RETRACTED: Commentary: Computational Analysis for ERAS and Other Surgical Processes: Commentary From Clinical Perspective
- 1The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 2Department of Orthopedics, Hunan Provincial People’s Hospital (The First-Affiliated Hospital of Hunan Normal University), Changsha, China
Objective: In order to better understand the relative surgical process, this work used a model-based computational analysis on the effectiveness of enhanced recovery after surgery (ERAS) in the operating room with nursing.
Methods: A total of 360 surgical patients in the First Affiliated Hospital, Sun Yat-sen University, from the period June 2020 to March 2021, were randomly divided into two groups, namely, observation group and control group, with 180 cases in each group. Routine nursing was used in the control group, while ERAS was implemented in the observation group from the point of view of four aspects, namely, preoperative visit, intraoperative cooperation, postoperative return visit, and psychological intervention.
Results: Postoperative complications, average hospital stay, nursing satisfaction, and postoperative quality of life in the observation group were significantly better than those in the control group (all p < 0.05).
Conclusion: The application of ERAS for surgical patients can enhance team awareness, optimize the process of cooperation, reduce surgical complications and improve nursing quality, and prognosis, and it is worth popularizing in the operating room.
Introduction
Surgery refers to the treatment that doctors use with knives, scissors, needles, and other medical instruments to cut off and sew parts of the human body to maintain or even save the patient’s health. This surgical treatment is commonly known as “operation”. The purpose is to treat or diagnose diseases to improve the body’s function and shape, such as removing diseased tissues (1, 2), repairing injuries (3, 4), and organ transplantation (5, 6). Early surgery is limited to cutting and suturing on the body surface by simple manual methods such as abscess drainage, tumor resection, and trauma suturing. With the development of surgery, the field of surgery has been expanding, and today, it can be performed in any part of the human body (7–10). In addition, it has been reported that surgery has greater efficacy than non-surgical treatments in curing some human diseases (11, 12).
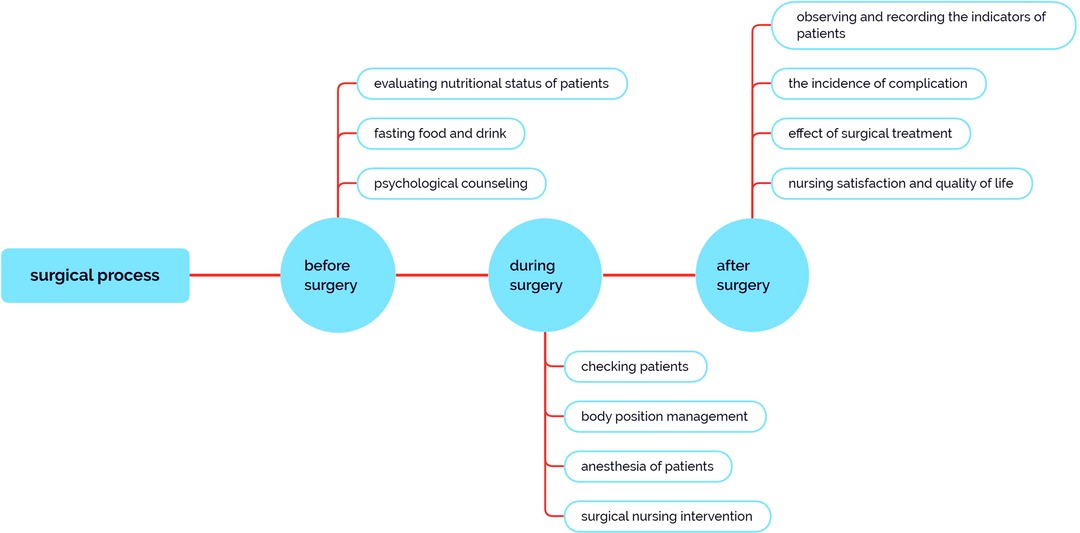
However, various intraoperative complications and postoperative complications may occur due to injury, bleeding, or infection caused by surgical treatment (13–15). In addition, when patients undergo surgery, they have to experience the stimulation of anesthesia and surgical trauma. Their body will be in a state of stress, which will lead to both psychological and physiological burden (16). Therefore, some kind of good and effective perioperative nursing is required to provide patients with holistic physical and mental care so that they can successfully spend their perioperative period in the best frame of mind (Figure 1). Such nursing also plays an extremely important role in preventing or reducing postoperative complications (17).
