
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 05 September 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.975026
This article is part of the Research Topic Clinical Application of Medical Imaging for Functional Evaluation in Orthopaedics View all 21 articles
 Jianzhou Luo1
Jianzhou Luo1 Kai Yang2
Kai Yang2 Zili Yang1
Zili Yang1 Chaoshuai Feng2
Chaoshuai Feng2 Xian Li1
Xian Li1 Zhenjuan Luo1
Zhenjuan Luo1 Huiren Tao1
Huiren Tao1 Chunguang Duan1,†
Chunguang Duan1,† Tailin Wu1,3*†
Tailin Wu1,3*†
Purpose: To investigate the optimal immediate sagittal alignment of kyphosis in ankylosing spondylitis (AS) following corrective osteotomy.
Methods: Seventy-seven AS patients who underwent osteotomy were enrolled. Radiographic parameters, including global kyphosis (GK), lumbar lordosis (LL), T1 spinopelvic inclination (T1SPI), sagittal vertical axis (SVA), T1 pelvic angle (TPA), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and PI and LL mismatch (PI–LL), were collected. The clinical outcome was evaluated using the Scoliosis Research Society-22 (SRS-22) questionnaire and Oswestry Disability Index (ODI). At the final follow-up, SVA > 5 cm was regarded as sagittal imbalance, and a total ODI ≤ 20 or total SRS-22 score ≥4 was considered to indicate a good clinical outcome.
Results: Seventy-seven patients with an average age of 37.4 ± 8.6 years were followed up for 29.4 ± 4.2 months. At the final follow-up, GK, LL, PT, SS, TPA, and T1SPI showed some degree of correction loss (P < 0.05). The follow-up parameters could be predicted with the immediate postoperative parameters through their linear regression equation (P < 0.05). The postoperative immediate T1SPI, TPA, SVA, and PI were also highly correlated with the clinical outcome (ODI and/or SRS-22) at the final follow-up (P < 0.05). Based on the relationship, the optimal immediate sagittal alignment for obtaining good clinical outcome was determined: T1SPI ≤ 0.9°, TPA ≤ 31.5°, and SVA ≤ 9.3cm. AS patients with PI ≤ 49.2° were more likely to achieve the optimal alignment and obtained lower ODI and a lower incidence of sagittal imbalance than those with PI > 49.2° at the final follow-up (P < 0.05).
Conclusion: Postoperative immediate parameters could be used to predict the final follow-up parameters and clinical outcome. The optimal postoperative immediate sagittal alignment of AS patients was T1SPI ≤ 0.9°, TPA ≤ 31.5°, and SVA ≤ 9.3 cm, providing a reference for kyphosis correction and a means for clinical outcome evaluation. Patients with a lower PI (≤49.2°) were more likely to achieve optimal alignment and obtain satisfactory clinical outcomes.
Ankylosing spondylitis (AS) is a chronic inflammatory disease. In advanced stages, AS is usually complicated by total spinal stiffness, thoracolumbar kyphosis, and pelvic retroversion. Individuals with AS might have trouble looking horizontally, lying flat, and standing or walking upright, seriously impairing their daily activities and quality of life (1). Osteotomy is the only effective method for correcting these deformities and providing these individuals with the opportunity for a normal life. However, for AS patients with kyphosis, the correction standard is elusive and the optimal postoperative immediate sagittal alignment following osteotomy is still not well understood (2).
Schwab et al. (3) proposed a sagittal vertical axis (SVA) <5.0 cm, pelvic tilt (PT) <25°, and pelvic incidence and lumbar lordosis mismatch (PI–LL) = ±9° as realignment objectives for adult spinal deformity (ASD). However, these values are different in AS patients. Recently, Huang et al. (4) reported PT < 24°, spinosacral angle >108°, T1 pelvic angle (TPA) < 22°, and spinopelvic angle >152° as the optimal sagittal objectives for AS patients at the 2-year follow-up. Notably, Huang proposed these values as goals for the 2-year follow-up; however, the optimal values for immediate alignment after surgery are still unknown and could be more pragmatic and meaningful for guiding kyphosis correction.
Therefore, in this study, we (1) determined the relationship between the immediate postoperative parameters and final follow-up parameters and clinical outcome in AS patients, (2) investigated an optimal immediate sagittal alignment based on the relationship, and (3) clarified the influence of PI on sagittal alignment and clinical outcome at the final follow-up.
Consecutive AS patients who underwent modified three-column osteotomy from January 2010 to July 2019 were reviewed retrospectively. The inclusion criteria were as follows: (1) age between 18 and 65 years old, (2) global kyphosis (GK) over 50°, (3) completed radiographs and clinical outcome measurements, and (4) a minimum of 2 years of follow-up. Patients with a history of previous spinal surgery, ankylosed hip or knee joints, postoperative pseudarthrosis, or instrumentation failure during the follow-up were excluded. Finally, a total of 77 AS patients, including 57 who underwent one-level osteotomy and 20 who underwent two-level osteotomy, met the criteria and were enrolled in this study.
The study was performed in accordance with the Declaration of Helsinki and approved by the institutional review board of Shenzhen University General Hospital. Informed consent was obtained from all participants before surgery.
Standing anteroposterior and lateral radiographs of the whole spine were obtained preoperatively, immediately postoperatively (3–4 weeks after surgery), and at the final follow-up (a minimum of 2 years after surgery). Several parameters were measured using lateral radiographs, including GK, LL, SVA, T1 spinopelvic inclination (T1SPI), TPA, pelvic incidence (PI), PT, sacral slope (SS), and PI–LL (Figure 1). The clinical outcome was evaluated using the Scoliosis Research Society-22 (SRS-22) questionnaire and Oswestry Disability Index (ODI). Data were collected before and after surgery as well as at the final follow-up. At the final follow-up, an SVA of >5 cm was regarded as sagittal imbalance (3), and a total ODI ≤ 20 or total SRS-22 score ≥4.0 was considered to indicate a good clinical outcome (4–6).
