
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 11 October 2022
Sec. Genitourinary Surgery and Interventions
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.922158
Objective: This pilot study aimed to assess the practicability and effectiveness of percutaneous nephrolithotomy (PCNL) with vacuum-assisted nephrostomy sheaths for patients under modified local anesthesia (m-LA).
Methods: PCNL with a vacuum-assisted nephrostomy sheath under m-LA was performed in 83 patients between November 2020 and May 2021. An 18F or 20F ClearPetra Nephrostomy Sheath connected vacuum aspiration was used in surgery to keep low pressure in the renal pelvis. For LA, lidocaine and ropivacaine hydrochloride were 1:1 mixed and instilled under ultrasound guidance through the percutaneous nephrolithotomy channel directed toward the design calix. Demographic characteristics, stone characteristics, visual analogue scale (VAS) score, vital signs, operation time, complications, and stone clear rate were recorded and analyzed.
Results: All operations were completed. The mean VAS score was 3.9 ± 1.0. The mean operation time was 55.1 ± 23.6 min. The changes for systolic blood pressure, diastolic blood pressure, and heart rate were 3 ± 21 mmHg, 1 ± 14 mmHg, and −6 ± 14 beats/min, respectively. The change for hemoglobin was −10.7 ± 10.9 g/L. The change for C-reactive protein was 5.39 ± 43.1 mg/L. The total stone-free rate was 69.9% (93.8% for simple stones and 54.9% for complex stones).
Conclusion: Performing PCNL with vacuum-assisted nephrostomy sheaths under modified local anesthesia under ultrasound guidance was found to be strongly practical and effective.
Percutaneous nephrolithotomy (PCNL) is a minimally invasive treatment for some indicated renal stones and upper ureteral calculi. Guidelines recommend PCNL as the preferential treatment modality for all renal stones >20 mm owing to the increased stone-free rate and reduced re-treatment sessions (1). Mini tract size, vacuum suction, and other technological advances in PCNL improved the safety and effectivity, broaden the application, and enhanced recovery after surgery (2, 3). Apart from these developments, the method of anesthesia was a key point that affects the safety and recovery of patients. The American Society of Anesthesiologists (ASA) classification is a system in which patients are evaluated according to the risk of anesthesia before surgery. ASA-I represents a completely healthy patient, ASA-II represents a patient with mild systemic disease, ASA-III represents a patient with severe systemic disease that is not incapacitating, ASA-IV represents a patient with incapacitating disease that is a constant threat to life, and ASA-V represents a moribund patient who is not expected to live for 24 h with or without surgery. This system could be used to choose the type of anesthesia and to assess the tolerance of patients to various surgical manipulations such as surgical position. Staying in a prone position during PCNL could lead to some difficulties, such as those in controlling the airway and maintaining the vascular access and ventilation of patients with lung diseases (4).
Generally, PCNL is performed under general anesthesia (GA); however, comorbidities such as coronary heart disease and chronic obstructive pulmonary disease increase the risk of anesthesia (5). GA also deferred the recovery from surgery and increased the economic burden (6), increasing the research focus on local anesthesia (LA) in PCNL for decades (7–11). LA offers many advantages compared with other methods of anesthesia, as it minimally affects patients’ physiological status leading to their enhanced recovery (12). In this study, we used a vacuum-assisted nephrostomy sheath to keep low pressure in the renal pelvis and suck out the stone fragments. We modified the LA (m-LA) that was previously reported (7, 13, 14) and performed precise local anesthesia in a percutaneous nephrolithotomy channel under ultrasonic guidance; it was convinced that eventual capsular puncture site was the same spot the anesthesia needle is inserted. We performed m-LA for patients with ASA score I–III, and we also compared the practicability and effectiveness of this new procedure for different ASA score. Data on visual analogue scale (VAS) score, vital signs, operation time, complications, and stone clear rate were recorded and analyzed.
