- Department of Urology Surgery, Shunyi Hospital, Beijing, China
Objective: This study aims to compare the efficacy of plasma kinetic loop resection of the prostate (PKRP) and transurethral vaporization of the prostate (TUVP) for the treatment of high-risk benign prostatic hyperplasia (BPH), and analyze the influence of the related factors on the operation of BPH.
Methods: A total of 108 high-risk BPH patients diagnosed in our hospital from March 2018 to September 2021 were selected and randomly divided into an observation group and a control group, with 54 cases in each group. The control group was treated with TUVP, and the observation group was treated with PKRP. The international prostate symptom score (IPSS), quality of life (QOL) index, maximum urine flow rate (Qmax), and residual urine volume (RU) were observed before and after treatment. The general information such as age, educational level, residence, and residence status of the patient, as well as clinical information such as surgical method, nocturia frequency, preoperative IPSS score, RU, medical history, and prostate texture, were also recorded. All patients were followed up for 1 month, and complications were recorded.
Results: The IPSS score, QOL score, and RU of patients in the two groups were lower after treatment than those before treatment, and the Qmax was higher than that before treatment (P < 0.05). The IPSS score, QOL score, and RU of the observation group were lower than those of the control group, and the Qmax was higher than that of the control group (P < 0.05). The incidence of postoperative complications in the observation group was lower than in the control group (P < 0.05). Univariate analysis showed that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, medical history, and prostatic texture all could affect the postoperative condition of patients with BPH (P < 0.05). Multivariate logistic analysis showed that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, and medical history were the independent influencing factors of the postoperative condition of patients with BPH (P < 0.05).
Conclusion: PKRP in the treatment of high-risk BPH patients can effectively reduce the IPSS score, QOL score, and RU and significantly increase Qmax, with fewer complications and a good prognosis. Patients’ postoperative recovery was related to their age, surgical method, nocturia frequency, preoperative IPSS score, RU, and medical history. Therefore, choosing PKRP to treat high-risk BPH patients can effectively improve the postoperative urethral functional recovery of patients and reduce the occurrence of complications.
Introduction
Benign prostatic hyperplasia (BPH) is a urological disease commonly occurring in middle-aged and elderly men, which manifests as lower urinary tract symptoms caused by enlarged prostate glands and outlet obstruction of the bladder neck, and seriously affects the quality of life of patients (1, 2). High-risk patients with BPH are often accompanied by basic diseases such as hypertension and diabetes. In addition, they are elderly and have poor body resistance, which greatly increases the difficulty of treatment (3, 4). At present, surgical treatment is commonly used in clinical practice. Transurethral resection of the prostate (TURP) is one of the main methods for the clinical treatment of BPH, but due to the inability to completely remove the gland tissue, the gland can still continue to proliferate and lower urinary tract symptoms appear again, which greatly impacts patients (5, 6). Transurethral vaporization of the prostate (TUVP) is an improved resection method based on TURP, which can effectively shorten the operation time and improve the resection quality. However, its effect on the improvement of postoperative urethral symptoms is limited (7, 8). Plasma kinetic loop resection of the prostate (PKRP) is a new type of prostatectomy, which is different from TURP in the working principle. A current does not need to pass through the body, but it can form a local control loop through normal saline to break the molecular bonds in the prostate tissue and thus destroy the tissue to relieve the symptoms of obstruction (9, 10). The purpose of this study was to compare the efficacy of PKRP and TUVP in the treatment of BPH and analyze the effects of relevant factors on the operation of BPH.
Materials and methods
Patients
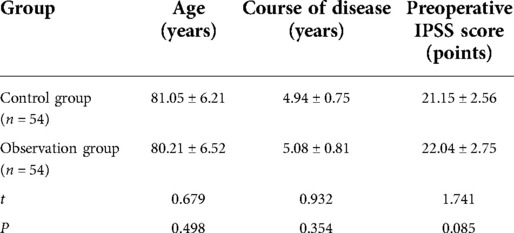
A total of 108 patients with high-risk BPH diagnosed in our hospital from March 2018 to September 2021 were selected. Inclusion criteria are as follows: all of them met the guidelines for the diagnosis and treatment of benign prostatic hyperplasia (11); there were no contraindications of operation and use of anesthetic drugs; and patients with renal insufficiency did not improve significantly. Exclusion criteria are as follows: acute infection of the urinary system; patients with prostate cancer; patients with bladder stones and other diseases; patients with other additional serious organ diseases; patients with drug allergy; and patients who dropped out during follow-up. A total of 108 high-risk BPH patients were randomly divided into an observation group and a control group, with 54 cases in each group. There was no significant difference in general data between the two groups, as shown in Table 1.