The theory of Enhanced Recovery after Surgery (ERAS) was proposed systematically by Danish surgeon Professor Kehlet (18) for the first time in 1997, which refers to the adoption of a series of perioperative optimization measures with evidence-based medical evidence to block or reduce the stress response of the body. It can promote the accelerated recovery of patients after surgery and achieve the purpose of shortening the patient’s hospitalization time so as to reduce postoperative complications and also the risk of readmission and death (19). It has been verified that ERAS has a very positive application (20, 21). The purpose of this study is to research and analyze the effect of ERAS on perioperative nursing and provide a reference for further study.
Materials and Methods
General Description
A total of 360 (223 males and 137 females) surgical patients in the First Affiliated Hospital, Sun Yat-sen University, from the period June 2020 to March 2021, were selected as the research objects. All the selected patients underwent elective surgery, following which all of them could actively cooperate with perioperative nursing guidance. The whole study was carried out with the informed consent of these patients and approved by the hospital ethics committee.
All patients were randomly divided into two groups, 180 in each group. Of these, 118 males and 62 females with age ranging from 61 to 78 years and an average of (62.50 ± 15.60) years were in the observation group, in which ERAS was implemented in the form of preoperative visit, intraoperative cooperation, postoperative return visit, and psychological intervention. A total of 105 males and 75 females with age ranging from 51 to 81 years and an average of (62.70 ± 14.60) years were in the control group, in which routine nursing was implemented. There was no significant difference between the two groups in the general data such as gender, age, and gastrointestinal diseases (all p < 0.05), which indicated that they were comparable in this study.
Materials
Routine Nursing
The control group was given routine nursing care. Preoperative nursing was carried out for the purpose of education. Patients were required to fast for 8–12 h and abstain from drinking for 4 h (7). After entering the operating room, the patients were checked, and venous access was established. After general anesthesia, the patients were placed in the operating position. They could eat after anal exhaust, the complications of which were observed and recorded.
ERAS Pathway
The observation group received routine nursing and the corresponding nursing intervention combined with ERAS, including preoperative nursing, operation room nursing, and postoperative nursing, which are described in the following paragraphs.
In the ERAS pathway, good preoperative preparation and psychological nursing play a key role in the smooth conduct of operation. Nurses should visit patients 1 day before operation and give them appropriate diet and psychological nursing.
2.2.2.1.1Surgery is an invasive operation, which causes serious psychological burden to patients. Anxiety is a common psychological condition of patients before surgery. Psychological counseling should be done well before surgery to enhance the confidence of patients during surgery.
2.2.2.1.2The self-care ability of the patients were evaluated according to the inputs provided by the patients in the self-care ability evaluation form. Self-care ability was divided into four levels, namely, no dependence, mild dependence, moderate dependence, and severe dependence. The self-care ability of these levels was evaluated as none needed for care, a few needed care, most needed care, and all needed care, respectively. Dynamic evaluation was made according to the changes in the patients’ condition and nursing levels, and corresponding nursing measures such as secondary care, primary care, and special care were implemented.
2.2.2.1.3The nutritional status of the patients was evaluated. Patients without gastrointestinal motility disorder were required to fast solid food for 6 h and liquid food for 2 h before operation. They were required to take two bottles of “Suqian beverage” (a kind of maltose fructose drink made in China) of approximately 800 ml orally at 22:00 and one bottle of approximately 400 ml 2 h before operation. Reducing the hunger, thirst and anxiety of patients can lower the incidence of postoperative nausea and vomiting, which will accelerate their recovery.
