- Department of Neurosurgery, The First Affiliated Hospital of Nanchang University, Nanchang, China
Background: Traumatic spinal cord injury (TSCI) is a type of highly disabling central nervous system trauma. In this study, we investigated the epidemiological characteristics of 1,806 TSCI patients and compared the characteristics of patients with traumatic cervical spinal cord injury (TCSCI) caused by cervical fracture/dislocation and disc herniation/bulging.
Methods: We retrospectively reviewed the hospital records of 1,806 TSCI patients. The detailed information included gender, marital status, occupation, age, neurological level of injury, etiology, American Spinal Injury Association (ASIA) grade, combined injuries, complications, treatment, the interval between admission and surgery, intubation/tracheostomy requirement, and the length of hospital stay.
Results: Cervical spinal cord injury (CSCI) was the most common injury. Compared to non-CSCI cases, patients with TCSCI were older, and more likely to suffer from tetraplegia and require intubation/tracheostomy, but had fewer other injuries or complications and a shorter length of hospital stay. Compared to patients with cervical fracture/dislocation, those with TCSCI caused by disc herniation/bulging were older and more likely to suffer from paraplegia, but required intubation/tracheostomy less frequently, exhibited fewer other injuries and complications, and required shorter hospitalization.
Conclusions: Men, married individuals, manual laborers, and individuals aged 31–75 years had the highest risk of TSCI. Patients with TCSCI tended to have a shorter length of hospital stay than patients with non-CSCI. More attention should be paid to the other injuries and complications of non-CSCI patients, which may increase the length of hospital stay and delay rehabilitation. Compared to patients with cervical disc herniation, the patients with fracture/dislocation tended to be younger, but prognosis was severely compromised by tetraplegia, a greater need for intubation/tracheostomy, additional injuries, and complications.
Introduction
Central nervous system trauma can cause varying degrees of sensory and motor dysfunction, which seriously affect quality of life and increase the economic burden on the family and society. Traumatic brain injury is common but can occasionally be prevented by wearing a safety helmet to reduce injuries. However, traumatic spinal cord injury (TSCI) sometimes occurs in the absence of effective preventive measures. The life expectancy of spinal cord injury (SCI) patients in the USA has not improved in the past three decades; the overall age-standardized mortality rate from 2010 to 2017 was threefold greater for individuals with SCI than for members of the general population (1). Compared with the 2008 TSCI population profile, Americans living with TSCI during 2015–2019 (mean years since injury: 18 years, 79.4% men, and 62.5% Caucasian) were older (51.6 vs. 45.0 years) and had a higher percentage of C1–C4 (21.9% vs. 17.0%) and American Spinal Injury Association (ASIA) D injuries (31.5% vs. 26.0%) than did individuals in other group (2). In Korea, the mean age (standard deviation) at the time of injury increased from 32.4 (12.4) years in the 1990s to 47.1 (16.2) years in the 2010s. Land transport and falls were the most common causes of TSCI. Tetraplegia was more common than paraplegia; incomplete tetraplegia was highest in the 2010s (3).
TSCI is often caused by falls and traffic accidents, and can induce severe and irreversible dysfunction of both the motor and sensory systems, as well as tetraplegia or paraplegia, and an inability to live unassisted (4, 5). Thus, TSCI impose a major burden on individuals, families, and society, because of the high costs of treatment and rehabilitation and lost productivity (6, 7). Traumatic cervical spinal cord injury (TCSCI) can cause tetraplegia and death. In the acute stage of TCSCI, 84% of patients with C1–4 injuries and 60% with C5–8 injuries experience respiratory complications (8). Timely intubation and tracheostomy are essential (9, 10).
A traumatic cervical spinal fracture (TCSF) is typically caused by severe violence; if this is combined with a dislocation, the risk of CSCI is greatly increased. The mean annual incidence of TCSF is 65 cases per 100,000 hospital admissions; risk factors include an age of 31–45 years, male sex, fall from a height, and traumatic [C5, C6] vertebral fractures (11). The intervertebral discs separate the vertebral bodies and evenly spread the loads among them. These discs degenerate with age and become more susceptible to injury (12). TCSF/dislocation has received a great deal of attention worldwide (13–15). However, cervical disc herniation and bulging have not been well-studied. The posterior ligamentous complex includes the intervertebral disc, ligamentum flavum, and interspinous and nuchal ligaments; this complex plays a critical role in cervical spine stability (16, 17). This retrospective and descriptive study examined the epidemiological data of 1,806 TSCI patients who were admitted from 1 January 2012 to 31 December 2020. We also retrospectively analyzed the epidemiology of TCSCI and non-CSCI, and compared the clinical characteristics of patients with TCSCI caused by cervical fracture/dislocation and disc herniation/bulging.
Patients and methods
Two researchers separately reviewed the data of all hospitalized patients diagnosed with SCI. Detailed information were recorded, including gender, marital status, occupation, age, neurological level of injury, etiology, American Spinal Injury Association (ASIA) grade, combined injuries, complications, treatment, the interval between admission and surgery, intubation/tracheostomy requirement, and the length of hospital stay. The inclusion criteria were spinal cord or cauda equina injury, confirmed by clinical symptoms and an imaging examination or surgery; injury resulting from trauma; and reasonable and detailed patient records. The exclusion criteria were: non-traumatic spinal cord or cauda equina injury; treatment in departments other than orthopedics or neurosurgery; and unreasonable or incomplete patient records.
In this study, the TCSCI group included only patients with simple cervical injuries. The non-CSCI group included patients with injuries in the thoracic, lumbar, cervical and thoracic; thoracic and lumbar; cervical and lumbar; and cervical, thoracic and lumbar regions. The fracture/dislocation group included patients with at least one cervical vertebral fracture/dislocation other than disc herniation/bulging. Patients in the disc herniation/bulging group exhibited herniation/bulging of at least one cervical disc without any fracture/dislocation. SPSS software version 25.0 and GraphPad Prism software version 8.0 were used for the data analysis. The data are presented as numbers, percentages and medians with interquartile range (IQR). The Mann-Whitney U test and chi-squared (χ2) test were used to compare the two groups; the level of statistical significance was set to p < 0.05.