Surgical methods
Perioperative risk assessment was conducted before surgery, and surgery was arranged in the absence of absolute contraindication. If a urinary tract infection exists before surgery, empiric antibiotic treatment can be given, and a drug sensitivity test can be performed at the same time. Antibiotic medication can be adjusted according to the drug sensitivity test, urinary tract infection symptoms can be significantly improved, and surgical treatment can be performed later. If the patient has a history of urethral stricture, urethral dilation is feasible.
In both groups, the surgery was performed according to the standard procedures after lumbar anesthesia or continuous epidural anesthesia. The bladder lithotomy position was adopted, and the conventional bladder puncture fistulization was performed under television monitoring. The control group was treated with TUVP: a F26STORZ electrocision mirror (STORZ, Germany) was used, the power of vaporization electrocision was 200–230 W, the power of electrocoagulation was 80 W, and the content of lavage fluid was 5% mannitol. First, the hyperplastic glands were excised at 5–7 o’clock in advance and gradually cut in different regions. Finally, the periphery of the verruca was cut. With the bladder neck and the verruca as the marker points, the cutting depth is as deep as the surgical capsule as far as possible. The prostate fragment tissue was punched out by an Ellik evacuator, and the presence of the fragment residue was carefully examined again. F22 catheter was indwelled and bladder irrigation continued.
The observation group was treated with PKRP (GYRUS, UK). After successful anesthesia (continuous epidural block anesthesia was adopted for all patients), the lithotomy position was taken for the patient. The skin in the operation area was routinely sterilized with high-efficiency iodophor and then covered with a sterile towel. During the operation, the bladder was continuously rinsed, and amedical paraffin cotton ball was used to lubricate the electrocision lens sheath. After the lens sheath with the lens core was inserted, the lens core was extracted (if the external urethral orifice was relatively narrow, the urethral probe was used to expand and then the lens sheath was placed). An F26 resectoscope was placed along the sheath to observe the bladder and identify the location of the trigone of the bladder and bilateral ureterostoma, and then, the resectoscope was retreated to the posterior urethra to identify the prostatic hyperplasia and determine the location of the caruncle. The resection point was selected according to the location and degree of BPH. The bleeding was stopped by electric coagulation while the resection was performed. For obvious bilateral lobe hyperplasia, a landmark groove was cut at 6 o'clock to reach the level of the upper margin of Giemu, and the bilateral lobes were cut in sequence. If the hyperplasia of the middle lobe is more obvious, the 5:00 and 7: 00 positions should be marked first, and then the hyperplastic tissues of both lateral lobes and the middle lobe should be successively excised to the level of the upper margin of the Giemu to the depth of the prostatic capsule. Finally, the bladder neck and the prostatic apex were trimmed to ensure that the prostatic part of the urethra was a smooth tunnel. After careful electrocoagulation, hemostasis was performed on the whole wound surface and no active bleeding was detected. The endoscope was retracted. An Eric flusher was used to suck out the resected BPH tissue. An F20 or F22 three-cavity urinary catheter was retained, and the airbag was filled with water. The sterile oil yarn was used to tie a knot at the external orifice of the urethra. After a little traction and pressurization hemostasis were performed, the bladder was continuously rinsed with 0.9% sodium chloride isotonic rinse. And the operation was completed. The prostate tissue resected during the operation was sent for pathological examination for a definite diagnosis. After surgery, patients' consciousness and consciousness were closely monitored, ECG and pulse oxygen were monitored, and vital signs were closely monitored.
Observation indicators
Intraoperative blood loss and hospital stay in the two groups were recorded. The international prostate symptom score (IPSS) (12), quality of life index (QOL) (13), maximum urine flow rate (Qmax), and residual urine volume (RU) were observed before and after treatment. The general information such as age, educational level, residence, and residence status of the patient, as well as clinical information such as surgical method, nocturia frequency, preoperative IPSS score, RU, medical history, and prostate texture, was also recorded. All patients were followed up for 1 month, and complications were recorded.
