
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 09 September 2022
Sec. Reconstructive and Plastic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.984732
This article is part of the Research Topic Recent Innovations in Breast Reconstructive Surgery View all 8 articles
 Yan Zheng1,2
Yan Zheng1,2 Yan-Yan Hu2
Yan-Yan Hu2 Wan-Yi Zhao2
Wan-Yi Zhao2 Xiao-Feng Wang2
Xiao-Feng Wang2 Qing-Qing Fang2
Qing-Qing Fang2 Xiong Lv1
Xiong Lv1 Chun Xiang1
Chun Xiang1 Jian-Min Yao3*
Jian-Min Yao3* Wei-Qiang Tan2*
Wei-Qiang Tan2*
Capsular contracture is one of the most common complications of breast implants, which often leads to secondary surgery. Patients with unconspicuous breast contracture do not need treatment, while for those with severe symptoms, a capsule revision surgery is of great necessity, including a total periprosthetic capsulectomy and replacement with a new implant. However, if the capsular contracture happens in the submuscular space, it will be very difficult to release it completely, and it may lead to more complications such as damage to surrounding tissue. The new method of pouch can create a new subpectoral plane for the insertion of a new implant instead of a total capsulectomy, but this method is unsuitable for patients who have little breast tissue or thin skin. To solve this thorny clinical problem, we invented a double-headed separating instrument and came up with a novel operation method to release the capsular contracture, which opened from the nipple by the punctiform-incision approach and caused only a mild and undetectable trauma. This operation went off without a hitch, and the postoperative breast shape was good, and the breast felt and moved naturally. In addition, there were no significant complications throughout the one-year follow-up period. This case was an excellent demonstration of the novel breast capsular contracture release surgery using our optimized double-headed capsule contracture separator.
The implant-based breast augmentation surgery has become a common operation in the field of plastic surgery. Millions of breast implants are surgically inserted into the body worldwide every year. But on the flip side, these implants cause a lot of unpalatable complications to patients, of which capsule contracture was reported to be the most common and severe complication found in a 25-year longitudinal study. This occurred in more than 50% of the patients with breast implants (1–3). Capsular contracture is a local complication caused by excessive fibrous reaction to the implant. When contracture occurs, the capsule becomes thick and hard, leading to pain, deformation, displacement, and sometimes rupture of the implant (4). Most of the current evidence suggests that immunological mechanisms and infection play an important role, but these mechanisms have not been fully elucidated (5–10). Factors influencing the formation of capsular contracture mainly include the incision type, the usage of antibiotics, the types of implant surfaces, and fillings (11, 12).
The Baker classification system defines capsular contracture into four classes: grade I, natural breast; grade II, minimum contracture with no patient complaints; grade III, moderate contracture with some hardness; and grade IV, severe contracture, evident on observation. Patients of grades III and IV usually need surgical treatment (13).
The standard management of symptomatic capsular contracture usually involves capsulectomy or capsulotomy. However, if contracture occurs in the submuscular space, a complete release of the contracture will be difficult, and it may cause damage to the surrounding tissues (14). For better surgical results and less unnecessary injury, we invented a new surgical procedure using a series of novel techniques to deal with capsular contracture. Here, we would like to describe in detail this surgical innovation with a case study.
The capsule-releasing devices (Figure 1A) include a pair of plastic shears, an olive-head splitter, a blunt stripper, a pair of double-headed separating rod and sleeve, and the separating rod with a pointed tip and a round tip (Figure 1B).
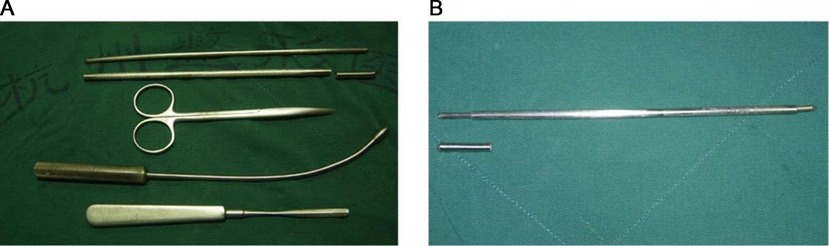
Figure 1. The capsule contraction-releasing devices. (A) All the devices. From top to bottom are a double-headed separating rod, a sleeve and cap, a straight vascular clamp, an olive-head splitter, and a blunt stripper. (B) The double-headed separating rod in the sleeve and sleeve cap.
