
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 12 September 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.945013
This article is part of the Research Topic Surgical Innovation and Advancement in Orthopedics View all 57 articles
Background: There is no consensus on the best surgery option for thumb carpometacarpal osteoarthritis (CMC OA). The traditional method has the risk of large trauma, obvious metacarpal subsidence, and decreased stability. The aim of this study is to introduce a different technique to restore the function and stability of the first carpal metacarpal joint with minimal trauma, rapid pain relief, reduced complications, and the clinical outcomes in the long-term follow-up was evaluated and statistically analyzed.
Methods: This was a retrospective study of 10 patients with a mean age of 51.8 years. The surgery consisted of removing partial trapezium through arthroscopy, reconstructing the stability with flexor carpi radialis suspension and tendon interposition. The subjective assessment included visual analog scale (VAS) of pain, quick disabilities of the arm, shoulder, and hand (Quick-DASH) score, and patient satisfaction. The range of motion, grip strength, pinch strength, and radiographic assessment, which can reflect stability of the thumb, were objectively evaluated and statistically analyzed.
Results: Ten patients were monitored at a mean follow-up of 6.8 years. The mean grip strength improved significantly from 16.64 to 22.57 kg after surgery. Pinch strength improved significantly from 3.72 to 5.71 kg on average. The Kapandji score improved significantly from 5.7 to 8.6 on average. 80% (8/10) of the patients were satisfied with this surgery. On objective indicators, the VAS score decreased significantly from 6.4 to 1.3 on average. The mean Quick-DASH score improved significantly from 6.1 to 28.9. Postoperative x-ray showed slight subsidence and dislocation of the first metacarpal in two patients and did not affect the function by measurement.
Conclusion: Arthroscopy-assisted partial trapezium resection combined with ligament reconstruction could be a workable and promising surgical technique in patients with thumb CMC OA. It can offer the advantages of minimizing surgical injury by preserving the first carpal metacarpal joint capsule to protect its stability, with a rapid pain relief, function improvement, and satisfactory results in patients’ clinical measurements.
One out of three people aged 55 years and older have radiographic signs of carpometacarpal osteoarthritis (CMC OA) (1–3). Patients with mild symptoms in stage I and II can wear braces to increase stability and reduce mechanical stress. Patients of stage II to stage IV, in whom symptoms remain despite conservative treatment, should be treated by operation. There are numerous options in surgical treatment, such as trapeziectomy, ligament reconstruction, and tendon interposition or suspension arthroplasty (4–6). The traditional open trapeziectomy will destroy the joint capsule and affect the stability of the joint. Second, the classical flexor carpi radialis tendon reconstruction bypasses itself and is sutured and fixed in the first metacarpal bone, which will produce a downward pulling force during movement and may aggravate the sinking of the first metacarpal bone. In recent years, many studies have focused on new methods of tendon and ligament reconstruction, as well as minimally invasive surgery under wrist arthroscopy. However, there is still no consensus on the optimal treatment.
Compared with previous studies, this article introduced a different technique of arthroscopy-assisted partial trapezium resection, combined with ligament reconstruction and tendon interposition at the same time. This method not only reduces the damage to the capsular ligament and reduces the trauma but also partially maintains the height and stability of the metacarpal bone, which can be applied to more complex cases. Specifically, arthroscopy-assisted partial trapezium resection is less invasive compared with the parallel cross section of traditional open surgery. Moreover, the ball-and-socket joint was innovatively proposed in the surgery of the first carpal and metacarpal joint in this study. By modifying the saddle shape of the first carpal metacarpal joint into ball-and-socket joint, it may be more consistent with joint physiology and more stably adapt to the multidirectional activity requirements of the first carpal metacarpal joint. Finally, the classical approach of wrapping around the flexor carpi radialis has a downward force, which may aggravate the sinking of the first metacarpal. In our surgery, the approach of suturing around the first metacarpal itself creates an upward lifting force, theoretically reducing the sinking of the metacarpal.
The aim of this study was to introduce this different surgery, and the clinical outcomes in the long-term follow-up were evaluated and statistically analyzed.
