- 1Department of Orthopaedics, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, Jiangsu, China
- 2School of Medicine, Southeast University, Nanjing, Jiangsu, China
- 3Orthopaedic Trauma Institute (OTI), Southeast University, Nanjing, Jiangsu, China
- 4Trauma Center, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, Jiangsu, China
Background: Ankle fracture-dislocations are one of the most severe types of ankle injuries. Compared to the simple ankle fractures, ankle fracture-dislocations are usually more severely traumatized and can cause worse functional outcomes. The purpose of this study was to review the previous literatures to understand the anatomy, mechanisms, treatment, and functional outcomes associated with ankle fracture-dislocations.
Methods: The available literatures from January 1985 to December 2021 in three main medical databases were searched and analyzed. The detailed information was extracted for each article, such as researchers, age, gender, groups, type of study, type of center research, level of evidence, significant findings, study aim, cause of injury, time from injury to surgery, type of fracture, direction of dislocation, follow-up, postoperative complications and functional evaluation scores.
Results: A total of 15 studies (1,089 patients) met the inclusion criteria. Only one study was a prospective randomized trial. The top-ranked cause of injury was high-energy injury (21.3%). Moreover, the most frequent type of fracture in ankle dislocations was supination-external rotation (SER) ankle fracture (43.8%), while the most common directions of dislocation were lateral (50%) and posterior (38.9%).
Conclusions: Collectively, most ankle fracture-dislocations are caused by high-energy injuries and usually have poor functional outcomes. The mechanism of injury can be dissected by the ankle anatomy and Lauge-Hansen's classification. The treatment of ankle fracture-dislocations still requires more detailed and rational solutions due to the urgency of occurrence, the severity of injury, and the postoperative complications.
Introduction
Ankle fractures are one of the most widespread fractures in adults, with a morbidity of 174 per 100,000 per years (1). The dislocation of ankle fracture is a more severe injury and is characterized by the loss of alignment of tibial and talar articular surfaces. The characteristics and mechanisms of pure ankle dislocations have been summarized in a previous systematic review (2). However, the progress of research related to the ankle fracture-dislocations have not been well summarized and analyzed recently.
The patients who experience the ankle fracture-dislocations tend to have poorer functional outcomes (3–6). This may be due to the fact that higher-violence injuries exacerbate the damage to ligaments surrounding the ankle joint. Hence, the treatment of this type of injury also needs to be supported by a higher level of evidence to develop a more detailed and better treatment process, including the emergency management, surgical timing, surgical approach and so on. The purpose of this study was to provide a systematic review of the epidemiology, anatomy, mechanism of injury, treatment and prognosis of the ankle fracture-dislocations, so as to provide certain reference for the relevant researches in the future.
Methods
Search strategy
The electronic literatures were searched from PubMed, Web of science and Scopus databases using the search terms of “ankle fracture-dislocations”, “dislocated ankle fractures”, “fracture-dislocation of the ankles” and “Malleolar fracture dislocation”. The overall search procedures, including literatures search, data extraction and quality evaluation were performed by the two independent reviewers. The referenced papers included in reviewed articles were also examined, and the final search was performed on 5 January 2022.