Patients with capsular contracture, small capsular contents, and intact and usable prosthesis can be the best indications for this technique.
Exclusion criteria are as follows: (1) severe cardiopulmonary insufficiency, unable to tolerate anesthesia and corresponding surgical trauma; (2) coagulopathy and obvious bleeding tendency; (3) infection, inflammation, and burn in the surgical site or nearby tissues; (4) significantly damaged prosthesis, or the patient needs to remove the prosthesis; (5) leakage of the prosthesis into the tissue space.
This surgery was performed at Hangzhou Grammy Medical Cosmetology. The patient was a 39-year-old woman, who underwent a subpectoral breast augmentation surgery with a smooth silicone implant 10 years ago. She was suffering from grade IV capsular contracture. Hyperconvex deformity could obviously be seen on her left breast when she lied down, and the left breast felt quite hard (Figure 2A). All preoperative examinations were normal, and no obvious leakage was found after a preoperative ultrasonic examination. Written informed consent was obtained.
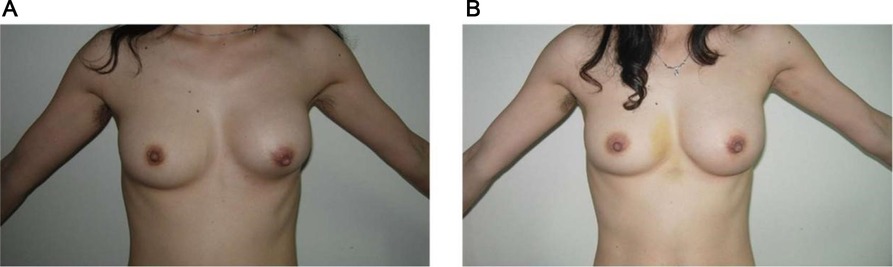
Figure 2. Comparison before and after surgery. (A) Preoperative appearance. (B) Nine days after surgery.
Topical anesthesia was induced with a tumescent solution consisting of 250 ml of normal saline, 0.5 ml of 0.1% epinephrine, and 10 ml of 2% lidocaine. This solution was injected into the nipple with capsular contracture.
Surgical procedures are shown in Figure 3. First, a punctiform incision was made in the nipple with a sharp blade, and the nipple wound was extended to the capsule by using a vascular clamp (Supplementary Figure 1A); then, blunt separation was performed using vascular clamp to break through the capsule and entering the lumen. Second, the olive-head splitter was inserted to push the implant to one side (Supplementary Figure 1B). Then, innovative tools were used in eight steps: (1) put the separation rod into the smooth sleeve, with the circular tip turning the deep direction of the breast; (2) cover the sleeve with the cap on the top of the separation rod, to control the exposure length of the separation rod, which can be adjusted accordingly; (3) insert the separator from the nipple incision, passing through the broken capsule wall and entering the capsule cavity, then penetrate along the surface of the prosthesis to the outer edge of the prosthesis. Be careful to keep the sleeve in the same position to avoid contacting the implant; (4) pull out the separator rod and change the sharp tip turning to the deep direction of the breast; (5) rotate the tip 360° with the nipple as the central point of the cone, completely scratching the contracture capsule and destroying the continuity of the hard capsule; (6) take out the separator and use the olive-head splitter and stripping ion to completely release the capsule; (7) use the splitter to push the implant for reduction; and (8) remove the capsule release device. Unfortunately, the original silicone prosthesis was found to seep during the operation, which was not detected by preoperative ultrasound examination, so we replaced it with a 200 ml textured implant through axillary incision. The leakage of the silicone implant was not caused by our surgical procedures because the removed implant was cosmetically intact with no breakage (Supplementary Figure 2). Leakage would have been caused by the poor quality of the implant itself and the long time taken since its implantation. At this point, the operation was completed.