From January 2012 to December 2021, 13 patients with thumb CMC arthritis were empirically selected and treated with this method, out of which 3 patients were lost to follow-up, leaving 10 patients (5 males and 5 females) for analysis. The indication criteria were patients with thumb CMC OA in stage II and stage III, combined with metacarpal dislocation, which required tendon and ligament reconstruction. One patient in stage IV strongly requested to attempt this surgery to delay the progression of arthritis due to the risk of metacarpal subsidence and instability after total trapeziectomy. All patients had clinical symptoms after at least 3 months of conservative treatment, confirmed by x-ray examination (Figure 1). According to Eaton staging (7), there were five patients in stage II, four patients in stage III, and one patient in stage IV.
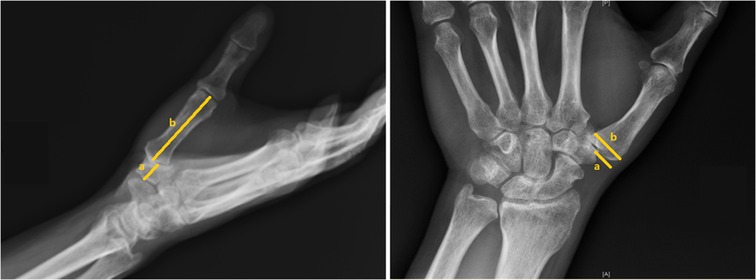
Figure 1. Radiograph of CMC OA with loss of joint space and radial dislocation. (Left) (a): axis of the trapezium and (b): axis of the first metacarpal; (right) (a): uncovered length of trapezium and (b): total length of trapezium.
Under general anesthesia, the patient was supine on an operating table with an arm board. A tourniquet (pressure: 34 kPa, limit time: 60 min) and wrist joint distraction of 15 lb were applied.
In the first step, two 4 mm transverse portals are made along the dorsoradial border of the hand with the thumb CMC joint as the center. The viewing camera is placed on the dorsoradial 1R portal to explore the articular surface; the shaver and radiofrequency are introduced in the dorsoulnar 1U portal to remove the hyperplastic synovium in the first CMC joint. The scaphoid trapezium trapezoid joint was explored and treated with the same method if needed. Then, arthroscopic partial resection of the trapezium is performed. Partial trapeziectomy is performed with the 1.9 mm burr, and part of the articular surface is removed until it shows hemispherical fossa of 3 mm depth (Figure 2). We polish the saddle joint and create a space for a tendon ball (Supplementary Video S1). The spur is resected to improve the range of motion (ROM) and symptoms as well as increase the stability of the basal joint.
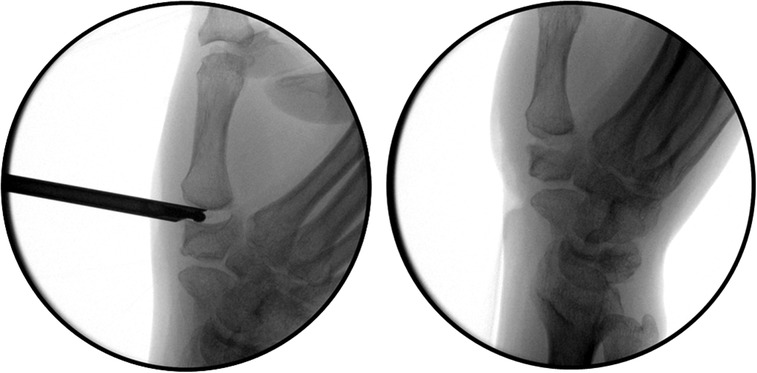
Figure 2. Arthroscopy-assisted partial trapezium resection. (Left): Partial trapeziectomy is performed with the 1.9 mm burr. (Right): The articular surface of the part of the trapezium is removed until it shows hemispherical fossa.
A transverse incision is made at approximately 5 cm level of the transverse wrist lines to expose the flexor carpi radialis. The radial half of the tendon is transected and dissociated distally to the level of the CMC joints (Figure 3). A 3.0 mm k-wire is drilled gradually to expand the bone hole. Then, the strip of the flexor carpi radialis is passed from the palmar side through the transosseous tunnel in the first metacarpal to the dorsal side, and the first metacarpal bone is fixed to the second metacarpal bone with a 1.5 mm k-wire. After wrapping around the base of first metacarpal, the spare flexor tendon is sutured with itself on the volar side. The remaining tendons are sutured to form a tendon ball.