Between November 2020 and May 2021, 83 cases that met the criteria were enrolled in the study. Inclusion criteria were (1) renal stone larger than 2 cm, (2) upper ureteral calculi larger than 1 cm, and (3) the patient was willing to receive local anesthesia. Exclusion criteria were (1) concomitant middle or lower ureteral calculi, (2) stone secondary to ureteral stricture, (3) second-stage operation, (4) BMI >30 kg/m2, and (5) local anesthesia drug allergies. Patients routinely received urinalysis, urine culture, routine blood test, serum creatinine, and electrolyte test. Upper urinary calculi were diagnosed by ultrasound, kidney, ureter, bladder x-ray, and CT scans. Simple stones refer to single renal or ureteral stones, and complex stones refer to multiple stones, except in patients with anatomical abnormalities. In addition, complex stone included staghorn calculi.
Antibiotics including latamoxef or etimicin were administered to patients 30 min before the operation. The patient was in the prone position, and precise local anesthesia in the percutaneous nephrolithotomy channel was performed under ultrasonic guidance; the key points were (1) 1% lidocaine 10 ml and 1% ropivacaine hydrochloride 10 ml were mixed for local injection, lidocaine had rapid onset, but short effectiveness, ropivacaine had a long-term effect, and the mixture giving full play of merits. (2) A 20GA 1.88IN venous indwelling needle [Singapore Becton Dickinson Medical (S) Pte Limited] with a 20 ml syringe was used for drugs injection, with the fine needle relieving the injection pain. (3) The injection of anesthetic was along the percutaneous nephrolithotomy channel under ultrasonic guidance (Noblus, Hitachi, Ltd.), and anesthesia reached the renal fascia. (4) Using an 18F or 20F ClearPetra Nephrostomy Sheath (Cat No: 90121617, 90121817, Well Lead Medical Co., Ltd) in surgery to keep low pressure in the renal pelvis can avoid distending pain in the kidney. (5) No ureteral catheter was inserted in any of the patients; it can avoid the pain caused by inserting a ureteral catheter, and furosemide (20 mg) would be given by injection into a vein to form artificial hydronephrosis, which was convenient for puncture.
Other procedures were routinely performed as previously reported (8), and some were modified accordingly (15, 16). After anesthesia, percutaneous punctures using an 18-gauge needle (Cat No: G01377, Cook Medical) were guided by ultrasound in the channel. After removing the needle core, the guidewire was inserted into the collecting system through the needle, the skin was incised, and the needle was removed with recording the depth. A 12F or 14F fascial dilator was applied for dilation and entered the depth of the earlier record. The ureteroscope (8/9.8F) was moved to the renal pelvis following the guidewire to confirm channel passage through the renal papilla. An 18F or 20F ClearPetra Nephrostomy Sheath was subsequently placed into the channel. The stone was fragmented by a high-power holmium laser (2.5 J × 35 Hz); fragments were pushed out by an endoscopic pulsed perfusion pump and vacuum aspiration (Figure 1). Finally, a 4.7F or 6F double-J stent was inserted in the ureter; a nephrostomy tube was used depending on inflammation, residual stones, and hemorrhage.
