
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 01 July 2022
Sec. Obstetrics and Gynecological Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.937371
This article is part of the Research Topic Women in Obstetrics and Gynecology View all 32 articles
Primary vaginal stones have been rarely reported; the reports that do exist are usually case reports. Because of their low incidence, they are often misdiagnosed. This case report and literature review of a primary vaginal stone presents an assessment of symptoms and common risk factors for vaginal stone formation. A 28-year-old woman with spastic quadriplegia who had been bedridden for most of her life presented to the emergency department for abdominal distension and fever. She had chronic constipation, recurrent urinary tract infections (UTIs), and vaginal discharge. Abdominopelvic computed tomography (CT) was performed and a large stone observed. The vaginal stone was completely removed through the vaginal stump after hysterectomy. Differential diagnoses of vesicovaginal fistula, urethrovaginal fistula, genital anomaly, and ectopic ureter were made by performing several tests using indigo-carmine dye. She recovered from surgery without any complications. There was no recurrence of vaginal stones after 3 months. A biochemical analysis reported that the vaginal stone was 100% struvite. Vaginal stones are caused by repeated infections in an environment in which urine collects gradually. Patients with recurrent UTIs who are bedridden should be able to prevent vaginal stones with periodic gynecological examinations for early diagnosis and management.
Vaginal stones are rare and have been presented only in case reports (1). Stones can occur in the kidney, ureter, bladder, gallbladder, and salivary glands; however, they are commonly found in the urinary system (2). Vaginal stones, also called vaginal calculus, are formed by a mechanism similar to that of urinary stones (3). They are classified as primary or secondary depending on the presence or absence of nidus. Primary vaginal stones result from urine stasis in the vagina; however, secondary vaginal stones form as urine crystalizes around foreign bodies in the vagina (4, 5).
There have been several case reports of vaginal stones; however, they have been found sporadically over the course of approximately 80 years. Therefore, we conducted a review of case reports published in English after the 2000s. While reviewing these case reports, paralyzed patients who spent most of their time bedridden accounted for a high proportion of vaginal stone cases. We aimed to contribute to the knowledge of the origin of vaginal stones among bedridden patients and to prevent this disease by reviewing the literature and sharing our case.
A 28-year-old woman presented with fever and abdominal distension to our tertiary hospital emergency department. Abdominopelvic contrast-enhanced computed tomography (CECT) was performed to find the cause of the fever, and a large, hard mass was observed in the vagina (Figure 1). Therefore, she was referred to the gynecology department. The patient was living in a social welfare facility because she had no relatives. Therefore, her caregiver, who was a staff member at the facility, had limited knowledge of the patient's family history and medical history. The caregiver told us that the patient had chronic constipation, recurrent urinary tract infections (UTIs), and vaginal discharge with odor for a prolonged time. The patient had quadriplegia as a result of cerebral palsy when she was young and had undergone laparotomy for peritonitis at approximately 7 years of age. She had severe mental and motor disabilities, joint contractures involving the lower and upper limbs, and spasticity. She spent most of her time bedridden in a supine position and defecating in diapers. Both ovaries and the uterus were normal according to CECT, and there was a 9.3 cm × 8 cm × 6 cm mass compressing the rectum between the bladder and colon; therefore, we suspected that the stone was inside the vagina (Figure 1). During physical examination, her abdomen was distended, her external genitalia was normal, and her hymen was intact. Vaginal discharge was mucoid, yellowish-gray, and had an unpleasant odor. During the speculum