Study selection
Studies were excluded if they were case reports, case series, conference abstracts. Moreover, the manuscripts were unable to be reviewed if it cannot be presented in a type of full-text. A fracture-dislocation was diagnosed when radiographs demonstrated ankle fractures with the presence of separation of the talus relative to the tibia on either the anteroposterior or lateral view. The search was performed by each reviewer independently with any disagreements in article eligibility resolved by the consensus discussion among all authors. Moreover, studies on the ankle fracture-dislocations that were written in English and presented as full-text were included in this review. Studies that were not written in English, not related to the topic of ankle fracture-dislocations, pure ankle dislocations, included only specific types of ankle fracture-dislocations, such as the “Logsplitter” injury (7), and lacked population characteristics were also excluded.
Data extraction and study quality assessment
All data were collected by the two reviewers according to the uniform criteria. We documented the first author, title, published journal, year, type of study, design, and level of evidence of each study. The demographic data were recorded and extracted, including the groups, sample size, gender and age. The detailed data includes time from injury to surgery, operative time, fracture classification, surgical technique, clinical outcomes and postoperative complications. Moreover, the postoperative complications mainly included infection, posttraumatic arthritis, delayed union, nonunion, malunion and so on. The level of evidence was evaluated based on the guidelines of the Oxford Centre for Evidence-Based Medicine (8).
Statistical analysis
The overall data in this current review were exhibited as the count (percentage) or mean ± standard deviation (SD). The pooled means were calculated for the mean age, time from injury to surgery and length of follow-up.
Results
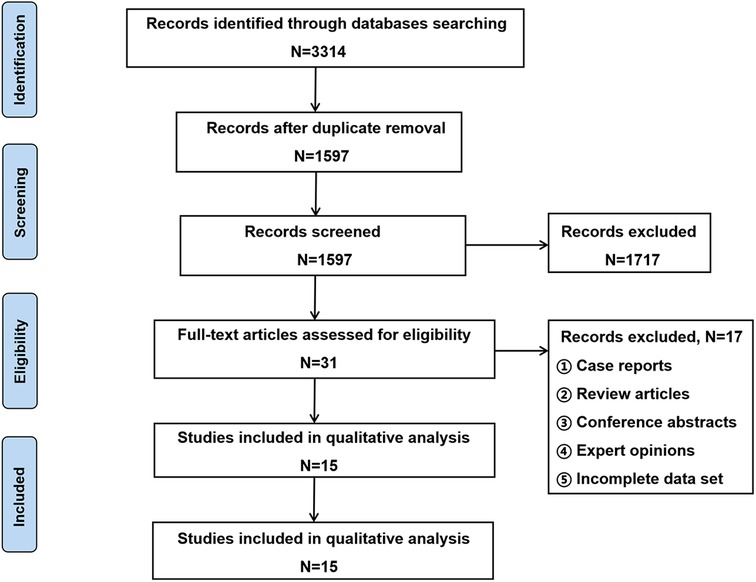
The results of search strategy and study selection criteria are shown in Figure 1, and a total of 15 studies were included in this study (3–6, 9–19). This study was reported on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
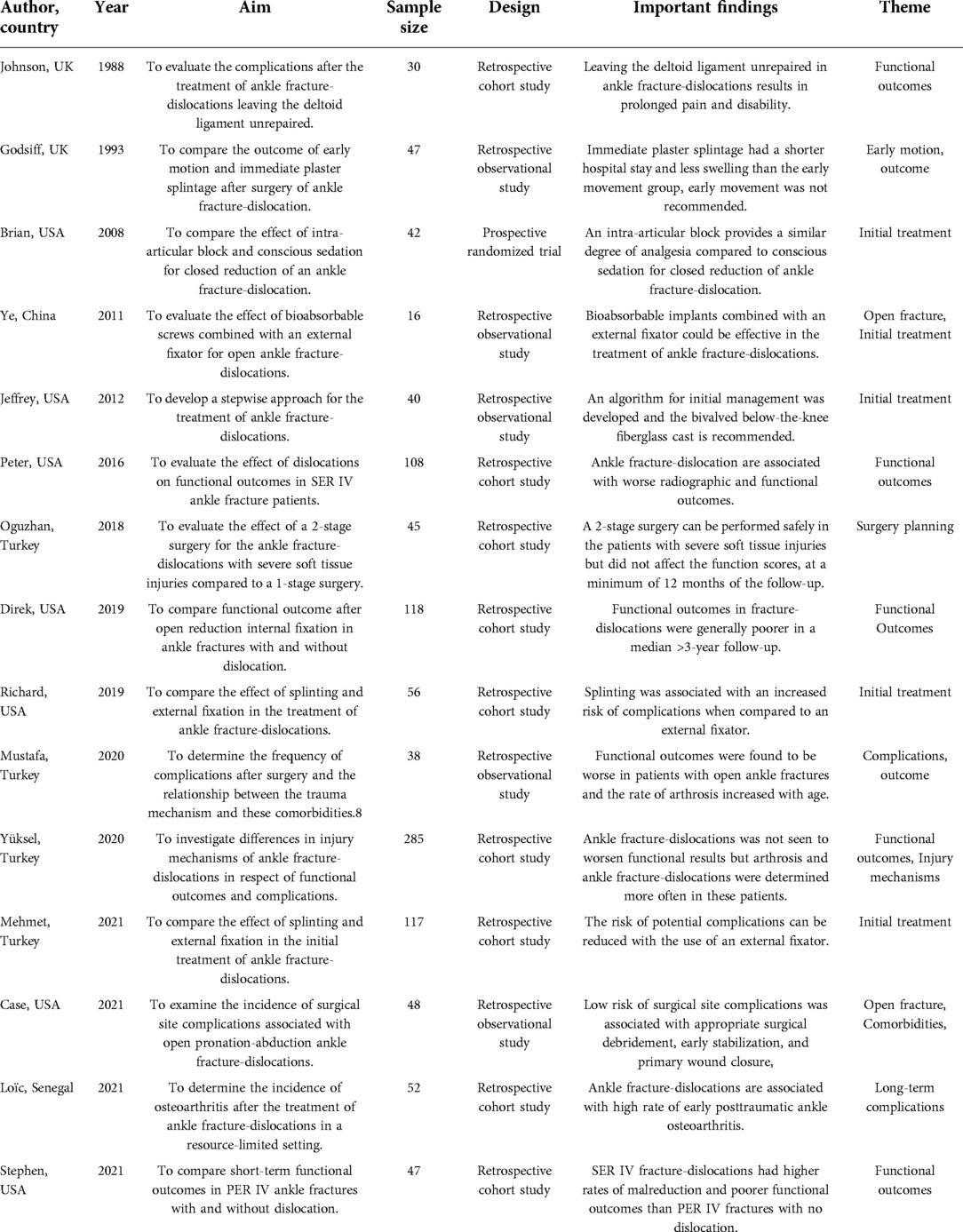
Key information
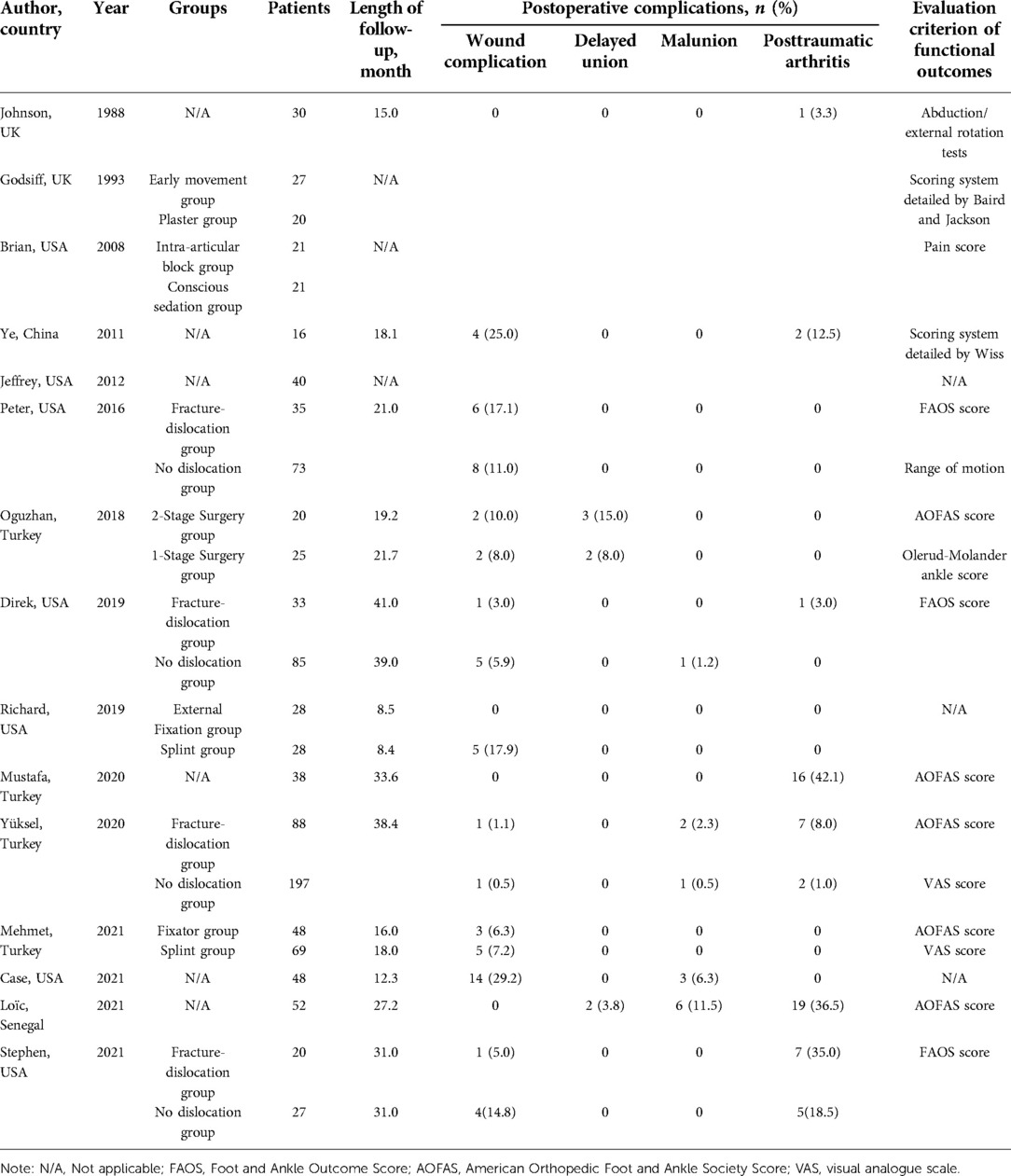
A total of 1,089 patients were enrolled in 15 included studies. As shown in Table 1, eight of these studies focused on the complications and functional outcomes after the surgery of ankle fracture-dislocations. Seven studies focused on comparing different treatment approaches for ankle fracture-dislocations. Two of seven studies compared the efficacy of splinting versus temporary external fixation. Moreover, only one study was prospective, while the remaining were retrospective. Generally, the patients with ankle fracture-dislocations had worse functional outcomes compared to those without dislocations, but the postoperative complications were similar. In the initial course of treatment, the block in closed reduction was comparable to conscious sedation, and the temporary external fixation and two-stage surgery were recommended for the treatment of ankle fracture-dislocations.
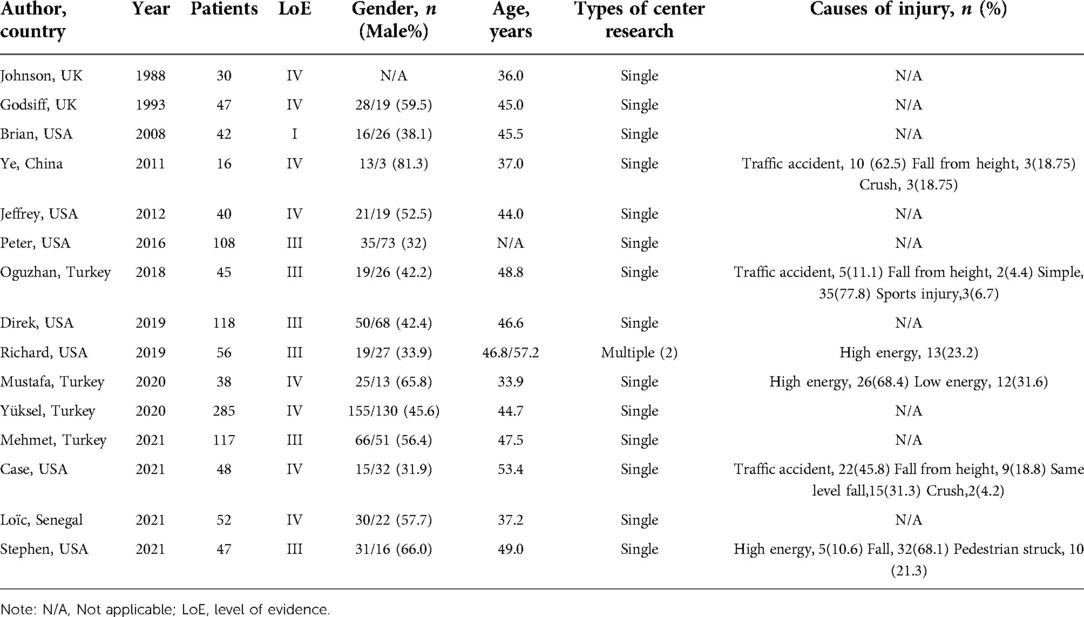
Population characteristics
As exhibited in the Table 2, only one study was a multi-center study, while the rest were single-center studies. The mean age of all patients was 44.84 years. Males and females were equally represented, accounting for 49.4% and 50.6% of the total number, respectively. Six studies reported the cause of injury, with the highest percentage of high-energy injuries (21.3%), followed by traffic accidents (17.9%).