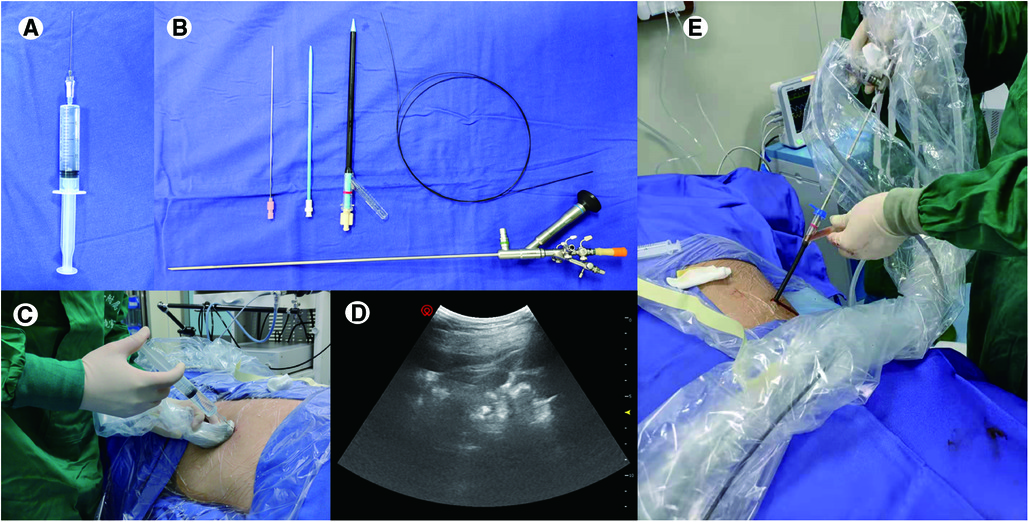
Figure 1. Main instruments and operation procedures of percutaneous nephrolithotomy for modified local anesthesia. (A) 1% lidocaine 10 ml and ropivacaine hydrochloride 10 ml were mixed for local injection, and a 20GA 1.88IN venous indwelling needle [Singapore Becton Dickinson Medical (S) Pte Limited] with a 20 ml syringe was used for drug injection. (B) An 18-gauge needle was used for percutaneous punctures, a 12F or 14F fascial dilator was applied for dilation, and an ureteroscope (8/9.8F) was for laser lithotripsy. (C,D). The injection of anesthetic was along the percutaneous nephrolithotomy channel under ultrasonic guidance. (E) An 18F or 20F ClearPetra Nephrostomy Sheath was used for the establishment of a percutaneous renal channel; the lateral channel of the sheath connected with negative suction ensures intrapelvic low pressure and stone fragments were easy to flush out.
The demographic characteristics that included sex, age, size of the stone, location of the stone (single stone in renal or ureter was recorded as simple, others were complex), and comorbidity (chronic obstructive pulmonary disease, cardiovascular disease, etc.) of the patients were recorded. The surgery data that included the tract number, duration of the operation, systolic blood pressure (SBP), heart rate (HR), and VAS scores were evaluated. Postoperative evaluations were drop in hemoglobin, fever, perirenal hematoma, pleural effusion, residual stone, length of hospital stay, medical cost, and Barthel index. An x-ray of KUB was taken after one day after surgery. We defined stone-free rate as the radiological absence of stone in asymptomatic patients with residual stone fragments <3 mm (17). Blood pressure and heart rate were recorded before surgery, and the highest and lowest values were recorded during the operation.
The characteristics of included patients are listed in Table 1. A total of 52 men and 31 women received m-LA for PCNL. The mean age was 53.6 ± 13.9 years. Nine patients had hypertension, 6 had diabetes, 2 had paraplegia, 10 had coronary heart disease, and 7 had poor pulmonary function. Preoperative SBP was 133 ± 20 mmHg, and diastolic blood pressure (DBP) was 83 ± 12 mmHg, heart rate was 79 ± 11 beats/min, and the body mass index was 23.4 ± 4 kg/m2. Patients with ASA score I–III were 51, 17, and 15, respectively. The mean hemoglobin was 130 ± 20 g/L, and the mean C-reactive protein (CRP) was 15.3 ± 32.9 mg/L. A total of 32 cases were simple stones, and 51 cases were complex stones. The size of the stone was 19.4 ± 8.1 mm.
The mean VAS score was 3.9 ± 1.0. The mean operation time was 55.1 ± 23.6 min. The postoperative hospital stay was 4.1 ± 1.2 days. The changes for SBP, DBP, and heart rate were 3 ± 21 mmHg, 1 ± 14 mmHg, and −6 ± 14 beats/min, respectively. The change for hemoglobin was −10.7 ± 10.9 g/L. The change for C-reactive protein was 5.39 ± 43.1 mg/L. There were 64, 17, and 2 patients who received 1, 2, and 3 tracts, respectively. It was noted that 55, 26, and 2 patients retained 0, 1, and 2 nephrostomy tubes. One patient received a blood transfusion and renal arterial embolization, and there was no Clavien grade IV–V complications. The total stone-free rate was 69.9%, which was 93.8% for simple stones and 54.9% for complex stones. The main clinical results of the patients are listed in Table 2.