Results
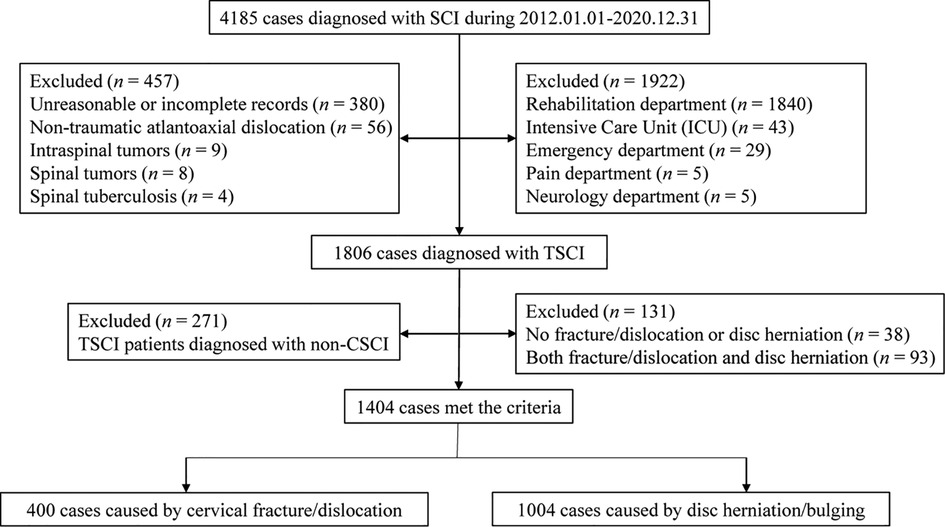
The flow chart for patient selection is displayed in Figure 1. In total, 4,185 patients were diagnosed with SCI; of these, 1,806 were diagnosed with TSCI, 2,379 were excluded for some reasons. 1,922 cases were excluded because they involved treatment in departments other than orthopedics or neurosurgery. 380 were excluded because of unreasonable or incomplete medical records. 77 cases were excluded because of non-traumatic factors.
Gender and age
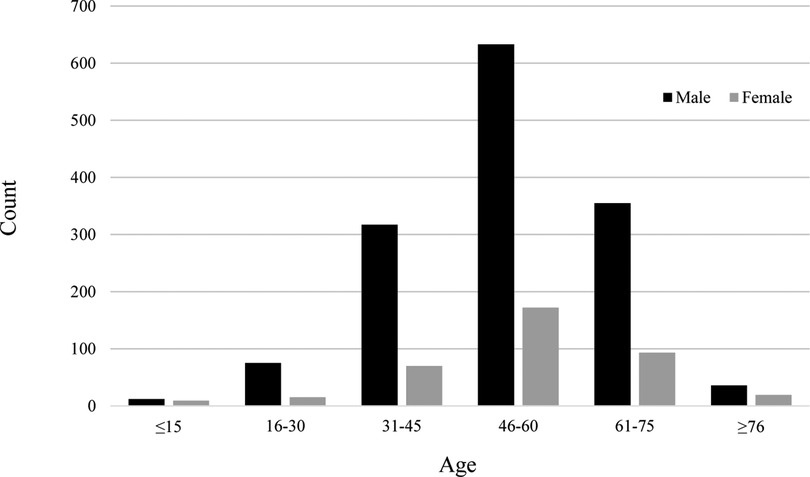
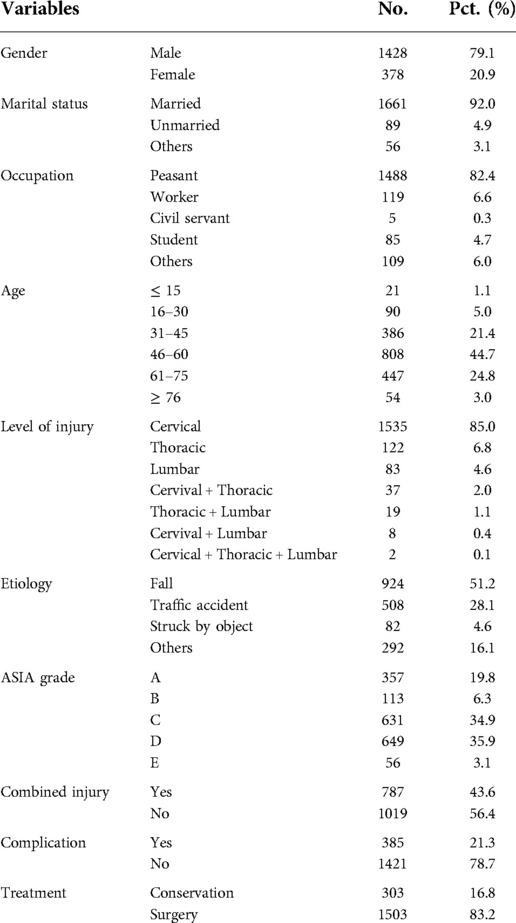
The ratio of men to women was 3.8:1. The patients were divided into six age groups: ≤ 15, 16–30, 31–45, 46–60, 61–75, and ≥ 76 years. The median age (IQR) of the 1,806 patients was 53 (IQR = 45–61) years [men: 53 (IQR = 44–61), women: 53 years (IQR = 46–62)]. The three age groups with the largest numbers of patients were 46–60, 61–75, and 31–45 years (Table 1). Patients in these groups constituted 90.9% of all included patients. The high-risk age group was similar for men and women (Figure 2). The 46–60 years age group was the largest, followed by the 61–75 years and 31–45 years age groups.