Statistical methods
SPSS22.0 software was used for processing. The measurement data were expressed by mean ± standard deviation, and t-test analysis was used for pairwise comparisons. Count data were expressed by rate, and the chi-square test was used for the comparison between groups. A multivariate logistic regression model was used for multivariate analysis. P < 0.05 indicated that the difference was statistically significant.
Results
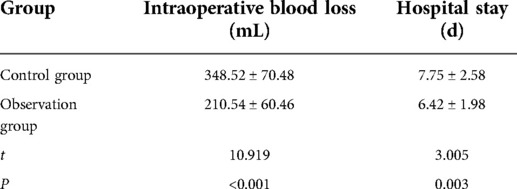
Comparison of intraoperative blood loss and hospital stay between two groups
The intraoperative blood loss and hospital stay in the observation group were lower than those in the control group (P < 0.05), as shown in Table 2.
Comparison of various efficacy indicators between the two groups
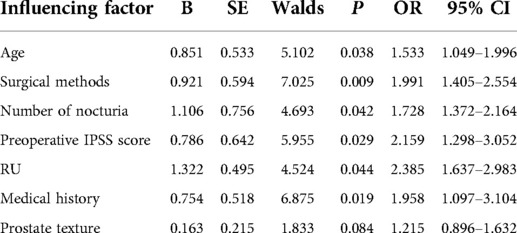
The IPSS score, QOL score, and RU of the two groups of patients after treatment were lower than those before treatment, and the Qmax was higher than that before treatment (P < 0.05). After the treatment, the IPSS score, QOL score, and RU of the observation group were lower than those of the control group, and the Qmax was higher than that of the control group (P < 0.05), as shown in Figure 1.
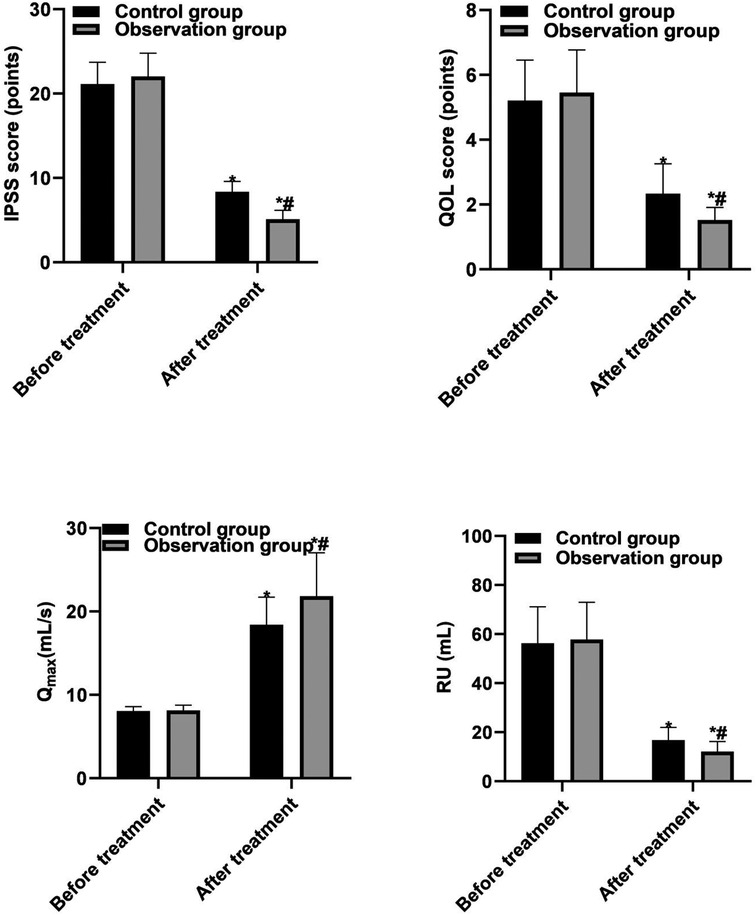
Figure 1. Comparison of various efficacy indicators between the two groups. Note: Compared with before treatment, *P < 0.05; compared with the control group, #P < 0.05.
Postoperative complications in two groups
In the control group, urethral stricture was found in four cases, postoperative hemorrhage in two cases, transient urinary incontinence in two cases, and epididymitis in one case. The complication rate was 16.67% (9/54). In the observation group, there was one case of urethral stricture, one case of transient urinary incontinence, and one case of epididymitis, and the incidence of complications was 5.56% (3/54). There was a significant difference in the incidence of complications between the two groups (P < 0.05), as shown in Figure 2.
