
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 11 July 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.942881
This article is part of the Research Topic Experimental and Computational Processes in Surgery View all 10 articles
Background: Influenced by individual differences, the depth of gastric tube placement is often different. Clinically, it is necessary to seek a simple and accurate gastric tube insertion scheme to improve the clinical efficacy of indwelling gastric tube.
Materials and Methods: A total of 100 adult patients undergoing transesophageal manometry via nose were included in the study. The in vivo length (NCL) of apex-cardia was measured. At the same time, we entered our institutional database, summarized the clinical data of 100 patients, and analyzed the risk factors affecting NCL using stepwise regression analysis.
Results: The NCL length scores of patients with different gender, age, marital status, height, weight, BMI, sitting height, sternum length, hairline-xiphoid process, nose tip-earlobe-xiphoid process and earlobe-xiphoid process were statistically significant (P < 0.05). Height, sitting height, gender, BMI and earlobe-xiphoid process were the factors that affected the NCL length score (P < 0.05). The prediction equation of the estimation method of gastric tube insertion length was as follows: NCL length score = 39.907 + 2.909× height +0.865× sitting height. Adjust R2 to 0.506. NCL was positively correlated with height and sitting height. Among them, the correlation with height (r = 0.711, P < 0.001) and sitting height (r = 0.397, P < 0.001).
Conclusion: Height, sitting height, gender, BMI and earlobe-xiphoid process were the factors that affected the score of NCL length. There was a significant positive correlation between height, sitting height and NCL length. On this basis, the length of nasogastric tube insertion could be estimated.
Refers to inserting the catheter into the gastrointestinal tract through the nasal cavity or oral cavity, and providing the patients with the necessary food, nutrient solution, water and drugs through the catheter, or performing gastric lavage and gastrointestinal decompression through the catheter, which is a routine nursing operation with wide clinical application (1, 2). Indwelling gastric tube can not only supply the necessary nutrition for clinical patients, but also achieve the effect of gastrointestinal decompression. Compared with foreign countries, only a small number of studies in China have explored the factors affecting the length of gastric tube placement in adults and its prediction equation through correlation or regression analysis. The existing guidelines also fail to address such issues as the specific length to be extended of gastric tube insertion, and whether it is safe to extend the insertion length. Although the length from the hairline to the xiphoid process or from the earlobe to the xiphoid process is often used as the insertion depth in clinic, the insertion depth is often not the same due to individual differences of patients, so the accuracy of this method has always been questioned (3, 4). Therefore, in this study, the in vivo length (NCL) of nasal tip–cardia in adults used as a dependent variable to explore its relationship with other clinical data such as gender, age, height, and weight. At the same time, the prediction equation with optimal stability and accuracy was established based on the above results, in order to provide a theoretical basis for the estimation of the length of gastric tube placement.
The convenience sampling method was used to select adult patients who required transesophageal manometry via nose or gastroscopy via mouth in a 3A hospital in Changsha from March 2020 to February 2022.
Inclusion criteria: (1) Age ≥ 18 years old. (2) Conscious, willing to undergo gastroscopy or esophageal manometry, and willing to participate in this study. (3) There is no obvious thoracic deformity, spinal deformity and developmental abnormality. (4) There is no previous operation history of upper digestive tract such as esophagus and stomach. (5) Patients with the course of disease less than three months.
Exclusion criteria: (1) Patients whose esophageal dentate line was found to be vague by gastroscopy. (2) Patients who had obvious vomiting during gastroscopy and failed to complete gastroscopy. (3) Gastroscopy shows esophageal abnormalities, affecting the measurement of esophageal length. (4) esophageal manometry shows severe disorder of esophageal movement. (5) Those who cannot lie flat or sit upright due to scleroderma, neck disease or other reasons.
This study was approved by the Hospital Ethics Committee with the patient's consent and informed consent form signed.
The length of gastric tube insertion was the in vivo length from the tip of the nose to the cardia. The manometer was placed into the esophagus through the nasal cavity, and the position of the front end of the manometer in the esophagus was determined according to the waveform obtained from the pressure measurement. Read the scale when the front end of the manometer reaches the junction of esophagus and stomach. This distance is the in vivo length of nasal tip–cardia, and record as NCL (5).
Clinical data of all patients were collected, including gender, age, marital status, height, weight, BMI of the patients before gastric tube insertion, whether the gastric tube was indwelling for the first time, sitting height, sternal length, diagnosis, chest circumference, waist circumference, hip circumference, xiphoid process-navel length, hairline-xiphoid process, nasal tip-earlobe-xiphoid process, earlobe-xiphoid process and the material of gastric tube.