The bladder of the patients should be confirmed empty while the nurse brings them into the operating room. An equilibrium liquid of approximately 30 drops/min was given to the patients after confirming the standby state of the indwelling needle and slowly dripping it for maintenance (22, 23). The roving nurse and the workers jointly verified the general information of the patients and handed over their intraoperative medication, imaging data, special supplies, and medical records. After signing the printed operation handover form, the patients were sent to the operating room.
The patients were under anesthesia during the operation. Excessive blood loss and fluid loss may be caused by long operation time and trauma. Therefore, it is highly important to implement operating room nursing intervention in the ERAS pathway. The infusion channel should be reasonable, and the appropriate venous catheter should be selected. In case of significant blood loss and fluid loss during the operation, the large-diameter venous channel and central venous catheters anti-infection catheter should be selected and the three-way pipe should be managed well. It is reported that the pollution rate of the three-way pipe during the operation can reach 23%. The integrated board was used to prevent infection. In addition, body position management should be standardized. The exposed field should be convenient for the operator to conduct the operation. The body should be placed gently and the functional position should be maintained after the body is placed. Personalized body position should be adopted to avoid skin damage and nerve damage. Physical preventive measures such as elastic socks and intermittent pressurizing devices can be used to avoid low blood volume. A specialist group should be set up, with a specialist nurse as the team leader. Daily staff should be arranged by the specialist group every day. Operational materials should be prepared well according to the doctor’s instructions, and the staff should actively cooperate with the surgeons to shorten the operation time.
The patients went back to the ward after anesthesia. Evaluation and handover were made according to the observation record sheet of the anesthesia recovery room (PACU). The handover contents mainly include the following: identity confirmation, vital signs, consciousness, respiration, circulation, oxygen saturation, the patient’s limb mobility, oral and lip color, infusion, urinary catheter, medication, drainage and wound dressing, and skin.
Observation Indicators
The incidence of postoperative complications, treatment effect, nursing satisfaction, and quality of life were compared between the two groups (22–24). According to the questionnaire of patient satisfaction in the operating room developed by our hospital, the patients scored on the spot to judge their nursing satisfaction during the postoperative return visit. Satisfaction rate = very satisfied + satisfied (the total number of people).
Statistical Method
SPSS 26.0 statistical software was used to analyze the data. The measurement data were expressed by average and the t-test was used. The counting data were expressed by percentage (%) and the X2 test was used. The difference was statistically significant (p < 0.05).
Results and Discussions
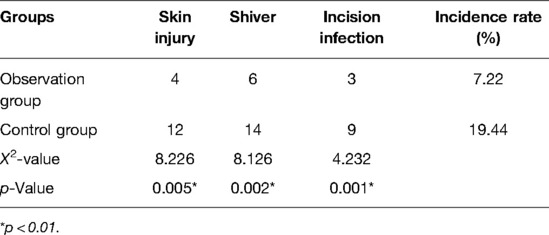
As shown in Table 1, complications such as skin injury, shiver, and incision infection occurred in both groups, which include 13 cases in the observation group (7.22%) and 35 cases in the control group (19.44%). The number of patients with complications in the observation group was significantly less than those in the control group, which indicated better nursing effect on ERAS (p < 0.05). One of the concepts of ERAS is to reduce the incidence of postoperative complications and promote the recovery of patients’ physical and psychological health (25), which is consistent with the results in Table 1. Nursing staff made a comprehensive evaluation of the preoperative visits of the patients in the observation group before the operation. The infusion pipeline was well managed during the operation, and the operation position was correctly placed to prevent hypothermia. In addition, a series of nursing interventions to prevent deep vein thrombosis and control incision infection were adopted, which significantly reduced the complication rate of the patients.
