- Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: Reconstruction of proximal humeral tumours after resection is still controversial. And there are few articles describing oncology patients' postoperative function after reversed tumour shoulder prosthesis reconstruction. We investigated the functional results of patients who underwent reversed tumour shoulder prosthesis, including those who did not preserve the deltoid ending point.
Patients and methods: We retrospectively evaluated 16 patients with proximal humerus tumours who had undergone reversed tumour shoulder prosthesis. All patients underwent type Malawer I proximal humeral resection surgery and standard reverse tumour shoulder arthroplasty with a modular reverse shoulder prosthesis. We sutured the severed end of the deltoid to the brachialis muscle using the artificial patch for patients who had their deltoid ending point resected. Patients are rehabilitated and followed up according to our instructions.
Result: All patients were followed up for a mean of 27.4 months (13–59), and their mean age was 45.9 years (15–74). The mean length of the humeral resection was 11.6 cm (5–15). The mean shoulder mobility was 122° (82°–180°) in forward flexion; 39° (31°–45°) in posterior extension; 102° (65°–172°) in abduction; 43° (30°–60°) in external rotation; 83° (61°–90°) in internal rotation, and a mean MSTS score of 77.9% (63.3%–93.3%). The mean DASH score was 20.8 (2.5–35.8). The mean VAS score was 0.9. For patients who had their deltoid ending point resected, the mean length of the humeral resection was 14.0 cm; the mean shoulder mobility was 109° in forward flexion; 37.8° in posterior extension; 102.0° in abduction; 38.3° in external rotation; 86.3° in internal rotation, and the mean MSTS score was 78.8%; the mean DASH score was 21.6; the mean VAS score was 1.0.
Conclusion: Patients who underwent reverse tumour shoulder arthroplasty can achieve good early postoperative function, survival rate and low complication rate. In addition, patients who had their deltoid ending point removed also obtained good function after particular reconstruction.
Introduction
The proximal humerus is the third most common site for primary bone and soft tissue tumours (1). Currently, preservation or salvage of shoulder function after surgery is still the most critical part of the treatment process for these patients. For many patients, resection of large areas of soft tissue is necessary to get negative surgical margins. Traditionally, traditional reconstruction methods have included anatomic endoprostheses, osteoarticular allografts, and allograft-prosthetic composites. Although each method preserves a portion of the shoulder joint function, the overall postoperative shoulder function was unsatisfactory for the patients, especially those with rotator cuff injuries (2). Over the past two decades, more and more surgeons have started to use reverse total shoulder arthroplasty(rTSA) to improve the function of patients after oncologic reconstruction of the proximal humerus (3). The reverse shoulder arthroplasty medializes and distalizes the centre of rotation of the shoulder, allowing the shoulder joint to complete abduction, forward flexion and external rotation through the deltoid muscle without the rotator cuff (4).
Few articles describe oncology patients’ postoperative function after reverse tumour shoulder prosthesis reconstruction. Reverse allograft-prosthetic composite reconstruction has achieved good outcomes for malignant tumours of the proximal humerus, and very few studies have begun to use modular prostheses (5, 6). But the preservation of the deltoid ending point is necessary for each method. We collected postoperative functional data from patients who underwent modular reverse tumour shoulder arthroplasty at our institution in the last five years and found that all patients achieved good postoperative function. Moreover, some patients with long humeral osteotomy lengths and without preserved deltoid ending points also achieved good function by reconstructing the deltoid.
Patients and methods
We conducted a retrospective study of all patients who underwent reverse tumour shoulder arthroplasty for benign and malignant tumours at West China Hospital between 2017 and 2022. There were 16 patients (seven males and nine females). All patients had imaging evidence of a lesion in the proximal humerus (4 metastatic carcinomas, 4 chondrosarcomas, 3 osteosarcomas, 2 Giant-cell tumours of bone, 1 malignant neurinoma, 2 benign tumours). All were evaluated preoperatively with Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) for the extent of soft tissue and bone involvement.