examination, a stone-like mass was found within the vagina. Because of her fever, bacteriuria, and pyuria, our diagnosis was UTI accompanied by a vaginal calculus. Proteus vulgaris and Streptococcus anginosus were found in her urine culture. The UTI was treated antibiotics. We consulted with a urologist and decided to use Holmium laser lithotripsy to cut the vaginal stone into pieces so it could be removed through the vaginal opening. Under general anesthesia, we placed her in the lithotomy position and tried to cut into the vaginal stone with Holmium laser lithotripsy for about 6 h and 45 min; however, the stone was too hard. Consequently, surgery was ended without removing the vaginal stone. She recovered well from surgery and was discharged approximately 1 week later. However, during her follow-up examination at the clinic, it was observed that an edge of the broken stone had stabbed the vaginal wall, resulting in bleeding and inflammation. The secretion worsened and the UTI recurred. After discussion with one of her caregivers, we decided to remove the vaginal stone by performing hysterectomy through laparotomy after treating UTI with antibiotics and daily vaginal irrigation. Under general anesthesia, hysterectomy was performed with a low-midline incision in the lithotomy position. After hysterectomy, the stone was carved out of the vaginal stump using a small drill for approximately 1 h (Figure 2). The vaginal stone was completely removed (Figure 3). To rule out other causes of vaginal stone formation during surgery, the vaginal wall was inspected closely after injection of intravenous indigo-carmine dye. We did not find an ectopic ureter or fistula. The patient was discharged without complications 10 days after surgery. Her caregiver was instructed to maintain the patient's posture upright at least twice per day and to visit the gynecology clinic periodically to prevent the recurrence of vaginal stones. Three months after surgery, the patient had no vaginal stone or UTI recurrence. The vaginal stone weighted 600 g. The biochemical analysis indicated that it comprised 100% struvite.
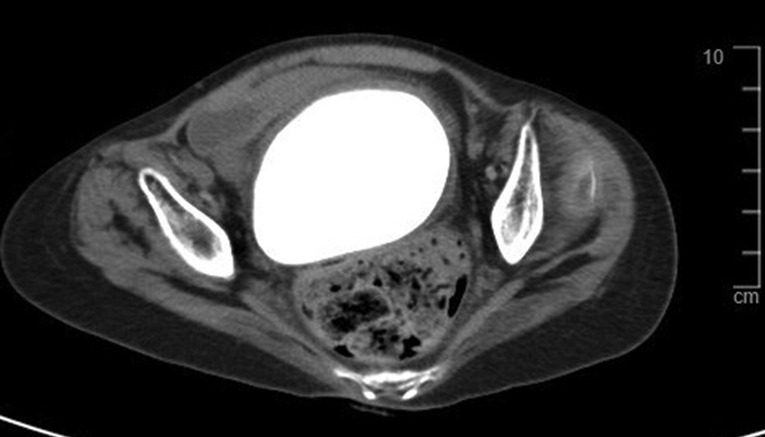
Figure 1. Computed tomography (axial view) show 9.3 cm × 8.0 cm high density mass with smooth margin between bladder and rectum.
We searched PubMed and EMBASE for primary vaginal stones and primary vaginal calculus. The search was limited to articles published from January 1, 2000 to March 30, 2022. We included pediatric articles; however, we excluded articles related to secondary vaginal stones. The relevant data summarized in Table 1 were extracted from the case report descriptions. The ages of the patients ranged was from 4 to 69 years. Of a total of 24 patients, 14 presented with urogenital defects or anomalies such as vesicovaginal fistula, urethrovaginal fistula, and vaginal outlet obstruction. Ten out of 24 patients were bedridden with paraplegia or tetraplegia (42%). The periods when patients were bedridden ranged from 5 years to 42 years. The correlation between the length of the bedridden period and the vaginal stone size was not significant. Most case reports included urinary incontinence and recurrent UTIs. Nonspecific symptoms such as fever and stone passage were observed in children and paralyzed individuals. The main causes of vaginal stones are described in Table 1. In 22 of the 24 case reports, urine stagnation was the main cause of vaginal stones. The two excluded case reports, which included vaginal outlet obstruction, assumed that the cause of the vaginal stone was of hematic origin. Among the 24 case reports, six did not describe the stone composition. Forteen of the eighteen case reports that described the composition of the vaginal stones reported that they contained struvite. Other reported components of the stones were carbonate apatite, calcium phosphate, oxalate, and hemosiderine. They were found simultaneously with struvite in three case reports. Four of the 18 case reports that described the composition of vaginal stones did not indicate that the stones contained struvite. In three of the 24 case reports, vaginal stones were removed transperitoneally; in the remaining 21 case reports, episiotomy or hymenectomy was performed to remove the stones vaginally.