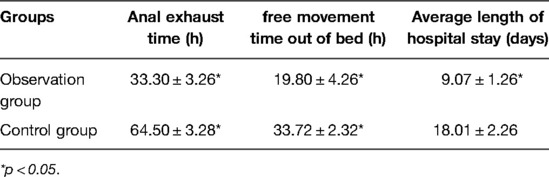
Generally, surgical patients experienced moderate and severe pain. Good postoperative analgesia can relieve their tension and anxiety. In the ERAS pathway, a return visit was made to correctly evaluate the patients’ pain after the operation. It is beneficial for wound healing and will speed up recovery if analgesia is given in a preventive, timely, and multimode manner (26). ERAS has been shown to allow patients to move out of bed sooner (27, 28) and reduce the length of stay in hospital (29, 30). From Table 2, it can be seen that the patients in the observation group were significantly better than those in the control group in terms of exhaust time, free movement time out of bed, and average length of hospital stay (p < 0.05), which showed consistency with the previous report.
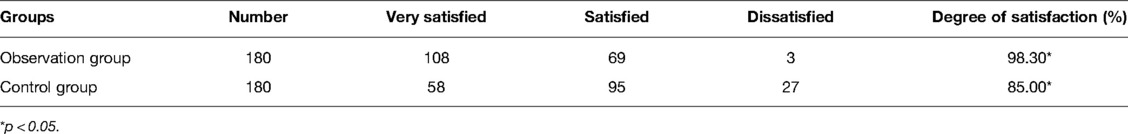
As shown in Table 3, patients’ satisfaction with nursing in the observation group (98.30%) was significantly higher than that in the control group (85.00%), and the difference was statistically significant (p < 0.05). Compared with patients who underwent routine nursing, the time of fasting food and drink of those who adopted ERAS was shortened. The patients’ hunger, panic, and fear caused by long-term fasting were avoided. Effective communication with the patients was made before the operation. The patients could more clearly understand the purpose and time of fasting so that they could more actively cooperate during the perioperative period. Therefore, nursing satisfaction was improved (31).
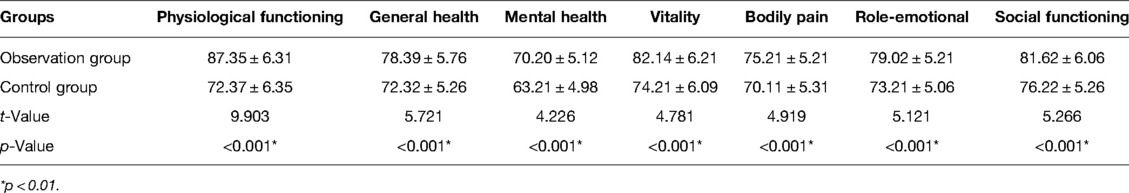
Quality of life was positively correlated with the score. The higher the total scores, the higher the quality of life. As shown in Table 4, the scores of quality of life after nursing in the observation group were significantly higher than those in the control group (p < 0.05) after psychological intervention. It was reported that ERAS can significantly improve patients’ mental health and physical health, which was basically consistent with the conclusion in Table 4 of this study (32). Moreover, psychological intervention can improve the patient compliance following the ERAS after operation.
Conclusions
In this study, the effects of routine nursing and ERAS on perioperative nursing were compared. The results indicated that the ERAS pathway can not only reduce postoperative complications and shorten the length of hospital stay, but also improve patients’ quality of life. From this study, we can see that for patients, the application of the ERAS theory during the perioperative period can shorten the operation time and reduce their postoperative complications so as to improve the prognosis and enhance their overall satisfaction with the quality of care. For surgeons, ERAS can enhance the awareness of the operation team and optimize the operation process of cooperation, which is worth popularizing.
