- 1Department of Traumatology, Hand and Reconstructive Surgery, University Medical Centre Rostock, Rostock, Germany
- 2Department of Pediatrics, University Medical Centre Rostock, Rostock, Germany
- 3Department of Diagnostic and Interventional Radiology, Pediatric Radiology and Neuroradiology, University Medical Centre Rostock, Rostock, Germany
Background: Surgical reconstruction of anterior cruciate ligament ruptures is a well-established procedure, and although it is for the vast majority of patients without severe complications, total knee joint arthroplasty, arthrodesis of the knee, and finally transfemoral amputation have to be considered in the worst-case scenario.
The case: We report a case of a patient with a 13-year history of recurrent failure after anterior cruciate ligament reconstruction. She claimed she had severely impaired mobility secondary to a knee joint arthrodesis via an Ilizarov circular frame 2 years ago and chronic immobilizing pain, making a permanent medication with opioids necessary. She was aware of the therapeutic options and asked for transfemoral amputation and concomitant supply with a transcutaneous osseointegrated prosthesis system (TOPS).
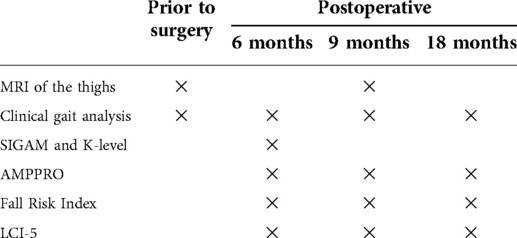
Procedures: After careful evaluation and clinical work-up, the indication for transfemoral amputation and concomitant implantation of the prosthetic stem into the femoral cavity was secured. Six weeks after the creation of the stoma for coupling of the artificial limb and onset of physiotherapy, balance and gait training were scheduled. Full weight-bearing and walking without crutches were allowed 12 weeks after the index procedure. This sequence of events was paralleled by a series of pre-defined examinations, that is, questionnaires and mobility scores addressing the situation of transfemoral amputees, as well as standardized clinical gait analysis. The latter was performed before surgery and 6, 9, and 18 months after the index procedure.
Outcome: At the time of the index procedure, opioids could be tapered to zero, and the patient quickly regained her walking abilities during the rehabilitation period. Clinical gait analysis confirmed the restoration of bilateral symmetry by mutual approximation of kinematics and kinetics to a standard gait pattern.
Conclusion: The outcome of our patient strengthens the therapeutic potential of a unilateral transfemoral amputation in combination with TOPS. Nevertheless, long-term follow-up is necessary to detect future complications of this approach.
Introduction
Anterior cruciate ligament (ACL) ruptures are among the most common knee injuries, and surgical reconstruction generally allows for return to pre-injury level of activity in 75%–97% of patients (1). However, failure of the procedure and severe complications such as persistent functional impairments, osteoarthritis, chronic pain, and deep infections may occur in a reasonable number of patients (1). In the worst-case scenario, total knee joint arthroplasty, arthrodesis of the knee, and transfemoral amputation have to be considered as salvage procedures (2, 3). Although the latter option is irreversible by nature, it has the potential to restore functional abilities if performed properly, that is, surgery and fitting with an artificial leg (4). In general, coupling between the artificial leg and the residual limb is achieved by the use of an individually designed socket and corresponding liner to ensure optimal fit and transfer of force required for walking with the artificial leg. Apart from problems related to force transmission, socket-related problems such as skin irritations ranging up to ulcerations, excessive sweating, time-consuming donning, and doffing are commonly noted [for a review, see other studies (5–9)]. During the last two to three decades, transcutaneous bone-anchored osseointegrated prosthesis systems (TOPS) have become a reliable alternative for rehabilitation, especially for patients with recurrent problems associated with the socket (7–11). While the risk of recurrent infections due to the transcutaneous implant turned out to be much lower than expected, switching from socket prosthesis to a bone-anchored one is associated with numerous advantages ranging from improved rehabilitation and autonomous mobility up to the restoration of osseoperception (7, 8, 10, 11). Apart from differences regarding the geometry, the retention as well as the bone- and skin-implant interfaces, and the abutment for connection of the exoprosthesis, the principle of function is always the same (12).