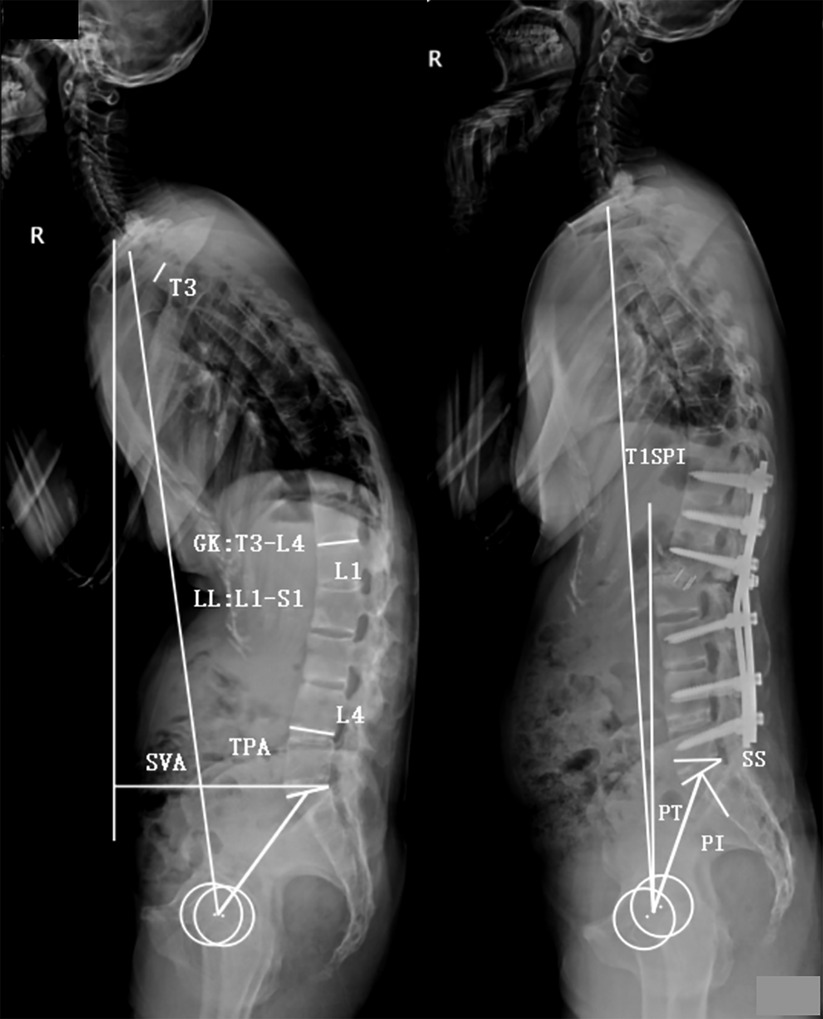
Figure 1. Illustration of radiographic parameters. Global kyphosis (GK): the angle between the superior endplate of the maximally tilted upper-end vertebra and the inferior endplate of the maximally tilted lower-end vertebra. Lumbar lordosis (LL): the Cobb angle from the L1 upper endplate to the S1 upper endplate (negative number represents lordosis, and positive number represents kyphosis). Sagittal vertical axis (SVA): the distance between the C7 plumb line and the posterior-superior corner of S1. T1 pelvic angle (TPA): the angle between a line joining the center of T1 and the femoral head axis and a line from the center of the femoral head axis to the midpoint of the S1 upper endplate. T1 spinopelvic inclination (T1SPI): the angle between the vertical line and a line from the center of the femoral head axis to the center of the T1 vertebral body (a negative number represents that T1 is posterior to the femoral head, and a positive number represents that T1 is anterior to the femoral head). Pelvic tilt (PT): the angle between the vertical line and the line from the center of the S1 upper endplate to the center of the femoral head axis. Pelvic incidence (PI): the angle between the perpendicular line to the S1 upper endplate and the line from the center of the S1 upper endplate to the center of the femoral head axis. Sacral slope (SS): the angle between the S1 upper endplate and the horizontal line. Pelvic incidence and lumbar lordosis mismatch (PI–LL): pelvic incidence value minus lumbar lordosis value.
The modified three-column osteotomy was usually performed in the apical region of kyphosis so that substantial kyphosis correction could be achieved. The whole procedure was performed under somatosensory-evoked potential and motor-evoked potential monitoring. The resection area of the corrective osteotomy included the spinous process, the upper part of the lamina and superior articular processes of the osteotomized vertebra, as well as the lower part of the lamina and inferior articular processes of the cranially adjacent vertebra. The transverse process of the osteotomized vertebra was exposed and resected; then, subtotal resection was performed along the upper part of the pedicles to the front of the vertebral body, which usually involved resecting 1/3–1/2 of the upper part of the vertebral body together with the cranially adjacent intervertebral disc. The lower half of the vertebral pedicle, part of the lamina, and the intact inferior articular processes of the osteotomized vertebra were preserved.
Temporary rods were implanted after finishing the osteotomy. Before correction, the spinal cord was slightly shortened in advance by compressing the rods, with the aim of preserving the space for potential spinal cord lengthening during correction. Sequentially, kyphosis was corrected gradually by lifting up the patient's shoulders while simultaneously bending the rods. After achieving satisfying correction, the temporary rods were replaced with precontoured rods successively. Subsequently, a local bone graft and a cage filled with autogenetic bone were implanted sequentially in the osteotomy space, further compressing the rods. The bone autograft was spread on the surface of the lamina to facilitate spinal fusion. Postoperatively, the patients were allowed to ambulate with a customized thoracolumbosacral orthosis 3 days after surgery, which was typically maintained for 6 months.