With the development of medical technology, minimally invasive surgery and precise medications have led to fewer contraindications for surgical treatment. Surgery, as the main method of invasive treatment, has a great impact on the status of patients’ psychology and physiology. In order to alleviate patients’ anxiety and fear before operation, improve nursing quality, and reduce postoperative complications, operating room nursing staff are required to keep pace with the times and garner new ideas to serve patients. However, due to a wide range of departments involved in ERAS, multiteam and multidisciplinary assistance are required. In our study, ERAS proved to be an effective way to help patients recover quickly and comprehensively, thus providing a good reference and theoretical basis for studying ERAS and changing traditional nursing concepts to devise more effective nursing measures.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author/s.
Author Contributions
WL and SH conceptualized and designed the study and wrote the first draft of the manuscript. YX, GC, and JY were involved in data collection and analysis. YY contributed in terms of manuscript revision, reading, and project management. All authors contributed to the article and approved the submitted version.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical approval for this work was obtained from The Ethical Review Committee of The First Affiliated Hospital, Sun Yat-sen University. The patients/participants provided their written informed consent to participate in this study.
Acknowledgments
The work is supported by The First Affiliated Hospital, Sun Yat-sen University, and the Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University). This study was supported by the Natural Science Foundation of Hunan Province (2021JJ70016), Hunan University Reform and Development Fund (2021CZT01), Hunan University Reform and Development Fund (2020CZT01), and Educational Reform of Degree and Graduate Education in Hunan Normal University (18JG20).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yin X, Duan H, Yi Z, Lu R, Li C, Li L. Clinical characteristics, surgical treatment, and risk factor analysis of postoperative functional outcome in patients with intracranial hemangioblastoma. World Neurosurg. (2022) 161:e427–35. doi: 10.1016/j.wneu.2022.02.027
2. Obeidat RF, Masri MA, Marzouq M. Factors affecting Jordanian women’s surgical treatment decisions for early-stage breast cancer. Asia Pac J Oncol Nurs. (2021) 8(6):711–9. doi: 10.4103/apjon.apjon-20105
3. Yang YP, Ma X, An H, Liu XP, An N, Ao YF. Meniscus repair with simultaneous anterior cruciate ligament reconstruction: clinical outcomes, failure rates and subsequent processing. Chin J Traumatol. (2022) 25(1):37–44. doi: 10.1016/j.cjtee.2021.09.005
4. Labarre C, Graveleau N, Bouguennec N. Meniscal ramp lesions repair: an under-meniscus all-inside suture in cases of isolated meniscotibial ligament tears. Arthrosc Tech. (2021) 10(6):e1417–24. doi: 10.1016/j.eats.2021.02.005
5. Rosenthal LL, Ulrich SM, Zimmerling L, Brenner P, Müller C, Michel S, et al. Pediatric heart transplantation in infants and small children under 3 years of age: single center experience—“early and long-term results”. Int J Cardiol. (2022) 356:45–50. doi: 10.1016/j.ijcard.2022.04.002
6. Heindl LM, Riss S, Laaser K, Bachmann BO, Kruse FE, Cursiefen C. Split cornea transplantation for 2 recipients—review of the first 100 consecutive patients. Am J Ophthalmol. (2011) 152(4):523–32. doi: 10.1016/j.ajo.2011.03.021