All patients underwent type I proximal humeral resection surgery (surgical classification system described by Malawer in 1991) and standard reverse tumour shoulder arthroplasty with a reverse shoulder prosthesis (Chunli Co, Ltd., Tongzhou, Beijing, China). The prosthesis consisted of a non-anatomical design with a hemispherical glenoid component and a con-cave matching cup on a stem fixed to the humerus (7).
All patients required partial or total removal of the rotator cuff to achieve a negative margin. The senior surgeon at our institution (C. T.) performed all the surgeries. The surgical approach was the pectoralis major deltoid approach. The affected proximal humerus was resected according to the preoperative design using vernier callipers to determine the length of the osteotomy, including en bloc of the surrounding soft tissues and muscles to achieve a negative margin. The deltoid ending point was removed in four of these patients due to extensive tumour invasion. The axillary nerve was preserved intact in all patients. Mark the long head of the pectoralis major, latissimus dorsi, and biceps brachii with sutures. And then, we implant a reverse shoulder joint prosthesis. Finally, we repair muscles marked by previous sutures to ensure the stability of the joint prosthesis. For the four patients who had their deltoid ending point removed, we sutured the severed end of the deltoid to the brachialis muscle using the artificial patch to ensure abduction muscle strength and adjusted it to the appropriate muscle tone. Postoperative antibiotics such as cefuroxime were routinely used to prevent infection for 24–48 h. A 45°–75° abduction brace was used for four weeks after surgery. Active functional exercise of the hand, wrist and elbow and small passive movements of the shoulder joint was started the day after surgery. Patients with reconstructed deltoid need to start abduction activity 6 weeks after surgery and other patients from postoperative day 2–7 according to the instructions of the senior surgeon. The brace was removed one month after surgery.