The occurrence of vaginal stones is rare and has been reported only in case reports since 1926 (6). Most of the vaginal stones reported so far comprised struvite. Struvite is composed of magnesium ammonium phosphate. It is formed by a combination of two factors: decreased urine volume and infection with bacterial species such as Proteus, Staphylococcus, Pseudomonas, and Klebsiella, which increase the urine pH by producing urease (7, 8). Many of the case reports classified vaginal stones as primary or secondary according to the presence or absence of a nidus (6). Secondary vaginal stones are caused by repeated infections caused by foreign bodies such as an intrauterine device (5), surgical gauze (9), or mesh (10) that act as the nidus and promote mineral accumulation. In contrast, primary vaginal stones do not have a nidus. Related case reports are listed in Table 1.
We reviewed the case reports of primary vaginal stones published since 2000. The majority of the case reports described urine stasis in the vagina and recurrent UTIs, which might be important risk factors for the formation of vaginal stones. Vesicovaginal fistula, urethrovaginal fistula, urogenital sinus anomaly, and genital anomaly cause urinary retention in the vagina. Of 25 cases reports (including our case report), 14 cases involved a urogenital anatomic abnormality such as a vaginal outlet obstruction, fistula, or urogenital sinus anomaly. Notably, 11 of the 24 patients reported (including our patient) were bedridden for a long period of time because of disability. In other words, patients with a vaginal stone seem to be bedridden for long periods or have a genitourinary malformation. In particular, the lying position can result in urine retention that is severe enough to form a fistula. During surgery of our patient, we found that the bladder capacity was approximately 50 ml, which is approximately 10-times smaller than that of the adult bladder. Presumably, dissonance between contraction of the bladder detrusor muscle and the urethral sphincter causes decreased bladder capacity and leads to urine leakage. Leaked urine passes through the vaginal wall and stagnates in the vaginal cavity, thus leading to bacterial colonization in the stagnant urine. Because Proteus species proliferate in urine, and because the urine pH was 9 in our patient, the infected urine passed to the vagina, resulting in urease production and an alkaline vaginal environment. Ureolysis caused by urease increases ammonia and bicarbonate, thus creating a supersaturated state and resulting in struvite crystal formation (8). Because the enlarged vaginal stone pressed the bladder, the bladder became atrophied, and urine leakage became more frequent. Because the stone remained in the vagina, more frequent UTIs occurred. The patient had no history of child birth, and the stump was expected to be too small after hysterectomy to remove the vaginal stone through laparotomy; therefore, we attempted to remove it through vaginal extraction. However, Holmium laser lithotripsy was unsuccessful because the stone was difficult to break. The second surgery confirmed that our prediction was wrong. The stump and vaginal wall, which were exposed after hysterectomy, were sufficiently dilatated; therefore, the vaginal stone was cut into pieces (Figures 2, 3).
This case report and literature review had several limitations. The vaginal stone in this case did not undergo culture testing; hence, it was inferred through urine culture testing that it was not the primary cause of bacteria. Because only case reports were reviewed and there was no control group for comparison, we could not estimate the general incidence of vaginal stones among nonimmobilized patients or accurately define the risk factors for vaginal stones.
Vaginal stones are rare and have been described only by reports. Therefore, we reviewed other case reports to contribute to the knowledge of vaginal stones in immobilized patients. These patients present to the hospital with nonspecific symptoms because they are not able to express their discomfort or pain. If patients with immobility have recurrent UTIs, then clinicians should perform simple radiography or consult a gynecologist to confirm or dismiss the diagnosis of vaginal stones and prevent their complications.
When treating bedridden patients, especially those with recurrent UTIs, it is necessary to consider the possibility of vaginal stones because their symptoms are not specific. For women, a gynecologic examination and simple radiography should be considered.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the patients and caregiver for the publication of any potentially identifiable images and data included in this article.