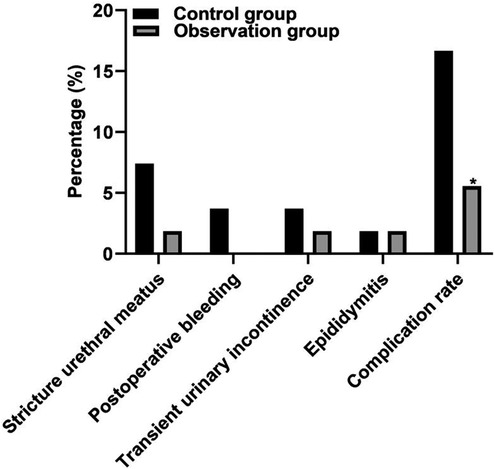
Figure 2. Postoperative complications in two groups. Note: Compared with the control group, *P < 0.05.
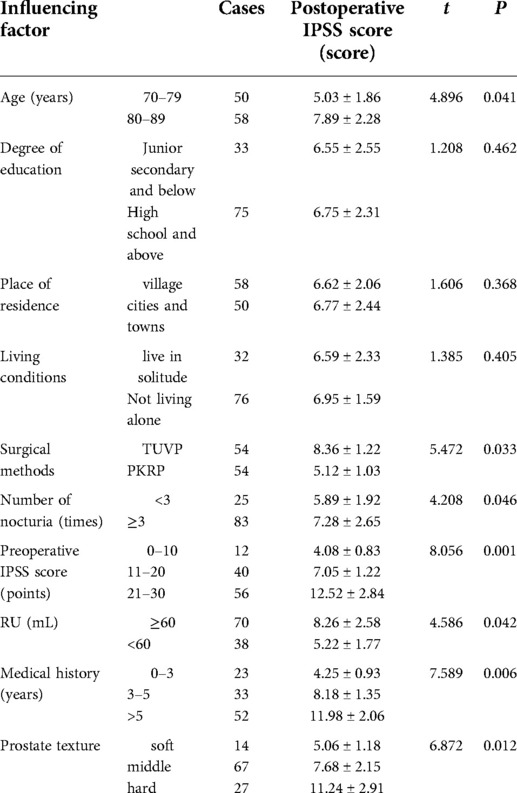
Single-factor analysis of the postoperative condition (IPSS score) of patients with BPH
Univariate analysis showed that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, medical history, and prostatic texture all could affect the postoperative condition of patients with BPH (P < 0.05), as shown in Table 3.
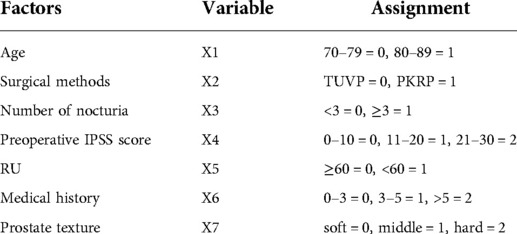
Multifactor analysis of the postoperative condition (IPSS score) of patients with BPH
Multivariate logistic analysis showed that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, and medical history were the independent influencing factors of the postoperative condition of patients with BPH (P < 0.05), as shown in Tables 4, 5.
Discussion
Patients with BPH are mainly men over 40 years old. The main symptoms of BPH are enlarged prostate glands and a blocked bladder outlet, causing lower urinary tract symptoms and even possibly leading to renal dysfunction. Especially for high-risk BPH patients, their older age, poorer body function, and more basic diseases increase the difficulty of treatment (14, 15). The treatment of BPH currently mainly includes surgical treatment and nonsurgical treatment. Nonoperative treatment is mainly performed through drugs. Drug treatment is mainly applied to mild lower urinary tract (LUT) symptoms caused by BPH. Most of the LUT symptoms are in the early stage of disease development. LUT symptoms exist but have not yet seriously affected daily life. Such patients can relieve LUT symptoms, delay disease development, inhibit bladder overactivity, promote urination, protect kidney function, prevent and avoid hematuria through drug treatment, and can also be given antibiotics to control urinary system infection and reduce the occurrence of acute urinary retention (16, 17). When the symptoms of LUT are serious, they can seriously affect and interfere with the daily life of patients; Or only have mild LUTs symptoms and have received drug treatment, but the symptoms are not significantly relieved or even worsened, the patient's subjective tolerance is poor, and the patient is seriously troubled; Or repeated hematuria, multiple urinary system infections, urinary retention cannot be alleviated, bladder stones appear, and secondary upper urinary tract hydronephrosis appear (18, 19). TURP is still the gold standard for the treatment of BPH, but it still has certain limitations in practice. High-risk prostatic hyperplasia is considered the relative contraindication for TURP surgery. Most patients can only receive palliative indwelling urinary catheter, cystostomy, and medication, resulting in poor quality of life (20, 21). Therefore, it is extremely important to select effective treatment methods for high-risk BPH patients.