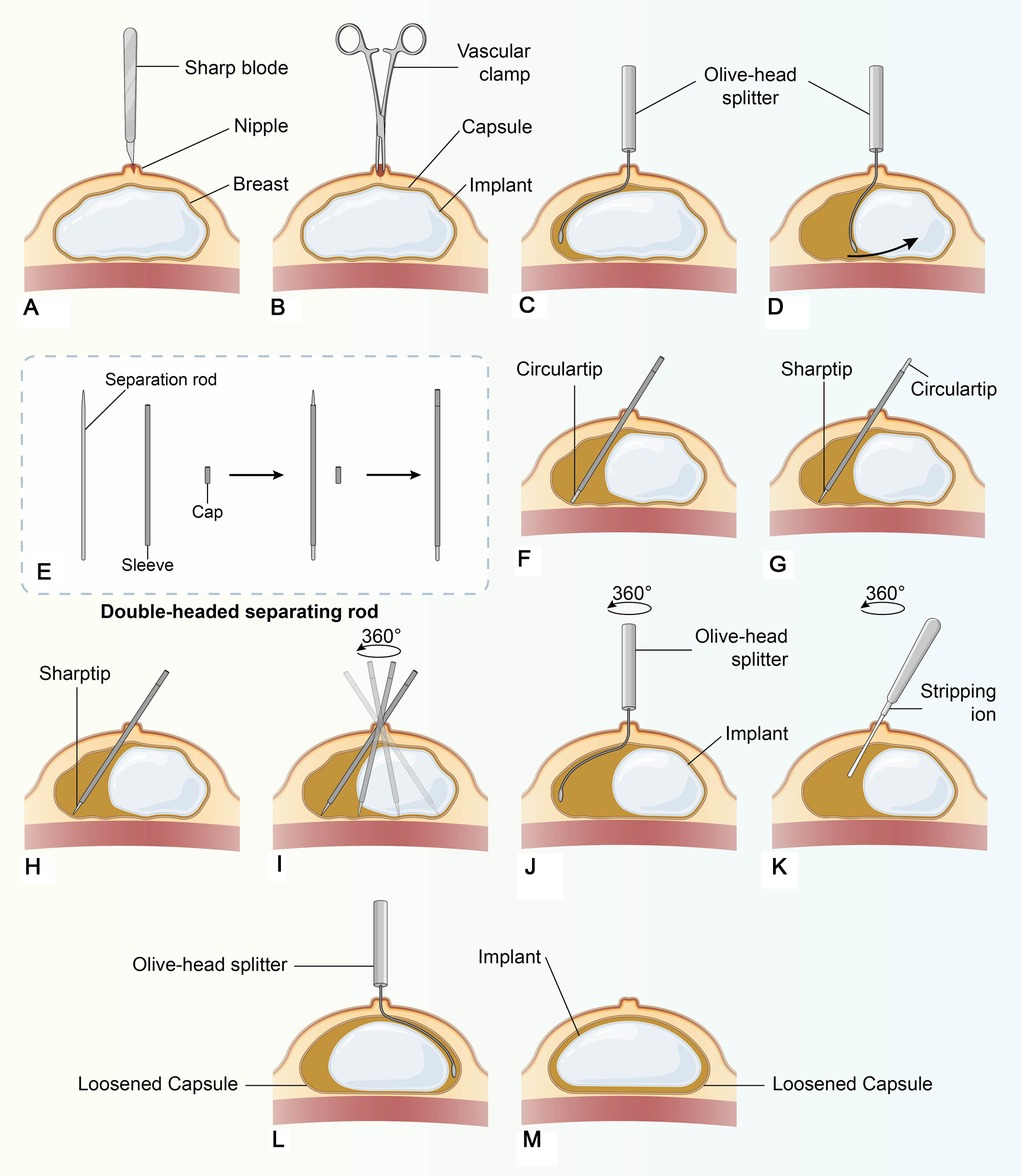
Figure 3. Operation flow chart of treatment for breast capsular contracture by the punctiform-incision approach through the nipple, as shown in the figure: A–M.