Clinical characteristics
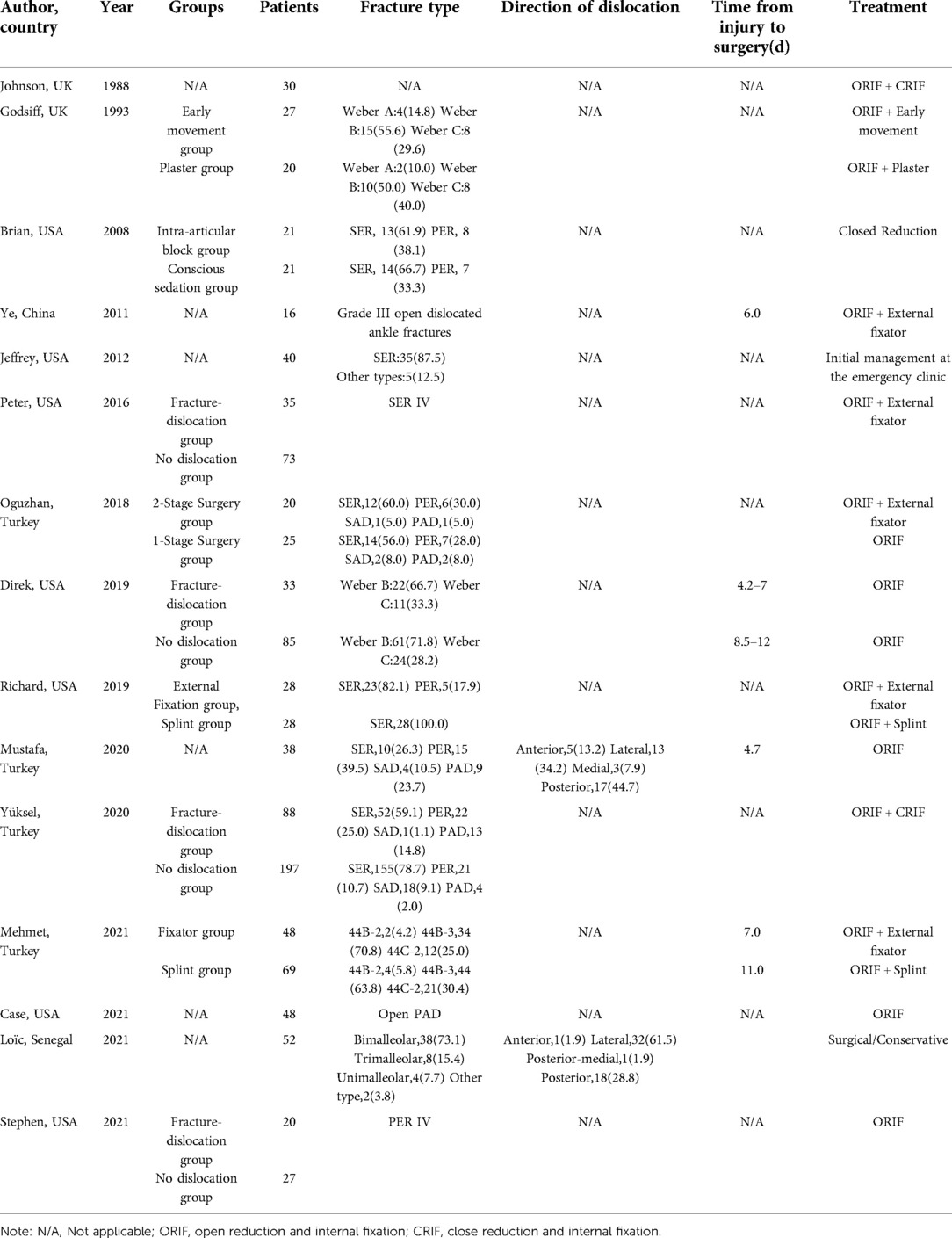
As shown in the Table 3, nine studies were grouped to compare. Fourteen studies described the type of fracture, with the highest percentage of SER fracture (43.8%) followed by pronation-external rotation (PER) fracture (13.0%). Moreover, two studies documented the direction of dislocation, with the vast majority of these being lateral dislocations (50.0%) and posterior dislocations (38.9%). The pooled mean time from injury to surgery was 7.2 (range 4.7 to 11.0) days. The most significant method of treating ankle fracture-dislocations was the open reduction and internal fixation (ORIF) and was supplemented by closed reduction and internal fixation (CRIF) and external fixator or splinting.
Clinical outcomes
As shown in Table 4, the pooled mean follow-up time was 21.7 (range 8.4 to 41.0) days. Twelve studies reported the postoperative complications, including the wound complications in 62 patients (6.5%), arthritis in 62 patients (6.5%), and delayed healing and nonhealing in 7 patients (0.7%) and 13 patients (1.4%), respectively. Of the 12 studies that reported functional evaluation criterion, 3 studies used FAOS score, while 5 studies used AOFAS score as the functional evaluation score.
Discussion
Based on the key findings of our systematic review of ankle fracture-dislocations, most studies have focused on the treatment and functional outcomes. In order to explore the injury in depth, we decided to look at the anatomy as well as the pathological mechanisms of the ankle joint and further discuss the treatment as well as the prognosis by analyzing the pattern of injury. The purpose of this systematic review is to provide a more scientific and comprehensive understanding of ankle fracture-dislocations to guide treatment selection and subsequent related studies from the following aspects.
Epidemiology
Ankle fractures are one of the most common types of lower-extremity fractures, accounting for approximately 10% of all fractures (1, 20–22). Dislocation referred to a complete discontinuity of the tibial talocrural joint, while subluxation was defined as a loss of coherence of the articular surfaces in contact with the articular cartilage with respect to the tibia on either the anteroposterior or lateral view (24). The proportion of ankle subluxations or dislocations is difficult to realistically reflect because many patients with ankle fracture-dislocations may have undergone closed reduction prior to radiographic evaluation. Several studies have shown that dislocation occurs in approximately 30%–50% of ankle fractures (3–5), and risk factors associated with ankle fracture-dislocation were also noted, including the old age, female, diabetes, and so on (5). Other than that, the probability of recurrence of ankle dislocation was minimal, compared to the high re-dislocation rate of shoulder and hip dislocations (23). Speaking further back to the dislocation, lateral, posterior and posterolateral were the top three subtypes of the ankle dislocations. Predictably, the type of ankle fracture most prone to dislocation is the triple ankle fracture, which accounts for nearly half of the patients. In addition, about 7% of patients were combined with the open ankle fracture-dislocations (24).
Anatomy
The ankle joint is consisted of the talocrural joint and distal tibiofibular joint. Therein, the talocrural joint, is a modified hinged and uniaxial joint and the lateral surface of medial ankle is covered with cartilage as seen in an arthroscopic anatomical study (25). The talar body is wedge-shaped and is approximately 4–5 mm wider anteriorly than posteriorly (22), and the width between medial and lateral ankles is greater anteriorly than posteriorly, which allows the trochlea to closely match the malleoli during plantar dorsiflexion and flexion (26). The tight connection of three bony structures forms the cornerstone of ankle stability.
Moreover, the ankle joint is primarily supported by three groups of ligaments (Figure 2), including the lateral ligament, medial deltoid ligament, and the ligaments of tibiofibular syndesmosis. The lateral collateral ligament is consisted of anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL). The ATFL is the most vulnerable of ankle ligaments and has a role in limiting the anterior displacement of talus and plantar flexion (27). The PTFL is a multi-fascicular ligament that primarily limits the external rotation of talus and is tense during the process of plantar dorsiflexion (28, 29). Moreover, medial deltoid ligament is often considered to be the strongest of the peri-ankle ligaments. The deltoid ligament limits the external rotation of talus and excessive valgus of ankle joint. It is susceptible to injury during the excessive anterior external rotation or posterior external rotation of the ankle (30).
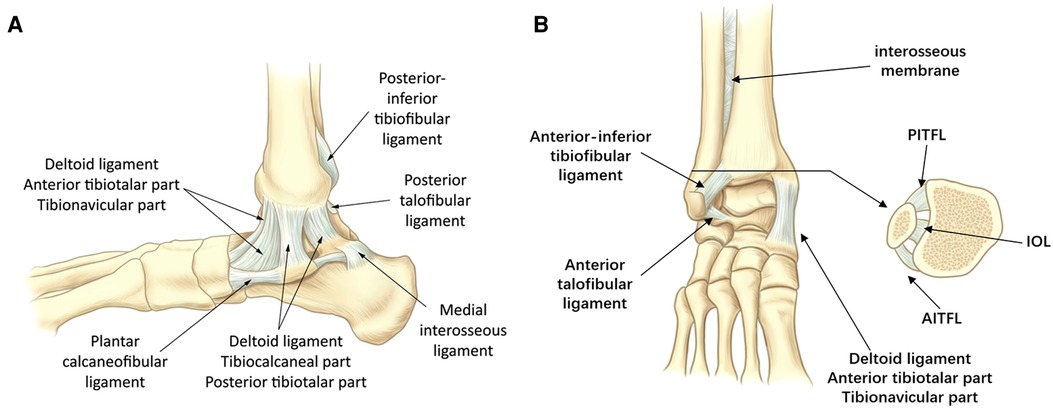
Figure 2. The periprosthetic ligament of the ankle joint complex. (A) Medial view. (B) Anterior view. Note: AITFL, anterior tibiofibular ligament; IOL, interosseous ligament; PITFL, Posterior tibiofibular ligament.