The results of this study showed that intraoperative blood loss and hospital stay in the observation group were lower than those in the control group, indicating that PKRP could effectively reduce the intraoperative blood loss and hospital stay. The results of this study showed that the IPSS score, QOL score, and RU of patients in the two groups after treatment were lower than those before treatment, and Qmax was higher than that before treatment. The IPSS score, QOL score, and RU of patients in the observation group were lower than those of patients in the control group, and Qmax was higher than that of patients in the control group. One of the reasons was that the working principles of PKRP were different from those of TUVP. The working current of PKRP did not need to pass through the body but could directly pass through normal saline to form a local control loop, breaking the molecular bonds in the prostate tissue to destroy the tissue and relieve the symptoms of obstruction, which effectively reduced the tissue damage and improved the symptoms of postoperative urethral stimulation (22, 23). In addition, the research results show that the incidence of postoperative complications in the observation group is significantly lower than that in the control group. Urethral stricture may be caused by a urinary tract infection. The preoperative urinary tract infection is not completely controlled, the preoperative examination and surgical instruments are not disinfected thoroughly, the urethral mucosa is damaged due to lithotripsy and stone removal during the operation for the patients who are accompanied by bladder stones, the postoperative anti-infection treatment and perioperative nursing care were insufficient, and so on. All these aggravate the edema of local tissues, prolong the wound healing time, and finally lead to wound fibrosis and hyperplasia, and then scar healing, the formation of urethral stenosis (24, 25). Urethral stricture may also be caused by preoperative or intraoperative urethral dilatation. When the lens sheath is not sufficiently lubricated, it can also cause damage to the urethral mucosa during the insertion of the lens sheath, and in addition, the long-time compression of the electrotomy lens sheath can lead to ischemia, necrosis, fibrotic hyperplasia, and cicatrix healing of local tissue mucosa, finally forming urethral stricture. Stenosis caused by iatrogenic injury is usually caused by ischemia following uroendoscopic surgery or long-term indwelling catheter. During catheterization, the operator did not act gently enough and the catheter model was thick, hard, and not lubricated enough, thus damaging the urethral wall. Indwelling the postoperative catheter for a long time and long-term compression of the urethral wall lead to local tissue mucosal edema, ischemic necrosis scar healing, and then formation of urethral meatus stenosis (26, 27).
The results of this study show that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, medical history, and prostate texture can all affect the postoperative condition of patients with BPH. Multivariate logistic analysis showed that the patient's age, surgical method, nocturia frequency, preoperative IPSS score, RU, and medical history were the independent influencing factors of the postoperative condition in patients with BPH. The reasons were analyzed as follows: As patients get older, their body immunity weakens and their tolerance to large-scale surgery weakens. Moreover, elderly patients often suffer from chronic diseases such as hypertension, which greatly affects their recovery after surgery. PKRP and TUVP work on different principles. Current does not need to pass through the body, causing little damage to the prostate tissue. Moreover, due to the clear surgical field, the prostate tissue can be excised more accurately, which is conducive to the patient's postoperative urethral recovery. For patients with severe disease and a long history of prostate hyperplasia, it is difficult to resect the prostate tissue during the operation, so it is very easy to affect the curative effect of the operation.
Conclusion
PKRP in the treatment of high-risk BPH patients can effectively reduce the IPSS score, QOL score, and RU and significantly increase Qmax, with fewer complications and a good prognosis. Postoperative recovery was related to the patients’ age, nocturia frequency, preoperative IPSS score, RU, and medical history, and the surgical method used. Therefore, selecting PKRP for the treatment of high-risk BPH patients can effectively improve the postoperative urethral functional recovery of patients and reduce the occurrence of complications.