Breast shape and nipple position gradually became symmetrical since postoperative day 1 (Supplementary Figure 3A) to the ninth day (Figure 2B). The postoperative follow-up lasted for 12 months. The breast was well-shaped, and it felt and moved naturally (Supplementary Figure 3B). The patient was very satisfied with the postoperative recovery effect. No postoperative complication was reported in this case.
Breast prosthesis implantation is one of the most common procedures in plastic surgery for cosmetic or reconstructive purposes. Because the prosthesis is implanted, it will be surrounded by tissue, causing tissue rejection and local inflammation, which will eventually lead to the formation of a fibrous capsule. Therefore, patients often suffer from capsular contracture. However, there is no particularly effective treatment other than secondary surgery. Encapsulation excision, site modification, and prosthesis replacement are universally recommended. However, the thick capsule adherent to the chest is quite difficult to excise, and a thorough dissection of the capsular contracture may increase the associated risks such as excessive bleeding and even pneumothorax (15, 16). In some cases, traditional capsulectomy may not be the best solution for capsular contracture. For patients who abandon the prosthesis, the capsule will naturally recede even if it is not removed. For patients who want to keep the prosthesis, the capsule will slowly re-form as long as the prosthesis is still in place, and there is a possibility of capsular contracture occurring again. Therefore, for capsular contracture, our innovative capsule release procedure not only has a good therapeutic effect but also has a strong advantage of minimal damage.
In this article, we introduced an innovative surgery for capsular contraction using our own creative release devices. This surgery provided access to the most basal layer of the implant through the small point incision of the nipple. The sleeve device was inserted into the capsule for pointlike separation to avoid unnecessary trauma. Even if the capsule was loosened by 360°, the blood supply to the skin tissue would not be affected. The olive-head splitter could perfectly match the shape of the implant and open a passage to the capsule with no risk of pricking the implant. The double-headed separator made it easy to release the capsule and preserve the overall esthetic. Finally, the innovative double-headed capsule-releasing devices are small and portable, which helps us to simplify the operation and shorten the recovery time. Although this new method places high requirements on the operator's skill and experience, ultrasound and MRI can help less skilled doctors perform these procedures. Ultrasound can assist in judging the thickness of the capsule and the integrity of the prosthesis before operation, help in the localization of ion stripping during operation, as well as help in the evaluation of the surgical effect including blood supply, etc. Nonetheless, it should be noted that if there is not much exudate from the implant, ultrasound may not be able to detect the gap between the contracture capsule and the prosthesis. Therefore, it is necessary to conduct a more accurate MRI examination before surgery to avoid the awkward situation of temporary replacement of prosthesis.
The surgical improvement seen in this study is the result of the design of a clever dissection tool that minimizes the incision and reduces unnecessary tissue damage. Perfect preoperative examination and judgment are helpful in obtaining better surgical results. Therefore, we will learn from this experience and use more accurate preoperative examinations such as MRI in future practice to avoid errors in judgment. We are also trying to confirm the effectiveness and long-term effect of this method by dealing with more cases.
We proposed an innovative surgical method for capsular contracture release after prosthesis breast augmentation. Our innovative surgical tools gave us the following results: reduced surgical trauma, a faster operation speed, a better effect, and a shorter recovery time. Ours is a new technique of capsule contracture release that is worth promoting.
The original contributions presented in the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Sir Run Run Shaw Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YZ and Y-YH contributed equally to this paper by way of drafting and revising the paper. W-YZ, X-FW, Q-QF, XL, and CX contributed in terms of performing the surgery and paper revision. W-QT and J-MY were senior authors with contributions in the form of performing the surgery, conceiving the study, and drafting and revising the paper. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the National Natural Science Foundation of China (No. 81671918 and 81372072), the Zhejiang Provincial Medical and Healthy Science Foundation of China (No. 2019ZD028), and the National Key Research Program of China (2016YFC1101004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.984732/full#supplementary-material.