Measurement data are expressed as the mean ± standard deviation. Statistical analysis was performed using SPSS software (version 22.0, SPSS, Inc., Chicago, IL, USA). Paired t-tests were used to compare differences in the radiographic parameters and clinical outcome before and after surgery as well as at follow-up. The relationship between postoperative immediate parameters and final follow-up parameters was assessed with linear regression analysis. Correlations between postoperative immediate parameters and clinical outcome were evaluated using Pearson's correlation coefficient. Optimal thresholds of clinically relevant parameters were evaluated using receiver operating characteristic (ROC) curve analysis. Multiple stepwise linear regression analysis was performed to determine the key clinically relevant parameter and establish a predictive model for the total SRS-22 score. The difference between groups which was divided by the threshold of PI was using two independent t-tests and χ2 tests. A difference with a P-value <0.05 was considered statistically significant.
Seventy-seven AS patients (67 men and 10 women) with an average age of 37.4 ± 8.6 years (range, 20–64 years) and an average follow-up of 29.4 ± 4.2 months (range, 24–84 months) were included. The postoperative immediate GK, LL, PT, SS, PI–LL, TPA, T1SPI, and SVA were significantly improved (P < 0.01). At the final follow-up, GK, LL, PT, SS, TPA, and T1SPI showed some degree of correction loss (P < 0.05). Although the difference was not statistically significant, PI–LL (P = 0.078) and SVA (P = 0.115) also showed some loss of correction at the final follow-up. There was no significant difference in PI before and after surgery (P > 0.05) (Table 1).
Linear regression analysis showed that the postoperative immediate GK, LL, PT, SS, PI–LL, TPA, T1SPI, and SVA were positively correlated with the corresponding parameters at the final follow-up (R2 = 0.835, 0.817, 0.742, 0.551, 0.818, 0.857, 0.427, and 0.554, respectively, all P < 0.001, Figure 2). All these parameters at the final follow-up could be predicted with the immediate postoperative parameters through their linear regression equation.
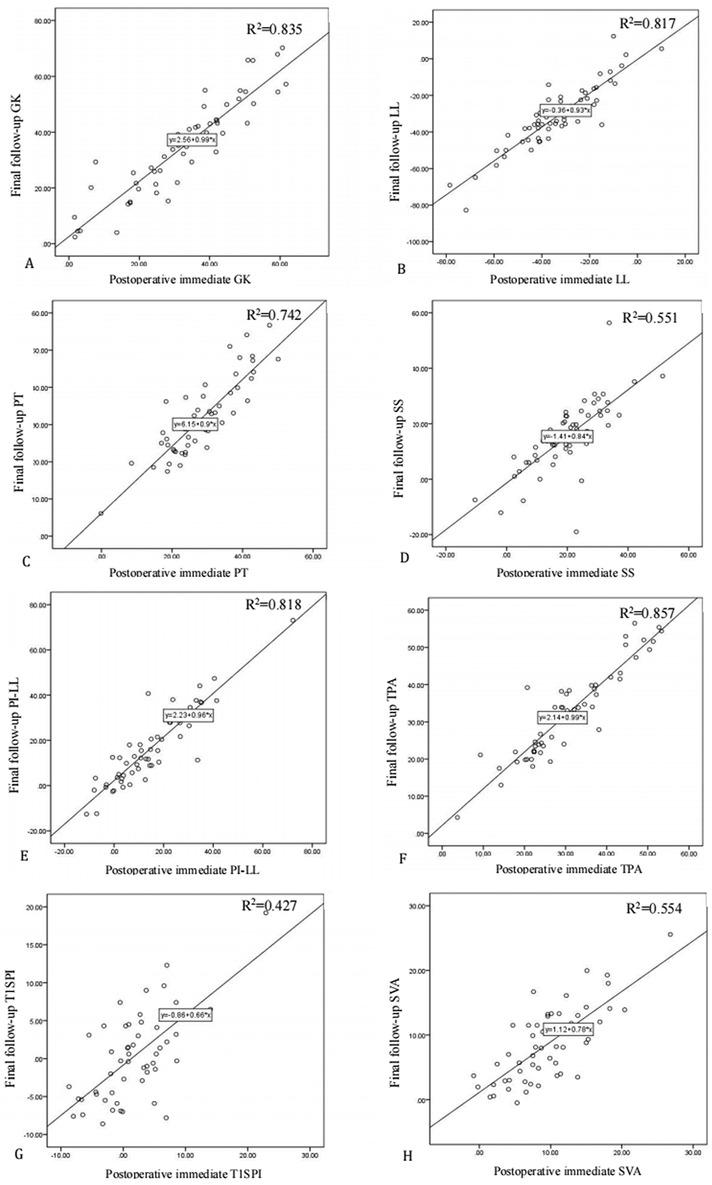
Figure 2. Linear regression analysis of postoperative immediate parameters and final follow-up parameters. (A) Final follow-up global kyphosis (GK) = 2.56 + 0.99 × postoperative immediate GK, R2 = 0.835; (B) final follow-up lumbar lordosis (LL) = −0.36 + 0.93 × postoperative immediate LL, R2 = 0.817; (C) final follow-up pelvic tilt (PT) = 6.15 + 0.9 × postoperative immediate PT, R2 = 0.742; (D) final follow-up sacral slope (SS) = −1.41 + 0.84 × postoperative immediate SS, R2 = 0.551; (E) final follow-up pelvic incidence and lumbar lordosis mismatch (PI–LL) = 2.23 + 0.96 × postoperative immediate PI–LL, R2 = 0.818; (F) final follow-up T1 pelvic angle (TPA) = 2.14 + 0.99 × postoperative immediate TPA, R2 = 0.857; (G) final follow-up T1 spinopelvic inclination (T1SPI) = −0.86 + 0.66 × postoperative immediate T1SPI, R2 = 0.427; and (H) final follow-up sagittal vertical axis (SVA) = 1.12 + 0.78 × postoperative immediate SVA, R2 = 0.554.