Marital Status, occupation, and etiology
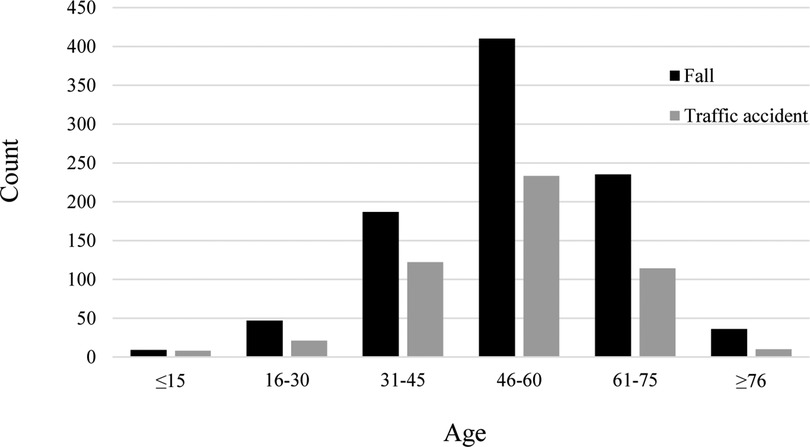
As shown in Table 1, 92.0% of patients were married. Manual laborers (peasant and worker, 89.0%) were the main group of TSCI patients. Falls (51.2%) and traffic accidents (28.1%) were the two most common causes of TSCI. Patients with impact-related injuries included 72 who were struck by objects falling from a high altitude, 6 who received lateral impacts because of operating errors during work, and 4 who received cattle impacts. Other patients experienced knife wounds (n = 5), fighting injuries (n = 7), and unclassified trauma (n = 280). The high-risk age group experienced similar rates of the two most common causes (Figure 3). The data had a unimodal distribution and both peaks were in the 46–60 years age group.
Level of injury and ASIA grade
The SCI segment was determined on the basis of clinical symptoms, computed tomography and magnetic resonance imaging findings, or postoperative records. The cervical spinal cord was more often injured than the thoracic or lumbar segments, with a total operation rate of 73.4% (1227/1740). Few cases were encountered involving combined (i.e., simultaneous) injuries of two or three segments, but their operation rate was higher (93.9%; 62/66). ASIA grades D and C constituted 70.8% of the total cases (Table 1).
Combined injuries, complications and treatment
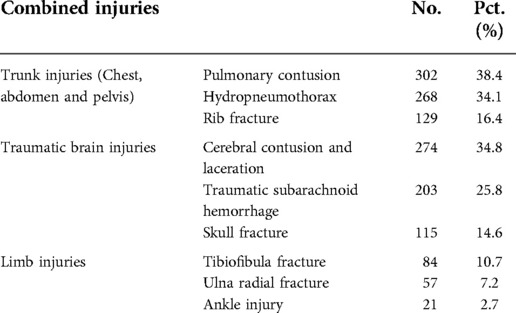
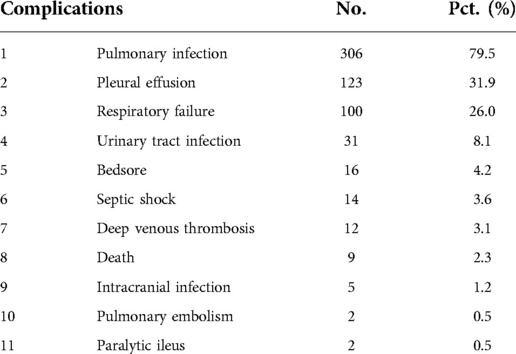
Approximately 44% of the TSCI patients had at least one combined injury upon admission to the hospital (Table 1). As shown in Table 2, the percentage of trunk injuries was higher than the percentages of traumatic brain injury or limb injuries. Pulmonary contusion, hydropneumothorax, and rib fracture were the three most common trunk injuries. The most common traumatic brain injury was a cerebral contusion and laceration, while tibiofibular fracture was the most common limb injury. In total, 21.3% of patients had at least one complication during their hospitalization (Table 1). The percentage of complications is shown in Table 3. The three most common complications were pulmonary infection, pleural effusion, and respiratory failure. Among the 1,806 TSCI patients treated in our hospital, the operation rate was 83.2% (Table 1). In total, 303 patients were not treated because they discontinued treatment (n = 156), were transferred to a specialized rehabilitation department or hospital (n = 142), or were transferred to another large hospital (n = 5).
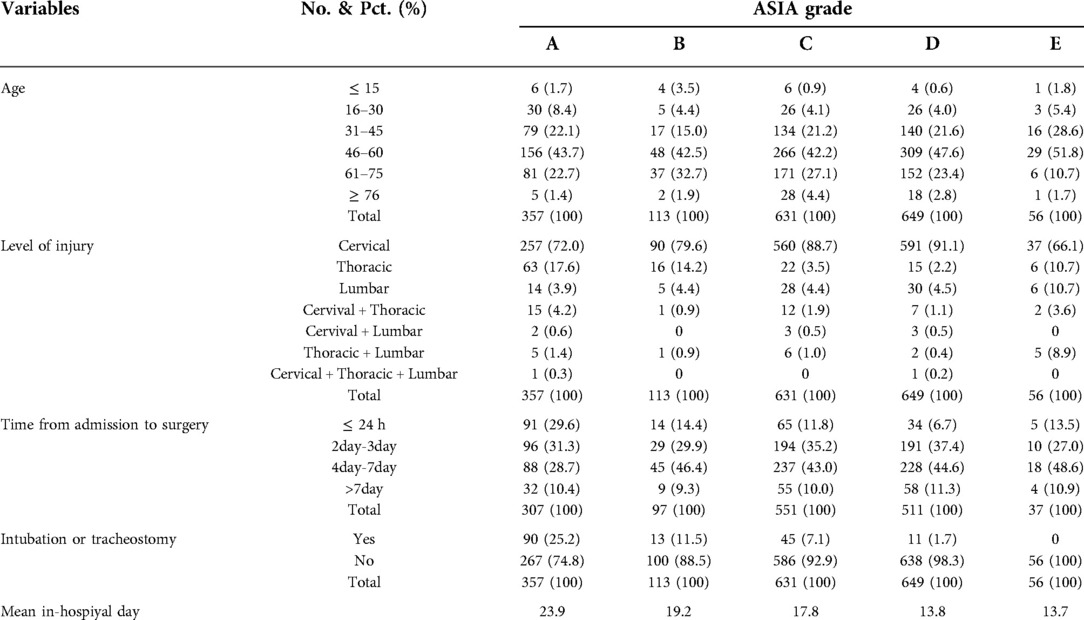
Characteristics of the 1,806 patients with different ASIA grades
As shown in Table 4, the 46–60 years age group had the greatest proportion of different ASIA grades. CSCI was much more frequent than SCI involving other segments. The proportion of patients who underwent surgery within 24 h after admission was low; most patients underwent surgery within 4–7 days after admission. Nearly 90% of patients in each grade underwent surgery within 7 days of admission. The artificial airway management status and the mean in-hospital stay findings were consistent with injury severity. Patients with a worse ASIA grade were more likely to receive tracheostomy or intubation and have a longer mean in-hospital stay.
