
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 02 September 2022
Sec. Thoracic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.953989
This article is part of the Research Topic Case Reports in Thoracic Surgery: 2021 View all 11 articles
Introduction: Primary pleural squamous cell carcinoma (PPSCC) is a sporadic disease that is rarely reported in the literature. Due to its low incidence, the pathogenesis of PPSCC is unknown.
Case summary: We report a case of a 68-year-old male with PPSCC and sizable pulmonary bullae. Two months after complete resection of both lesions, a total dose of 50 Gy radiotherapy was administered over the operative field. After more than a year of follow-up, the patient is in steady condition without any sign of recurrence.
Conclusion: Since PPSCC is rarely reported, our case proposed that complete surgical resection combined with radiotherapy may be a promising therapeutic approach.
Among epithelial tumors derived from the pleura, the most common are mesothelial tumors such as malignant mesothelioma (1). However, there is a rarely reported epithelial tumor that originates from the pleura—primary pleural squamous cell carcinoma (PPSCC) (2). Very few case reports have reported the incidence of this disease, and its pathogenic mechanism is poorly understood (3, 4). Therefore, there is no standard treatment for PPSCC. Herein, we report on a patient with a PPSCC case accompanied by pulmonary bullae, who completely recovered after receiving complete resection and radiotherapy. Our report will provide a reference for the treatment of PPSCC combined with pulmonary bullae.
A 68-year-old male complained of right-sided chest pain for 4 months with no other symptoms. He did not have history of echinococcosis, tumor, or tuberculosis. However, he had been smoking 20 cigaretes and drinking 100 g of alcohol daily for 40 years. Physical examination revealed no relevant findings. Routine blood and urine tests showed no anemia or proteinuria, respectively. Computed tomography (CT) revealed thickened pleura on the right anterolateral aspect of the chest wall, a soft tissue mass adjacent to the chest wall surrounding part of the 3rd and 4th ribs, a big pulmonary bulla with a size of 4.4 cm × 5.1 cm, and normal mediastinal lymph nodes (Figures 1A–C). We recommended PET/CT to the patient, who declined due to financial reasons. No positive lesion was found after a series of examinations were performed, including cranial magnetic resonance imaging (MRI), contrast-enhanced neck and abdominal CT scans, bronchoscopy, and whole body radionuclide bone scintigraphy. Because all these examinations did not reveal any evidence of regional or distant spread, invasive staging of the mediastinum by mediastinoscopy or of the pleural space by video-thoracoscopy was not indicated. The initial diagnosis was localized mesothelioma with pulmonary bulla. The lesion was deemed completely resectable, and the patient underwent right thoracotomy through the third intercostal space. The intraoperative exploration revealed that the mass of the subcutaneous tissue had a size of 4 cm × 5 cm, accompanied by a pleural lesion with a size of 5 cm × 6 cm. The internal margin of the lesion was attached to the edge of a small part of the adjacent bulla, but the wall of most of the remaining bulla was intact. Intraoperative frozen biopsy of the mass reported a malignant tumor, compatible with squamous cell carcinoma. Therefore, the tumor and bullae were entirely removed. The resection included the chest wall, part of the third and fourth ribs, tissues of the intercostal space and pleura, and a wedge resection of the pulmonary bulla. Appropriate nickel–titanium memory alloy embracing device was fixed on the third and fourth rib stumps to avoid the local collapse of the chest wall. The postoperative histopathological examination confirmed that the tumor was a squamous cell carcinoma that had invaded the adjacent ribs. The wall of the pulmonary bulla showed chronic inflammation (Figures 2A–D). The immunohistochemistry staining showed positive results of P63 and P40 and negative results of TTF1, napsin A, WT1, D2-40, c-kit, and calretinin (Figures 2E,F). Because there were no signs of tumor in other organs, such as lung, mediastinum, head, neck, and abdomen, it was diagnosed as a primary pleural tumor (5). There were no postoperative complications. Two months after the surgery, the patient returned and received radiotherapy over the operative field, with a total dose of 50 Gy. After more than a year of follow-up, no sign of tumor recurrence was detected (Figures 1D–F). The patient was satisfied to our treatment.