Figure 3. The radial half of the tendon is transected and dissociated distally to the level of the CMC joints.
A grasper was inserted into the CMC joint from the 1R portal, which came out from the volar portal, to take the tendon ball from palmer side into the CMC joint space. Suture was used to fix the tendon ball to the dorsal side of joint capsule to prevent displacement. Large incision of the thumb CMC capsule is avoided during the whole procedure (Figure 4).
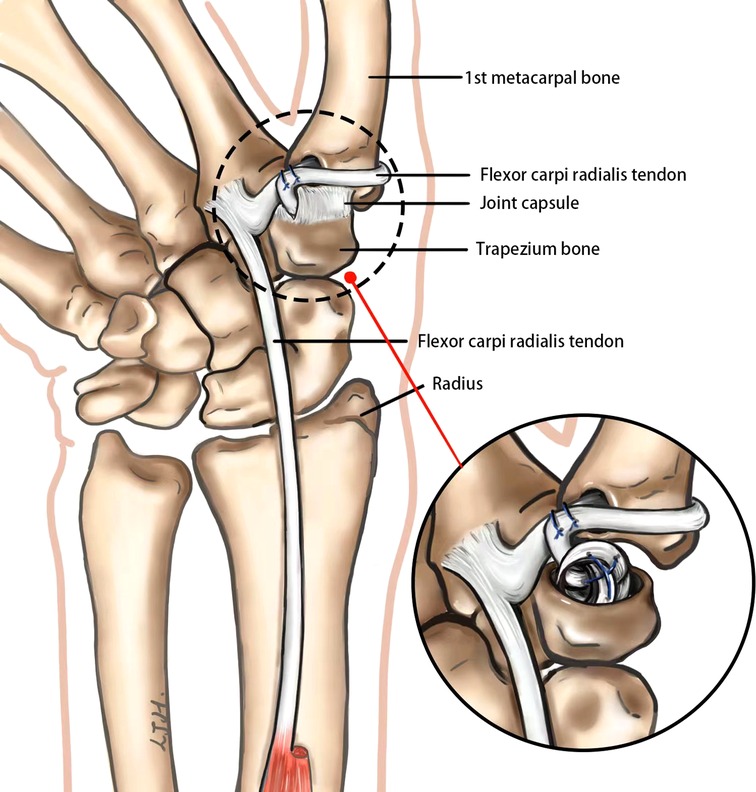
Figure 4. Ligament reconstruction. Surrounding the base of first metacarpal, one half of the tendon passes from the volar side to the dorsal side through the transosseous tunnel in first metacarpal and sutures with itself on the volar side.
After the surgery, a short-arm cast is fixed for 4 weeks, followed by a removable splint for another 4 weeks. The Kirschner wire was removed after 2 months (Figure 5). Then, patients were allowed unrestricted use of the wrist.
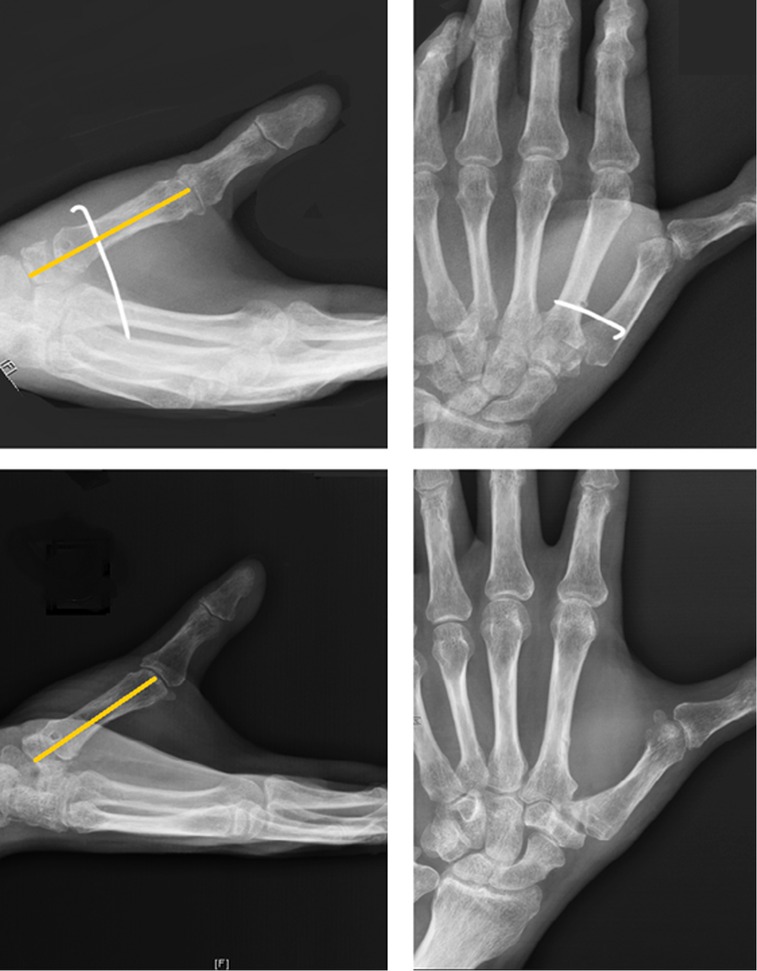
Figure 5. Fluoroscopy shows a good position with slight subsidence of the first metacarpal bone. (Above): Two months after surgery. (Below): Six months after surgery.
Patients were followed up at 2 months, 6 months, and every year after surgery. Clinical data were collected by an independent examiner. As compared with the preoperative condition and contralateral side, the clinical evaluation studied the ROM of the first column according to the Kapandji score (8). Grip strength was measured in kg using a Jamar (9) dynamometer, and pinch strength were measured in kg using the Preston (10) pinchmeter. Radiographs were taken in anterior and lateral planes before and after surgery. They were screened for dislocation, subsidence, and adjacent joint OA and can be used to assess joint stability (11).
At the last follow-up visit before summary, the pain intensity was evaluated on a visual analog scale (VAS) (12) from 0 (no pain) to 10 (worst imaginable pain). The ability to carry out daily life activities was evaluated based on the quick disabilities of the arm, shoulder, and hand (Quick-DASH) (13) questionnaire. Subjective evaluation of satisfaction was done with an analytical questionnaire ranging from 0 (dissatisfaction) to 10 (great satisfaction). In addition, the patient’s impression of thumb stability and ROM were evaluated by subjective as compared with the preoperative condition.