Subgroup analysis was performed according to ASA status; the patient's perioperative status is recorded in Table 3. Sex, BMI, type of stone, VAS score, stone-free rate, preoperative SBP, DBP, hemoglobin, CRP, duration, tract number, and postoperative SBP, DBP, HR, and CRP showed, no significant differences among the ASA-I–III patients. Patients were younger in the ASA I group, and postoperative hemoglobin was higher. However, hemoglobin change showed no significant difference.
Local anesthesia broadens the indications for PCNL. It hedged risks caused by deformity (chest and spine), and poor heart and lung function; meanwhile, the renal function may be maximum preserved (5, 14). Other advantages were obvious, such as reduced medical cost, short hospitalization time, less influence on patients’ physiological functions, and faster recovery (12, 13). In this study, we modified the LA to perform precise local anesthesia, through which we wanted to control pain throughout the surgery.
Previous reports about LA in PCNL were improvable (8, 10, 18, 19). The characteristics of LA are listed in Table 4, and progresses in our study were noticed in the methods. First, patients received premedication such as pethidine or promethazine 0.5–1 h before surgery as in a previous study; we did not apply these drugs to avoid possible side effects. Second, the local anesthetic was lidocaine or ropivacaine in a previous study, which cannot reconcile rapid onset and long duration; the mixture combined the advantages of both. Third, we applied a ClearPetra Nephrostomy Sheath rather than a Peel-Away Sheath; the new sheath could effectively control intrarenal pressure and reduce pain in surgery. Fourth, we performed precise LA (i.e., injection of anesthetics in percutaneous nephrolithotomy channel under ultrasonic guidance), which maximized the anesthetic effect. Finally, for some patients with none or mild hydronephrosis, the usage of furosemide can avoid retrograde ureteral catheterization. Thus, we modified LA and assessed its practicability and effectiveness.
In our study, m-LA in PCNL achieved satisfactory results. All operations were completed successfully, and none of m-LA was converted to GA; we continuously communicated with patients during the operation to monitor pain, and local anesthetics can be added for analgesia during the operation. For some stones with large angles, the stone clearing rate may be sacrificed to complete the operation. No serious cardiovascular incident occurred, no death occurred, and postoperative rehabilitation was satisfactory. The pain was evaluated using a VAS score. The mean VAS score was 3.9 ± 1.0, and the pain levels during the operation were mild and could be tolerated, which was similar to previous reports (8, 10). Our method had advantages compared with other research studies (12). The vital signs were not reported by previous studies. Our research recorded the heart rate and blood pressure during surgery, and results showed that the indexes were changed within a limited range, indicating m-LA had a minor impact on hemodynamics.
Other parameters also evaluated the effect of surgery. Operation times were 55.1 ± 23.6 min. One patient felt discomfort and discontinued surgery because of keeping a long-time prone position; due to the lack of preoperative preparation of jejunitas, the patient was not converted to GA. He received a II-stage operation under m-LA on the second day, and the stone was removed. The total stone-free rate was 69.9%, which was 93.8% for simple stones and 54.9% for complex stones. It seems that the total stone-free rate was inferior to what was previously reported (20); the reason may be complex stones were the majority (61.4%) in this research. Complications were seldom, Clavien grade IV–V complications, and injury in the renal collecting system did not occur in our group; however, transfusion was needed for one patient. The mean hemoglobin change was −10.7 ± 10.9 g/L. The important skill to reduce complications relied on precise ultrasonic guidance, not only performing m-LA but also choosing the puncture site, to avoid bleeding and organ injury. Owing to the complication reduction and rapid recovery, hospital stay was only 4.1 ± 1.2 days.
Our study did not simply duplicate the work of our predecessors, and the key points for our study are listed as follows. First, although obesity was not a contraindication, obese patients were not encouraged for PCNL under m-LA, although data indicated that BMI was not associated with VAS score (the Pearson coefficient was 0.113, P = 0.309). The swing of the sheath was restricted and increased pain. Second, patients with renal stones in the polar calix were not included for the same reason. Third, we recommended two-step puncture techniques for PCNL (15). It reduced pain caused by re-dilation procedures and ensured the channel through renal papillae. Fourth, ClearPetra Nephrostomy Sheath was important for reducing intrarenal pressure and distending pain because it was of Y type to connect with vacuum aspiration, and the use of ordinary sheath should control the pump to limit the intrarenal pressure. Fifth, this was the first time to analyze the vital signs and the changes in PCNL under m-LA, and we found that m-LA did not significantly alter the blood pressure and heart rate. Sixth, previous studies did not assess the practicability and effectiveness of LA for patients according to ASA score, and our research indicated that m-LA was safe for ASA-III patients.