Patients were followed up at the second week, the first month, the third month, the sixth month, the first year, and every year after surgery. Follow-up included physical examination, x-rays, CT, shoulder mobility, and functional assessment of the shoulder. Shoulder function was assessed using Musculoskeletal Tumor Society(MSTS) scores (8) and Disabilities of the Arm, Shoulder and Hand (DASH) score (9). We used the Visual Analog Scale (VAS) score (10) for the pain to assess patients' pain. The first author measured shoulder mobility using a protractor on a photograph of the patient (Figures 1, 2). Additional information on the patient's age, gender, tumour pathology type, complications, length and extent of resection, and whether to remove the deltoid ending point were tallied according to the patient's inpatient medical record.
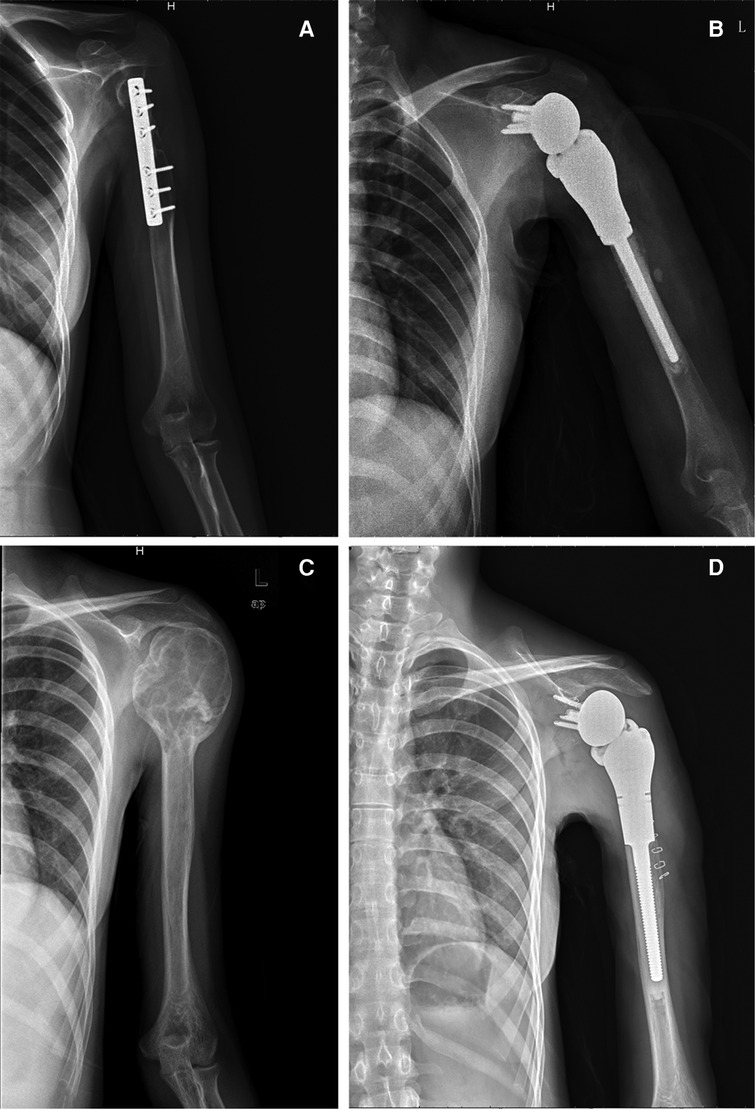
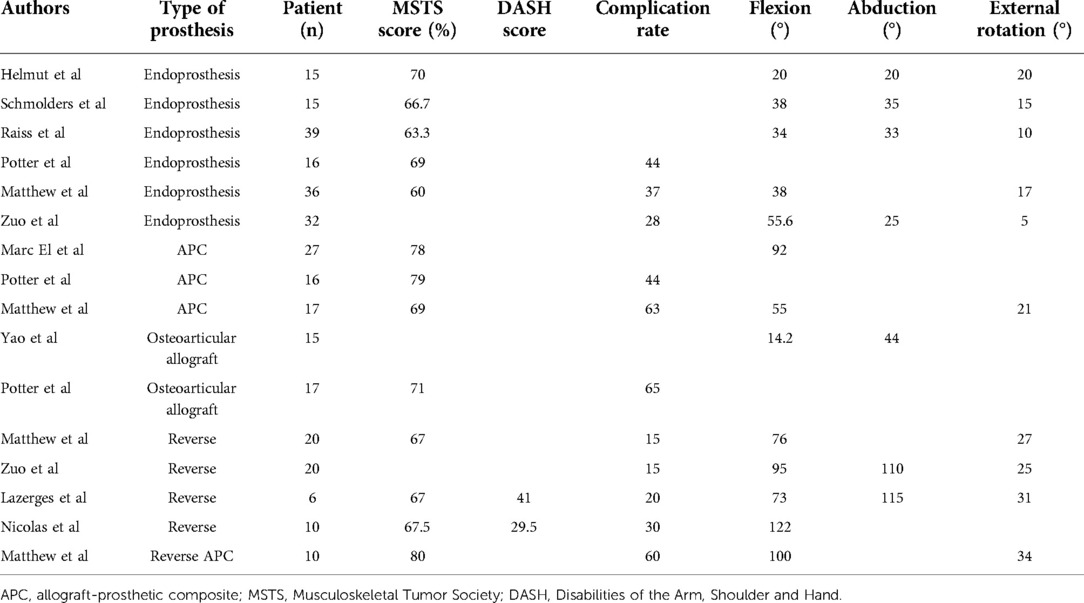
Figure 1. Imaging of two typical patients. (A) Preoperative x-ray of typical patient 1. (B) Postoperative x-ray of typical patient 1. (C) Preoperative x-ray of typical patient 2. (D) Postoperative x-ray of typical patient 2.

Figure 2. Postoperative functional photographs of two typical patients. (A) Postoperative functional photograph of typical patient 1. (B) Postoperative functional photograph of typical patient 2.
Result
Two of the 16 patients with metastatic cancer (1 male, 1 female) died 14 and 21 months after surgery, and both patients were followed up to the time of death. All patients (7 male, 9 female) were followed up for a mean of 27.4 months (13–59), and their mean age was 45.9 years (15–74). The pathological type of the tumour is shown in Table 1. The length of the humeral resection ranged from 5–15 cm, with a mean of 11.6 cm.

