
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 05 July 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.944509
This article is part of the Research Topic Endoscopic Spine Surgery: New concepts and advancements View all 23 articles
Introduction: Unilateral biportal endoscopy (UBE) is a relatively new yet common minimally invasive procedure in spine surgery, capable of achieving adequate decompression for lumbar spinal stenosis through unilateral laminectomy bilateral decompression (ULBD). Neither additional fusion nor rigid fixation is required, as UBE-ULBD rarely causes iatrogenic lumbar instability. However, to our knowledge, five-level ULBD via two-stage UBE without lumbar fusion has been yet to be reported in the treatment of multilevel lumbar spinal stenosis.
Case description: We present a case of an 80-year-old female patient who developed progressive paralysis of the lower extremities. Radiographic examinations showed multilevel degenerative lumbar spinal stenosis and extensive compression of the dural sac and nerve roots from L1-2 to L5-S1. The patient underwent five-level ULBD through two-stage UBE without lumbar fusion or fixation. One week after the final procedure, the patient could ambulate with walking aids and braces. Moreover, no back pain or limited lumbar motion was observed at the 6-month follow-up.
Conclusion: Multilevel ULBD through UBE may provide elderly patients with an alternative, minimally invasive procedure for treating spinal stenosis. This procedure could be achieved by staging surgeries. In this case, we reported complaints of little back pain, despite not needing to perform lumbar fusion or fixation.
Unilateral biportal endoscopy (UBE) is a minimally invasive procedure in which water-medium endoscopic surgery is performed to achieve neural decompression or spinal fusion. Unilateral laminectomy bilateral decompression (ULBD) via UBE is indicated for lumbar spinal stenosis (LSS), as confirmed by several randomized controlled trials (1, 2). Although many studies on this technique have published, most only reported 1- or 2-level UBE-ULBD. This is the first report on 5-level ULBD via two-stage UBE for multilevel LSS.
The patient was an 80-year-old female who developed progressive paralysis of the lower extremities and radicular pain of the left leg, which confined her to a wheelchair daily over the past two years. Sensory disturbances of the anterior bilateral thighs, lateral crura and dorsum of the feet were found through physical examination. The Lasegue sign of the left leg was positive, and the bilateral Babinski signs were negative. Flexion and extension lateral lumbar radiographs showed relative dynamic stability at all lumbar segments (Figure 1A). Lumbar computed tomography (CT) showed multilevel degenerative stenosis and L4 spondylolisthesis (Figure 1B). Magnetic resonance imaging (MRI) revealed serious stenosis from L1-2 to L5-S1 and left lateral recess stenosis at L5-S1 (Figure 1C).

Figure 1. Flexion and extension lateral lumbar X-ray radiograph demonstrating relative dynamic stability at all lumbar segments (A). Lumbar CT showing hyperplasia and cohesion of the facet joints, ossification of the ligamentum flavum and multilevel stenosis of the lateral recesses and central canals (B). Sagittal and axial T2-weighted lumbar MRI revealing serious central canal stenosis from L1-2 to L4-5, lumbar disc herniation and left lateral recess stenosis at L5-S1 (C).
According to the patient's symptoms, physical examination, and imaging findings, the patient did not have significant lumbar instability, which was also the indication of non-fusion surgery. Because of multilevel severe stenosis and extensive neurological defects, it was difficult to identify one or two segments as the responsible segments. One stage surgery would take longer operation time and more intraoperative blood loss. So we performed staged procedures. In the first stage procedure, the patient's radicular pain of lower limb was considered, double ULBD at L4-5 and L5-S1 from the left side was performed through first-stage UBE to decompress the bilateral L5 and S1 nerve roots and dural sacs (Figure 2).