JJ drafted the work, obtained the data, performed searches and analyses, and completed most of the writing. SL and WC prepared radiographic images. JS contributed to the conception and substantively revised the manuscript. IC was responsible for revising the manuscript and its knowledge content. All authors contributed to the article and approved the submitted version.
We would like to thank Editage (www.editage.co.kr) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Castellan P, Nicolai M, De Francesco P, Di Tizio L, Castellucci R, Bada M, et al. Primary vaginal calculus in a woman with disability: case report and literature review. J Endourol Case Rep. (2017) 3(1):182–5. doi: 10.1089/cren.2017.0100
2. Rodgers AL, Spector M. Human stones. Endeavour. (1981) 5(3):119–26. doi: 10.1016/0160-9327(81)90044-2
3. Malhotra N, Kumar S, Roy KK, Agarwal R, Verma V. Vaginal calculus secondary to vaginal outlet obstruction. J Clin Ultrasound. (2004) 32(4):204–6. doi: 10.1002/jcu.20015
4. Oguzkurt P, Ince E, Ezer SS, Temiz A, Demir S, Hicsonmez A. Primary vaginal calculus secondary to urethrovaginal fistula with imperforate hymen in a 6-year-old girl. J Pediatr Surg. (2009) 44(7):e11–3. doi: 10.1016/j.jpedsurg.2009.03.040
5. Aronson SL, Hovius MC, Janszen EWM. Large primary vaginal stone in a woman with multiple sclerosis. BMJ Case Rep. (2020) 13(10):e235103. doi: 10.1136/bcr-2020-235103
6. Navani S, Tessier PA. A primary vaginal stone. Br J Radiol. (1970) 43(507):222–3. doi: 10.1259/0007-1285-43-507-222
7. Vella M, Karydi M, Coraci G, Oriti R, Melloni D. Pathophysiology and clinical aspects of urinary lithiasis. Urol Int. (2007) 79(Suppl. 1):26–31. doi: 10.1159/000104438
9. Patankar S, Dobhada S, Bhansali M. Vesicovaginal fistula with secondary vaginal stones. J Laparoendosc Adv Surg Tech. (2006) 16(4):386–9. doi: 10.1089/lap.2006.16.386
10. Griffiths KM, Towers GD, Yaklic JL. Vaginal urinary calculi formation secondary to vaginal mesh exposure with urinary incontinence. Case Rep Obstet Gynecol. (2017) 2017:1–3. doi: 10.1155/2017/8710315
11. Yoshimura T, Nagata Y, Matsuura K, Okamura H. Primary vaginal stone in an 11-year-old recumbent girl. Gynecol Obstet Invest. (2000) 50(1):64–6. doi: 10.1159/000010283
12. Bar-Moshe O, Oboy G, Assi J. Vaginal calculi in a young woman. Eur Urol. (2000) 37(4):505–7. doi: 10.1159/000020176
13. Plaire JC, Snodgrass WT, Grady RW, Mitchell ME. Vaginal calculi secondary to partial vaginal outlet obstruction in pediatric patients. J Urol. (2000) 164(1):132–3. doi: 10.1016/S0022-5347(05)67478-2
14. Cetinkurşun S, Surer I, Demirbag S, Oztürk H. A primary vaginal stone in a disabled child. Obstet Gynecol. (2001) 98(5 Pt 2):978–9. doi: 10.1097/00006250-200111001-00038
15. Ergün SS, Babalioglu R, Aydin S, Ozmen N, Sidal B, Koser RM. Vaginal stones with a pinpoint hymenal opening. Arch Gynecol Obstet. (2002) 266(1):58–9. doi: 10.1007/pl00007503
16. Lin C-J, Chen C-P, Wu C-H, Chen H-Y, Hsu H-H. Huge primary vaginal stone in a recumbent woman. Taiwan J Obstet Gynecol. (2005) 44(1):80–2. doi: 10.1016/S1028-4559(09)60114-5
17. Ho TC, Lin IL. Primary vaginal stone in a young active woman. Taiwan J Obstet Gynecol. (2008) 47(4):457–9. doi: 10.1016/s1028-4559(09)60019-x