7. Seo D, Jo H, Jeong HG, Kim YD, Lee SU, Ban SP, et al. Simultaneous craniotomies for multiple intracranial aneurysm clippings—one-stage surgery with multiple craniotomies. World Neurosurg. (2022) 158:689–96. doi: 10.1016/j.wneu.2021.11.045
8. Shetye B, Hamilton FR, Bays HE. Bariatric surgery, gastrointestinal hormones, and the microbiome: an Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022. Obes Pillars. (2022) 2(2022):100015. doi: 10.1016/j.obpill.2022.100015
9. Matsuo K, Klar M, Ciccone MA, Nusbaum DJ, Shimada M, Roman LD, et al. Incorporation of sentinel lymph node biopsy in cervical cancer surgery: recent U.S. trends. Eur J Surg Oncol. (2022) S0748–S7983(22):00112–3. doi: 10.1016/j.ejso.2022.02.018. [Epub ahead of print]
10. Shu HT, Mikula JD, Yu AT, Shafiq B. Tranexamic acid use in pelvic and/or acetabular fracture surgery: a systematic review and meta-analysis. J Orthop. (2021) 28:112–6. doi: 10.1016/j.jor.2021.11.018
11. Jia Y, Peng Z, Qin Y, Wang G. Surgical versus nonsurgical treatment for adult spinal deformity: a systematic review and meta-analysis. World Neurosurg. (2022) 159:1–11. doi: 10.1016/j.wneu.2021.12.017
12. Lemke J, Cammerer G, Ganser J, Scheele J, Xu P, Sander S, et al. Survival and prognostic factors of colorectal liver metastases after surgical and nonsurgical treatment. Clin Colorectal Cancer. (2016) 15(4):183–92. doi: 10.1016/j.clcc.2016.04.007
13. Purwoto G, Dalimunthe BE, Kekalih A, Aditianingsih D, Mazni Y, Wahyudi I, et al. Complications of ovarian cancer surgery in Dr. Cipto Mangunkusumo National Referral Hospital, Jakarta: a cross-sectional study. Ann Med Surg. (2022) 77:103581. doi: 10.1016/j.amsu.2022.103581
14. Rahm C, Adok C, Dahm-Kähler P, Bohlin KS. Complications and risk factors in vulvar cancer surgery—a population-based study. Eur J Surg Oncol. (2022) S0748–7983(22):00079–8. doi: 10.1016/j.ejso.2022.02.006. [Epub ahead of print].
15. Rodriguez AN, Schleck K, LaPrade RF. Complications of medial and lateral knee surgery and how to best avoid them. Oper Tech Sports Med. (2022):150914. doi: 10.1016/j.otsm.2022.150914
16. Moisak GI, Amelina EV, Zubok NA, Rzaev JA. Psychological status before and after surgery in patients with trigeminal neuralgia. Clin Neurol Neurosurg. (2021) 203:106578. doi: 10.1016/j.clineuro.2021.106578
17. Goktas S, Gezginci E, Oymaagaclio K. Adaptation of the person-centered perioperative nursing scale to Turkish: a validity and reliability analysis. J Perianesth Nurs. (2022) S1089–9472(21):00450–0. doi: 10.1016/j.jopan.2021.12.009. [Epub ahead of print]
18. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. (1997) 78(5):606–17. doi: 10.1093/bja/78.5.606
19. Smith TW Jr, Wang X, Singer MA, Godellas CV, Vaince FT. Enhanced recovery after surgery: a clinical review of implementation across multiple surgical subspecialties. Am J Surg. (2020) 219(3):530–4. doi: 10.1016/j.amjsurg.2019.11.009
20. Lu Y, Yuan Z, Han Y, Zhang Y, Xu R. Summary of best evidence for enhanced recovery after surgery for patients undergoing lung cancer operations. Asia Pac J Oncol Nurs. (2022). doi: 10.1016/j.apjon.2022.03.006
21. Jensen BT, Retinger NL, Lauridsen SV. From fast-track to enhanced recovery after surgery (ERAS) in radical cystectomy pathways—a nursing perspective. Asia Pac J Oncol Nurs. (2022). doi: 10.1016/j.apjon.2022.02.010
22. Smith TW Jr, Wang X, Singer MA, Godellas CV, Vaince FT. Enhanced recovery after surgery: a clinical review of implementation across multiple surgical subspecialties. Review Am J Surg. (2020) 219(3):530–4. doi: 10.1016/j.amjsurg.2019.11.009