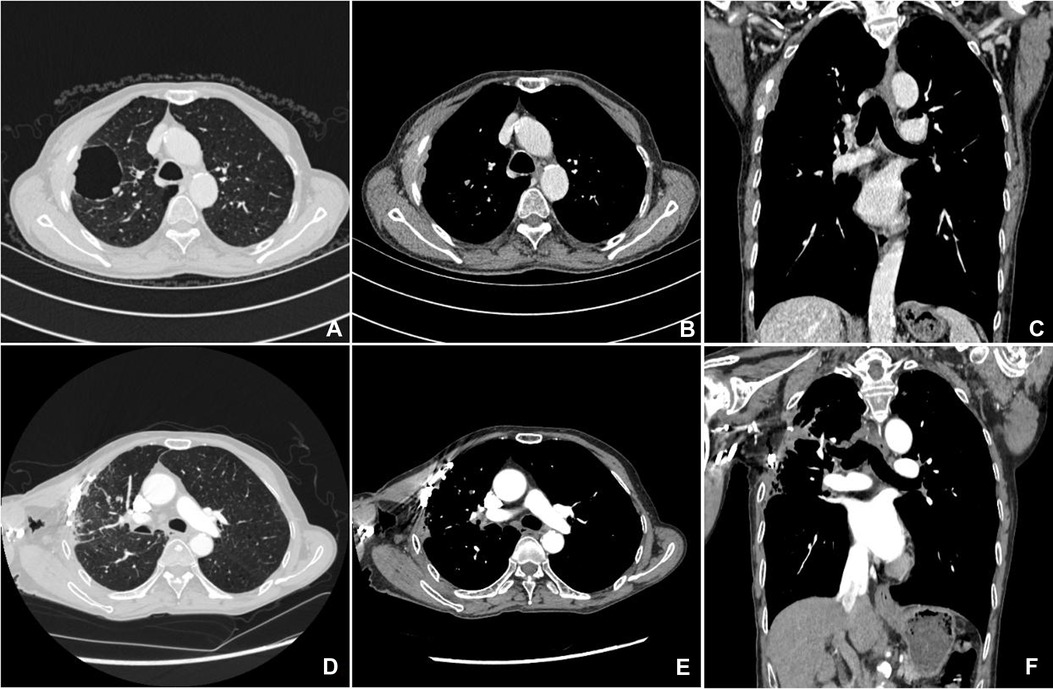
Figure 1. Preoperative chest CT scan (A–C); postoperative chest CT scan after more than a year of follow-up (D–F).
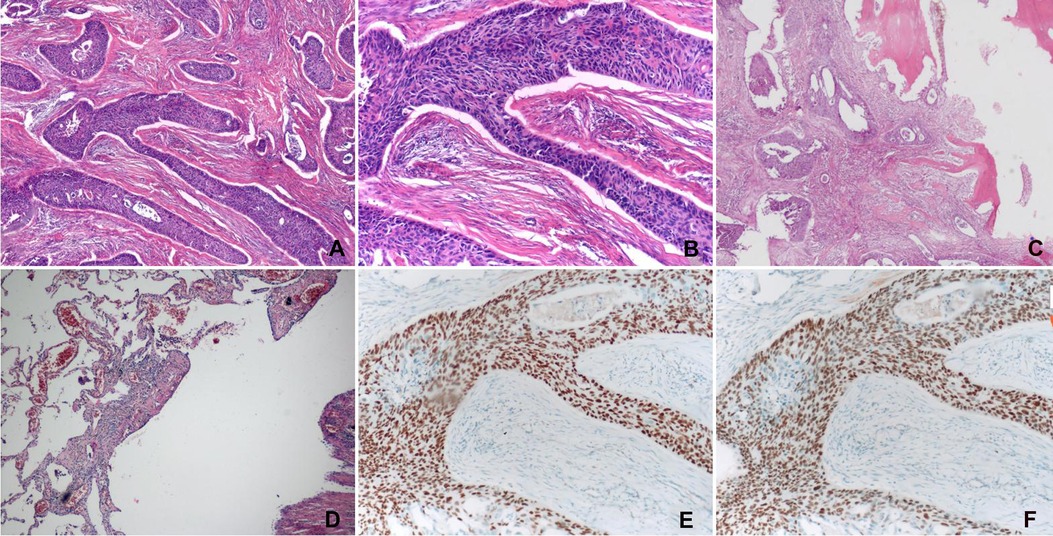
Figure 2. (A) The neoplastic cells were arranged in the form of nests with different sizes and showed various intercellular bridges (H&E stain, magnification ×40). (B) The cells were round or ovoid, with abundant cytoplasm, large nuclei, apparent nucleoli, and intracellular keratinization in focal areas (H&E stain, magnification ×100). (C) Squamous cell carcinoma invading the adjacent ribs (H&E stain, magnification ×40). (D) Pulmonary bullae with chronic inflammation (H&E stain, magnification ×40). (E,F) Immunohistochemical staining of neoplastic cells was performed with the use of antisera against p40 and p63, respectively, which showed evident nuclear positivity for both (E) p40 and (F) p63.