Table 1. The data of all patients who underwent reverse tumour shoulder arthroplasty at West China Hospital between 2017 and 2022.
The mean shoulder mobility at the last follow-up was 122° (82°–180°) in forward flexion; 39° (31°–45°) in posterior extension; 102° (65°–172°) in abduction; 43° (30°–60°) in external rotation; 83° (61°–90°) in internal rotation, and a mean MSTS score of 77.9% (63.3%–93.3%). The factor with the highest MSTS score was manual dexterity; the lowest was upper extremity weight-bearing capacity, which was significantly reduced in all patients.
The mean DASH score was 20.8 (2.5–35.8). The lowest scoring item was opening bottle caps, which all patients could do independently. The highest scoring item was lifting heavy objects over 5 kg, which is difficult for patients after shoulder arthroplasty.
The mean VAS score was 0.9. Eight patients did not have any pain and had a score of 0. The rest of the patients scored 1 or 2. Only one patient with a severed axillary nerve presented had pronounced pain. This patient's pain occurred mainly during activity; the VAS score was 4. The patient was also the most recent (13 months) to the last follow-up. The pain symptoms may resolve with a longer recovery time and rehabilitation training.
We counted the mean data from four patients with deltoid ending point removed. The mean length of the humeral resection was 14.0 cm. The mean shoulder mobility was 109° in forward flexion; 37.8° in posterior extension; 102.0° in abduction; 38.3° in external rotation; 86.3° in internal rotation, and the mean MSTS score was 78.8%; the mean DASH score was 21.6; the mean VAS score was 1.0.
As of the last follow-up, no patient had developed complications. Except for one patient with metastatic cancer with a lumbar metastasis, all patients had no distant metastasis of the tumour at follow-up. No patient had prosthesis loosening or periprosthetic fracture.
Discussion
Tumours of the proximal humerus are the third most common bone tumour and the most common bone tumour of the upper extremity. Limb-preserving surgery for tumours of the proximal humeral has yielded good oncologic results (4, 11, 12). Since almost all tumour resections of the proximal humerus require resection of the rotator cuff insertions, although there are many types of shoulder reconstruction, the patient's postoperative upper extremity function, especially shoulder mobility, was poor after either surgery (Table 2) (13–18). Some investigators used reverse shoulder arthroplasty and allograft-prosthetic composite reverse shoulder arthroplasty to improve the function of the patients and achieved good results (Table 2) (5, 6, 19–21).
Complications of shoulder replacement include shoulder instability, infection, nerve palsy, implant loosening, prosthesis dislocation, periprosthetic fracture, and for Allograft-Prosthetic Composite Reconstruction, nonunion and allograft fracture (4, 22–24). For rTSA, the most common complication is shoulder instability. The tendency to postoperative shoulder instability is also the biggest shortcoming of reverse tumour shoulder arthroplasty. Reconstructing as much muscle around the prosthesis as possible can somewhat prevent shoulder instability (4). Allograft-Prosthetic Composite Reconstruction can address the problem of easy loosening of the prosthesis after surgery because the composite prosthesis helps the bone grow. However, at the same time, the rate of postoperative complications is significantly higher because of the risk of nonunion, allograft fracture and bone resorption (16, 25). So, for Reverse Allograft-Prosthetic Composite Reconstruction, nonunion was the most common complication (24). The average rate of postoperative complications after traditional and reverse shoulder arthroplasty by other authors in Table 2 was 46.8% and 20%. As of the last follow-up, our patient had no significant complications. However, our mean follow-up time was too short, and a long follow-up observation is needed because some researchers have noted that the longer the postoperative period, the greater the probability of prosthetic loosening occurring (16).