Data availability statement
The original contributions presented in the study are included in the article/Suplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of our Hospital (2018006). The patients/participants provided their written informed consent to participate in this study.
Author contributions
YS, SP, and GL are mainly responsible for the writing and research design of the article. SL and YH are mainly responsible for data analysis. The corresponding author is JY, and he is responsible for ensuring that the descriptions are accurate and agreed upon by all authors. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Meng Q, Li J, Li M, Qiu R. Evaluation of efficacy and safety of improved transurethral plasma kinetic enucleation of the prostate in high-risk patients with benign prostatic hyperplasia and coronary artery disease. J Int Med Res. (2021) 49:675845478. doi: 10.1177/03000605211060890
2. Zi H, Wang XJ, Zhao MJ, Huang Q, Wang XH, Zeng XT. Fasting blood glucose level and hypertension risk in aging benign prostatic hyperplasia patients. Aging (Albany NY). (2019) 11:4438–45. doi: 10.18632/aging.102061
3. Vartak KP, Raghuvanshi K. Outcome of thulium laser enucleation of prostate surgery in high-risk patients with benign prostatic hyperplasia. Urol Ann. (2019) 11:358–62. doi: 10.4103/UA.UA_175_18
4. Barco-Castillo C, Plata M, Zuluaga L, Santander J, Trujillo CG, Caicedo JI, et al. Functional outcomes and safety of GreenLight photovaporization of the prostate in the high-risk patient with lower urinary tract symptoms due to benign prostatic enlargement. Neurourol Urodyn. (2020) 39:303–9. doi: 10.1002/nau.24195
5. Gabr AH, Gabr MF, Elmohamady BN, Ahmed AF. Prostatic artery embolization: a promising technique in the treatment of high-risk patients with benign prostatic hyperplasia. Urol Int. (2016) 97:320–4. doi: 10.1159/000447360
6. Reich O, Corvin S, Oberneder R, Sroka R, Muschter R, Hofstetter A. In vitro comparison of transurethral vaporization of the prostate (TUVP), resection of the prostate (TURP), and vaporization-resection of the prostate (TUVRP). Urol Res. (2002) 30:15–20. doi: 10.1007/s00240-001-0231-4
7. Abdel-Khalek M, El-Hammady S, Ibrahiem E. A 4-year follow-up of a randomized prospective study comparing transurethral electrovaporization of the prostate with neodymium: YAG laser therapy for treating benign prostatic hyperplasia. Bju Int. (2003) 91:801–5. doi: 10.1046/j.1464-410x.2003.04245.x
8. Hammadeh MY, Philp T. Transurethral electrovaporization of the prostate (TUVP) is effective, safe and durable. Prostate Cancer Prostatic Dis. (2003) 6:121–6. doi: 10.1038/sj.pcan.4500654
9. Wang Z, Zhang J, Zhang H, Liu S, Sun D, Hu L, et al. Impact on sexual function of plasma button transurethral vapour enucleation versus plasmakinetic resection of the large prostate >90ml: results of a prospective, randomized trial. Andrologia. (2020) 52:e13390. doi: 10.1111/and.13390
10. Yang Z, Wang X, Liu T. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology. (2013) 81:396–400. doi: 10.1016/j.urology.2012.08.069
11. Roehrborn CG, Bartsch G, Kirby R, Andriole G, Boyle P, de la Rosette J, et al. Guidelines for the diagnosis and treatment of benign prostatic hyperplasia: a comparative, international overview. Urology. (2001) 58(5):642–50. doi: 10.1016/s0090-4295(01)01402-9
12. Bayoud Y, de la Taille A, Ouzzane A, Ploussard G, Allory Y, Yiou R, et al. International Prostate Symptom Score is a predictive factor of lower urinary tract symptoms after radical prostatectomy. Int J Urol. (2015) 22(3):283–7. doi: 10.1111/iju.12681
13. Estoque RC, Togawa T, Ooba M, Gomi K, Nakamura S, Hijioka Y, et al. A review of quality of life (QOL) assessments and indicators: towards a “QOL-climate” assessment framework. Ambio. (2019) 48(6):619–38. doi: 10.1007/s13280-018-1090-3