PPSCC is an extremely rare disease, with sporadic cases reported in the literature. Due to its low incidence, the pathogenesis of PPSCC remains largely unknown (4). Emerging evidence indicated that inflammation played a critical role in tumorigenesis (6). When tissues have chronic inflammation, the susceptibility to cancer will be promoted. In contrast, the long-term application of non-steroidal anti-inflammatory drugs will decrease the risk of several cancers (7). Previous studies suggested that chronic inflammation may be a pathogenic factor for PPSCC, which was supported by the fact that some patients with PPSCC had empyema, pleurocutaneous fistula (8), extrapleural pneumothorax without fistula in the treatment of tuberculosis (8), tuberculosis (9), or bronchopleural fistula caused by bronchiectasis (10). In this case, the presence of a pulmonary bulla with chronic inflammation in the vicinity of the tumor might promote neoplastic changes of the adjacent pleura, resulting in the development of squamous cell carcinoma. However, we are aware that this finding may be simply coincidental in our patient. Meanwhile, genetic deficiency may also account for the occurrence of PPSCC. Yoshida et al. reported that a 33-year-old female with extensive PPSCC had a deficiency of SMARCB1/INI1 gene, which was a tumor suppressor gene. The loss of SMARCB1 was associated with malignant tumors of the kidney, gastrointestinal tract, pancreas, and uterus (5). As for the diagnosis of PPSCC, there are no symptom which is specific for PPSCC. CT or PET–CT are typical approaches for the diagnosis of PPSCC. The preoperative biopsy using transthoracic Tru-Cut needle biopsy, is an approach for the diagnosis of pleural tumors. However, the diagnostic accuracy rate is not satisfactory (3). In this case, the differential diagnosis included focal mesothelioma, primary or secondary chest wall tumors, pleural metastasis, and thymic carcinoma, among which mesothelioma had the highest incidence rate. However, this potential was excluded by the diffuse expression of p40 and p63 and the negative expression of WT1, calretinin, and D2-40 in the tumor (4, 5, 11). Besides, primary chest wall tumors arise from muscle, fat, blood vessel, nerve sheath, cartilage, or bone of the chest wall. Therefore, the postoperative histopathological report of squamous cell carcinoma excluded the possibility of primary chest wall tumors. Furthermore, there was no tumor history and radiological evidence indicating that this tumor originated from lung, mediastinum, head, neck, or abdomen. Therefore, secondary chest wall tumors and pleural metastasis were further excluded. Although most thymic carcinomas were found to be squamous cell carcinoma, the tumor in the present case did not locate in the mediastinum and lacked the expression of CD117 (c-kit) that was a highly specific biomarker for thymic cancer (5). Consequently, we made the diagnosis of PPSCC.
Resection is a recommended approach for local tumors (4). Rüttner et al. reported that two PPSCC patients received surgery and were free of disease for 3 and 5 years after the operation, respectively (8). On the other hand, Prabhakar et al. reported that one PPSCC patient died from massive hemorrhage 5 months after resection. However, local or distant tumor recurrence could not be ruled out since necropsy was not performed (10). Sigala et al. reported that a patient with extensive PPSCC was treated with nivolumab after six cycles of cisplatinum and docetaxel combined with regional radiotherapy. Even though some tumor responses were observed, the tumor progressed locally and distantly, and the patient died 2 years after diagnosis (12). Besides, Yoshida et al. reported that a patient with extensive PPSCC died 10 months after diagnosis even treated with intensive chemotherapy (5). Therefore, chemotherapy might not be efficacious for PPSCC. In this case, the patient received complete resection and radiotherapy, and the follow-up indicated no tumor recurrence. Although no evidence suggested that radiotherapy could improve the prognosis of patients with PPSCC, our case report suggest that the combination of resection and adjuvant radiotherapy may be useful in the management of these patients.