Data are presented as the mean ± standard deviation and 95% confidence intervals. The group means were compared using analysis of Student’s t test. Statistical analysis was performed using SPSS 20 and p < 0.05 was recognized as significant.
All patients underwent surgery in the same center between January 2012 and December 2021. The average age at admission was 51.8 years (range: 33–62). Mean follow-up was 6.8 years (range: 10–128 months). Preoperative characteristics are summarized in Table 1.
First, the 1-year follow-up data were analyzed in Table 2. Compared to the preoperative condition, the grip strength improved significantly to an average of 22.57 kg (p = 0.003). There was no significant difference relative to the grip strength in the healthy hand, which was 24.61 kg on average (p = 0.29). The postoperative pinch strength was also better than preoperative condition (3.72 kg preoperative, 5.71 kg postoperative, p = 0.04). Range of motion improved in the Kapandji score (preoperative at 5.70, postoperative at 8.60, p < 0.001).
Postoperative x-ray showed good joint position with neat axis alignment. Except for one patient who needed joint replacement due to severe polyarthritis of unknown cause, there was no complication like radial nerve injury, tendon rupture, tendinitis, or adjacent joint OA. At 1-year follow-up, two patients had slight metacarpal subsidence and dislocation, which did not affect the function according to the measurement.
At the final assessment, the pain was significantly decreased in all patients, the mean VAS decreased from 6.4 ± 1.3 to 1.1 ± 1.6 (p < 0.001), and the dexterity of the injury hand recovered well with a mean Quick-DASH score increased from 6.1 ± 13.2 to 28.9 ± 13.2 (p = 0.001). All patients reported a significant reduction in pain, and the Quick-DASH score was significantly increased than the preoperative condition (Figure 6). Meanwhile, thumb stability and ROM were also greatly improved than the preoperative condition. 80% (8/10) of the patients were satisfied with this surgery, and the mean satisfaction rating score was 8.8 ± 1.7. Detailed results are summarized in Table 3.