14. Tao W, Sun C, Xue B, Yang D, Wang M, Cai C, et al. The efficacy and safety of 2-μm continuous laser in the treatment of high-risk patients with benign prostatic hyperplasia. Lasers Med Sci. (2017) 32:351–6. doi: 10.1007/s10103-016-2122-5
15. Zhou J, He Z, Ma S, Liu R. AST/ALT ratio as a significant predictor of the incidence risk of prostate cancer. Cancer Med. (2020) 9:5672–7. doi: 10.1002/cam4.3086
16. Zhu Z, Shen Z, Tu F, Zhu Y, Sun F, Shao Y, et al. Thulium laser vaporesection versus transurethral electrovaporization of the prostate in high-risk patients with benign prostatic hyperplasia. Photomed Laser Surg. (2012) 30:714–8. doi: 10.1089/pho.2012.3316
17. Kamalov A, Kapranov S, Neymark A, Kurbatov D, Neymark B, Karpov V, et al. Prostatic artery embolization for benign prostatic hyperplasia treatment: a Russian multicenter study in more than 1,000 treated patients. Am J Mens Health. (2020) 14:1819201798. doi: 10.1177/1557988320923910
18. Zheng X, Qiu Y, Qiu S, Tang L, Nong K, Han X, et al. Photoselective vaporization has comparative efficacy and safety among high-risk benign prostate hyperplasia patients on or off systematic anticoagulation: a meta-analysis. World J Urol. (2019) 37:1377–87. doi: 10.1007/s00345-018-2530-1
19. Pachi PC, Khamari B, Lama M, Peketi A, Kumar P, Nagaraja V, et al. Draft genome sequence of pandrug-resistant Pseudomonas aeruginosa SPA03, isolated from a patient with benign prostatic hyperplasia. Microbiol Resour Announc. (2021) 10:e33621. doi: 10.1128/MRA.00336-21
20. Sun J, Shi A, Tong Z, Chi C. Green light photoselective vaporization of the prostate: a safe and effective treatment for elderly high-risk benign prostate hyperplasia patients with gland over 80 ml. Lasers Med Sci. (2018) 33:1693–8. doi: 10.1007/s10103-018-2521-x
21. Bhojani N, Yafi FA, Misrai V, Rijo E, Chughtai B, Zorn KC, et al. Review of sexual preservation after novel benign prostatic hyperplasia surgical treatment modalities from food and drug administration clinical trials. Sex Med Rev. (2021) 9:169–73. doi: 10.1016/j.sxmr.2020.09.003
22. Cheng X, Qin C, Xu P, Li Y, Peng M, Wu S, et al. Comparison of bipolar plasmakinetic resection of prostate versus photoselective vaporization of prostate by a three year retrospective observational study. Sci Rep. (2021) 11:10142. doi: 10.1038/s41598-021-89623-4
23. Li S, Kwong JS, Zeng XT, Ruan XL, Liu TZ, Weng H, et al. Plasmakinetic resection technology for the treatment of benign prostatic hyperplasia: evidence from a systematic review and meta-analysis. Sci Rep. (2015) 5:12002. doi: 10.1038/srep12002
24. Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: aUA GUIDELINE PART I-initial work-up and medical management. J Urol. (2021) 206:806–17. doi: 10.1097/JU.0000000000002183
25. Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am. (2016) 43:289–97. doi: 10.1016/j.ucl.2016.04.001
26. Uberoi P, Smith CA, Lucioni A. Management of lower urinary tract symptoms after prostate radiation. Curr Urol Rep. (2021) 22:37. doi: 10.1007/s11934-021-01048-8
Keywords: high-risk benign prostatic hyperplasia, transurethral plasmakinetic resection of the prostate, transurethral electrovaporization of the prostate, therapeutic effect, influencing factors
Citation: Song Y, Pang S, Luo G, Li S, He Y and Yang J (2022) Comparison of PKRP and TUVP in the treatment of high-risk BPH and analysis of postoperative influencing factors. Front. Surg. 9:947027. doi: 10.3389/fsurg.2022.947027
Received: 18 May 2022; Accepted: 23 June 2022;
Published: 3 August 2022.
Edited by:
Songwen Tan, Central South University, ChinaReviewed by:
Jiangang Liu, The Second Affiliated Hospital of Shandong First Medical University, ChinaWenjie Song, Fourth Military Medical University, China
© 2022 Song, Pang, Luo, Li, He and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinqiang Yang dXJveWpxQDEyNi5jb20=
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Yao Song
Yao Song Jinqiang Yang
Jinqiang Yang