Characteristics of TSCI and TCSCI
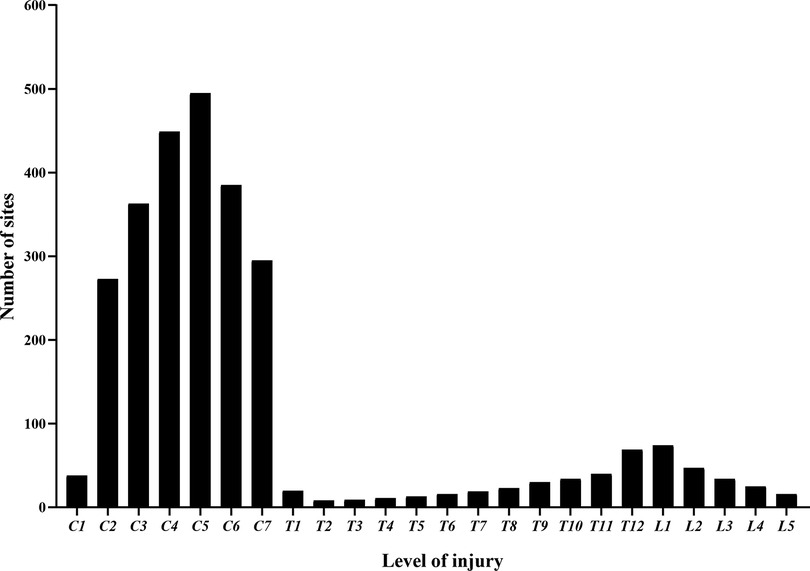
Figure 1 shows that 1,806 patients were diagnosed with TSCI, some of whom had multi-segment or multi-site injuries (Figure 4). All injury sites were detected via computed tomography (CT) or magnetic resonance imaging (MRI), or postoperatively; and the most common injuries were CSCI (Figure 5). There were 1,535 patients in the TCSCI group and 271 in the non-CSCI group. We focused on 400 TCSCI patients (526 sites of injury) who suffered cervical fracture/dislocation and 1,004 patients (1,537 sites of injury) with cervical disc herniation/bulging (Figure 6).
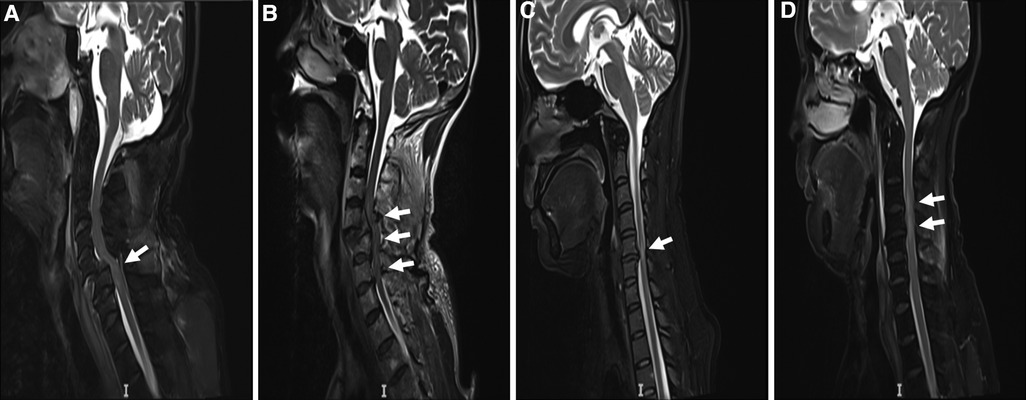
Figure 4. Two typical MRI scans of TCSCI patients. MRI scans of TCSCI patients with fracture/dislocation and disc herniation/bulging. (A) The C5 vertebral body slipped forward to the III° position; the spinal canal was narrowed and the cervical spinal cord was severely compressed. (B) The C4 vertebral body slipped forward to the II° position and a TCSCI is evident at the C4 -6 level. (C) The C5/6 intervertebral disc herniated backward and a TCSCI is apparent at the C5/6 level, especially C5. (D) The C3/4, C4/5, C5/6, and C6/7 intervertebral discs herniated posteriorly and a TCSCI is apparent at the C3/C4 level.
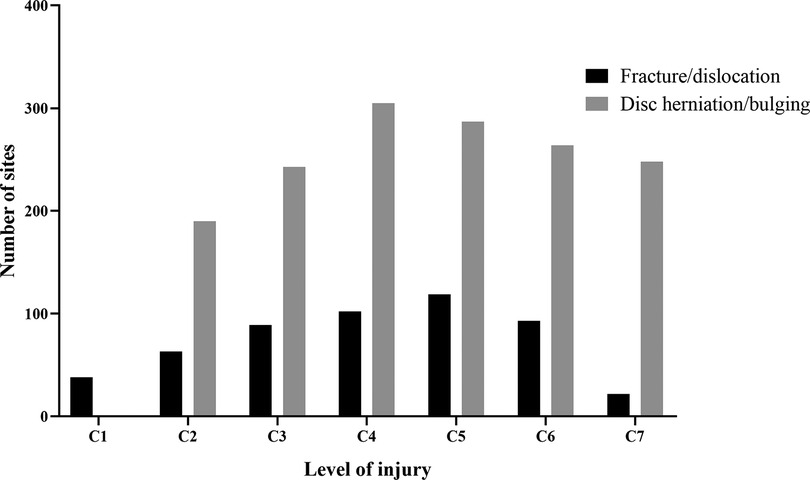
Figure 6. Distributions of all sites of injury (C1–C7) caused by fracture/dislocation and disc herniation/bulging.