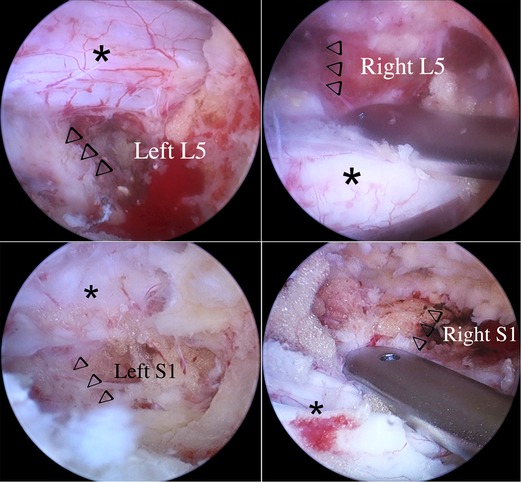
Figure 2. Bilateral L5 and S1 nerve roots and dural sacs after first-stage first stage UBE-ULBD (arrowheads indicate nerve roots, asterisks indicate dural sacs).
The left leg pain improved significantly the first day after the first-stage procedure. But the patient still could not realize to walk independently. So we continued to perform ULBD at L3-4, L2-3 and L1-2 from the same side one week after the first-stage surgery. The bilateral L3, L2, and L1 nerve roots and dural sacs were decompressed through the second-stage procedure (Figure 3). Bilateral nerve roots were exposed at all segments to ensure adequate lateral decompression of the lumbar canal (Supplementary Video 1).
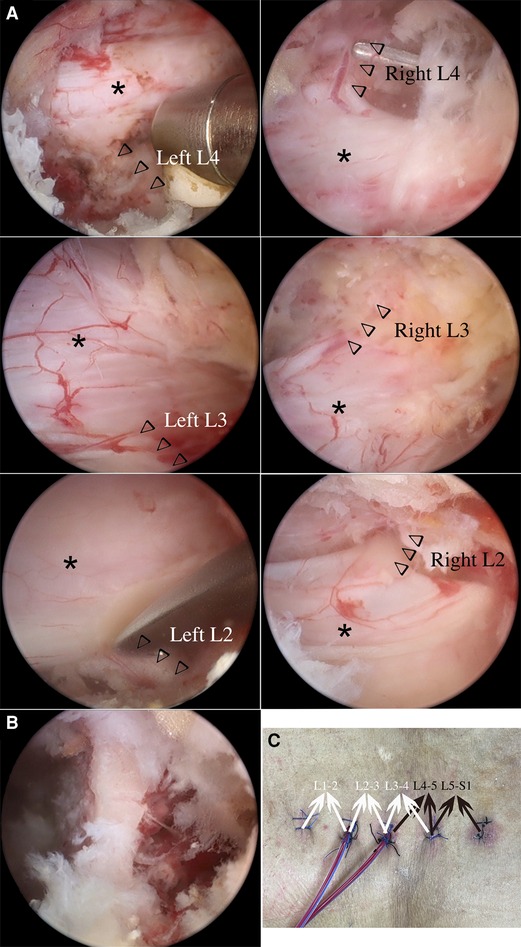
Figure 3. Bilateral L4, L3 and L2 nerve roots and dural sacs after second-stage UBE-ULBD (arrowheads indicate nerve roots, asterisks indicate dural sacs) (A). Residual left lamina of L4 after L4-5 and L3-4 UBE-ULBD (B). The surgical incisions after the two-stage procedure and the counterparts of the surgical segments (black arrowheads indicate the first-stage operation, white arrowheads indicate the second-stage operation) (C).
Celecoxib was given to relieve the low back pain postoperatively. The patient recovered to ambulate with a Boston brace after the second-stage surgery and rehabilitative training. The patient was discharged home after her low back pain was relieved, and she was able to bend and stretch her back (Figure 4A). Postoperative lumbar radiographs showed the range of laminectomies and decompressed lumbar spinal canals (Figure 4B). The patient has been followed-up for 1 year since the second-stage operation and reports significantly improved pain levels and the ability to complete daily activities. The 1-year follow-up's imagings showed satisfactory decompression of lumbar spinal canals, and the spondylolisthesis of L4 still not progressed (Figure 5).