At the final follow-up, 29 patients (37.7%) had ODI ≤ 20 and 32 patients (41.6%) had SRS-22 ≥ 4.0, which were considered to have achieved a good clinical outcome. All domains of the SRS-22 and ODI were significantly improved at the final follow-up (P < 0.05) (Table 2). The correlation between the immediate postoperative parameters and the final follow-up clinical outcomes (ODI and SRS-22) was examined. The results showed that the postoperative immediate PI, SS, T1SPI, and SVA values significantly correlated with the total ODI (all P < 0.05), while the postoperative immediate T1SPI, SVA, and TPA values significantly correlated with the total SRS-22 score (all P < 0.05) (Table 3). This means that the clinical outcomes at the final follow-up could be assessed and predicted with the immediate postoperative parameters.
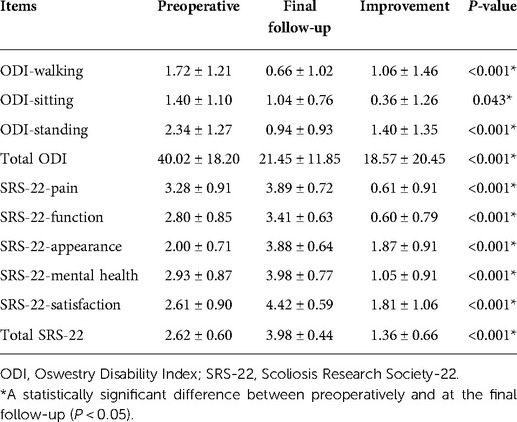
Table 2. Clinical outcomes of Oswestry Disability Index and Scoliosis Research Society-22 score after surgery.
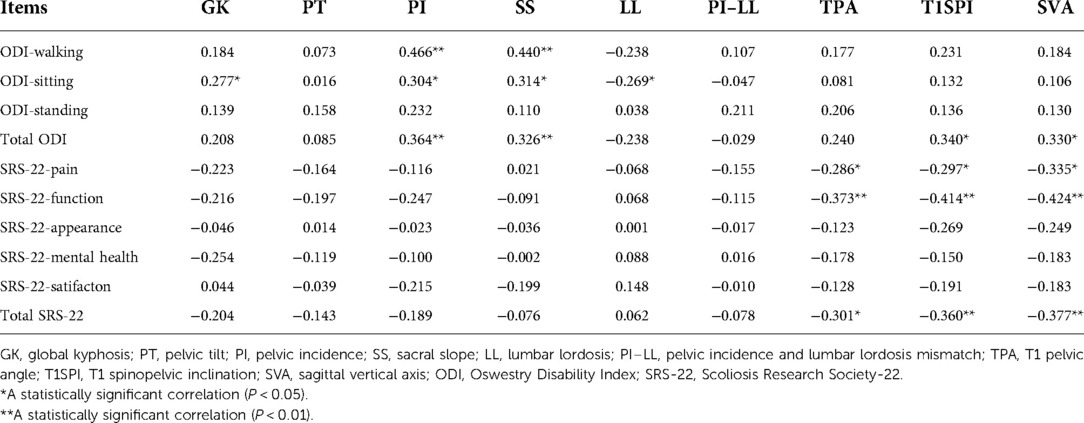
Table 3. Correlation between postoperative immediate parameters and final follow-up Oswestry Disability Index and Scoliosis Research Society-22 scores.
The clinically relevant parameters (PI, SS, T1SPI, SVA, and TPA) were subjected to ROC curve analysis to determine the optimal thresholds for obtaining good clinical outcomes. With total ODI as a state variable, only the PI showed a statistical significance (P < 0.05), while the SS, T1SPI, and SVA showed no significant difference (all P > 0.05). The optimal value of PI was ≤49.2° for obtaining good clinical outcome with a sensitivity of 99.8% and a false-positive rate of 36.7% (Figure 3A). With total SRS-22 as a state variable, all of the postoperative immediate T1SPI, TPA, and SVA were significantly different (all P < 0.05). The optimal value of T1SPI was ≤0.9° for obtaining good clinical outcome with a sensitivity of 70.0% and a false-positive rate of 17.6% (Figure 3B). The optimal value of TPA was ≤31.5° for obtaining good clinical outcome with a sensitivity of 63.3% and a false-positive rate of 11.8% (Figure 3C). The optimal value of SVA was ≤9.3 cm for obtaining good clinical outcome with a sensitivity of 63.3% and a false-positive rate of 11.8% (Figure 3D).
