol Sci. (2022) 23(10):5384. doi: 10.3390/ijms23105384
3. Villani A, Potestio L, Fabbrocini G, Troncone G, Malapelle U, Scalvenzi M. The treatment of advanced melanoma: therapeutic update. Int J Mol Sci. (2022) 23(12):6388. doi: 10.3390/ijms23126388
4. Rebecca VW, Somasundaram R, Herlyn M. Pre-clinical modeling of cutaneous melanoma. Nat Commun. (2020) 11(1):2858. doi: 10.1038/s41467-020-15546-9
5. Schadendorf D, van Akkooi ACJ, Berking C, Griewank KG, Gutzmer R, Hauschild A, et al. Melanoma. Lancet. (2018) 392(10151):971–84. doi: 10.1016/S0140-6736(18)31559-9
6. Kim G, McKee AE, Ning YM, Hazarika M, Theoret M, Johnson JR, et al. FDA Approval summary: vemurafenib for treatment of unresectable or metastatic melanoma with the BRAFV600E mutation. Clin Cancer Res. (2014) 20(19):4994–5000. doi: 10.1158/1078-0432.CCR-14-0776
7. Rajkumar S, Berry D, Heney KA, Strong C, Ramsay L, Lajoie M, et al. Melanomas with concurrent BRAF non-p.V600 and NF1 loss-of-function mutations are targetable by BRAF/MEK inhibitor combination therapy. Cell Rep. (2022) 39(1):110634. doi: 10.1016/j.celrep.2022.110634
8. Kuryk L, Bertinato L, Staniszewska M, Pancer K, Wieczorek M, Salmaso S, et al. From conventional therapies to immunotherapy: melanoma treatment in review. Cancers (Basel). (2020) 12(10):3057. doi: 10.3390/cancers12103057
9. Roesch K, Hynds PJ, Varga R, Tranebjaerg L, Koehler CM. The calcium-binding aspartate/glutamate carriers, citrin and aralar1, are new substrates for the DDP1/TIMM8a-TIMM13 complex. Hum Mol Genet. (2004) 13(18):2101–11. doi: 10.1093/hmg/ddh217
10. Roesch K, Curran SP, Tranebjaerg L, Koehler CM. Human deafness dystonia syndrome is caused by a defect in assembly of the DDP1/TIMM8a-TIMM13 complex. Hum Mol Genet. (2002) 11(5):477–86. doi: 10.1093/hmg/11.5.477
11. Blesa JR, Solano A, Briones P, Prieto-Ruiz JA, Hernandez-Yago J, Coria F. Molecular genetics of a patient with Mohr-Tranebjaerg Syndrome due to a new mutation in the DDP1 gene. Neuromolecular Med. (2007) 9(4):285–91. doi: 10.1007/s12017-007-8000-3
12. Shi X, Huang Z, Zhou G, Li C. Dietary protein from different sources exerted a great impact on lipid metabolism and mitochondrial oxidative phosphorylation in rat liver. Front Nutr. (2021) 8:719144. doi: 10.3389/fnut.2021.719144
13. Hu Y, Wu G, Rusch M, Lukes L, Buetow KH, Zhang J, et al. Integrated cross-species transcriptional network analysis of metastatic susceptibility. Proc Natl Acad Sci U S A. (2012) 109(8):3184–9. doi: 10.1073/pnas.1117872109
14. Li Z, Song G, Guo D, Zhou Z, Qiu C, Xiao C, et al. Identification of GINS2 prognostic potential and involvement in immune cell infiltration in hepatocellular carcinoma. J Cancer. (2022) 13(2):610–22. doi: 10.7150/jca.53841
15. Sanchez-Alvarez R, De Francesco EM, Fiorillo M, Sotgia F, Lisanti MP. Mitochondrial fission factor (MFF) inhibits mitochondrial metabolism and reduces breast cancer stem cell (CSC) activity. Front Oncol. (2020) 10:1776. doi: 10.3389/fonc.2020.01776
16. Yan Y, Li J, Ye M, Li Z, Li S. Tropomyosin is potential markers for the diagnosis and prognosis of bladder cancer. Dis Markers. (2022) 2022:6936262. doi: 10.1155/2022/6936262
17. The Cancer Genome Atlas Network. Genomic classification of cutaneous melanoma. Cell. (2015) 161(7):1681–96. doi: 10.1016/j.cell.2015.05.044
18. Consortium GT. The genotype-tissue expression (GTEx) project. Nat Genet. (2013) 45(6):580–5. doi: 10.1038/ng.2653