The main limitation of our study was the limited population. Some previous reports about LA contained hundreds or thousands of patients (8, 9), and a larger number would be needed to verify our procedures. In addition, the results were concluded from one single center, and we planned to extend the technique to assess the practicability and effectiveness. Nevertheless, we provided an innovation for percutaneous nephrolithotripsy under local anesthesia.
Performing PCNL with a vacuum-assisted nephrostomy sheath under modified local anesthesia under ultrasound guidance was found to be strongly practical and effective.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Nanchang University. The patients/participants provided their written informed consent to participate in this study.
HX and JH designed the study. YY, JH, WL, ZP, MW, and XZ performed the research. YY, JH, WL, and HX analyzed the data. JH wrote the paper. All authors contributed to the article and approved the submitted version.
This study was funded by the Project of the Education Department of Jiangxi Province (GJJ180007), supported by Jiangxi Provincial Natural Science Foundation (No: 20202BAB216033, 20212BAG70001), and Key Research and Development Program of Jiangxi Province (20171ACB20029).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hughes T, Ho HC, Pietropaolo A, Somani BK. Guideline of guidelines for kidney and bladder stones. Turk J Urol. (2020) 46(Supp. 1):S104–12. doi: 10.5152/tud.2020.20315 33052834
2. Deng J, Li J, Wang L, Hong Y, Zheng L, Hu J, et al. Standard versus mini-percutaneous nephrolithotomy for renal stones: a meta-analysis. Scand J Surg. (2020) 110(3):301–11. doi: 10.1177/1457496920920474
3. Saidian A, Nix JW. Enhanced recovery after surgery: urology. Surg Clin North Am. (2018) 98(6):1265–74. doi: 10.1016/j.suc.2018.07.012
4. Kisa E, Yucel C, Budak S, Ucar M, Keskin MZ, Cakmak O, et al. The effect of the American Society of Anesthesiology classification scores on complications associated with percutaneous nephrolithotomy. Arch Ital Urol Androl. (2018) 90(2):112–6. doi: 10.4081/aiua.2018.2.112
5. Zhai J, Wang H, Xu X, Liu Z, Man L. PCNL in COPD patient in the sit position under local infiltration anesthesia case report. BMC Urol. (2020) 20(1):70. doi: 10.1186/s12894-020-00640-3
6. Ranjan R, Malviya D, Misra S, Nath SS, Rastogi S. To compare the changes in hemodynamic parameters and blood loss during percutaneous nephrolithotomy—general anesthesia versus subarachnoid block. Anesth Essays Res. (2020) 14(1):72–4. doi: 10.4103/aer.AER_14_20
7. Özdilek A, Beyoğlu ÇA, Demirdağ Ç, Şen Ö, Erbabacan ŞE, Ekici B, et al. Perioperative analgesic effects of preemptive ultrasound-guided subcostal transversus abdominis plane block for percutaneous nephrolithotomy: a prospective, randomized trial. J Endourol. (2020) 34(4):434–40. doi: 10.1089/end.2019.0766
8. Li H, Xu K, Li B, Chen B, Xu A, Chen Y, et al. Percutaneous nephrolithotomy under local infiltration anesthesia: a single-center experience of 2000 Chinese cases. Urology. (2013) 82(5):1020–5. doi: 10.1016/j.urology.2013.07.007
9. Ecke TH, Barski D, Weingart G, Lange C, Hallmann S, Ruttloff J, et al. Presentation of a method at the exploration stage according to IDEAL: percutaneous nephrolithotomy (PCNL) under local infiltrative anesthesia is a feasible and effective method—retrospective analysis of 439 patients. Int J Med Sci. (2017) 14(4):302–9. doi: 10.7150/ijms.17963