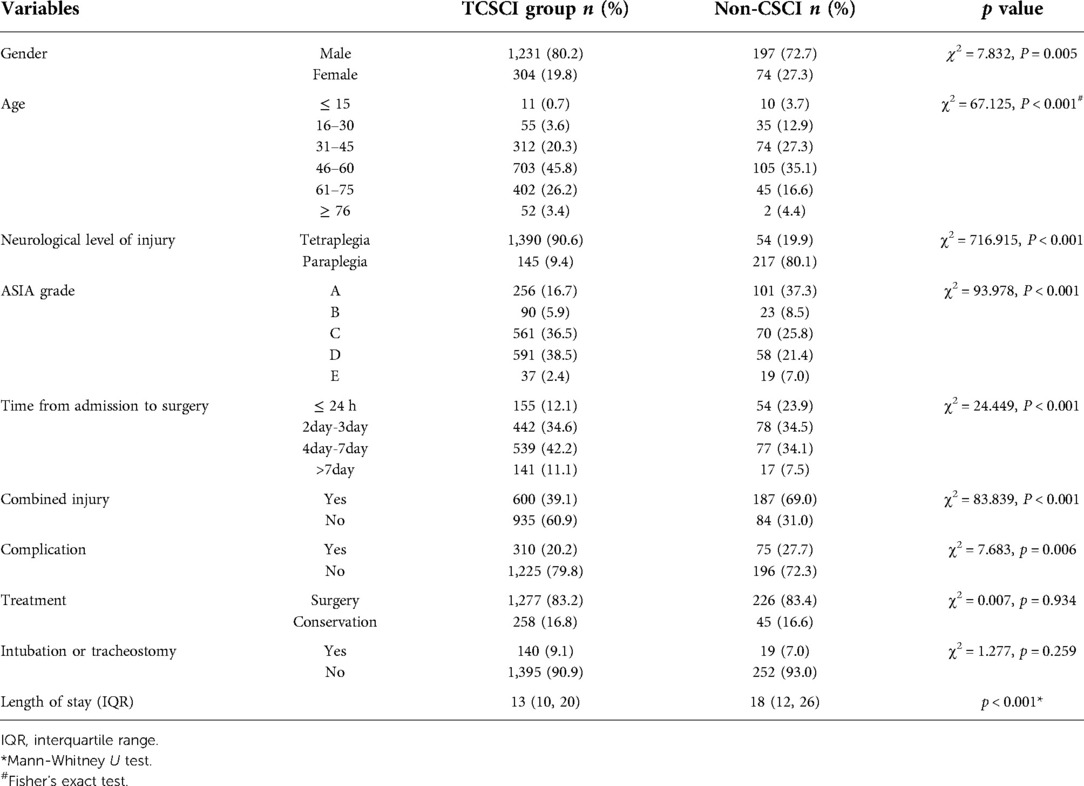
Characteristics of the 1,806 patients with TCSCI and non-CSCI
Table 5 compares the medical characteristics of the 1,535 TCSCI patients to those of the 271 non-CSCI patients. In the TCSCI group, the male: female ratio was 4.0:1, the age group with the highest risk was the 46–60 years group (followed by the 61–75 and 31–45 years groups), the tetraplegia rate was 90.6% and most patients were of ASIA grade D or C (in that order). In the non-CSCI group, the male: female ratio was 2.7:1, the age group with the highest risk was the 46–60 years group (followed by the 31–45 and 61–75 years groups), the paraplegia rate was 80.1% and most patients were of ASIA grade A or C (in that order). Patients with TCSCI (median age, 54 years; IQR = 46–62 years) tended to be older than those with non-CSCI (median age, 48 years; IQR = 37–57 years) (p < 0.001). Significant differences between the TCSCI and non-CSCI patients were seen for gender, age, neurological injury level, ASIA grade, interval between admission and surgery, other injuries, complications, and the length of hospital stay, but not in treatment or the intubation/tracheostomy requirement.
Characteristics of the 1,404 patients with cervical fracture/dislocation and disc herniation/bulging
Table 6 summarizes the medical characteristics of the 1,404 TCSCI patients with cervical fracture/dislocation and disc herniation/bulging. In the cervical fracture/dislocation group, the male: female ratio was higher than in the other group (5.5:1 vs. 3.5:1). Patients with cervical disc herniation/bulging were older (median age, 54 years; IQR = 47–62.75 years) compared to the other patients (median age, 51 years; IQR = 42.25–61 years) (p < 0.001). In the fracture/dislocation group, the rate of tetraplegia was higher than in the other group (93.5% vs. 89.2%) and most patients were of ASIA grade C. In the disc herniation/bulging group, the rate of paraplegia was higher than in the other group (10.8% vs. 6.5%) and most patients were of ASIA grade D. With the exception of treatment, there were significant group differences in all other parameters.