Figure 4. The patient achieved favorable flexion and extension of the back with little pain (A). Regions of bone resection after the two-stage procedure (red circles) (B).

Figure 5. The lumbar X-ray radiograph of 1-year follow-up demonstrating all surgical segments remained stable (A). Lumbar CT of 1-year follow-up showing the bony structure changes of surgical segments (B). Sagittal and axial T2-weighted lumbar MRI revealing satisfactory decompression of lumbar canal from L1-2 to L5-S1 (C).
LSS is caused by gradual degenerative narrowing of the spinal canal. According to a randomized controlled trial study, compared with decompression plus fusion surgery, single decompression surgery showed considerable clinical results (3). The ULBD technique was first reported by Young in 1988, and it has been rapidly improved by the use of various minimally invasive techniques, such as microscopy and microendoscopy. Nevertheless, the air medium required under microscopy and microendoscopy cannot provide a clear visual field, especially in contralateral decompression procedures (4, 5). Full endoscopic ULBD can achieve effective bilateral decompression via water medium, and several studies have reported favorable outcomes from this version of the procedure in the treatment of LSS (6). However, full endoscopic ULBD has a steep learning curve and a high rate of complications (7). ULBD via UBE is a relatively newly emerging technique that provides surgeons an alternative for conducting ULBD in a minimally invasive manner. Following the first report of this procedure from Egyptian and South Korean researchers, UBE-ULBD has been suggested to be a safe and effective surgery for LSS decompression (8, 9). Nevertheless, few studies have reported the clinical outcomes of multilevel UBE-ULBD, and its efficacy and safety remain unclear. In this case, a patient with multilevel LSS underwent five-level UBE-ULBD in two stages, which is the first report to our knowledge on such a large number of ULBD procedures for one patient.
For this patient, the long segmental lumbar fusion defects, including extensive detachment of the paravertebral extensors and limited back movement, were the reasons why we chose this minimally invasive, nonfusion surgery. In addition, this patient had no obvious degenerative spinal deformity or serious back pain. All her symptoms had developed as a result of compression of nerve roots and cauda equina. Staging the procedures can reduce the duration of each process, which is beneficial for the postoperative recovery of elderly patients. The range of bone resection in conventional ULBD mainly involves the partial unilateral lamina and internal cortex of the contralateral lamina. In this patient, bone resection involved the ventral side of the superior articular process due to decompression of the nerve root in the lateral recess. This procedure is also widely used in the full endoscopic version of ULBD surgery (10). Our experience with this patient demonstrates that ULBD with partial facet resection minimally damages the stability of the surgical segment, and the impairment of the paravertebral muscles was relatively limited. Additionally, the patient did not complain of obvious back pain during lumbar movement.
LSS is a very common pathological condition in elderly individuals. Complicating matters is that this pathological process frequently involves two or more levels, requiring the surgeon to attempt to balance wide-range decompression and spinal stability. UBE-ULBD could provide surgeons with a good alternative to expanded laminectomy or long segmental fusion. This minimally invasive procedure has remarkable advantages in producing early ambulation, inducing less incision pain, and requiring shorter hospital stays. All these factors could reduce the risk of postoperative complications, mortality and utilization in elderly patients. Moreover, many elderly patients who have multiple comorbidities, such as hypertension, diabetes mellitus and coronary heart disease, may have more opportunities to undergo lumbar surgery with the continuing development of minimally invasive nonfusion techniques.
UBE is an emerging minimally invasive spinal technique that can be performed for a variety of lumbar degenerative diseases, including multilevel lumbar spinal stenosis. ULBD via UBE can achieve safe and effective decompression, which may be crucial for allowing elderly patients to complete their daily activities. We presented a case of a patient who developed multilevel LSS and underwent two-stage, five-level UBE-ULBD, achieving a favorable clinical result.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Peking University Shougang Hospital Ethics Board. The patients/participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
W-lW: conceptualization, resources, writing (original draft preparation), writing (review and editing), visualization, and project administration. S-jW: software and data collection. ZL: chief surgeon and the patient's follow-up. All authors have read and agreed to the published version of the manuscript. All authors contributed to the article and approved the submitted version.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.944509/full#supplementary-material.