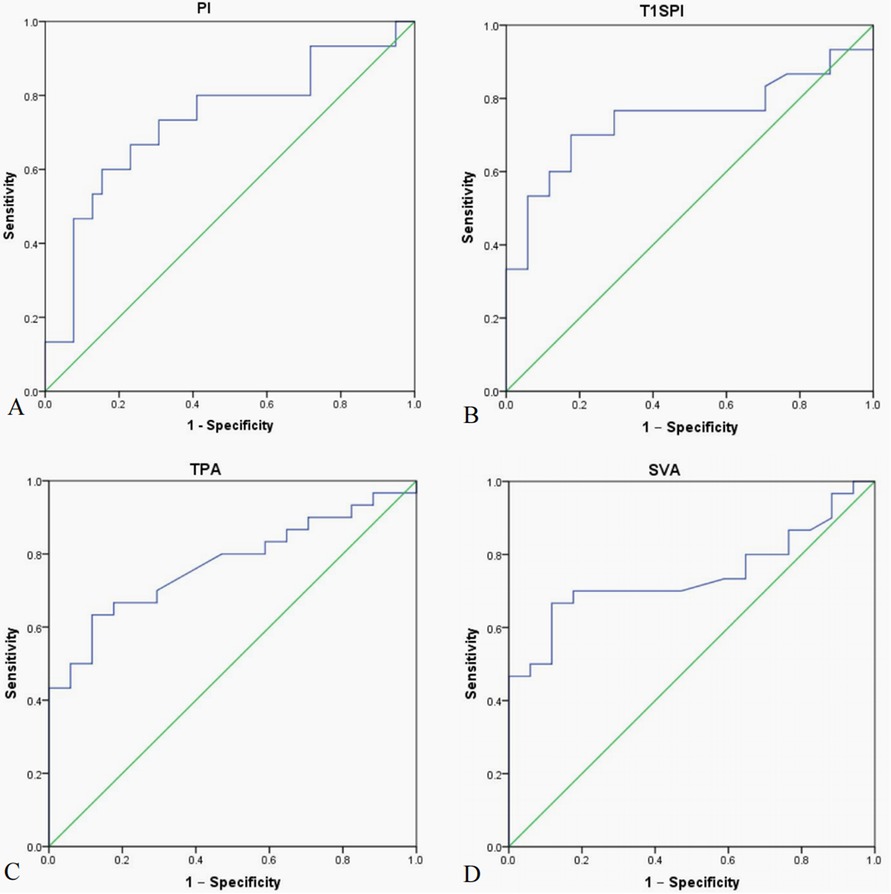
Figure 3. Receiver operating characteristic (ROC) curve analysis of clinically relevant parameters for the optimal threshold value. (A) The area under curve (AUC) for pelvic incidence (PI) was 0.733, the optimal threshold of PI was ≤49.2° for obtaining good clinical outcome with sensitivity of 73.3% and false-positive rate (1-Specificity) of 30.8%. (B) The AUC for T1 spinopelvic inclination (T1SPI) was 0.746, and the optimal threshold of T1SPI was ≤0.9° for obtaining a good clinical outcome with a sensitivity of 70.0% and a false-positive rate of 17.6%. (C) The AUC for T1 pelvic angle (TPA) was 0.772, and the optimal threshold of TPA was ≤31.5° for obtaining good clinical outcome with a sensitivity of 63.3% and a false-positive rate of 11.8%. (D) The AUC for sagittal vertical axis (SVA) was 0.741, and the optimal threshold of SVA was ≤9.3 cm for obtaining good clinical outcome with a sensitivity of 66.7% and a false-positive rate of 11.8%.
Multiple stepwise linear regression analysis was performed to determine the important clinically relevant parameters. With the total SRS-22 score as the dependent variable, the postoperative immediate T1SPI, TPA, and SVA were entered into the analysis. Finally, the SVA was the only parameter included in the regression model. The linear regression equation was total SRS-22 score = 4.247–0.033 × postoperative immediate SVA (adjusted R2 = 0.125, P = 0.006), which indicates that the model explains 12.5% of the variability in the cohort (Table 4).
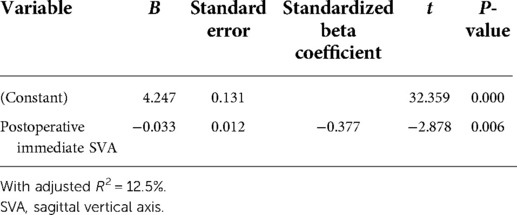
Table 4. Multiple stepwise linear regression analysis for the key clinically relevant parameter with total Scoliosis Research Society-22 as the dependent variable.
The cohort was divided into two groups according to the PI threshold of 49.2°. Forty-four patients with PI ≤ 49.2° were in group A, and 33 patients with PI > 49.2° were in group B. Preoperatively, group A had smaller PI, PT, SS, PI–LL, T1SPI, and TPA than group B (P < 0.05); there was no significant difference in all domains of ODI and SRS-22 (P > 0.05). Postoperatively, the PI, PT, SS, LL, PI–LL, TPA, and SVA were smaller in group A than in group B (P < 0.05). The average values of postoperative immediate T1SPI, TPA, and SVA in group A met the standard of optimal sagittal alignment (T1SPI ≤ 0.85°, TPA ≤ 31.5°, and SVA ≤ 9.3 cm), while all of them were over the threshold values in group B. At the final follow-up, the total ODI was lower in group A than in group B (P < 0.05), while there was no significant difference in SRS-22 (P > 0.05). The incidence of sagittal imbalance at the final follow-up was also lower in group A than in group B (Table 5 and Figure 4).
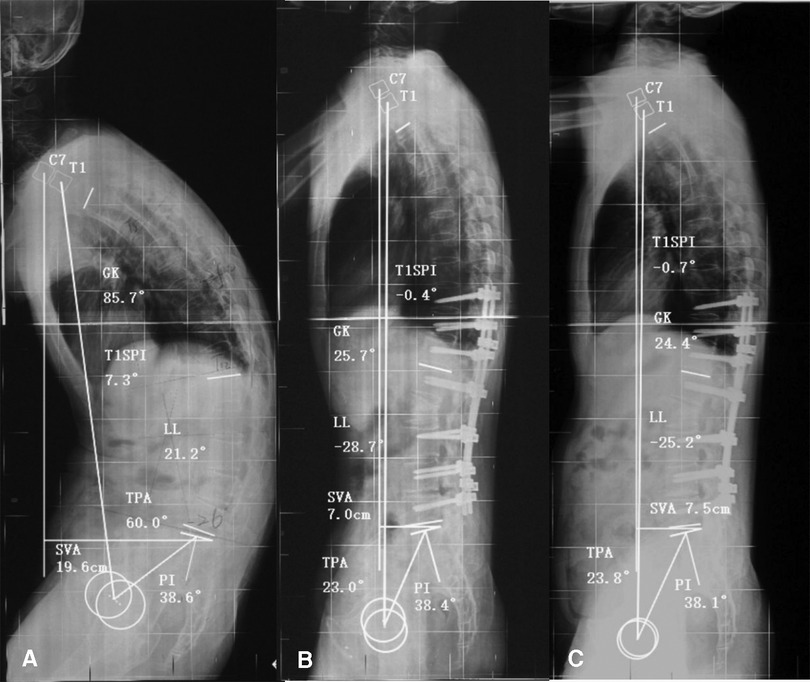
Figure 4. A 37-year-old man with ankylosing spondylitis kyphosis for 11 years. (A) The preoperative sagittal parameters were pelvic incidence (PI) = 38.6°, T1 spinopelvic inclination (T1SPI) = 7.3°, T1 pelvic angle (TPA) = 60.0°, and sagittal vertical axis (SVA) = 19.6 cm. (B) After L2 corrective osteotomy, the immediate postoperative sagittal parameters were PI = 38.4° (<49.2°), T1SPI = −0.4° (<0.9°), TPA = 23.0° (<31.5°), and SVA = 7.0 cm (<9.3 cm), all of which met the optimal parameter threshold values. (C) At the 25-month follow-up, the correction was well maintained, with PI = 38.1°, T1SPI = −0.7°, TPA = 23.8°, and SVA = 7.5 cm. The patient presented with a favorable health-related quality of life (total Oswestry Disability Index (ODI) = 0, total Scoliosis Research Society-22 (SRS-22) = 4.85).