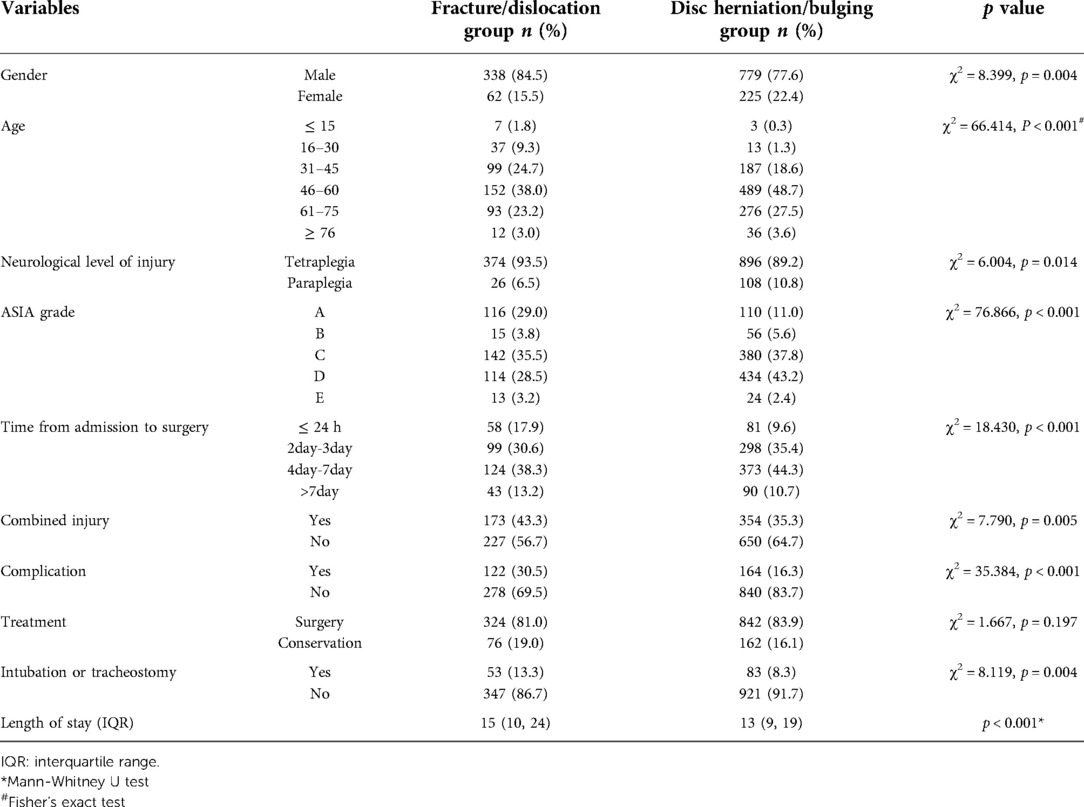
Table 6. Characteristics of 1,404 patients caused by fracture/dislocation and disc herniation/bulging.
Discussion
After careful selection, we identified 1,806 cases; the ratio of men to women in this study was 3.8:1, which was similar to the ratios in several previous studies in China (18–22). In other regions, the male: female ratios have been 2.4:1 in Russia, 2.6:1 in Finland, 3.0:1 in Japan, 3.6:1 in Mexico, 6.1:1 in India, and 7.3:1 in Saudi Arabia (23–28). China is the largest developing country in the world. The agricultural population of China has an absolute numerical advantage. Middle-aged and elderly people are always the “backbone of the family”; they engage in manual labor. In this study, married individuals, manual laborers, and individuals aged 31–75 years (especially 46–60 years) had the highest risk of TSCI. A previous comparative study indicated that TSCI caused by low and high falls has distinct epidemiological characteristics (29). In our study, some medical records were marked “fall” without a specific height or marked “traffic accident” without a specific vehicle type; they could not be further stratified into other subtypes. However, the results were consistent with previous findings; fall and traffic accidents were the two most common causes of TSCI (11, 18, 20, 22, 30–32).
CSCI is recognized as the most frequent type of TSCI. In this study, we examined the types and occurrence of combined injuries and complications to provide more clinically useful insights. Although surgical decompression should be performed as soon as possible (with the ideal surgical timing of 8 h post-injury) for both complete and incomplete lesions), many patients in this study underwent surgery within 4–7 days after admission (33–35). Possible reasons for such delay were as follows. First, many patients needed to maintain their physical status and stabilize their condition to reduce the risk of death after hospital admission. Second, imaging examinations and preoperative examinations (i.e., magnetic resonance imaging) could not be performed immediately. Third, specialists explained the need for surgery, but the family members required several days of consideration prior to consent for surgery. Our results also indicate that patients with a worse ASIA grade were more likely to undergo airway management with a longer mean in-hospital stay.
To the best of our knowledge, this is the first study to classify and compare the clinical characteristics of patients with TCSCI caused by fracture/dislocation and disc herniation/bulging. We first compared the clinical features of TCSCI and non-CSCI patients. The treatments and intubation/tracheostomy requirements did not differ between the two groups. A comparison of two subgroups of TCSCI patients indicated that those with fracture/dislocation were more likely to require intubation/tracheostomy. Treatment did not show a group difference, perhaps because all patients underwent careful initial evaluation followed by surgery if necessary.
A study conducted in Chongqing (China) reviewed 643 patients with TCSI; the mean age was 42.5 ± 13.8 years (range: 18–86 years), the male: female ratio was 4.3:1 and the most common site of injury was C5 (22.7% of cases) (11). A study conducted in Maryland (USA) evaluated 1,420 patients with TCSCI; 78.3% were male, with a mean age of 51.5 years. Complete TCSCI were noted in 29.6% of cases, and fracture dislocations were apparent in 44.7% (36). The incidence of traumatic disc herniation was 32% (37). In the present study, we screened more TCSCI patients with cervical disc herniations than fractures [71.5% (1,004/1,404) vs. 28.5% (400/1,404)]. The former patients were older (median age, 54 years; IQR = 47–62.75 years vs. 51 years; IQR = 42.25–61 years), as reflected in the higher proportion of patients aged 46–60 years (48.7% vs. 38.0%), and accounted for 71.5% (1,004/1,404) of all TCSCI cases. In general, the injuries were not as serious as those of patients with traumatic cervical fracture/dislocation. Thus, the rates of tetraplegia and operation within 24 h were lower in the former group, as were the intubation/tracheostomy rates and those of other injuries and complications. This may explain the short hospitalization period. These patients are quickly transferred for rehabilitation. Shorter hospitalization and rapid rehabilitation reduce the incidence of complications. Thus, in daily practice, patients with severe cervical fracture/dislocation require particular attention in terms of active treatment, including of other injuries, and prevention of complications. For patients with TCSCI caused by cervical disc herniation/bulging, early surgery, recovery, and rehabilitation are possible.