Few articles describe reverse tumour shoulder arthroplasty's function after proximal humeral tumour resection. Furthermore, each article included a few patients. The rating scale used to assess patients' limb function was also inconsistent. Therefore, it is not easy to perform a large-scale statistical analysis. However, compiling and comparing the function of traditional surgical approaches (anatomic endoprostheses, osteoarticular allografts, and allograft-prosthetic composites) with that of reverse shoulder arthroplasty in different articles also revealed significant differences (1, 5, 13–21). For the traditional surgical approach and the reverse shoulder replacement, mean MSTS scores were 69.5% and 69.7%; mean complication rates were 46.8° and 28°; mean anterior flexion angles were 50.9° and 93.2°; mean abduction angles were 34.5° and 112.5°, and mean external rotation angles were 14.3° and 29.2°. The reverse shoulder arthroplasty was significantly superior to the conventional surgical approach regarding complications and joint mobility.
The 16 patients who underwent modular reverse tumour shoulder arthroplasty at our centre also had a good function. Except for two patients with metastatic cancer who died, all 14 patients could function adequately in daily life. All remaining patients did not experience severe pain, with eight patients experiencing no pain symptoms. The mean MSTS score of our patients is higher than the mean scores in other reverse shoulder replacement articles (Table 2). Our centre used the Disabilities of the Arm, Shoulder and Hand (DASH) score to assess patient function, and the score is lower than others' articles that also used the DASH score to assess the function of patients undergoing reverse shoulder arthroplasty at their institutions.
The conventional theory is that if the deltoid ending point cannot be preserved, the patient is not a candidate for reverse shoulder arthroplasty. We separately counted the postoperative function of patients who had their deltoid ending point removed. The results showed that these patients also achieved good postoperative function by reconstructing the adductor muscle by suturing the deltoid dissection to the brachialis muscle. This may suggest expanding the surgical indications for reversed tumour shoulder prosthesis. In addition, whether the deltoid stop is preserved or not, preservation of the deltoid muscle is critical for postoperative function in patients undergoing reverse tumour shoulder arthroplasty because patients with more deltoid muscle sacrifice generally had a poorer postoperative function. The study of Lazerges et al. included patients with more deltoid muscle sacrifice, and the mean DASH score was 41 (5, 21).
In patients with proximal humeral tumours, reverse tumour shoulder arthroplasty can achieve better postoperative function and lower postoperative complication rates than traditional shoulder arthroplasty, and both can achieve the same oncologic outcomes and patient satisfaction (26). Therefore, except for patients whose axillary nerve cannot be preserved and whose survival time is expected to be short, reverse tumour shoulder arthroplasty can be an excellent reconstructive modality after proximal humeral tumor resection. Moreover, patients with negative margins beyond the deltoid ending point may achieve good postoperative function with a particular deltoid ending point reconstruction.
Our study also has some limitations. The first is the short follow-up period. We should perform a long-term follow-up to obtain data on long-term postoperative function, complication rates, and other data. Secondly, the sample size was small and more patients undergoing reverse tumour shoulder arthroplasty should be included in the future to obtain more reliable data.
Conclusion
The choice of reconstruction modality after tumor resection of the proximal humerus has been controversial. From the current follow-up results in our centre, patients who underwent reverse tumour shoulder arthroplasty can achieve good early postoperative function, survival rate and low complication rate. In addition, patients who had their deltoid ending point removed also obtained good function after particular reconstruction. Therefore, reverse tumour shoulder arthroplasty can be an option for shoulder reconstruction after resectioning the proximal humeral tumour. However, longer follow-up and larger sample sizes are also needed to obtain more reliable data.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
This study was approved by the West China Hospital's ethics committee, Sichuan University (Chengdu, People's Republic of China), and was permitted to be published. Written informed consent to have the case details and accompanying images published was obtained from the patient's parents.