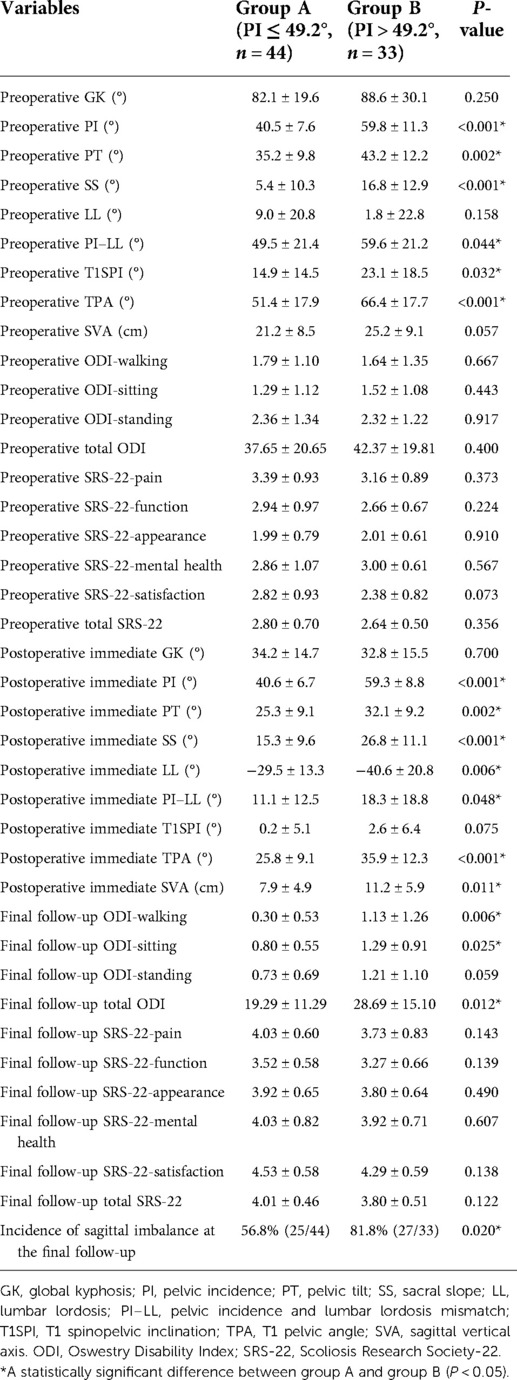
Table 5. Differences in radiographic parameters and clinical outcomes with different pelvic incidences.
Sagittal realignment in AS patients after the corrective osteotomy is a primary determinant of clinical outcome measures and is a complex challenge for surgeons (4, 7, 8). Failure to achieve optimal immediate sagittal alignment might result in residual kyphosis, increasing the risk of sagittal imbalance, instrumental failure, and even reoperation (8). However, until now, few studies have explored the immediate postoperative sagittal alignment in AS patients with kyphosis after corrective osteotomy. The goals for AS kyphosis correction are still unclear, which seriously limits preoperative planning and impairs postoperative clinical outcomes.
In this study, correction loss occurred in GK, LL, PT, SS, TPA, and T1SPI at the final follow-up. However, all the final follow-up parameters linearly correlated with their immediate postoperative parameters. This meant that sagittal alignment at the mid- or long-term follow-up could be evaluated and predicted with some parameters immediately after surgery and made it possible to intervene to prevent severe correction loss early. Furthermore, the postoperative immediate parameters were also significantly correlated with the clinical outcome (ODI and SRS-22) at the final follow-up. Among them, the pelvic parameters (PI and SS) and sagittal global parameters (T1SPI, TPA, and SVA) were closely correlated with ODI and/or SRS-22 scores, which were also consistent with the findings reported by Schwab and Lafage (3, 9). The results also revealed that the reconstruction of sagittal realignment (T1SPI, TPA, and SVA) and unique parameters (PI) could be used to assess and predict the clinical outcome measures at the final follow-up. The ROC analysis indicated that when postoperative immediate T1SPI ≤ 0.9°, TPA ≤ 31.5°, SVA ≤ 9.3 cm, and PI ≤ 49.2°, the AS patients were more likely to obtain a good clinical outcome at the final follow-up.
The T1SPI reflects the position of T1 relative to the pelvis through the hips. This parameter might be more pragmatic and accurate than the SVA in noncalibrated radiographs. In this study, the optimal T1SPI for achieving a satisfactory clinical outcome was ≤0.9°, while the normative value was −1.4° ± 2.7° (10). This means that corrective osteotomy should be performed to keep AS patients with a relatively low T1SPI to achieve a good clinical outcome because a large T1SPI might displace the trunk anteriorly relative to the femoral heads, resulting in malpositioning of the trunk in terms of its gravity and causing pain and disability (9). However, few studies have focused on the influence of T1SPIs on AS patients until now.