18. Liu B, Huang X, Lu J, Zhang Z, Wang P, Huang Z. Vaginal calculi secondary to urethrovaginal fistula with vaginal stenosis in a 14-year-old girl. Urol Res. (2008) 36(1):73–5. doi: 10.1007/s00240-007-0129-x
19. Urbanowicz W, Szymik-Kantorowicz S, Sulisławski J, Wolnicki M. Primary vaginal stone in a disabled child. Cent European J Urol. (2010) 63(4):187–9. doi: 10.5173/ceju.2010.04.art4
20. Jaspers JW, Kuppens SM, van Zundert AA, de Wildt MJ. Vaginal stones in a 5-year-old girl: a novel approach of removal. J Pediatr Adolesc Gynecol. (2010) 23(1):e23–5. doi: 10.1016/j.jpag.2009.05.006
21. Chen S, Ge R, Zhu L, Yang S, Wu W, Yang Y, et al. Giant primary vaginal calculus secondary to vesicovaginal fistula with partial vaginal outlet obstruction in a 12-year-old girl. Urology. (2011) 78(4):908–10. doi: 10.1016/j.urology.2011.01.026
22. Avsar AF, Keskin HL, Catma T, Kaya B, Sivaslioglu AA. A large primary vaginal calculus in a woman with paraplegia. J Low Genit Tract Dis. (2013) 17(1):61–5. doi: 10.1097/LGT.0b013e31824d6f9c
23. Ikeda Y, Oda K, Matsuzawa N, Shimizu K. Primary vaginal calculus in a middle-aged woman with mental and physical disabilities. Int Urogynecol J. (2013) 24(7):1229–31. doi: 10.1007/s00192-012-1902-0
24. Gunes A, Uygun I. Is every stone urinary stone? A rare case of stone. Pediatr Urol Case Rep. (2014) 1(2):18–20. doi: 10.14534/PUCR.201424453
25. Tokgöz Y, Erdem AO, Özbey BC, Terlemez S. A rare reason in a child with feeding intolerance: intravaginal struvite stone. Turk J Pediatr. (2018) 60(1):86–8. doi: 10.24953/turkjped.2018.01.013
26. Wei D, Xie Y, Niu X. Vaginal stones caused by urethrovaginal fistula: a case report. Medicine (Baltimore). (2019) 98(47):e18003. doi: 10.1097/md.0000000000018003
27. Xu Q, Zou Y. Primary vaginal calculus in a woman with urogenital sinus anomaly: a case report. BMC Urol. (2020) 20(1):142. doi: 10.1186/s12894-020-00708-0
28. Fedrigon D, Bretschneider CE, Muncey W, Stern K. Removal of large primary vaginal calculus using the nephroscope and endoscopic ultrasonic lithotrite: a case report. J Endourol Case Rep. (2020) 6(2):92–5. doi: 10.1089/cren.2019.0099
29. Ranawaka RS, Goyal A, Shabani A, Hennayake S, Dickson AP, Cervellione RM. Novel approach to vaginal calculus in a girl with urogenital sinus anomaly. J Pediatr Surg. (2020) 55(9):e4–5. doi: 10.1016/j.jpedsurg.2012.07.033
Keywords: vaginal stone, spastic quadriplegia, primary vaginal calculus, struvite, recurrent urinary tract infections (rUTIs)
Citation: Jo JY, Lee SM, Shin JK, Choi WJ and Cho IA (2022) Huge vaginal stone: Case report and review of the literature. Front. Surg. 9:937371. doi: 10.3389/fsurg.2022.937371
Received: 6 May 2022; Accepted: 16 June 2022;
Published: 1 July 2022.
Edited by:
Isabella Fabietti, Bambino Gesù Children’s Hospital (IRCCS), ItalyReviewed by:
Giacomo Maria Pirola, Ospedale San Donato di Arezzo, Italy© 2022 Jo, Lee, Shin, Choi and Cho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: In Ae Cho ZGV3ODI3NEBoYW5tYWlsLm5ldA==
Specialty section: This article was submitted to Obstetrics and Gynecological Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.