Author contributions
SW, YL, YZ and CT were involved with the concept and design of this manuscript. SW, YZ, YW and TG were involved with the acquisition of subjects and data. YL, YZ, and CT were involved in the design and implementation of surgery. SW and CT were involved in the post-surgical evaluation of the patient. SW, YL, YZ, and CT were involved with the writing and revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18036).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mankin HJ. Musculoskeletal tumor surgery. J Bone Joint Surg. (1983) 65:1361. doi: 10.2106/00004623-198365090-00031
2. Teunis T, Nota SPFT, Hornicek FJ, Schwab JH, Lozano-Calderón SA. Outcome after reconstruction of the proximal humerus for tumor resection: a systematic review. Clin Orthop Relat Res. (2014) 472:2245-53. doi: 10.1007/s11999-014-3474-4
3. Flatow EL, Harrison AK. A history of reverse total shoulder arthroplasty. Clin Orthop Relat Res. (2011) 469:2432-9. doi: 10.1007/s11999-010-1733-6
4. Ferlauto HR, Wickman JR, Lazarides AL, Hendren S, Visgauss JD, Brigman BE, et al. Reverse total shoulder arthroplasty for oncologic reconstruction of the proximal humerus: a systematic review. J Shoulder Elbow Surg. (2021) 30:e647-58. doi: 10.1016/j.jse.2021.06.004
5. Guven MF, Aslan L, Botanlioglu H, Kaynak G, Kesmezacar H, Babacan M. Functional outcome of reverse shoulder tumor prosthesis in the treatment of proximal humerus tumors. J Shoulder Elbow Surg. (2016) 25:e1-6. doi: 10.1016/j.jse.2015.06.012
6. Zuo D, Mu H, Yang Q, Sun M, Shen J, Wang H, et al. Do reverse total shoulder replacements have better clinical and functional outcomes than hemiarthroplasty for patients undergoing proximal humeral tumor resection using devitalized autograft composite reconstruction: a case-control study. J Orthop Surg Res. (2021) 16:453. doi: 10.1186/s13018-021-02488-1
7. Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. (1993) 16:65-8. doi: 10.3928/0147-7447-19930101-11
8. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. (1993) 286:241-6.
9. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. the upper extremity collaborative group (UECG). Am J Ind Med. (1996) 29:602-8. doi: 10.1002/(SICI)1097-0274(199606)29:6%3C602::AID-AJIM4%3E3.0.CO;2-L
11. De Wilde L, Boileau P, Van der Bracht H. Does reverse shoulder arthroplasty for tumors of the proximal humerus reduce impairment? Clin Orthop Relat Res. (2011) 469:2489-95. doi: 10.1007/s11999-010-1758-x
12. Tsuda Y, Fujiwara T, Evans S, Kaneuchi Y, Abudu A. Extra-articular resection of shoulder joint for bone sarcomas: oncologic and limb-salvage outcomes of 32 cases compared with shoulder disarticulation and forequarter amputation. J Surg Oncol. (2020) 121:612-9. doi: 10.1002/jso.25838
13. Potter BK, Adams SC, Pitcher JD Jr, Malinin TI, Temple HT. Proximal humerus reconstructions for tumors. Clin Orthop Relat Res. (2009) 467:1035-41. doi: 10.1007/s11999-008-0531-x
14. Raiss P, Kinkel S, Sauter U, Bruckner T, Lehner B. Replacement of the proximal humerus with MUTARS tumor endoprostheses. Eur J Surg Oncol. (2010) 36:371-7. doi: 10.1016/j.ejso.2009.11.001
15. Schmolders J, Koob S, Schepers P, Kehrer M, Frey SP, Wirtz DC, et al. Silver-coated endoprosthetic replacement of the proximal humerus in case of tumour-is there an increased risk of periprosthetic infection by using a trevira tube? Int Orthop. (2017) 41:423-8. doi: 10.1007/s00264-016-3329-6
16. El Beaino M, Liu J, Lewis VO, Lin PP. Do early results of proximal humeral allograft-prosthetic composite reconstructions persist at 5-year follow-up? Clin Orthop Relat Res. (2019) 477:758-65. doi: 10.1097/CORR.0000000000000354