SPSS 21.0 is used to establish the database and analyze the data, and the measurement data is described by . Count data use cases and percentage descriptions, and compare between groups by independent sample t test and one-way ANOVA. Pearson correlation analysis was used to analyze the correlation between NCL length score, height and sitting height. The variables with statistically significant differences between groups after t-test and Chi-square test were used as independent variables, and stepwise regression linear analysis was carried out, and the estimation equation of gastric tube insertion length was established. All analyses are based on 95% confidence intervals. P < 0.05 is statistically significant.
A total of 100 patients were included according to the inclusion and exclusion criteria of research subjects. There 27 females and 73 males. The mean age was (44.27 ± 14.86) years old. There were 55 cases of achalasia of cardia, 7 cases of abdominal pain, 16 cases of Crohn's disease, 9 cases of ulcerative colitis, 8 cases of dysphagia and 5 cases of gastrointestinal bleeding.
As shown in Table 1, the scores of NCL length among patients with different gender, age, marital status, height, weight, BMI, sitting height, sternal length, the length from hairline to xiphoid process, the length of nasal tip–earlobe–xiphoid process, and the length from earlobe to xiphoid process were statistically significant (P < 0.05). The scores of NCL length among patients with different diagnoses, the first indwelling gastric tube, history of hypertension, chest circumference, waist circumference, hip circumference, and the length from xiphoid process to navel, and gastric tube material were not significant (P > 0.05).
The length of NCL is always divided into dependent variables, and the items in general data that affect the length of NCL are included in the regression equation as independent variables. Independent variable assignment is shown in Table 2.
As shown in Table 3, height, sitting height, sex, BMI and the length from earlobe to xiphoid process are the factors that affect NCL length score (P < 0.05). According to the regression principle, an equation is established. At the same time, meaningful variables are screened according to regression analysis. The prediction equation of the gastric tube insertion length estimation method in this study is established as follows: NCL length score = 39.907 + 2.909× height +0.865× sitting height. R2 is 0.506, and the regression equation can explain 50.6% variation degree of dependent variable.
As shown in Table 4 and Figure 1, NCL was positively correlated with height and sitting height. Among them, the correlation with height (r = 0.711, P < 0.001) and sitting height (r = 0.397, P < 0.001).
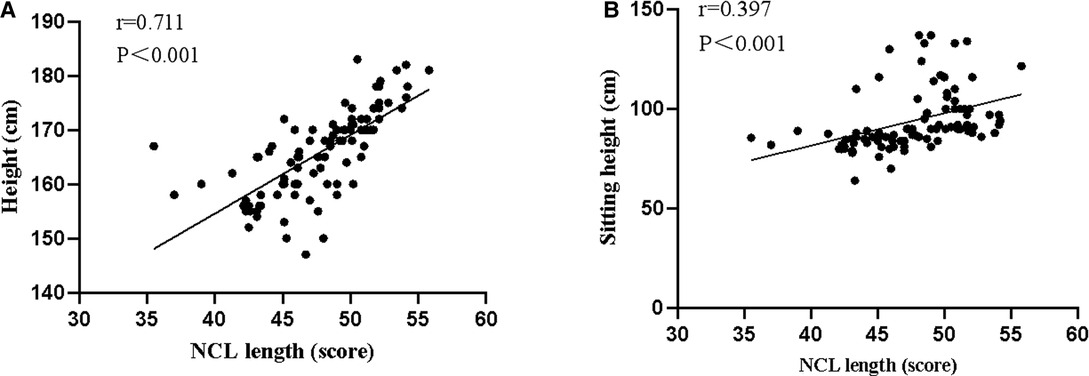
Figure 1. Scatter diagram for correlation analysis of NCL length score with height and sitting height ((A) Correlation analysis of NCL length score and height. (B) Correlation analysis of NCL length score and sitting height).
Gastric tube is a common drainage tube after surgery, its clinical effect has been widely recognized. The shape and size of the stomach are affected by such factors as the gastric volume, the stage of food digestion, the intestinal condition, and the body position. Therefore, although there are many studies on the estimation method of the insertion length of gastric tube in China and abroad, their views have not yet been unified. The lengths of gastric tube recommended by different institutes were different, and the common clinical values include 45–55 cm, 55–65 cm, 55–68 cm, and 55–70 cm (6–8). In addition, the commonly used body surface measurement methods for the length of gastric tube in clinic include the length from nasal tip to earlobe to xiphoid process (NEX), the length from nasal tip to earlobe to navel to the midpoint of xiphoid process (NEMU), the length from hairline to xiphoid process (FX), the length from hairline to navel (FU), and the length from hairline to navel to the midpoint of xiphoid process (FMU) (9–12). However, the determination of the above method is mainly based on the clinical experience of physicians and their observation of the treatment status quo, which is greatly affected by individual differences and has a large possibility of operation error.