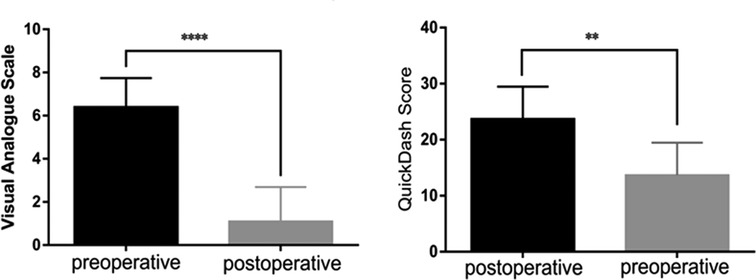
Figure 6. (Left) VAS values for pain. (Right) Quick-DASH score outcomes. **p = 0.001 and ****p < 0.0001.
Following the interphalangeal joints, the thumb CMC joint is the second most frequent site of hand OA (14–17). There are numerous options in surgical treatment for CMC OA, with evidence for pain relief and function improved (18). However, comparative studies on different methods and techniques have failed to clarify which techniques are best for treating CMC OA (19). In most hand surgery departments, trapeziectomy combined with ligament reconstruction and tendon interposition is still the most commonly performed technique (20). Compared to trapeziectomy alone, partial resection partially maintained the height of the first metacarpal, and the use of ligamentoplasty adds stability and hence decreases articular irritation (21). Moreover, tendon interposition provides a good buffer while maintaining height, which also helps delay the progression of arthritis. In addition, the advantages of arthroscopy are minimal trauma, rapid recovery, clear field exposure, and its convenience to remove the spur between first and second metacarpal base area to improve symptoms. Although the difficulty of the operation is slightly increased, the operation can be simplified according to the patient’s condition, and the application scope is wider, which has the opportunity to become the gold standard of such surgery.
The thumb CMC joint is known as the saddle joint; this shallow biconcave–convex saddle shape provides little bony stability, and thus the joint relies heavily on its flexible capsular ligaments to prevent subluxation and allow a wide arc of motion (22–24). The main advantage of our procedure is that the large incision of the thumb CMC capsule is avoided. Previous method of partial trapeziectomy is to open the capsule and make the partial trapeziectomy with oscillating saw to form a plain surface. In this procedure, a 1.9 mm burr was used to accomplish the partial trapeziectomy through small portal to minimize the injury to capsule. In addition, hemispherical fossa might be more suitable to hold the tendon ball rather than a plain surface. Although it partially changes the physiology of the joint, it has the opportunity to become a new surgical concept for the treatment of joint diseases and has the potential to be further explored. For the tendon ball interposition step, a grasper is used to take the tendon ball into the joint space. Thus, large incision of the thumb CMC capsule is avoided during the whole procedure. These modifications make it possible to preserve the joint capsule to protect joint instability.
The results of our research have shown that this technique can significantly improve patients’ clinical measurements, functional scores, and relieve patients’ pain with a low complication rate. Although two patients had slight metacarpal subsidence and dislocation, it did not affect function by measurement. This finding is consistent with a recent study which concluded that there was no relationship between postoperative first metacarpal subsidence and functional outcomes (25). The surgical precautions are as follows: (1) Blunt dissection to prevent damage to the radial nerves and CMC capsule; (2) The bone holes should be smooth to prevent the tendon from breaking under stress; (3) The spur should be resected to improve ROM and symptoms and also increase the stability of basal joint; (4) The tendon ball is sutured to the dorsal side of the capsule to prevent displacement.
The study has some limitations. First, our study is a retrospective long-term review, which may include the inherent bias and underestimated the complication rate (26). To overcome the lack of a comparison group for there is no gold standard procedure for this disease, we compared data with preoperative and healthy side. Because the recovery effect was well, further research with a larger sample size is needed for verification, and further horizontal comparison of different surgical methods to screen out the gold standard CMC OA treatment is meaningful.