The tibiofibular syndesmosis is generally composed of the anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL) and interosseous tibiofibular ligament (IOL). Functionally speaking, the role of the AITFL is to tighten the fibula to the tibia and limit the excessive motion of fibula and external rotation of talus (32, 33). A cadaveric study showed that cutting only the AITFL resulted in almost three times the distance of talus displacement compared to cutting only the PITFL. This result suggests that the AITFL appears to be more important for ankle stability (34).
The PITFL is generally considered to have two parts (a superficial and a deep component). Importantly, partial analyses indicate that transverse ligament is an important structure independent of the posterior inferior tibiofibular ligament (31). Its fibers often reach the medial ankle and form a posterior labrum deepening the articular surface of the distal tibia, and this structure can limit posterior displacement of the talus (35, 36).
The IOL is considered to be the distal continuation of interosseous membrane of tibiofibular joint, which mainly inhibits the lateral translation of fibula (37, 38). Several mechanical analyses have shown that the IOL is stronger than the AITFL (38, 39), and the injury to IOL is often accompanied with the injury to AITFL (32).
Pathophysiology
In terms of the injury pattern of ankle fracture-dislocations, strong violence causes the fracture and ligament damage and eventually results in the loss of alignment of the articular surfaces.
The Lauge-Hansen's classification is the basis of ankle fracture mechanism and four types of ankle fracture-dislocations according to classification are exhibited in Figure 3 (40). The most common type of Lauge-Hansen classification is the SER ankle fracture, which accounts for approximately 60%–85% of all ankle fractures (41, 42). One study showed that 25% of SER ankle fractures were combined with dislocation (6). Further, partial studies showed a higher percentage of SER III/IV fractures in the ankle fracture-dislocations group (3, 5, 43). Based on the sequence of violence transmission, it can be further hypothesized that SER IV ankle fractures are more likely to be accompanied with syndesmotic injury. Moreover, this injury pattern is also more likely to result in the occurrence of dislocation. The suggested mechanisms of syndesmotic injury include the external rotation of foot, the eversion of talus within the ankle mortise and excessive dorsiflexion (44, 45). In these patterns of injury, the distal fibula is pushed away from the distal tibia and causes the ankle mortise to widen. Hence, the severe injuries to syndesmosis often lead to the dislocation of ankle (46). In this case, with the direction of violence, the talus would dislocate laterally and posterior-laterally, followed by the dislocation to posterior side.
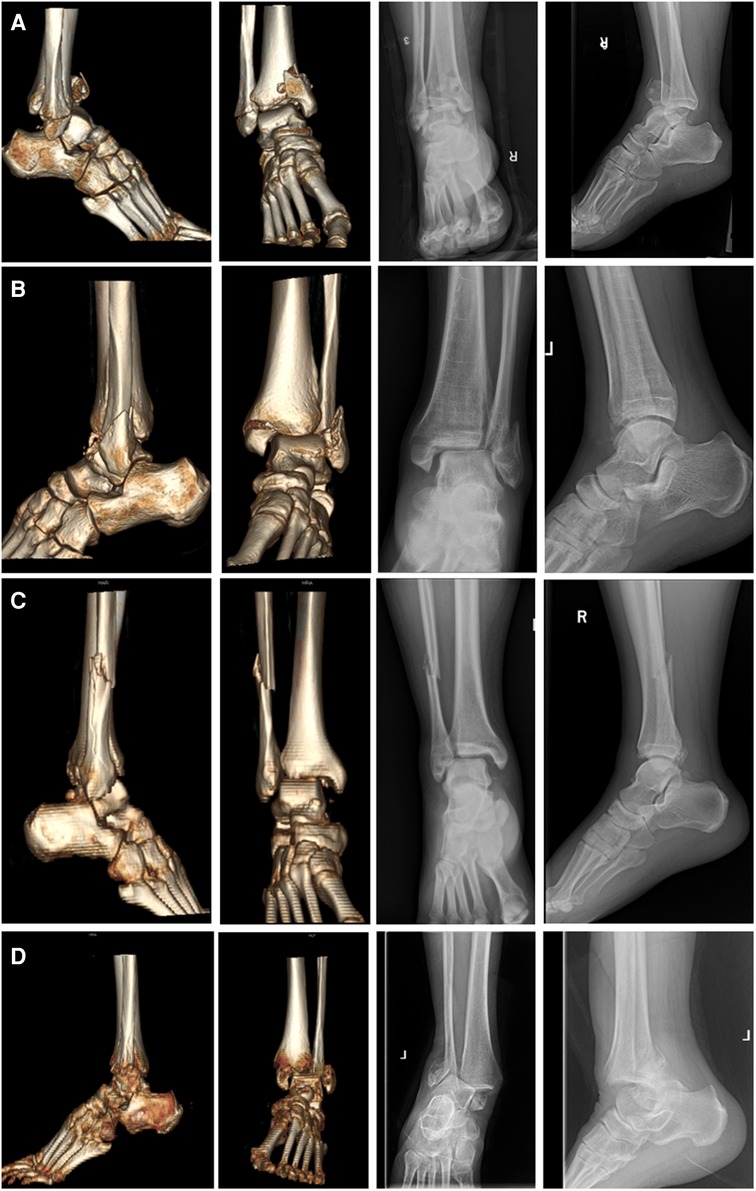
Figure 3. The CT reconstructions and radiographs of ankle fracture-dislocations with four different injury mechanisms according to the Lauge-Hansen's classification. (A) Supination-adduction; (B) Supination-external rotation; (C) Pronation abduction; (D) Pronation-external rotation.
In addition, it is clear that the AITFL will be the first to rupture. Since PITFL is a relatively strong ligament, its injury often takes the form of an avulsion posterior ankle fracture. Its deeper layer, the transverse ligament, forms a posterior labrum that limits the posterior displacement of talus, this results in a relatively rare posterior dislocation of talus. When the talus is extremely externally rotated, the injury to PTFL can occur and are essentially only seen in cases of ankle dislocation (47). The SER IV ankle fractures include either a rupture of the deltoid ligament or a medial ankle fracture, and a distinction needs to be made between these two different injuries when a dislocation occurs. Generally, the dislocation occurs only when there is a rupture of the deep portion of deltoid ligament (13).
As one of the most severely injured and intricate types of ankle fractures, a recent study has confirmed that trimalleolar fractures have a higher risk of dislocation (43). Biomechanical studies of trimalleolar fractures have found that contact stresses are concentrated on the articular cartilage (48). In addition to instability of the medial structures, ankle fracture-dislocations are also associated with larger posterior malleolar fragment (49). Posterior ankle malformations can lead to posterior lateral subluxation of the talus. In addition, the certain AITFL and PITFL injury and the underlying IOL injury in trimalleolar fractures contribute to instability of the syndesmosis. By reason of the foregoing, trimalleolar fractures are usually combined with injuries to the medial deltoid ligament as well as the syndesmosis, and the chances of dislocation are greatly increased with the addition of posterior ankle fractures.
The PER fractures are severe ankle injuries and account for approximately 14%–22% of all ankle fractures (42, 50). A recent study showed that about 41% of PER ankle fractures were dislocated. Unlike SER ankle fractures, the PER ankle fractures are first injured medially and the lateral fracture line is higher than the ankle plane. The injury of medial deltoid ligament will result in the talar instability (51, 52). A mechanical model study showed that when the deep deltoid ligament is ruptured, even if the fibula and syndesmosis were stable, the degree of external rotation in plantar flexion increases and the ankle dislocates at 20° to 30° plantar flexion, which also means that the talus will dislocate laterally. The most common types of dislocations in PER ankle fractures are the lateral dislocations (53). Noteworthily, when the syndesmosis injury is combined with deltoid ligament injury, the unstable talus rotates anterolaterally resulting in a decrease in tibiofibular joint contact area and an increase in intra-articular pressure, resulting in the subsequent dislocation (54). In general, the deltoid ligament, especially the deep deltoid ligament, is particularly important in the mechanism of dislocation in PER ankle fractures.
The other two uncommon types reveal relatively significant differences in dislocation rates. The probability of dislocation is 76% for the pronation-adduction (PAD) ankle fracture versus 5% for supination-adduction (SAD) ankle fracture (6). The greater violence of a PAD ankle fracture first damages the deltoid ligament, leading to the medial instability of ankle while the lateral structures of SAD ankle fracture are damaged first. Based on the previous analyses of mechanism, this is a situation in which the PAD ankle fractures are more likely to dislocate laterally. In contrast, the SAD ankle fractures can dislocate medially, but the probability of this occurring is relatively small.