The study found that if the actual length of gastric tube placement was taken as the dependent variable Y, the value of Y would not only be affected by such independent variables as height and weight as defined in the study, but also by the instability of its own endpoint. Moreover, the bias of self-endpoint is difficult to control, so it is difficult to establish a relatively stable prediction equation. Therefore, it is difficult to establish a relatively stable prediction equation clinically. Different from the front end of gastric tube, the right side of cardia is wrapped in lesser omentum together with the lower end of esophagus, the front and left sides were covered by peritoneum, and the back is diaphragm esophageal ligament Therefore, although the mobility of the stomach is great, the position of the cardia is relatively fixed (13). So when discussing the length of gastric tube insertion, converting the dependent variable Y to the in vivo length from the nasal tip to the cardia can reduce the bias caused by the movement of the dependent variable's own endpoint and is more conducive to establishing a relatively stable prediction equation. On this basis, NCL was replaced in this study by the in vivo length of the nasal tip-cardia.
It has been suggested that the accuracy of the inserted length is closely related to the prognosis of patients, so it is necessary to analyze the factors affecting the inserted length of gastric tube. The results of this study showed that height, sitting height, gender, BMI and the length from the earlobe to the xiphoid process were the factors that affected the NCL length score (P < 0.05), and height, sitting height and NCL had a positive correlation. Ellett et al. based on the accuracy of children of similar age to the length of gastric tube insertion by comparing their height (ARHB), the length from tip to earlobe to xiphoid process (NEX), and the length from tip to earlobe to navel (NEMU), and found that the height (ARHB) and the length from tip to earlobe to navel (NEMU) were more accurate than the length from tip to earlobe to xiphoid process (NEX) (14). Malta et al. explored the relationship between the distance from the incisors to the gastroesophageal junction (recorded as EGD), height, the distance from the earlobe to the xiphoid process (EX), and other measured values in vitro, and found that height was one of the independent variables with the strongest correlation with EGD (15). Meanwhile, studies have also shown that the height is directly proportional to the length of the gastric tube placement (16), which is similar to the results of this study. The NCL values of patients with different BMI have significant differences. As the height and weight of men are generally higher than those of women, it is believed that there should be differences between men and women in the intubation length (17). Meanwhile, with height and sitting height as independent variables and NCL length as dependent variable, the regression equation was derived: NCL length score = 39.907 + 2.909× height +0.865× sitting height. This further clarified that we could estimate the length of nasogastric tube insertion based on the formula. At the same time, this formula has a certain guiding significance for early calculation of the required length of the catheter for patients, and provides a new reference method for clinical evaluation.
The shortcoming of this study was that the sample size in this study was relatively small, and the formula was not further verified. Therefore, this formula needs to be further corrected. In the future, researchers can conduct multi-center and large sample verification of the correction formula, and achieve individualized nursing operation, thereby improving the therapeutic effect of gastric tube indwelling.
In summary, height, sitting height, gender, BMI and the length from earlobe to xiphoid process are the factors affecting NCL. There is a significant positive correlation between height and sitting height and NCL. On this basis, the length of nasogastric tube insertion can be estimated.
The original contributions presented in the study are included in the article/Suplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by This study was approved by the ethics committee of our hospital. The patients/participants provided their written informed consent to participate in this study.
HZ, HW are the mainly responsible for the writing of the article. XF is mainly responsible for research design. XC is mainly responsible for data analysis. WS is responsible for the guidance of the entire research. The corresponding author is BY, he is responsible for ensuring that the descriptions are accurate and agreed by all authors. All authors contributed to the article and approved the submitted version.
This study was supported by the Natural Science Foundation of Hunan Province (2019JJ50898).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tan JH, Sivadurai G, Tan H, Tan YR, Jahit S, Hans AM. A novel method of nasojejunal feeding and gastric decompression using a double lumen silicone tube for upper gastrointestinal obstruction. Surg Laparosc Endosc Percutan Tech. (2020) 30:106–10. doi: 10.1097/SLE.0000000000000754.
2. Arvanitakis M, Gkolfakis P, Despott EJ, Ballarin A, Beyna T, Boeykens K, et al. Endoscopic management of enteral tubes in adult patients – Part 1: definitions and indications. European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. (2021) 53:81–92. doi: 10.1055/a-1303-7449.
3. Sturrock BR, Fanning SJ, Khan M, Sajid MS. Should nasogastric tube insertion during the COVID-19 pandemic be considered as an aerosol-generating procedure? Br J Hosp Med. (2020) 81:1–6. doi: 10.12968/hmed.2020.0307.