This long-term follow-up study indicates that arthroscopy-assisted partial trapezium resection combined with ligament reconstruction could be a workable and promising surgical technique in patients with thumb CMC OA. It can offer the advantages of minimizing surgical injury by preserving the first carpal metacarpal joint capsule to protect its stability, with rapid pain relief, function improvement, and satisfactory results in patients’ clinical measurements.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the ethics committee of our hospital. Written informed consent to participate in this study was obtained from all participants.
H-WY and W-DX designed the study. Y-CW, W-LZ, and Y-DS collected and prepared the data. W-LZ and H-WY drafted the article. All of the authors critically revised the article. W-DX supervised the study. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (81801941 and 82021002), the Shanghai Technology Innovation Plan (21Y11902900), the Shanghai Municipal Clinical Medical Center Project (2017ZZ01006), and the Program of Shanghai Municipal Commission of Health and Family Planning (20164Y0018).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.945013/full#supplementary-material.
1. Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, Pols HA, Hazes JM, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. (2005) 64(5):682–7. doi: 10.1136/ard.2004.023564
2. Becker SJ, Briet JP, Hageman MG, Ring D. Death, taxes, and trapeziometacarpal arthrosis. Clin Orthop Relat Res. (2013) 471(12):3738–44. doi: 10.1007/s11999-013-3243-9
3. Sodha S, Ring D, Zurakowski D, Jupiter JB. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. (2005) 87(12):2614–8. doi: 10.2106/00004623-200512000-00003
4. Cobb TK, Walden AL, Cao Y. Long-term outcome of arthroscopic resection arthroplasty with or without interposition for thumb basal joint arthritis. J Hand Surg Am. (2015) 40:1844–51. doi: 10.1016/j.jhsa.2015.05.010
5. Asltissimi M, Pataia E, Rampoldi M, Azzarà A, Braghiroli L. Trapeziectomy and suspension arthroplasty with the flexor carpi radialis tendon for treatment of trapeziometacarpal osteoarthritis. Hand Surg Rehabil. (2021) 40(2):162–6. doi: 10.1016/j.hansur.2020.11.010
6. Fulchignoni C, Morini A, Panzera RM, Merendi G, Rocchi L. F. brunelli ligamentoplasty as treatment in thumb basal joint arthritis: up to 9 years follow-up. Tech Hand Up Extrem Surg. (2020) 25(2):77–83. doi: 10.1097/BTH.0000000000000308
7. Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. (1987) 3(4):455–71. doi: 10.1016/S0749-0712(21)00761-7
8. Kapandji A. Clinical test of apposition and counter-apposition of the thumb. Ann Chir Main. (1986) 5:67–73. doi: 10.1016/S0753-9053(86)80053-9
9. Schmidt RT, Toews JV. Grip strength as measured by the Jamar dynamometer. Arch Phys Med Rehabil. (1970) 51:321–7. PMID: 5423802
10. Hook WE, Stanley JK. Assessment of thumb to index pulp to pulp pinch grip strengths. J Hand Surg Br. (1986) 11B:91–2. doi: 10.1016/0266-7681_86_90024-0
11. Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. (2006) 7:44. doi: 10.1186/1471-2474-7-44
12. Froschauer SM, Holzbauer M, Mihalic JA, Kwasny O. TOUCH® prosthesis for thumb carpometacarpal joint osteoarthritis: a prospective case series. J Clin Med. (2021) 10(18):4090. doi: 10.3390/jcm10184090
13. Villafañe JH, Valdes K, Bertozzi L, Negrini S. Minimal clinically important difference of grip and pinch strength in women with thumb carpometacarpal osteoarthritis when compared to healthy subjects. Rehabil Nurs. (2017) 42(3):139–45. doi: 10.1002/rnj.196
14. Marotta N, Demeco A, Marinaro C, Moggio L, Pino I, Barletta M, et al. Comparative effectiveness of orthoses for thumb osteoarthritis: a systematic review and network meta-analysis. Arch Phys Med Rehabil. (2021) 102(3):502–9. doi: 10.1016/j.apmr.2020.06.012