Clinical classification
The ankle fracture-dislocations are consisted of the fractures with total dislocation and subluxation. According to the relationship between direction of talus displacement and ankle mortise, ankle dislocations are classified into five types, including the anterior, posterior, medial, lateral, superior or the combination of these directions. The anterior ankle dislocation is generally where the foot remains stable, the ankle is forced into dorsiflexion, and there is a backward force on the lower leg. Due to the anterior dislocation of the talus, the dorsalis pedis artery may be damaged as a result (6, 55–57). The posterior ankle dislocation is the most common type of the dislocation and is often associated with injury to the tibiofibular syndesmosis and lateral malleolus fracture. There is also a greater risk of the injury to the posterior tibial nerve and accompanying vascular structures (58, 59). The medial and lateral ankle dislocations usually result from the eversion and inversion due to high intensity violence. The posterior medial dislocation often destroys the nervi peroneus superficialis and its related branches. The superior dislocations often occur in the falling injury when the talus is driven up into the mortise, and results in joint diastasis, disrupting the syndesmosis and allowing for talar dislocation. The superior dislocation can occur with or without the associated fractures (2, 60, 61). Regarding this, Ramasamy et al. (62) classified the complete ankle dislocation into two types. Type I is a dislocation without medial ankle fracture, and the type II is a dislocation with the medial ankle fracture. This typing strategy highlights the impact of injury to the medial ankle structures on the outcome of ankle fracture-dislocations.
Treatment
Closed reduction and external fixation after reduction
Ankle fracture-dislocations may increase the risk of the injury to soft tissues surrounding ankle and overlying skin and consequently result in severe complications. The main indication for conducting a non-surgical closed reduction is ankle subluxation (63). Non-displaced fractures generally do not require closed reduction. It is best to obtain radiographs prior to closed reduction to understand the type and extent of the ankle injury (64). Generally, the reduction is usually accompanied with the appropriate analgesia and conscious sedation. Recently, the local hematoma block has also been recommended for the closed reduction of ankle fracture-dislocations. The hematoma block can provide a similar effect compared to the anesthesia without additional cardiovascular risk (15). Most of the time if neurovascular injury is clearly or highly suspected, the time of closed reduction should not be delayed due to x-ray. The primary goal of closed reduction is to reduce the impact of ankle fracture-dislocations on the skin and soft tissues.
External fixation is mainly the application of gypsum or splinting after the closed reduction. The ankle is usually immobilized in a neutral position to maintain the ankle stability and avoid contracture of Achilles tendon, and the care must be taken to avoid the skin compression when using the plaster fixation, especially in the elderly who can develop the severe skin ulcers as a result (65). In addition, compared to the temporary external fixators, a recent study found that in the patients with ankle fracture-dislocations who did not undergo emergency ORIF, splinting increased the risk of complications (such as re-dislocation and skin necrosis) (19). Hence, when a patient experiences the ankle fracture-dislocations, the extent of their ankle injury should be carefully evaluated and splinting should be used with caution.
Surgical timing
The surgical timing for ankle fractures is not yet definitive. Generally, the ankle will begin to swell continuously within 48 h after the fracture occurs, especially if the ankle is dislocated. Most surgeons are concerned about the skin complications associated with early surgery on an overly swollen ankle (66–68). Current German guidelines for ankle fractures recommend the surgery should be performed within 6–8 h, but these recommendations should also be revalidated in further prospective randomized studies. Several studies have indicated that the early surgery for ankle fractures can shorten the length of hospital stay (LHS), reduce the hospital costs, and increase the rate of anatomic reductions (69–73). A case-control study revealed that the effect of emergency surgery and elective surgery for ankle fracture-dislocations was roughly consistent, but the LHS of emergency surgery was shorter and the cost was less, which can relatively save the medical expenses of patients. In contrast, postoperative wound complications are a major concern for the surgeons. If the ankle joint is highly swollen and the skin develops the tension blisters, the risk of surgical incision infection and necrosis will increase due to the excessive tension. However, partial studies have indicated that the early surgery has lower infected wound complications and a better functional prognosis than delayed surgery (20, 66). Currently, there are still no related study focusing on the surgical timing for ankle fracture-dislocations, and further studies are still needed to support the idea of early surgery.
Surgical treatment
The purpose of ankle fracture surgery is to restore the fibula length and maintain the stable anatomical reduction. The treatment of open ankle fracture-dislocations focuses on avoiding the infection, reducing the rate of complications, promoting the bone healing and restoring the good function (74). The most common complications include deep infection (17%) and skin necrosis (18%) (75). An evidence-based study provides several guidelines for the surgical treatment of the open ankle fractures. In short, strong internal fixation should be given to restore the anatomy of the ankle fossa, and external fixation should be considered only if the soft tissue cannot cover the internal fixation. If the wound has no tension or needs to be opened for other purposes, the Grade I wound can be closed. Grade II wounds should wait for delayed closure or close after postoperative exclusion of infection. Grade III wounds should remain open and require postoperative skin grafting or flap treatment (76).
Ankle fracture-dislocations represent a more significant injury to the bony and soft-tissue structures of ankle joint. Thus, we need to focus on the treatment of periarticular ligament injuries in addition to ORIF routinely. Based on the previous analysis of the mechanism of injury, the ankle fracture-dislocations are usually combined with the syndesmotic injuries. Moreover, the instability of the syndesmotic complex may result in the long-term dysfunction and osteoarthritis (77). Although a prospective randomized study has revealed that the insertion of inferior tibiofibular screws is unnecessary in the SER-type ankle fractures (78). However, the current overwhelming opinion is that the insertion of syndesmosis screws is the gold standard when a syndesmotic injury has occurred (79, 80). The syndesmosis screws are typically inserted 2–3 cm above the articular surface and is angled approximately 20° anteromedially (81, 82). There is insufficient evidence for the early removal of syndesmosis screws and the sufficient time may be required to ensure the adequate recovery of syndesmotic complex (83–85). However, the prolonged insertion may result in the loss of repositioning or screw fracture. Hence, further studies are still needed to clarify the optimal insertion time and position. Besides, a variety of novel surgical instruments have been developed to replace the syndesmosis screws recently. Five meta-analyses have compared the efficacy of suture-button versus screws and confirmed the similar functional outcomes and postoperative complications in both groups (86–90). Another novel surgical instrument is the bioresorbable screws, which has the advantage of not requiring screw removal. Two latest meta-analyses suggested a higher complication rate of bioresorbable screws compared to syndesmosis screws, and the use of bioresorbable screws is not recommended (86, 90). In addition, dynamic fixation is another surgical device that can ensure an effective reduction. A study indicated that the dynamic fixation reduces the complications and improves clinical outcomes, with a lower risk of reoperation (91).
Judging by the mechanism of injury, the ankle fracture-dislocations are likely to be accompanied with the injury to medial deltoid ligament. It is worth being vigilant that 58.3% of acute ankle fractures were associated with the medial triangular ligament injury (92). Approximately 39.6% of ankle fracture-dislocations were associated with the rupture of deltoid ligament (93). Furthermore, the non-anatomic healing of deltoid ligament may result in the persistent medial pain and ankle instability, and even the risk of early arthritis. The most common surgical approach to repair the deltoid ligament is fixing the superficial deltoid ligament and the deep deltoid ligament on a suture anchor inserted in the medial ankle (94–97). Several retrospective studies did not recommend the additional deltoid ligament repair, since it can scar heal and eventually become a functional ligament (98–100). Other studies have indicated better outcomes in the deltoid repair group in terms of pain scores and functional scores during the follow-up (101–103). However, a randomized controlled trial reported that the deltoid ligament repair was not necessary when the fibular anatomy returned to normal. Although this trial had limitations such as no analysis of violence energy and no assessment of medial stability (104). In a recent Meta-analysis, the authors found that patients who repaired the deltoid ligament had better radiographic correction of the medial clear space and had relatively better pain scores (105). In summary, additional deltoid ligament repair surgery may be helpful in terms of repositioning results and pain scores in the early stages of recovery, but it also adds additional operative time and cost. A syndesmotic reduction could be much more significant than deltoid repair in restoring the mortise and keeping ankle stability.
Efficacy and prognosis
With the increasing demand for functional movement in modern society, more and more orthopaedic surgeons are currently concerned about the functional outcomes of ankle fracture-dislocations. A study on the prognosis of ankle fracture-dislocation found that the functional outcomes were worse in the open ankle fracture-dislocations. Talar cartilage injury after dislocation tends to be prone to arthrosis, and its prevalence increases with age (18). However, in a retrospective study analyzing mechanism and functional outcomes of dislocations according to the Lauge-Hansen classification, the investigators found that functional outcomes did not worsen in the mid-term, but the patients with dislocations were more likely to develop the reflex sympathetic dystrophy syndrome (6). Moreover, another analysis showed no increased wound complications but worse functional outcomes in the dislocation group, except for the lower pain scores (5). These results suggest that more detailed and precise studies need to be further implemented in the future. In the patients with SER IV ankle fractures, the dislocation is associated with worse radiographic and functional outcomes (3). Other than that, the dislocations may result in higher rates of articular malreduction and worse functional outcomes in patients with PER IV ankle fractures due to higher energy damage (4).