10. Aravantinos E, Karatzas A, Gravas S, Tzortzis V, Melekos M. Feasibility of percutaneous nephrolithotomy under assisted local anaesthesia: a prospective study on selected patients with upper urinary tract obstruction. Eur Urol. (2007) 51(1):224–7, discussion 228. doi: 10.1016/j.eururo.2006.06.027
11. Dalela D, Goel A, Singh P, Shankhwar SN. Renal capsular block: a novel method for performing percutaneous nephrolithotomy under local anesthesia. J Endourol. (2004) 18(6):544–6. doi: 10.1089/end.2004.18.544
12. Wang X, Ye Q, Liu X, Chen J, Wang Z, Xu W, et al. Comparison of the clinical efficacy of sonography-guided percutaneous nephrolithotomy (PCNL) under local and general anesthesia. J Int Med Res. (2019) 47(9):4143–50. doi: 10.1177/0300060519859767
13. Chen K, Xu K, Li B, Wang S, Xiang S, Li H. Predictive factors of stone-free rate and complications in patients undergoing minimally invasive percutaneous nephrolithotomy under local infiltration anesthesia. World J Urol. (2020) 38(10):2637–43. doi: 10.1007/s00345-019-03070-5
14. Yu Z, Lin W, Xu A, Liu C, Li H, Huang P. Percutaneous nephrolithotomy under local infiltration anesthesia in kneeling prone position for a patient with spinal deformity. Acta Med Okayama. (2020) 74(2):175–8. doi: 10.18926/amo/58278
15. Yu X, Xia D, Peng EJ, Yang H, Li C, Yuan HX, et al. Clinical investigation of ultrasound-guided percutaneous nephrolithotomy accessed by SVOF-principle and two-step puncture techniques. Zhonghua Waike Zazhi [Chin J Surg]. (2018) 56(10):764–7. doi: 10.3760/cma.j.issn.0529-5815.2018.10.012
16. Xiong J, Shi Y, Zhang X, Xing Y, Li W. Chinese one-shot dilation versus sequential fascial dilation for percutaneous nephrolithotomy: a feasibility study and comparison. Urol J. (2019) 16(1):21–6. doi: 10.22037/uj.v16i1.4610
17. Kumar A, Vasudeva P, Nanda B, Kumar N, Das MK, Jha SK. A prospective randomized comparison between shock wave lithotripsy and flexible ureterorenoscopy for lower caliceal stones ≤2 cm: a single-center experience. J Endourol. (2015) 29(5):575–9. doi: 10.1089/end.2013.0473
18. Chen Y, Zhou Z, Sun W, Zhao T, Wang H. Minimally invasive percutaneous nephrolithotomy under peritubal local infiltration anesthesia. World J Urol. (2011) 29(6):773–7. doi: 10.1007/s00345-011-0730-z
19. Dundar G, Gokcen K, Gokce G, Gultekin EY. The effect of local anesthetic agent infiltration around nephrostomy tract on postoperative pain control after percutaneous nephrolithotomy: a single-centre, randomised, double-blind, placebocontrolled clinical trial. Urol J. (2018) 15(6):306–12. doi: 10.22037/uj.v0i0.4145
Keywords: modified local anesthesia, percutaneous nephrolithotomy (PCNL), ASA—American Society of Anesthesiologists, physical status, renal stone
Citation: Yu Y, Hu J, Liu W, Peng Z, Wang M, Zhou X and Xi H (2022) Performing percutaneous nephrolithotomy under modified local anesthesia. Front. Surg. 9:922158. doi: 10.3389/fsurg.2022.922158
Received: 17 April 2022; Accepted: 16 September 2022;
Published: 11 October 2022.
Edited by:
Christian P. Meyer, Ruhr University Bochum, GermanyReviewed by:
Chaohui Gu, First Affiliated Hospital of Zhengzhou University, China© 2022 Yu, Hu, Liu, Peng, Wang, Zhou and Xi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haibo Xi MTM4NzA4MzQ1NzhAMTYzLmNvbQ== Jieping Hu aHVfamllcGluZ0AxNjMuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.