Notably, this study did not include data regarding TSCI patients from other affiliated hospitals or large grade A tertiary hospitals in Jiangxi Province. We only examined the epidemiological characteristics of some TSCI patients; thus, these findings are limited to the current status of diagnosis and treatment of TSCI patients in our hospital.
Data availability statement
All data generated or analysed are included in this article and are available from the corresponding author on reasonable request.
Ethics statement
Hospitalization information of TSCI patients was considered exempt by the Human Investigation Ethical Committee of the first affiliated hospital of Nanchang University.
Author contributions
ZW: study design and concept; data collection, analysis and visualization; article writing and revising. WZ: data collection, analysis and visualization; article revising and reviewing. ML: study design and concept; article reviewing. All authors contributed to the article and approved the submitted version.
Acknowledgments
This work was funded by the National Natural Science Foundation of China (NSFC; No. 81860225) and the key research and development plan of Jiangxi Province (No. 20203BBG73060).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SCI, spinal cord injury; TSCI, traumatic spinal cord injury; TCSCI, traumatic cervical spinal cord injury; CSCI, cervical spinal cord injury; ASIA, American Spinal Injury Association; TCSF, traumatic cervical spinal fracture; IQR, interquartile range; CT, computed tomography; MRI, magnetic resonance imaging.
References
1. DeVivo MJ, Chen Y, Wen H. Cause of death trends among persons with spinal cord injury in the United States: 1960–2017. Arch Phys Med Rehabil. (2022) 103(4):634–41. doi: 10.1016/j.apmr.2021.09.019
2. Chen Y, Wen H, Baidwan NK, DeVivo MJ. Demographic and health profiles of people living with traumatic spinal cord injury in the United States during 2015–2019: findings from the spinal cord injury model systems database. Arch Phys Med Rehabil. (2022) 103(4):622–33. doi: 10.1016/j.apmr.2021.11.001
3. Lee BS, Kim O, Ham D. Epidemiological changes in traumatic spinal cord injuries for the last 30 years (1990–2019) in South Korea. Spinal Cord. (2022) 60(7):612–7. doi: 10.1038/s41393-021-00694-6
4. Yorke AM, Littleton S, Alsalaheen BA. Concussion attitudes and beliefs, knowledge, and clinical practice: survey of physical therapists. Phys Ther. (2016) 96(7):1018–28. doi: 10.2522/ptj.20140598
5. Yokota K, Kubota K, Kobayakawa K, Saito T, Hara M, Kijima K, et al. Pathological changes of distal motor neurons after complete spinal cord injury. Mol Brain. (2019) 12(1):4. doi: 10.1186/s13041-018-0422-3
6. Pickelsimer E, Shiroma EJ, Wilson DA. Statewide investigation of medically attended adverse health conditions of persons with spinal cord injury. J Spinal Cord Med. (2010) 33(3):221–31. doi: 10.1080/10790268.2010.11689699
7. Baaj AA, Uribe JS, Nichols TA, Theodore N, Crawford NR, Sonntag VK, et al. Health care burden of cervical spine fractures in the United States: analysis of a nationwide database over a 10-year period. J Neurosurg Spine. (2010) 13(1):61–6. doi: 10.3171/2010.3.SPINE09530
8. Berney S, Bragge P, Granger C, Opdam H, Denehy L. The acute respiratory management of cervical spinal cord injury in the first 6 weeks after injury: a systematic review. Spinal Cord. (2011) 49(1):17–29. doi: 10.1038/sc.2010.39
9. Hou YF, Lv Y, Zhou F, Tian Y, Ji HQ, Zhang ZS, et al. Development and validation of a risk prediction model for tracheostomy in acute traumatic cervical spinal cord injury patients. Eur Spine J. (2015) 24(5):975–84. doi: 10.1007/s00586-014-3731-y
10. Flanagan CD, Childs BR, Moore TA, Vallier HA. Early tracheostomy in patients with traumatic cervical spinal cord injury appears safe and may improve outcomes. Spine (Phila Pa 1976). (2018) 43(16):1110–6. doi: 10.1097/BRS.0000000000002537
11. Wang H, Xiang Q, Li C, Zhou Y. Epidemiology of traumatic cervical spinal fractures and risk factors for traumatic cervical spinal cord injury in China. J Spinal Disord Tech. (2013) 26(8):E306–13. doi: 10.1097/BSD.0b013e3182886db9
12. Desmoulin GT, Pradhan V, Milner TE. Mechanical aspects of intervertebral disc injury and implications on biomechanics. Spine (Phila Pa 1976). (2020) 45(8):E457–E64. doi: 10.1097/BRS.0000000000003291
13. Leucht P, Fischer K, Muhr G, Mueller EJ. Epidemiology of traumatic spine fractures. Injury. (2009) 40(2):166–72. doi: 10.1016/j.injury.2008.06.040
14. Pirouzmand F. Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. J Neurosurg Spine. (2010) 12(2):131–40. doi: 10.3171/2009.9.SPINE0943
15. Ren C, Qin R, Wang P, Wang P. Comparison of anterior and posterior approaches for treatment of traumatic cervical dislocation combined with spinal cord injury: minimum 10-year follow-up. Sci Rep. (2020) 10(1):10346. doi: 10.1038/s41598-020-67265-2
16. Rasoulinejad P, McLachlin SD, Bailey SI, Gurr KR, Bailey CS, Dunning CE. The importance of the posterior osteoligamentous complex to subaxial cervical spine stability in relation to a unilateral facet injury. Spine J. (2012) 12(7):590–5. doi: 10.1016/j.spinee.2012.07.003