The goal for postoperative SVA varies among previous studies. Kim et al. (11) reported that the maintenance of SVA < 8 cm was important for ultimate sagittal reconstruction in fixed sagittal imbalance. Van Royen et al. (12) reported that the postoperative SVA ideally ranged from 5 cm to 10 cm, while Schwab et al. (13) reported that a postoperative SVA of more than 10 cm could be considered to indicate failed realignment. In this study, the optimal SVA was ≤9.3 cm for a good clinical outcome. In patients with ankylosed cervical vertebrae, sagittal alignment cannot be corrected perfectly to be within a normal range because a chin-brow vertical angle in the range of 10°–20° needs to be ensured and horizontal vision needs to be maintained for patients postoperatively (14). Meanwhile, although there may be some residual deformity in these patients, it might not affect their ability to perform basic daily tasks, and the corrections are maintained well over the follow-up period. Therefore, it might not be necessary to correct the SVA to a normal value with excessive expanding operations, placing these patients at an increased risk for various surgical complications. Thus, an immediate postoperative SVA of 9.3 cm or less might be sufficient for the correction of severe kyphosis in AS.
Moreover, the postoperative SVA was found to be a key clinically relevant parameter by multiple linear regression analysis, which is in agreement with the findings of previous studies (9, 13). A predictive model of the postoperative SRS-22 score was calculated, i.e., total SRS-22 score = 4.247–0.033 × postoperative immediate SVA. This equation allows the follow-up total SRS-22 score to be predicted in AS patients, whereas only ODI predictive methods have been reported in previous studies (4, 7, 13).
Unlike the SVA, the TPA is an angle reflecting global sagittal alignment, which does not vary on the basis of pelvic retroversion or patient standing posture (15, 16). To date, the optimal TPA for AS patients after the corrective osteotomy is still unclear. Protopsaltis et al. (15) found that TPA > 20° might result in severe disability (ODI > 40) for ASD, and they recommended TPA < 14° as a postoperative target (ODI < 20). However, Banno et al. (16) investigated 656 elderly healthy volunteers and determined that a TPA of 26° was the threshold value for an ODI of 40, while a TPA of 20° was the threshold value for an ODI of 20. Their study also noted that the optimal TPA varies widely by race, sex, and disease (16). Recently, Huang et al. (4) reported TPA < 22° as a goal in AS patients to achieve a satisfactory clinical outcome (ODI < 20) following osteotomy. According to our data, the optimal TPA was <31.5°, which was calculated on the basis of a total SRS-22 score ≥4.0. Several reasons could explain the difference between this optimal TPA and that reported by Huang et al. (4). First, the patients in this study had more severe deformities than those in the study by Huang and were thus hard to correct perfectly but still satisfied with the improvement in quality of life. Second, the optimal threshold value for the TPA in this study was calculated by ROC curve analysis based on a total SRS-22 score ≥4.0, while Huang used linear regression equations to calculate the TPA based on ODI <20.
PI is a constant morphological parameter that is unique regardless of the rotation of the pelvis (7, 8, 17). Our data indicated that PI plays a key role in sagittal alignment reconstruction and significantly affects clinical outcome measures. Although PI showed no change after surgery, it was highly correlated with the recovery of clinically relevant parameters (1, 8, 17). For patients with a large PI value, it is difficult to achieve spinal and pelvic balance, leading to a negative clinical outcome and potentially even large correction loss at the final follow-up (7, 18, 19). Qian et al. (8) reported that patients with PI ≤ 50° were more likely to achieve spinopelvic matching and decrease the chance of sagittal imbalance on follow-up. Similar to the study by Qian et al. (8), this study validated the conclusion that AS patients with PI ≤ 49.2° achieved optimal immediate postoperative sagittal alignment and obtained better clinical outcomes and a lower incidence of sagittal imbalance than those with PI > 49.2° at the final follow-up. These results further confirmed that PI is a critical parameter for sagittal realignment that affects global balance achievement and clinical outcome restoration in AS patients after osteotomy. Therefore, the surgeon should pay more attention to PI in reconstructing sagittal alignment to achieve optimal sagittal alignment and should choose appropriate osteotomy techniques and the number of osteotomy segments to obtain enough correction for correction (3, 19).
Of the four key radiographic parameters determined in this study, the T1SPI, TPA, and SVA represent spinal alignment and can be corrected directly with surgical treatment; although PI, as a pelvic parameter, cannot be changed by surgery, it can influence the spine and pelvis harmony, affecting the maintenance of spinopelvic balance. Therefore, the spinal and pelvic parameters should be taken into consideration for a good clinical outcome while reconstructing an optimal sagittal alignment.
First, this was a retrospective study in which a limited number of patients were enrolled. Second, the influence of one-level and two-level osteotomy on the postoperative sagittal alignment was not compared separately. Third, radiographic parameter evaluation is only one aspect in evaluating the clinical outcome in AS patients. The surgery itself might influence the clinical outcome, and other potential factors, such as age, sex, and comorbidities, might also affect the clinical outcome reported by patients. Finally, although most of the AS patients who underwent osteotomy were in an inflammatory static state, AS did affect the quality of life on follow-up. In the future, a prospective study with a larger sample size is required to further confirm the conclusions.