Conclusions
Ankle fracture-dislocations are mostly due to the high-energy violence and can be accompanied with varying amount of bone and soft tissue injury. Dislocation often leads to worse functional outcomes in ankle fractures. According to Lauge-Hansen's classification, the injury of the deep deltoid ligament is closely related to the injury mechanism of SER and PER ankle fractures. Conservative treatment is not recommended in the event of fracture-dislocation. In addition to conventional ORIF, syndesmotic fixation is also important while additional deltoid ligament repair is unnecessary. Collectively, the ankle fracture-dislocations still require a more comprehensive and clearer treatment guideline in the future, as well as the prognostic evaluation system.
Author contributions
MC, YZ, and YR developed the idea for this paper. MC, YZ and SH developed the search strategy and performed the systematic review and data extraction. MC and YZ wrote the manuscript and all authors edited and agreed the final version. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: finnish statistics during 1970–2000 and projections for the future. Bone. (2002) 31(3):430–3. doi: 10.1016/s8756-3282(02)00832-3
2. Wight L, Owen D, Goldbloom D, Knupp M. Pure ankle dislocation: a systematic review of the literature and estimation of incidence. Injury. (2017) 48(10):2027–34. doi: 10.1016/j.injury.2017.08.011
3. Sculco PK, Lazaro LE, Little MM, Berkes MB, Warner SJ, Helfet DL, et al. Dislocation is a risk factor for poor outcome after supination external rotation type ankle fractures. Arch Orthop Trauma Surg. (2016) 136(1):9–15. doi: 10.1007/s00402-015-2353-0
4. Warner SJ, Schottel PC, Hinds RM, Helfet DL, Lorich DG. Fracture-dislocations demonstrate poorer postoperative functional outcomes among pronation external rotation IV ankle fractures. Foot Ankle Int. (2015) 36(6):641–7. doi: 10.1177/1071100715572222
5. Tantigate D, Ho G, Kirschenbaum J, Bäcker HC, Asherman B, Freibott C, et al. Functional outcomes after fracture-dislocation of the ankle. Foot Ankle Spec. (2020) 13(1):18–26. doi: 10.1177/1938640019826701
6. Yaradilmis YU, Öğük C, Okkaoglu MC, Ateş A, Demirkale İ, Altay M. Injury mechanisms of ankle fractures with dislocation and analysis of differences on functional outcome. Ulus Travma Acil Cerrahi Derg. (2020) 26(5):818–25. doi: 10.14744/tjtes.2020.57034
7. Zhang YW, Rui YF. A systematic review of the “Logsplitter” injury: how much do we know? Injury. (2021) 52(3):358–65. doi: 10.1016/j.injury.2020.11.043
8. Russell S, Steers W, McVary KT. Systematic evidence-based analysis of plaque injection therapy for Peyronie's Disease. Eur Urol. (2007) 51(3):640–7. doi: 10.1016/j.eururo.2006.10.042
9. Tanoğlu O, Gökgöz MB, Özmeriç A, Alemdaroğlu KB. Two-stage surgery for the malleolar fracture-dislocation with severe soft tissue injuries does not affect the functional results. J Foot Ankle Surg. (2019) 58(4):702–5. doi: 10.1053/j.jfas.2018.11.033
10. Buyukkuscu MO, Basilgan S, Mollaomeroglu A, Misir A, Basar H. Splinting vs temporary external fixation in the initial treatment of ankle fracture-dislocations. Foot Ankle Surg. (2022) 28(2):235–39. doi: 10.1016/j.fas.2021.03.018
11. Martin CW, Ryan JC, Bullock TS, Cabot JH, Makhani AA, Griffin LP, et al. Surgical site complications in open pronation-abduction ankle fracture-dislocations with medial tension failure wounds. J Orthop Trauma. (2021) 35(12):e481–5. doi: 10.1097/bot.0000000000002128
12. Ye T, Chen A, Yuan W, Gou S. Management of grade III open dislocated ankle fractures: combined internal fixation with bioabsorbable screws/rods and external fixation. J Am Podiatr Med Assoc. (2011) 101(4):307–15. doi: 10.7547/1010307
13. Johnson DP, Hill J. Fracture-dislocation of the ankle with rupture of the deltoid ligament. Injury. (1988) 19(2):59–61. doi: 10.1016/0020-1383(88)90071-x
14. Fonkoue L, Sarr L, Muluem KO, Gueye AB, Dembele B, Fon C, et al. Early posttraumatic ankle osteoarthritis following ankle fracture-dislocations in a sub-Saharan African setting. Orthop Traumatol Surg Res. (2021) 107(6):102996. doi: 10.1016/j.otsr.2021.102996
15. White BJ, Walsh M, Egol KA, Tejwani NC. Intra-articular block compared with conscious sedation for closed reduction of ankle fracture-dislocations: a prospective randomized trial. J Bone Joint Surg Am. (2008) 90(4):731–4. doi: 10.2106/jbjs.G.00733
16. Baker JR, Patel SN, Teichman AJ, Bochat SE, Fleischer AE, Knight JM. Bivalved fiberglass cast compared with plaster splint immobilization for initial management of ankle fracture-dislocations: a treatment algorithm. Foot Ankle Spec. (2012) 5(3):160–7. doi: 10.1177/1938640012443283
17. Godsiff SP, Trakru S, Kefer G, Maniar RN, Flanagan JP, Tuite JD. A comparative study of early motion and immediate plaster splintage after internal fixation of unstable fractures of the ankle. Injury. (1993) 24(8):529–30. doi: 10.1016/0020-1383(93)90029-6
18. Yalın M, Aslantaş F, Duramaz A, Bilgili MG, Baca E, Koluman A. The common comorbidities leading to poor clinical outcomes after the surgical treatment of ankle fracture-dislocations. Ulus Travma Acil Cerrahi Derg. (2020) 26(6):943–50. doi: 10.14744/tjtes.2020.35392
19. Wawrose RA, Grossman LS, Tagliaferro M, Siska PA, Moloney GB, Tarkin IS. Temporizing external fixation vs splinting following ankle fracture dislocation. Foot Ankle Int. (2020) 41(2):177–82. doi: 10.1177/1071100719879431
20. Schepers T, De Vries MR, Van Lieshout EM, Van der Elst M. The timing of ankle fracture surgery and the effect on infectious complications; a case series and systematic review of the literature. Int Orthop. (2013) 37(3):489–94. doi: 10.1007/s00264-012-1753-9
21. Shibuya N, Davis ML, Jupiter DC. Epidemiology of foot and ankle fractures in the United States: an analysis of the National Trauma Data Bank (2007 to 2011). J Foot Ankle Surg. (2014) 53(5):606–8. doi: 10.1053/j.jfas.2014.03.011
22. Pretterklieber ML. Anatomy and kinematics of the human ankle joint. Radiologe. (1999) 39(1):1–7. doi: 10.1007/s001170050469
23. Yang NP, Chen HC, Phan DV, Yu IL, Lee YH, Chan CL, et al. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000–2005. BMC Musculoskelet Disord. (2011) 12:253. doi: 10.1186/1471-2474-12-253
24. Hindle P, Davidson EK, Biant LC, Court-Brown CM. Appendicular joint dislocations. Injury. (2013) 44(8):1022–7. doi: 10.1016/j.injury.2013.01.043
25. Ray RG. Arthroscopic anatomy of the ankle joint. Clin Podiatr Med Surg. (2016) 33(4):467–80. doi: 10.1016/j.cpm.2016.06.001
26. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. (2002) 37(4):364–75.12937557
27. van den Bekerom MP, Oostra RJ, Golanó P, van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat. (2008) 21(7):619–26. doi: 10.1002/ca.20703
28. Oh CS, Won HS, Hur MS, Chung IH, Kim S, Suh JS, et al. Anatomic variations and MRI of the intermalleolar ligament. AJR Am J Roentgenol. (2006) 186(4):943–7. doi: 10.2214/ajr.04.1784
29. Golanò P, Mariani PP, Rodríguez-Niedenfuhr M, Mariani PF, Ruano-Gil D. Arthroscopic anatomy of the posterior ankle ligaments. Arthroscopy. (2002) 18(4):353–8. doi: 10.1053/jars.2002.32318
30. Crim J. Medial-sided ankle pain: deltoid ligament and beyond. Magn Reson Imaging Clin N Am. (2017) 25(1):63–77. doi: 10.1016/j.mric.2016.08.003
31. Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int. (2016) 37(8):882–90. doi: 10.1177/1071100716643083