23. Stumpo V, Staartjes VE, Quddusi A, Corniola MV, Tessitore E, Schröder ML, et al. Enhanced recovery after surgery strategies for elective craniotomy: a systematic review. J Neurosurg. (2021):1–25. doi: 10.3171/2020.10.JNS203160. [Epub ahead of print]
24. Seow-En I, Wu J, Yang L, Tan J, Seah A, Foo FJ, et al. Results of a colorectal enhanced recovery after surgery (ERAS) programme and a qualitative analysis of healthcare workers’ perspectives. Asian J Surg. (2021) 44(1):307–12. doi: 10.1016/j.asjsur.2020.07.020
25. Ripollés-Melchor J, Abad-Motos A, Cecconi M, Pearse R, Jaber S, Slim K, et al. Association between use of enhanced recovery after surgery protocols and postoperative complications in colorectal surgery in Europe: the EuroPOWER international observational study. J Clin Anesth. (2022) 80:110752. doi: 10.1016/j.jclinane.2022.110752
26. Band IC, Yenicay AO, Montemurno TD, Chan JS, Ogden AT. Enhanced recovery after surgery protocol in minimally invasive lumbar fusion surgery reduces length of hospital stay and inpatient narcotic use. World Neurosurg: X. (2022) 14:100120. doi: 10.1016/j.wnsx.2022.100120
27. Ifrach J, Basu R, Joshi DS, Flanders TM, Ozturk AK, Malhotra NR, et al. Efficacy of an enhanced recovery after surgery (ERAS) pathway in elderly patients undergoing spine and peripheral nerve surgery. Clin Neurol Neurosurg. (2020) 197:106115. doi: 10.1016/j.clineuro.2020.106115
28. Young R, Cottrill E, Pennington Z, Ehresman J, Ahmed AK, Kim T, et al. Experience with an enhanced recovery after spine surgery protocol at an academic community hospital. J Neurosurg Spine. (2021) 34(4):680–7. doi: 10.3171/2020.7.SPINE20358
29. Xiao SM, Ma HL, Xu R, Yang C, Ding Z. Enhanced recovery after surgery protocol for elderly gastric cancer patients: a prospective study for safety and efficacy. Asian J Surg. (2022) S1015–9584(21):00703–X. doi: 10.1016/j.asjsur.2021.10.040. [Epub ahead of print]
30. Brusko GD, Kolcun J, Heger JA, Levi AD, Manzano GR, Madhavan K, et al. Reductions in length of stay, narcotics use, and pain following implementation of an enhanced recovery after surgery for 1- to 3-level lumbar fusion surgery. Neurosurg Focus. (2019) 46(4). doi: 10.3171/2019.1.FOCUS18692
31. Liu VX, Rosas E, Hwang J, Cain E, Foss-Durant A, Clopp M, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. (2017) 152(7):171032. doi: 10.1001/jamasurg.2017.1032
32. Yu Y, Li M, Kang R, Liu X, Wang N, Zhu Q, et al. The effectiveness of telephone and Internet-based supportive care for patients with esophageal cancer on enhanced recovery after surgery in China: a randomized controlled trial. Asia Pac J Oncol Nurs. (2022) 9(4):217–28. doi: 10.1016/j.apjon.2022.02.007
Keywords: surgery, operating room nursing, enhanced recovery after surgery, complication, satisfaction
Citation: Li W, Huang S, Xie Y, Chen G, Yuan J and Yang Y (2022) Model-Based Computational Analysis on the Effectiveness of Enhanced Recovery after Surgery in the Operating Room with Nursing. Front. Surg. 9:922684. doi: 10.3389/fsurg.2022.922684
Received: 18 April 2022; Accepted: 25 April 2022;
Published: 18 May 2022.
Edited by:
Weiguo Li, Harbin Institute of Technology, ChinaReviewed by:
Zhengqiu Li, Hunan Children’s Hospital, ChinaYunrun Liu, Hong Kong Baptist University, Hong Kong SAR, China
Copyright © 2022 Li, Huang, Xie, Chen, Yuan and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Yang MTE3MDU4MDk4MkBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Wenji Li1†
Wenji Li1† Shu Huang
Shu Huang Yun Yang
Yun Yang