17. Nadeau M, McLachlin SD, Bailey SI, Gurr KR, Dunning CE, Bailey CS. A biomechanical assessment of soft-tissue damage in the cervical spine following a unilateral facet injury. J Bone Joint Surg Am. (2012) 94(21):e156. doi: 10.2106/JBJS.K.00694
18. Feng H, Xu H, Zhang H, Ji C, Luo D, Hao Z, et al. Epidemiological profile of 338 traumatic spinal cord injury cases in shandong province, China. Spinal Cord. (2022) 60:635–40. doi: 10.1038/s41393-021-00709-2
19. Chen J, Chen Z, Zhang K, Song D, Wang C, Xuan T. Epidemiological features of traumatic spinal cord injury in guangdong province, China. J Spinal Cord Med. (2021) 44(2):276–81. doi: 10.1080/10790268.2019.1654190
20. Wang HF, Yin ZS, Chen Y, Duan ZH, Hou S, He J. Epidemiological features of traumatic spinal cord injury in anhui province, China. Spinal Cord. (2013) 51(1):20–2. doi: 10.1038/sc.2012.92
21. Feng HY, Ning GZ, Feng SQ, Yu TQ, Zhou HX. Epidemiological profile of 239 traumatic spinal cord injury cases over a period of 12 years in Tianjin, China. J Spinal Cord Med. (2011) 34(4):388–94. doi: 10.1179/2045772311Y.0000000017
22. Liu J, Liu HW, Gao F, Li J, Li JJ. Epidemiological features of traumatic spinal cord injury in Beijing, China. J Spinal Cord Med. (2022) 45(2):214–20. doi: 10.1080/10790268.2020.1793505
23. Mirzaeva L, Gilhus NE, Lobzin S, Rekand T. Incidence of adult traumatic spinal cord injury in saint petersburg, Russia. Spinal Cord. (2019) 57(8):692–9. doi: 10.1038/s41393-019-0266-4
24. Johansson E, Luoto TM, Vainionpaa A, Kauppila AM, Kallinen M, Vaarala E, et al. Epidemiology of traumatic spinal cord injury in Finland. Spinal Cord. (2021) 59(7):761–8. doi: 10.1038/s41393-020-00575-4
25. Kudo D, Miyakoshi N, Hongo M, Kasukawa Y, Ishikawa Y, Ishikawa N, et al. An epidemiological study of traumatic spinal cord injuries in the fastest aging area in Japan. Spinal Cord. (2019) 57(6):509–15. doi: 10.1038/s41393-019-0255-7
26. Rodriguez-Meza MV, Paredes-Cruz M, Grijalva I, Rojano-Mejia D. Clinical and demographic profile of traumatic spinal cord injury: a Mexican hospital-based study. Spinal Cord. (2016) 54(4):266–9. doi: 10.1038/sc.2015.164
27. Chhabra HS, Arora M. Demographic profile of traumatic spinal cord injuries admitted at Indian spinal injuries centre with special emphasis on mode of injury: a retrospective study. Spinal Cord. (2012) 50(10):745–54. doi: 10.1038/sc.2012.45
28. Alshahri SS, Cripps RA, Lee BB, Al-Jadid MS. Traumatic spinal cord injury in Saudi Arabia: an epidemiological estimate from Riyadh. Spinal Cord. (2012) 50(12):882–4. doi: 10.1038/sc.2012.65
29. Zhang ZR, Wu Y, Wang FY, Wang WJ. Traumatic spinal cord injury caused by low falls and high falls: a comparative study. J Orthop Surg Res. (2021) 16(1):222. doi: 10.1186/s13018-021-02379-5
30. Yang R, Guo L, Huang L, Wang P, Tang Y, Ye J, et al. Epidemiological characteristics of traumatic spinal cord injury in guangdong. China. Spine (Phila Pa 1976). (2017) 42(9):E555–E61. doi: 10.1097/BRS.0000000000001896
31. Liu H, Liu J, Shen M, Yang X, Du L, Yang M, et al. The changing demographics of traumatic spinal cord injury in Beijing, China: a single-centre report of 2448 cases over 7 years. Spinal Cord. (2021) 59(3):298–305. doi: 10.1038/s41393-020-00564-7
32. Du J, Hao D, He B, Yan L, Tang Q, Zhang Z, et al. Epidemiological characteristics of traumatic spinal cord injury in Xi'an, China. Spinal Cord. (2021) 59(7):804–13. doi: 10.1038/s41393-020-00592-3
33. Sanchez JAS, Sharif S, Costa F, Rangel J, Anania CD, Zileli M. Early management of spinal cord injury: wFNS spine committee recommendations. Neurospine. (2020) 17(4):759–84. doi: 10.14245/ns.2040366.183
34. Jug M, Kejzar N, Vesel M, Al Mawed S, Dobravec M, Herman S, et al. Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma. (2015) 32(18):1385–92. doi: 10.1089/neu.2014.3767
35. Burke JF, Yue JK, Ngwenya LB, Winkler EA, Talbott JF, Pan JZ, et al. Ultra-Early (<12 hours) surgery correlates with higher rate of American spinal injury association impairment scale conversion after cervical spinal cord injury. Neurosurgery. (2019) 85(2):199–203. doi: 10.1093/neuros/nyy537
36. Aarabi B, Albrecht JS, Simard JM, Chryssikos T, Schwartzbauer G, Sansur CA, et al. Trends in demographics and markers of injury severity in traumatic cervical spinal cord injury. J Neurotrauma. (2021) 38(6):756–64. doi: 10.1089/neu.2020.7415
Keywords: traumatic spinal cord injury, cervical fracture/dislocation, cervical disc herniation/bulging, prevention, epidemiology
Citation: Wang Z, Zhou W and Li M (2023) Epidemiological characteristics of 1,806 patients with traumatic spinal cord injury: A retrospective study. Front. Surg. 9:988853. doi: 10.3389/fsurg.2022.988853
Received: 7 July 2022; Accepted: 26 October 2022;
Published: 6 January 2023.
Edited by:
Xinghuo Wu, Tongji Medical College, Huazhong University of Science and Technology, ChinaReviewed by:
Bahram Biglari, BG-Trauma Center Ludwigshafen, GermanyXiaodong Guo, Huazhong University of Science and Technology, China
© 2023 Wang, Zhou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mei-hua Li bGltZWlodWEyMDAwQHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Zhihua Wang
Zhihua Wang Wu Zhou
Wu Zhou Meihua Li
Meihua Li