32. Campbell KJ, Michalski MP, Wilson KJ, Goldsmith MT, Wijdicks CA, LaPrade RF, et al. The ligament anatomy of the deltoid complex of the ankle: a qualitative and quantitative anatomical study. J Bone Joint Surg Am. (2014) 96(8):e62. doi: 10.2106/jbjs.M.00870
33. Sarsam IM, Hughes SP. The role of the anterior tibio-fibular ligament in talar rotation: an anatomical study. Injury. (1988) 19(2):62–4. doi: 10.1016/0020-1383(88)90072-1
34. Littlechild J, Mayne A, Harrold F, Chami G. A cadaveric study investigating the role of the anterior inferior tibio-fibular ligament and the posterior inferior tibio-fibular ligament in ankle fracture syndesmosis stability. Foot Ankle Surg. (2020) 26(5):547–50. doi: 10.1016/j.fas.2019.06.009
35. Bartonícek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. (2003) 25(5-6):379–86. doi: 10.1007/s00276-003-0156-4
36. Taylor DC, Englehardt DL, Bassett FH 3rd. Syndesmosis sprains of the ankle. The influence of heterotopic ossification. Am J Sports Med. (1992) 20(2):146–50. doi: 10.1177/036354659202000209
37. Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI Findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. (2004) 182(1):131–6. doi: 10.2214/ajr.182.1.1820131
38. Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int. (2007) 28(5):602–4. doi: 10.3113/fai.2007.0602
39. Clanton TO, Williams BT, Backus JD, Dornan GJ, Liechti DJ, Whitlow SR, et al. Biomechanical analysis of the individual ligament contributions to syndesmotic stability. Foot Ankle Int. (2017) 38(1):66–75. doi: 10.1177/1071100716666277
40. Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma. (2006) 20(4):267–72. doi: 10.1097/00005131-200604000-00006
41. Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Joint Surg Br. (1965) 47(4):634–60. doi: 10.1302/0301-620X.47B4.634
42. Jensen SL, Andresen BK, Mencke S, Nielsen PT. Epidemiology of ankle fractures: a prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand. (1998) 69(1):48–50. doi: 10.3109/17453679809002356
43. Pina G, Fonseca F, Vaz A, Carvalho A, Borralho N. Unstable malleolar ankle fractures: evaluation of prognostic factors and sports return. Arch Orthop Trauma Surg. (2021) 141(1):99–104. doi: 10.1007/s00402-020-03650-w
44. Guise ER. Rotational ligamentous injuries to the ankle in football. Am J Sports Med. (1976) 4(1):1–6. doi: 10.1177/036354657600400101
45. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. (1991) 19(3):294–8. doi: 10.1177/036354659101900315
46. Edwards GS Jr, DeLee JC. Ankle diastasis without fracture. Foot Ankle. (1984) 4(6):305–12. doi: 10.1177/107110078400400606
47. Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. (2010) 18(5):557–69. doi: 10.1007/s00167-010-1100-x
48. Fitzpatrick DC, Otto JK, McKinley TO, Marsh JL, Brown TD. Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma. (2004) 18(5):271–8. doi: 10.1097/00005131-200405000-00002
49. De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. (2005) 44(3):211–7. doi: 10.1053/j.jfas.2005.02.002
50. Bauer M, Jonsson K, Nilsson B. Thirty-year follow-up of ankle fractures. Acta Orthop Scand. (1985) 56(2):103–6. doi: 10.3109/17453678508994329
51. Lee S, Lin J, Hamid KS, Bohl DD. Deltoid ligament rupture in ankle fracture: diagnosis and management. J Am Acad Orthop Surg. (2019) 27(14):e648–58. doi: 10.5435/jaaos-d-18-00198
52. Harper MC. An anatomic study of the short oblique fracture of the distal fibula and ankle stability. Foot Ankle. (1983) 4(1):23–9. doi: 10.1177/107110078300400106
53. Frank A. L., Charette R. S. and Groen K.: Ankle dislocation. In: Statpearls. StatPearls Publishing Copyright © 2022, Treasure Island (FL): StatPearls Publishing LLC., (2022) 1–17.
54. Michelson JD, Waldman B. An axially loaded model of the ankle after pronation external rotation injury. Clin Orthop Relat Res. (1996) 328:285–93. doi: 10.1097/00003086-199607000-00043
55. Georgilas I, Mouzopoulos G. Anterior ankle dislocation without associated fracture: a case with an 11 year follow-up. Acta Orthop Belg. (2008) 74(2):266–9.18564487
56. Karampinas PK, Stathopoulos IP, Vlamis J, Polyzois VD, Pneumatikos SG. Conservative treatment of an anterior-lateral ankle dislocation without an associated fracture in a diabetic patient: a case report. Diabet Foot Ankle. (2012) 3. doi: 10.3402/dfa.v3i0.18411
57. Segal LS, Lynch CJ, Stauffer ES. Anterior ankle dislocation with associated trigonal process fracture. A case report and literature review. Clin Orthop Relat Res. (1992) 1992(278):171–6.
58. Bois AJ, Dust W. Posterior fracture dislocation of the ankle: technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma. (2008) 22(9):629–36. doi: 10.1097/BOT.0b013e318184ba4e
59. Lampridis V, Gougoulias N, Sakellariou A. Stability in ankle fractures: diagnosis and treatment. EFORT Open Rev. (2018) 3(5):294–303. doi: 10.1302/2058-5241.3.170057
60. Shaik MM, Tandon T, Agrawal Y, Jadhav A, Taylor LJ. Medial and lateral rotatory dislocations of the ankle after trivial trauma–pathomechanics and management of two cases. J Foot Ankle Surg. (2006) 45(5):346–50. doi: 10.1053/j.jfas.2006.05.002
61. Wight L, Owen D, James D. Pure ankle dislocation: management with early weight bearing and mobilization. ANZ J Surg. (2017) 87(6):520–2. doi: 10.1111/ans.12958
62. Ramasamy P, Ward A. Distal tibiofibular joint dislocation with an intact fibula: a classification system. Injury. (2003) 34(11):862–5. doi: 10.1016/s0020-1383(01)00193-0
63. Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. (1950) 60(5):957–85. doi: 10.1001/archsurg.1950.01250010980011
64. von Keudell AG, Rajab TK, Vrahas MS, Rodriguez EK, Harris MB, Weaver MJ. Closed reduction of a fractured and dislocated ankle. N Engl J Med. (2019) 381(12):e25. doi: 10.1056/NEJMvcm1511693
65. Halanski MA, Halanski AD, Oza A, Vanderby R, Munoz A, Noonan KJ. Thermal injury with contemporary cast-application techniques and methods to circumvent morbidity. J Bone Joint Surg Am. (2007) 89(11):2369–77. doi: 10.2106/jbjs.F.01208
66. Høiness P, Strømsøe K. The influence of the timing of surgery on soft tissue complications and hospital stay. A review of 84 closed ankle fractures. Ann Chir Gynaecol. (2000) 89(1):6–9.
67. Phillips WA, Schwartz HS, Keller CS, Woodward HR, Rudd WS, Spiegel PG, et al. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. (1985) 67(1):67–78. doi: 10.2106/00004623-198567010-00010
68. Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am. (2012) 94(22):2047–52. doi: 10.2106/jbjs.K.01088
69. Breederveld RS, van Straaten J, Patka P, van Mourik JC. Immediate or delayed operative treatment of fractures of the ankle. Injury. (1988) 19(6):436–8. doi: 10.1016/0020-1383(88)90142-8
70. James LA, Sookhan N, Subar D. Timing of operative intervention in the management of acutely fractured ankles and the cost implications. Injury. (2001) 32(6):469–72. doi: 10.1016/s0020-1383(00)00254-0
71. Pietzik P, Qureshi I, Langdon J, Molloy S, Solan M. Cost benefit with early operative fixation of unstable ankle fractures. Ann R Coll Surg Engl. (2006) 88(4):405–7. doi: 10.1308/003588406(106504
72. Singh RA, Trickett R, Hodgson P. Early versus late surgery for closed ankle fractures. J Orthop Surg (Hong Kong). (2015) 23(3):341–4. doi: 10.1177/230949901502300317
73. Porter DA, May BD, Berney T. Functional outcome after operative treatment for ankle fractures in young athletes: a retrospective case series. Foot Ankle Int. (2008) 29(9):887–94. doi: 10.3113/fai.2008.0887
74. Olerud S, Karlstrom G, Danckwardt-Lillieström G. Treatment of open fractures of the tibia and ankle. Clin Orthop Relat Res. (1978) 1978(136):212–24.