4. Shao X, Tang W, Chen Q, He Y. [Design and application of a new gastrointestinal nutrition pipeline]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2020) 32:611–2. doi: 10.3760/cma.j.cn121430-20200327-00236.
5. O'Connell F, Ong J, Donelan C, Pourmand A. Emergency department approach to gastric tube complications and review of the literature. Am J Emerg Med. (2021) 39:255–9. doi: 10.1016/j.ajem.2020.07.038.
6. Ashouri M, Vezvaei P, Kazemeini A, Sherafati A, Mirfazaelian H. Acute gastric dilation following trauma: a case report. Adv J Emerg Med. (2020) 4:e13. doi: 10.22114/ajem.v0i0.192.
7. Venara A, Hamel JF, Cotte E, Meillat H, Sage PY, Slim K, et al. Intraoperative nasogastric tube during colorectal surgery may not be mandatory: a propensity score analysis of a prospective database. Surg Endosc. (2020) 34:5583–92. doi: 10.1007/s00464-019-07359-9.
8. Song IH. Tension gastrothorax in late-onset congenital diaphragmatic hernia, a rare but life-threatening condition: a case report. Medicine. (2021) 100:e24815. doi: 10.1097/MD.0000000000024815.
9. Tamamori Y, Sakurai K, Kubo N, Yonemitsu K, Fukui Y, Nishimura J, et al. Percutaneous transesophageal gastro-tubing for the management of anastomotic leakage after upper GI surgery: a report of two clinical cases. Surg Case Rep. (2020) 6:214. doi: 10.1186/s40792-020-00965-z.
10. Zhu C, Platoff R, Ghobrial G, Saddemi J, Evangelisti T, Bucher E, et al. What to do when decompressive gastrostomies and jejunostomies are not options? A scoping review of transesophageal gastrostomy tubes for advanced malignancies. Ann Surg Oncol. (2022) 29:262–71. doi: 10.1245/s10434-021-10667-x.
11. Siu W, Chan TT, Tang R. Gastrointestinal: beyond the gastrointestinal tract: emergency endoscopic ultrasound-guided decompression of bronchogenic cyst as a bridge to surgery. J Gastroenterol Hepatol. (2021) 49:456–96. doi: 10.1111/jgh.15750.
12. Naveed M, Jamil LH, Fujii-Lau LL, Al-Haddad M, Buxbaum JL, Fishman DS, et al. American Society for gastrointestinal endoscopy guideline on the role of endoscopy in the management of acute colonic pseudo-obstruction and colonic volvulus. Gastrointest Endosc. (2020) 91:228–35. doi: 10.1016/j.gie.2019.09.007.
13. van Hooft JE, Veld JV, Arnold D, Beets-Tan R, Everett S, Götz M, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: european society of gastrointestinal endoscopy (ESGE) guideline - update 2020. Endoscopy. (2020) 52:389–407. doi: 10.1055/a-1140-3017.
14. Ellett ML, Cohen MD, Perkins SM, Croffie JM, Lane KA, Austin JK. Comparing methods of determining insertion length for placing gastric tubes in children 1 month to 17 years of age. J Spec Pediatr Nurs. (2012) 17:19–32. doi: 10.1111/j.1744-6155.2011.00302.x.
15. Malta MA, Carvalho-Junior AF, Andreollo NA, Freitas MI. [Anthropometric measures for the introduction of the nasogastric tube for enteral nutrition employing the esophagogastroduodenoscopy]. Arq Bras Cir Dig. (2013) 26:107–11. doi: 10.1590/s0102-67202013000200007.
16. Zhang L, Zhu X, He Y, Zhang G. Study on the value of nasogastric tube nutrition nursing in critical patients with indwelling nasogastric tube. Am. J. Transl. Res. (2021) 13(8):9694–700.
Keywords: gastrointestinal decompression, gastric tube insertion, influencing factors, estimation method, insertion length
Citation: Zhang H, Wang H, Fan X, Cao X, Su W and Yang B (2022) Study on Influencing Factors Analysis of Gastric Tube Insertion Length and Construction of Estimation Method. Front. Surg. 9:942881. doi: 10.3389/fsurg.2022.942881
Received: 13 May 2022; Accepted: 13 June 2022;
Published: 11 July 2022.
Edited by:
Weiguo Li, Harbin Institute of Technology, ChinaReviewed by:
Jiangang Liu, The Second Affiliated Hospital of Shandong First Medical University, ChinaCopyright © 2022 Zhang, Wang, Fan, Cao, Su and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Yang NTAzODUxQGNzdS5lZHUuY24=
†These authors share first authorship
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.