The results of this study demonstrated that the immediate postoperative parameters could be used to evaluate and predict the final follow-up parameters and clinical outcome in AS patients. In particular, the PI and postoperative immediate T1SPI, TPA, and SVA significantly correlated with the clinical outcome measures. The optimal postoperative immediate sagittal alignment was T1SPI ≤ 0.9°, TPA ≤ 31.5°, and SVA ≤ 9.3 cm, providing a reference for kyphosis correction and a means for clinical outcome evaluation. Patients with lower PI values (≤49.2°) are more likely to achieve better sagittal alignment and clinical outcomes after corrective osteotomy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Human Investigation Committee of Shenzhen University General Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JL, KY, ZY, and CF collected the radiographic and clinical data and measured the parameters. XL and ZL analyzed the clinical data and measurements; JL wrote the manuscript; HT, CD, and TW revised the manuscript; CD and TW conceived the idea and designed the study. All authors reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Natural Science Foundation of Guangdong Province (2020A1515010726), Basic Research of Shenzhen Science and Technology Project (JCYJ20180305124242438), Shenzhen Major Project of Fundamental Research (JCYJ20200109114233670), Key Research and Development Program of Guangdong Province (2020B0909020002), Sanming Project of Medicine in Shenzhen (SZSM201911011), and the Shenzhen Key Laboratory Foundation (ZDSYS20200811143757022).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Shin JK, Lee JS, Goh TS, Son SM. Correlation between clinical outcome and spinopelvic parameters in ankylosing spondylitis. Eur Spine J. (2014) 23(1):242–7. doi: 10.1007/s00586-013-2929-8
2. Koller H, Koller J, Mayer M, Hempfing A, Hitzl W. Osteotomies in ankylosing spondylitis: where, how many, and how much? Eur Spine J. (2018) 27(Suppl 1):70–100. doi: 10.1007/s00586-017-5421-z
3. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). (2010) 35(25):2224–31. doi: 10.1097/BRS.0b013e3181ee6bd4
4. Huang JC, Qian BP, Qiu Y, Wang B, Yu Y, Qiao M. What is the optimal postoperative sagittal alignment in ankylosing spondylitis patients with thoracolumbar kyphosis following one-level pedicle subtraction osteotomy? Spine J. (2020) 20(5):765–75. doi: 10.1016/j.spinee.2019.11.005
5. Baldus C, Bridwell KH, Harrast J, Edwards C 2nd, Glassman S, Horton W, et al. Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: are all SRS domains disease specific? Spine (Phila Pa 1976). (2008) 33(20):2214–8. doi: 10.1097/BRS.0b013e31817c0466
6. Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK, Protopsaltis T, et al. Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine. (2015) 23(3):349–59. doi: 10.3171/2014.12.Spine14777
7. Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). (2013) 38(13):E803–12. doi: 10.1097/BRS.0b013e318292b7b9
8. Qian BP, Jiang J, Qiu Y, Wang B, Yu Y, Zhu ZZ. Radiographical predictors for postoperative sagittal imbalance in patients with thoracolumbar kyphosis secondary to ankylosing spondylitis after lumbar pedicle subtraction osteotomy. Spine (Phila Pa 1976). (2013) 38(26):E1669–75. doi: 10.1097/BRS.0000000000000021
9. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). (2009) 34(17):E599–606. doi: 10.1097/BRS.0b013e3181aad219
10. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. (2005) 87(2):260–7. doi: 10.2106/jbjs.D.02043
11. Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a Minimum 5-year follow-up study. Spine (Phila Pa 1976). (2007) 32(20):2189–97. doi: 10.1097/BRS.0b013e31814b8371
12. Van Royen BJ, De Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J. (2000) 9(6):492–8. doi: 10.1007/s005860000183
13. Schwab FJ, Patel A, Shaffrey CI, Smith JS, Farcy JP, Boachie-Adjei O, et al. Sagittal realignment failures following pedicle subtraction osteotomy surgery: are we doing enough? Clinical Article. J Neurosurg Spine. (2012) 16(6):539–46. doi: 10.3171/2012.2.Spine11120
14. Song K, Su X, Zhang Y, Liu C, Tang X, Zhang G, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J. (2016) 25(8):2596–604. doi: 10.1007/s00586-016-4588-z
15. Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, et al. Thet1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. (2014) 96(19):1631–40. doi: 10.2106/jbjs.M.01459
16. Banno T, Hasegawa T, Yamato Y, Kobayashi S, Togawa D, Oe S, et al. T1 pelvic angle is a useful parameter for postoperative evaluation in adult spinal deformity patients. Spine (Phila Pa 1976). (2016) 41(21):1641–8. doi: 10.1097/brs.0000000000001608
17. Sato T, Yonezawa I, Inoue H, Tada K, Kobayashi S, Hayashi E, et al. Relationship between characteristics of spinopelvic alignment and quality of life in Japanese patients with ankylosing spondylitis: a cross-sectional study. BMC Musculoskelet Disord. (2020) 21(1):41. doi: 10.1186/s12891-020-3040-z
18. Liu ZJ, Qian BP, Qiu Y, Mao SH, Jiang J, Wang B. Does postoperative PI-LL mismatching affect surgical outcomes in thoracolumbar kyphosis associated with ankylosing spondylitis patients? Clin Neurol Neurosurg. (2018) 169:71–6. doi: 10.1016/j.clineuro.2018.04.006
Keywords: ankylosing spondylitis, kyphosis, optimal sagittal alignment, osteotomy, clinical outcome
Citation: Luo J, Yang K, Yang Z, Feng C, Li X, Luo Z, Tao H, Duan C and Wu T (2022) Optimal immediate sagittal alignment for kyphosis in ankylosing spondylitis following corrective osteotomy. Front. Surg. 9:975026. doi: 10.3389/fsurg.2022.975026
Received: 21 June 2022; Accepted: 4 August 2022;
Published: 5 September 2022.
Edited by:
Yan Yu, Tongji University School of Medicine, ChinaReviewed by:
Osvaldo Mazza, Bambino Gesù Children's Hospital (IRCCS), Italy© 2022 Luo, Yang, Yang, Feng, Li, Luo, Tao, Duan and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tailin Wu VExfc3BpbmVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share last authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations AS, ankylosing spondylitis; ASD, adult spinal deformity; AUC, area under the curve; GK, global kyphosis; LL, lumbar lordosis; ODI, Oswestry Disability Index; PI, pelvic incidence; PI-LL, pelvic incidence and lumbar lordosis mismatch; PT, pelvic tilt; ROC, receiver operating characteristic curve; SRS-22, Scoliosis Research Society-22; SS, sacral slope; SVA, sagittal vertical axis; TPA, T1 pelvic angle; T1SPI, T1 spinopelvic inclination.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.