19. Chandrashekar DS, Karthikeyan SK, Korla PK, Patel H, Shovon AR, Athar M, et al. UALCAN: an update to the integrated cancer data analysis platform. Neoplasia. (2022) 25:18–27. doi: 10.1016/j.neo.2022.01.001
20. Li T, Fu J, Zeng Z, Cohen D, Li J, Chen Q, et al. TIMER2.0 For analysis of tumor-infiltrating immune cells. Nucleic Acids Res. (2020) 48(W1):W509–14. doi: 10.1093/nar/gkaa407
21. Ru B, Wong CN, Tong Y, Zhong JY, Zhong SSW, Wu WC, et al. TISIDB: an integrated repository portal for tumor-immune system interactions. Bioinformatics. (2019) 35(20):4200–2. doi: 10.1093/bioinformatics/btz210
22. Kim SH, Choi KY, Park Y, McLean C, Park J, Lee JH, et al. Enhanced expression of microRNA-1273g-3p contributes to Alzheimer’s disease pathogenesis by regulating the expression of mitochondrial genes. Cells. (2021) 10(10):2697. doi: 10.3390/cells10102697
23. Kim S, Kim A, Shin JY, Seo JS. The tumor immune microenvironmental analysis of 2,033 transcriptomes across 7 cancer types. Sci Rep. (2020) 10(1):9536. doi: 10.1038/s41598-020-66449-0
24. Georgescu SR, Tampa M, Mitran CI, Mitran MI, Caruntu C, Caruntu A, et al. Tumour microenvironment in skin carcinogenesis. Adv Exp Med Biol. (2020) 1226:123–42. doi: 10.1007/978-3-030-36214-0_10
25. Yan K, Wang Y, Lu Y, Yan Z. Coexpressed genes that promote the infiltration of M2 macrophages in melanoma can evaluate the prognosis and immunotherapy outcome. J Immunol Res. (2021) 2021:6664791. doi: 10.1155/2021/6664791
26. Pratt HG, Steinberger KJ, Mihalik NE, Ott S, Whalley T, Szomolay B, et al. Macrophage and neutrophil interactions in the pancreatic tumor microenvironment drive the pathogenesis of pancreatic cancer. Cancers (Basel). (2021) 14(1):194. doi: 10.3390/cancers14010194
27. Zhang H, Luo YB, Wu W, Zhang L, Wang Z, Dai Z, et al. The molecular feature of macrophages in tumor immune microenvironment of glioma patients. Comput Struct Biotechnol J. (2021) 19:4603–18. doi: 10.1016/j.csbj.2021.08.019
28. Yin W, Li Y, Song Y, Zhang J, Wu C, Chen Y, et al. CCRL2 Promotes antitumor T-cell immunity via amplifying TLR4-mediated immunostimulatory macrophage activation. Proc Natl Acad Sci U S A. (2021) 118(16):e2024171118. doi: 10.1073/pnas.2024171118
29. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. (2012) 12(4):252–64. doi: 10.1038/nrc3239
30. Jenkins L, Jungwirth U, Avgustinova A, Iravani M, Mills AP, Haider S, et al. Cancer-associated fibroblasts suppress CD8+ T cell infiltration and confer resistance to immune checkpoint blockade. Cancer Res. (2022). doi: 10.1158/0008-5472. [Epub ahead of print]35749591
Keywords: cutaneous melanoma, translocase of inner mitochondrial membrane 13 (TIMM13), prognosis, biomarker, tumor immune microenvironment
Citation: Zhou S, Han Y, Yang R, Pi X and Li J (2022) TIMM13 as a prognostic biomarker and associated with immune infiltration in skin cutaneous melanoma (SKCM). Front. Surg. 9:990749. doi: 10.3389/fsurg.2022.990749
Received: 10 July 2022; Accepted: 1 August 2022;
Published: 17 August 2022.
Edited by:
Jiliang Zhou, Georgia Health Sciences University, United States© 2022 Zhou, Han, Yang, Pi and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiehua Li amllaHVhbGlfZnNAMTYzLmNvbQ== Xiaobing Pi cHhiaW5naWNlQDE2My5jb20= Ronghua Yang YV9od2E5OTEzMTZAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Sitong Zhou
Sitong Zhou Yuanyuan Han
Yuanyuan Han Ronghua Yang
Ronghua Yang Xiaobing Pi1*
Xiaobing Pi1*