75. Ovaska MT, Madanat R, Honkamaa M, Mäkinen TJ. Contemporary demographics and complications of patients treated for open ankle fractures. Injury. (2015) 46(8):1650–5. doi: 10.1016/j.injury.2015.04.015
76. Hulsker CC, Kleinveld S, Zonnenberg CB, Hogervorst M, van den Bekerom MP. Evidence-based treatment of open ankle fractures. Arch Orthop Trauma Surg. (2011) 131(11):1545–53. doi: 10.1007/s00402-011-1349-7
77. Hunt KJ, George E, Harris AH, Dragoo JL. Epidemiology of syndesmosis injuries in intercollegiate football: incidence and risk factors from National Collegiate Athletic Association injury surveillance system data from 2004–2005 to 2008–2009. Clin J Sport Med. (2013) 23(4):278–82. doi: 10.1097/JSM.0b013e31827ee829
78. Kortekangas TH, Pakarinen HJ, Savola O, Niinimäki J, Lepojärvi S, Ohtonen P, et al. Syndesmotic fixation in supination-external rotation ankle fractures: a prospective randomized study. Foot Ankle Int. (2014) 35(10):988–95. doi: 10.1177/1071100714540894
79. de-Las-Heras Romero J, Alvarez AML, Sanchez FM, Garcia AP, Porcel PAG, Sarabia RV, et al. Management of syndesmotic injuries of the ankle. EFORT Open Rev. (2017) 2(9):403–9. doi: 10.1302/2058-5241.2.160084
80. van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, Ciuffreda M, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. (2016) 24(4):1200–16. doi: 10.1007/s00167-015-3942-8
81. Albers GH, de Kort AF, Middendorf PR, van Dijk CN. Distal tibiofibular synostosis after ankle fracture. A 14-year follow-up study. J Bone Joint Surg Br. (1996) 78(2):250–2. doi: 10.1302/0301-620X.78B2.0780250
82. McBryde A, Chiasson B, Wilhelm A, Donovan F, Ray T, Bacilla P. Syndesmotic screw placement: a biomechanical analysis. Foot Ankle Int. (1997) 18(5):262–6. doi: 10.1177/107110079701800503
83. Walley KC, Hofmann KJ, Velasco BT, Kwon JY. Removal of hardware after syndesmotic screw fixation: a systematic literature review. Foot Ankle Spec. (2017) 10(3):252–7. doi: 10.1177/1938640016685153
84. Dingemans SA, Rammelt S, White TO, Goslings JC, Schepers T. Should syndesmotic screws be removed after surgical fixation of unstable ankle fractures? A systematic review. Bone Joint J. (2016) 98-b(11):1497–504. doi: 10.1302/0301-620x.98b11.Bjj-2016-0202.R1
85. Yu GS, Lin YB, Xiong GS, Xu HB, Liu YY. Diagnosis and treatment of ankle syndesmosis injuries with associated interosseous membrane injury: a current concept review. Int Orthop. (2019) 43(11):2539–47. doi: 10.1007/s00264-019-04396-w
86. Chen B, Chen C, Yang Z, Huang P, Dong H, Zeng Z. To compare the efficacy between fixation with tightrope and screw in the treatment of syndesmotic injuries: a meta-analysis. Foot Ankle Surg. (2019) 25(1):63–70. doi: 10.1016/j.fas.2017.08.001
87. Lee JS, Curnutte B, Pan K, Liu J, Ebraheim NA. Biomechanical comparison of suture-button, bioabsorbable screw, and metal screw for ankle syndesmotic repair: a meta-analysis. Foot Ankle Surg. (2021) 27(2):117–22. doi: 10.1016/j.fas.2020.03.008
88. Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskelet Disord. (2017) 18(1):286. doi: 10.1186/s12891-017-1645-7
89. Wang C, Ma X, Wang X, Huang J, Zhang C, Chen L. Internal fixation of distal tibiofibular syndesmotic injuries: a systematic review with meta-analysis. Int Orthop. (2013) 37(9):1755–63. doi: 10.1007/s00264-013-1999-x
90. Onggo JR, Nambiar M, Phan K, Hickey B, Ambikaipalan A, Hau R, et al. Suture button versus syndesmosis screw constructs for acute ankle diastasis injuries: a meta-analysis and systematic review of randomised controlled trials. Foot Ankle Surg. (2020) 26(1):54–60. doi: 10.1016/j.fas.2018.11.008
91. van der Eng DM, Schep NW, Schepers T. Bioabsorbable versus metallic screw fixation for tibiofibular syndesmotic ruptures: a meta-analysis. J Foot Ankle Surg. (2015) 54(4):657–62. doi: 10.1053/j.jfas.2015.03.014
92. Grassi A, Samuelsson K, D'Hooghe P, Romagnoli M, Mosca M, Zaffagnini S, et al. Dynamic stabilization of syndesmosis injuries reduces complications and reoperations as compared with screw fixation: a meta-analysis of randomized controlled trials. Am J Sports Med. (2020) 48(4):1000–13. doi: 10.1177/0363546519849909
93. Jeong MS, Choi YS, Kim YJ, Kim JS, Young KW, Jung YY. Deltoid ligament in acute ankle injury: MR imaging analysis. Skeletal Radiol. (2014) 43(5):655–63. doi: 10.1007/s00256-014-1842-5
94. Hintermann B, Regazzoni P, Lampert C, Stutz G, Gächter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. (2000) 82(3):345–51. doi: 10.1302/0301-620x.82b3.10064
95. Lack W, Phisitkul P, Femino JE. Anatomic deltoid ligament repair with anchor-to-post suture reinforcement: technique tip. Iowa Orthop J. (2012) 32:227–30.23576946
96. Woo SH, Bae SY, Chung HJ. Short-term results of a ruptured deltoid ligament repair during an acute ankle fracture fixation. Foot Ankle Int. (2018) 39(1):35–45. doi: 10.1177/1071100717732383
97. Yu GR, Zhang MZ, Aiyer A, Tang X, Xie M, Zeng LR, et al. Repair of the acute deltoid ligament complex rupture associated with ankle fractures: a multicenter clinical study. J Foot Ankle Surg. (2015) 54(2):198–202. doi: 10.1053/j.jfas.2014.12.013
98. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in national football league players. Foot Ankle Int. (2015) 36(11):1272–8. doi: 10.1177/1071100715593374
99. de Souza LJ, Gustilo RB, Meyer TJ. Results of operative treatment of displaced external rotation-abduction fractures of the ankle. J Bone Joint Surg Am. (1985) 67(7):1066–74. doi: 10.2106/00004623-198567070-00010
100. Zeegers AV, van der Werken C. Rupture of the deltoid ligament in ankle fractures: should it be repaired? Injury. (1989) 20(1):39–41. doi: 10.1016/0020-1383(89)90043-0
101. Tourne Y, Charbel A, Picard F, Montbarbon E, Saragaglia D. Surgical treatment of bi- and trimalleolar ankle fractures: should the medial collateral ligament be sutured or not? J Foot Ankle Surg. (1999) 38(1):24–9. doi: 10.1016/s1067-2516(99)80084-2
102. Baird RA, Jackson ST. Fractures of the distal part of the fibula with associated disruption of the deltoid ligament. Treatment without repair of the deltoid ligament. J Bone Joint Surg Am. (1987) 69(9):1346–52. doi: 10.2106/00004623-198769090-00007
103. Maynou C, Lesage P, Mestdagh H, Butruille Y. Is surgical treatment of deltoid ligament rupture necessary in ankle fractures? Rev Chir Orthop Reparatrice Appar Mot. (1997) 83(7):652–7.9515134
104. Bluman EM. Deltoid ligament injuries in ankle fractures: should I leave it or fix it? Foot Ankle Int. (2012) 33(3):236–8. doi: 10.3113/fai.2012.0236
Keywords: ankle fracture-dislocations, injury mechanism, complications, functional outcomes, management
Citation: Cao M, Zhang Y, Hu S and Rui Y (2022) A systematic review of ankle fracture-dislocations: Recent update and future prospects. Front. Surg. 9:965814. doi: 10.3389/fsurg.2022.965814
Received: 10 June 2022; Accepted: 25 July 2022;
Published: 9 August 2022.
Edited by:
Angelo Gabriele Aulisa, Bambino Gesù Children's Hospital (IRCCS), ItalyReviewed by:
Jianfeng Xue, Shanghai Jiao Tong University, ChinaJunlin Zhou, Capital Medical University, China
© 2022 Cao, Zhang, Hu and Rui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun-Feng Rui cnVpeXVuZmVuZ0AxMjYuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Mu-Min Cao1,2,3,4,†
Mu-Min Cao1,2,3,4,† Yuan-Wei Zhang
Yuan-Wei Zhang Yun-Feng Rui
Yun-Feng Rui