1. Galdiero M, Larocca F, Iovene MR, Francesca M, Pieretti G, D'Oriano V, et al. Microbial evaluation in capsular contracture of breast implants. Plast Reconstr Surg. (2018) 141(1):23–30. doi: 10.1097/PRS.0000000000003915
2. Kaya S, Yaşar EK, Alagöz MS. The effect of omega-3 fatty acids on capsular tissue around the breast implants. Plast Reconstr Surg. (2021) 147(5):880e. doi: 10.1097/PRS.0000000000007811
3. Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. (2006) 117(3):757–72. doi: 10.1097/01.prs.0000201457.00772.1d
4. Tambasco D, Salgarello M. Prevention of capsular contracture with photochemical tissue passivation. Plast Reconstr Surg. (2014) 134(5):849e. doi: 10.1097/PRS.0000000000000632
5. Headon H, Kasem A, Mokbel K. Capsular contracture after breast augmentation: an update for clinical practice. Arch Plast Surg. (2015) 42(5):532–43. doi: 10.5999/aps.2015.42.5.532
6. Steiert AE, Boyce M, Sorg H. Capsular contracture by silicone breast implants: possible causes, biocompatibility, and prophylactic strategies. Med Devices (Auckl). (2013) 6:211–8. doi: 10.2147/MDER.S49522
7. Wolfram D, Rabensteiner E, Grundtman C, Böck G, Mayerl C, Parson W, et al. T regulatory cells and TH17 cells in peri-silicone implant capsular fibrosis. Plast Reconstr Surg. (2012) 129(2):327e–37e. doi: 10.1097/PRS.0b013e31823aeacf
8. Katzel EB, Koltz PF, Tierney R, Williams JP, Awad HA, O'Keefe RJ, et al. The impact of Smad3 loss of function on TGF-β signaling and radiation-induced capsular contracture. Plast Reconstr Surg. (2011) 127(6):2263–9. doi: 10.1097/PRS.0b013e3182131bea
9. Marques M, Brown SA, Cordeiro ND, Rodrigues-Pereira P, Cobrado ML, Morales-Helguera A, et al. Effects of coagulase-negative staphylococci and fibrin on breast capsule formation in a rabbit model. Aesthet Surg J. (2011) 31(4):420–8. doi: 10.1177/1090820X11404400
10. Tamboto H, Vickery K, Deva AK. Subclinical (biofilm) infection causes capsular contracture in a porcine model following augmentation mammaplasty. Plast Reconstr Surg. (2010) 126(3):835–42. doi: 10.1097/PRS.0b013e3181e3b456
11. Li S, Chen L, Liu W, Mu D, Luan J. Capsular contracture rate after breast augmentation with periareolar versus other two (inframammary and transaxillary) incisions: a meta-analysis. Aesthetic Plast Surg. (2018) 42(1):32–7. doi: 10.1007/s00266-017-0965-1
12. Wiener TC. Relationship of incision choice to capsular contracture. Aesthetic Plast Surg. (2008) 32(2):303–6. doi: 10.1007/s00266-007-9061-2
13. Wan D, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. (2016) 137(3):826–41. doi: 10.1097/01.prs.0000480095.23356.ae
14. Lee HK, Jin US, Lee YH. Subpectoral and precapsular implant repositioning technique: correction of capsular contracture and implant malposition. Aesthetic Plast Surg. (2011) 35(6):1126–32. doi: 10.1007/s00266-011-9714-z
15. Maxwell GP, Gabriel A. The neopectoral pocket in revisionary breast surgery. Aesthet Surg J. (2008) 28(4):463–7. doi: 10.1016/j.asj.2008.04.005
Keywords: capsular contraction release, breast implants, punctiform incision, nipple entry, innovative double-headed separator
Citation: Zheng Y, Hu Y, Zhao W, Wang X, Fang Q, Lv X, Xiang C, Yao J and Tan W (2022) Case Report: Improved surgical treatment for breast capsular contracture by the punctiform-incision approach through the nipple. Front. Surg. 9:984732. doi: 10.3389/fsurg.2022.984732
Received: 2 July 2022; Accepted: 15 August 2022;
Published: 9 September 2022.
Edited by:
Valeriano Vinci, Humanitas University, ItalyReviewed by:
Andrea Battistini, University of Milan, Italy© 2022 Zheng, Hu, Zhao, Wang, Fang, Lv, Xiang, Yao and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian-Min Yao eWptcHlAMTYzLmNvbQ== Wei-Qiang Tan dGFud2VpeHh4eEB6anUuZWR1LmNu
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.