15. Gillis J, Calder K, Williams J. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Can J Plast Surg. (2011) 19(4):134–8. doi: 10.1177/229255031101900409
16. Rocchi L, Merolli A, Giordani L, Albensi C, Foti C. Trapeziometacarpal joint osteoarthritis: a prospective trial on two widespread conservative therapies. Muscles Ligaments Tendons J. (2018) 7(4):603–10. doi: 10.32098/mltj.04.2017.16
17. Prosser R, Hancock MJ, Nicholson L, Merry C, Thorley F, Wheen D. Rigid versus semi-rigid orthotic use following TMC arthroplasty: a randomized controlled trial. J Hand Ther. (2014) 27(4):265–70, quiz 271. doi: 10.1016/j.jht.2014.06.002
18. Wolf JM, Turkiewicz A, Englund M, Karlsson J, Arner M, Atroshi I. What are the patient-reported outcomes of trapeziectomy and tendon suspension at long-term follow-up? Clin Orthop Relat Res. (2021) 479(9):2009–18. doi: 10.1097/CORR.0000000000001795
19. Hentz VR. Surgical treatment of trapeziometacarpal joint arthritis: a historical perspective. Clin Orthop Relat Res. (2014) 472:1184–9. doi: 10.1007/s11999-013-3374-z
20. Ashford-Wilson S, Ghazala CG, McLaughlin K, Harrison JWK. Failed trapeziectomy treated by thumb metacarpal base arthrodesis: a case series. Tech Hand Up Extrem Surg. (2021) 25(4):219–25. doi: 10.1097/BTH.0000000000000338
21. McVeigh KH, Kannas SN, Ivy CC, Garner HW, Barnes CS, Heckman MG, et al. Dynamic stabilization home exercise program for treatment of thumb carpometacarpal osteoarthritis: a prospective randomized control trial. J Hand Ther. (2021) S0894-1130(21):00083-1. doi: 10.1016/j.jht.2021.06.002
22. Goorens CK, Goubau J, Van Hoonacker P, Kerckhove D, Berghs B, Scheerlinck T. Addition-subtraction osteotomy without ligamentoplasty for symptomatic trapezial dysplasia with metacarpal instability. Acta Orthop Belg. (2013) 79(5):517–23. doi: 10.1016/j.main.2013.07.001
23. Rusli WMR, Mirza E, Tolerton S, Yong S, Johnson R, Horwitz MD, et al. Ligamentous constraint of the first carpometacarpal joint. J Biomech. (2021) 128:110789. doi: 10.1016/j.jbiomech.2021.110789
24. Ladd AL, Weiss AP, Crisco JJ, Hagert E, Wolf JM, Glickel SZ, et al. The thumb carpometacarpal joint: anatomy, hormones, and biomechanics. Instr Course Lect. (2013) 62:165–79. PMID: 23395023; PMCID: pmc3935621
25. Mirza A, Mirza JB, Klingbeil L, Pavlik JF 3rd, Muratori J, Thomas T. A modified suture suspension arthroplasty technique for the treatment of basal joint arthritis: short- to intermediate-term outcomes. Hand. (2021) 16(6):797–803. doi: 10.1177/1558944719886669
26. Van Laarhoven CMCA, Ottenhoff JSE, van Hoorn BTJA, van Heijl M, Schuurman AH, van der Heijden BEPA. Medium to long-term follow-up after pyrocarbon disc interposition arthroplasty for treatment of CMC thumb joint arthritis. J Hand Surg Am. (2021) 46(2):150.e1–150.e14. doi: 10.1016/j.jhsa.2020.07.025
Keywords: thumb, carpometacarpal joint (CMC), osteoarthritis, arthroscopy, ligament reconstruction and tendon interposition, trapeziectomy
Citation: Zheng W, Wu Y, Shen Y, Yin H and Xu W (2022) Arthroscopy-assisted partial trapeziectomy combined with ligament reconstruction for thumb carpometacarpal joint osteoarthritis: A different technique. Front. Surg. 9:945013. doi: 10.3389/fsurg.2022.945013
Received: 16 May 2022; Accepted: 23 August 2022;
Published: 12 September 2022.
Edited by:
Paphon Sa-ngasoongsong, Ramathibodi Hospital, Mahidol University, ThailandReviewed by:
Juitien Shih, Taoyuan Armed Forces General Hospital, Taiwan© 2022 Zheng, Wu, Shen, Yin and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua-Wei Yin eWluaHVhd2VpMTk4M0AxMjYuY29t
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.