17. Yao W, Cai Q, Wang J, Hou J. Mid- to long-term effects of two different biological reconstruction techniques for the treatment of humerus osteosarcoma involving caput humeri. World J Surg Oncol. (2020) 18:23. doi: 10.1186/s12957-020-1797-z
18. Ahrens H, Theil C, Gosheger G, Rödl R, Deventer N, Rickert C, et al. The bateman-type soft tissue reconstruction around proximal or total humeral megaprostheses in patients with primary malignant bone tumors-functional outcome and endoprosthetic complications. Cancers (Basel). (2021) 13:3971. doi: 10.3390/cancers13163971
19. Houdek MT, Bukowski BR, Athey AG, Elhassan BT, Barlow JD, Morrey ME, et al. Comparison of reconstructive techniques following oncologic intraarticular resection of proximal humerus. J Surg Oncol. (2021) 123:133-40. doi: 10.1002/jso.26271
20. Lazerges C, Dagneaux L, Degeorge B, Tardy N, Coulet B, Chammas M. Composite reverse shoulder arthroplasty can provide good function and quality of life in cases of malignant tumour of the proximal humerus. Int Orthop. (2017) 41:2619-25. doi: 10.1007/s00264-017-3538-7
21. Bonnevialle N, Mansat P, Lebon J, Laffosse JM, Bonnevialle P. Reverse shoulder arthroplasty for malignant tumors of proximal humerus. J Shoulder Elbow Surg. (2015) 24:36-44. doi: 10.1016/j.jse.2014.04.006
22. Kamalapathy P, Shah A, Raskin K, Schwab JH, Lozano-Calderon SA. Complications and survivorship of distal humeral allograft reconstruction after tumor resection: literature review and case series. J Am Acad Orthop Surg Glob Res Rev. (2021) 5:e20 00256-00258. doi: 10.5435/JAAOSGlobal-D-20-00256
23. Ayvaz M, Cetik RM, Bakircioglu S, Tokgozoglu AM. Proximal humerus tumors: higher-than-expected risk of revision with constrained reverse shoulder arthroplasty. Clin Orthop Relat Res. (2020) 478:2585-95. doi: 10.1097/CORR.0000000000001245
24. Sanchez-Sotelo J, Wagner ER, Sim FH, Houdek MT. Allograft-Prosthetic composite reconstruction for massive proximal humeral bone loss in reverse shoulder arthroplasty. J Bone Joint Surg Am. (2017) 99:2069-76. doi: 10.2106/JBJS.16.01495
25. Boileau P, Raynier J-L, Chelli M, Gonzalez J-F, Galvin JW. Reverse shoulder-allograft prosthesis composite, with or without tendon transfer, for the treatment of severe proximal humeral bone loss. Journal of Shoulder and Elbow Surgery. (2020) 29:e401-15. doi: 10.1016/j.jse.2020.03.016
26. Trovarelli G, Cappellari A, Angelini A, Pala E, Ruggieri P. What is the survival and function of modular reverse total shoulder prostheses in patients undergoing tumor resections in whom an innervated deltoid muscle can be preserved? Clin Orthop Relat Res. (2019) 477:2495-507. doi: 10.1097/CORR.0000000000000899
Keywords: reversed tumour shoulder prosthesis, function, proximal humerus tumour, deltoid ending point reconstruction, retrospective study
Citation: Wang S, Luo Y, Wang Y, Zhang Y, Gong T, Tu C and Zhou Y (2022) Early functional and therapeutic effect of reversed tumour shoulder prosthesis reconstruction after proximal humerus tumour resection. Front. Surg. 9:987161. doi: 10.3389/fsurg.2022.987161
Received: 5 July 2022; Accepted: 29 August 2022;
Published: 23 September 2022.
Edited by:
Jianxiang Liu, Tongji Medical College, Huazhong University of Science and Technology, ChinaReviewed by:
Chuanxi Zheng, Shenzhen University, ChinaZhicai Zhang, Huazhong University of Science and Technology, China
© 2022 Wang, Luo, Wang, Zhang, Gong, Tu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chongqi Tu VHVjcUBzY3UuZWR1LmNu Yong Zhou emhvdXlvbmdna0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Shang Wang
Shang Wang Yi Luo†
Yi Luo† Chongqi Tu
Chongqi Tu Yong Zhou
Yong Zhou