We reported a rare case of PPSCC combined with pulmonary bulla in an elderly patient. Complete surgical resection combined with radiotherapy achieved more than 1 year of disease-free survival, which may provide a reference for the treatment of PPSCC.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ethics Committee of Suining Central Hospital. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the patient for the publication of any potentially identifiable images or data included in this article.
Conceptualization: CZ; writing—original draft: CZ, HZ, and YZ; writing—review and editing: RR-P and CZ. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Galateau-Salle F, Churg A, Roggli V, Travis W.D, The World Health Organization committee for Tumors of the Pleura. The 2015 World Health Organization classification of tumors of the pleura: advances since the 2004 classification. J Thorac Oncol. (2016) 11(2):142–54. doi: 10.1016/j.jtho.2015.11.005
2. Franke M, Chung HD, Johnson FE. Squamous cell carcinoma arising from the pleura after pneumonectomy for squamous cell carcinoma of the lung. Am J Surg. (2010) 199:e34–5. doi: 10.1016/j.amjsurg.2009.05.004
3. Lin XM, Chi C, Chen J, Liu Y, Li P, Yang Y. Primary pleural squamous cell carcinoma misdiagnosed as localized mesothelioma: a case report and review of the literature. J Cardiothorac Surg. (2013) 8:50. doi: 10.1186/1749-8090-8-50
4. Ronchi A, Cozzolino I, Montella M, Vicidomini G, Morgillo F, Della Corte C M, et al. Primary pleural squamous cell carcinoma: a diagnostic challenge. Cytopathology. (2018) 29:205–7. doi: 10.1111/cyt.12498
5. Yoshida K, Fujiwara Y, Goto Y, Kohno T, Yoshida A, Tsuta K, et al. The first case of SMARCB1 (INI1)-deficient squamous cell carcinoma of the pleura: a case report. BMC Cancer. (2018) 18:398. doi: 10.1186/s12885-018-4321-x
6. Balkwill F, Coussens LM. Cancer: an inflammatory link. Nature. (2004) 431(7007):405–6. doi: 10.1038/431405a
7. Gupta RA, Dubois RN. Colorectal cancer prevention and treatment by inhibition of cyclooxygenase-2. Nat Rev Cancer. (2001) 1(1):11–21. doi: 10.1038/35094017
8. Rüttner JR, Heinzl S. Squamous-cell carcinoma of the pleura. Thorax. (1977) 32:497–500. doi: 10.1136/thx.32.4.497
9. Garty I, Straussberg R, Flatau E. Extraosseous 99mTc-MDP uptake in squamous cell carcinoma of the pleura. Eur J Nucl Med. (1987) 12:589–91. doi: 10.1007/BF00284531
10. Prabhakar G, Mitchell IM, Guha T, Norton R. Squamous cell carcinoma of the pleura following bronchopleural fistula. Thorax. (1989) 44:1053–4. doi: 10.1136/thx.44.12.1053
11. Ordóñez NG. Application of immunohistochemistry in the diagnosis of epithelioid mesothelioma: a review and update. Hum Pathol. (2013) 44(1):1–19. doi: 10.1016/j.humpath.2012.05.014
Keywords: primary pleural squamous cell carcinoma, surgical resection, radiotherapy, pulmonary bullae, a promising therapeutic approach
Citation: Zhong C, Zhou H, Rami-Porta R and Zhao Y (2022) Case report: Primary pleural squamous cell carcinoma in a 68-year-old male. Front. Surg. 9:953989. doi: 10.3389/fsurg.2022.953989
Received: 26 May 2022; Accepted: 26 July 2022;
Published: 2 September 2022.
Edited by:
Nuria Maria Novoa, University of Salamanca Health Care Complex, SpainReviewed by:
Maria Teresa Gomez Hernandez, University of Salamanca, Spain© 2022 Zhong, Zhou, Rami-Porta and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuan Zhong emNodWFuaGFwcHlAMTI2LmNvbQ==
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.