Supplementary Video 1 | The residual left lamina of L4 under the second-stage endoscopic visualization.The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Park SM, Kim GU, Kim HJ, Choi JH, Chang BS, Lee CK, et al. Is the use of a unilateral biportal endoscopic approach associated with rapid recovery after lumbar decompressive laminectomy? A preliminary analysis of a prospective randomized controlled trial. World Neurosurg. (2019) 128:e709–18. doi: 10.1016/j.wneu.2019.04.240
2. Kang T, Park SY, Kang CH, Lee SH, Park JH, Suh SW. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients?: a prospective randomized comparative study. Medicine (Baltimore). (2019) 98:e15451. doi: 10.1097/MD.0000000000015451
3. Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med. (2016) 374:1413–23. doi: 10.1056/NEJMoa1513721
4. Yang F, Chen R, Gu D, Ye Q, Liu W, Qi J, et al. Clinical comparison of full-endoscopic and microscopic unilateral laminotomy for bilateral decompression in the treatment of elderly lumbar spinal stenosis: a retrospective study with 12-month follow-up. J Pain Res. (2020) 13:1377–84. doi: 10.2147/JPR.S254275
5. Zhao XB, Ma HJ, Geng B, Zhou HG, Xia YY. Percutaneous endoscopic unilateral laminotomy and bilateral decompression for lumbar spinal stenosis. Orthop Surg. (2021) 13:641–50. doi: 10.1111/os.12925
6. Huang YH, Lien FC, Chao LY, Lin CH, Chen SH. Full endoscopic uniportal unilateral laminotomy for bilateral decompression in degenerative lumbar spinal stenosis: highlight of ligamentum flavum detachment and survey of efficacy and safety in 2 years of follow-up. World Neurosurg. (2020) 134:e672–81. doi: 10.1016/j.wneu.2019.10.162
7. Park SM, Park J, Jang HS, Heo YW, Han H, Kim HJ, et al. Biportal endoscopic versus microscopic lumbar decompressive laminectomy in patients with spinal stenosis: a randomized controlled trial. Spine J. (2020) 20:156–65. doi: 10.1016/j.spinee.2019.09.015
8. Soliman HM. Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J. (2015) 15:2282–9. doi: 10.1016/j.spinee.2015.07.009
9. Eum JH, Heo DH, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine. (2016) 24:602–7. doi: 10.3171/2015.7.SPINE15304
10. Komp M, Hahn P, Oezdemir S, Giannakopoulos A, Heikenfeld R, Kasch R, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. (2015) 18:61–70. doi: 10.36076/ppj/2015.18.61
Keywords: case report, unilateral laminectomy bilateral decompression (ULBD), unilateral biportal endoscopy (UBE), lumbar spinal stenosis (LSS), multilevel
Citation: Wang W, Liu Z and Wu S (2022) Case Report: Five-Level Unilateral Laminectomy Bilateral Decompression (ULBD) by Two-Stage Unilateral Biportal Endoscopy (UBE). Front. Surg. 9:944509. doi: 10.3389/fsurg.2022.944509
Received: 15 May 2022; Accepted: 13 June 2022;
Published: 5 July 2022.
Edited by:
Zhen-Zhou Li, Fourth Medical Center of PLA General Hospital, ChinaReviewed by:
Tian Dasheng, Anhui Medical University, ChinaCopyright © 2022 Wang, Liu and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng Liu bHozMDExOThAYWxpeXVuLmNvbQ==
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations: UBE, unilateral biportal endoscopic; ULBD, unilateral laminectomy bilateral decompression; LSS, lumbar spinal stenosis; CT, computed tomography; MRI, magnetic resonance imaging.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.