Case report
We report on a case of a 31-year-old woman who presented with a knee joint arthrodesis and an almost non-functioning leg, impeding her mobility and the care for her two children, ages 2 and 4 years, respectively. Clinical work-up revealed a 13-year history (Figure 1A) of recurrent failure following ACL reconstruction and numerous surgical interventions due to recalcitrant deep joint infection ending up with a knee joint arthrodesis via an Ilizarov circular frame (Figure 1A). Despite proven osseous fusion of the arthrodesis employing CT scanning, the patient suffered from immobilizing pain making a permanent medication with opioids necessary. In addition, signs and symptoms of early degenerative joint disease were already present in the contralateral hip. She was pretty well-informed on the rehabilitative power of a transfemoral amputation, especially when combined with a bone-anchored prosthesis. Given the clinical findings and the explicit wish of the patient, an elective transfemoral amputation with concomitant implantation of a bone-anchored prosthesis as well as a panel of follow-up examinations to evaluate rehabilitation and outcome even in the perception of the patient was consented (Table 1).
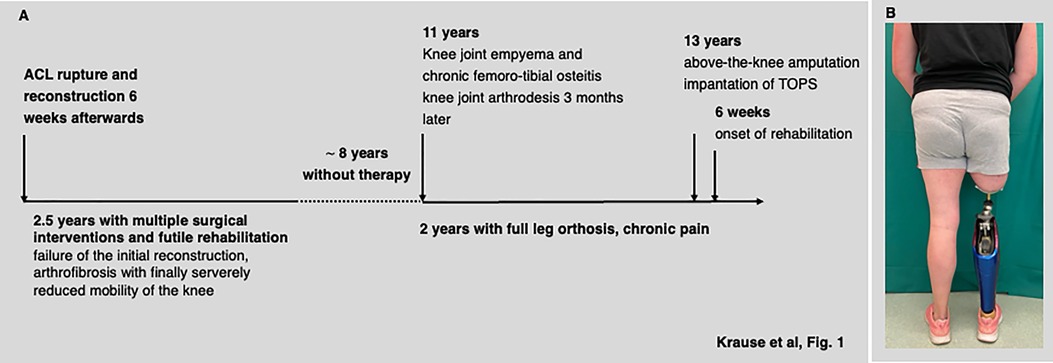
Figure 1. History of disease (A) and a photograph of the patient 18 months after switching to transcutaneous osseointegrated prosthesis system (TOPS) (B).
Surgical procedures and supportive treatment
The patient received preoperative routine antibiotic prophylaxis with a third-generation cephalosporin 30 min before induction of general anesthesia. The dysfunctional leg was dissected 25 cm below the greater trochanter, at a level determined by the length and diameter of the implant. During the preparation of the residual femur, multiple tissue samples were taken from the intramedullary canal for microbiological testing, and all of them scored negative. The femoral stem (Eska Orthopaedics, Lübeck, Germany) with a size of 15 mm × 180 mm (diameter × length) was driven into the medullary canal, and a tight press-fit was achieved (7). The muscles of the thigh were cut and shaped to avoid perspective interference with the prosthetic stem adaptor. The postoperative course was uneventful and, most interestingly, the patient was free of pain almost immediately after surgery in that opioids could be tapered to zero within less than 4 weeks. About 6 weeks after the first surgery the stoma of the TOPS was created using a specific circular punch. The skin-perforating bridging connector was attached to the femoral component essentially as described (7) and conventional means of postsurgical analgesics were employed. Starting the second postoperative day, the patient was instructed about daily self-care of the stoma, that is, to clean it twice daily with mild soap and water (7). Furthermore, she was equipped with a prosthesis, consisting of a microprocessor-controlled knee (Genium ×3, Otto Bock, Duderstadt, Germany) with a low-weight prosthetic foot (Taleo, Otto Bock, Duderstadt, Germany). She was encouraged to start walking with crutches to ensure partial weight-bearing of initially 5–10 kg. Full weight-bearing and walking without crutches were allowed about 6 weeks after the second surgery. Physiotherapy, gait, and balance training were initiated once she had received the prosthesis and was continued for about 4 months in order to restore her walking abilities (Figure 1B).
Clinical gait analysis and questionnaires
For standardized clinical gait analysis, the GRAIL (Gait Real-time Analysis Interactive Lab; Motekforce Link, Amsterdam) was used essentially as described and the same immersive virtual reality was presented throughout the examinations (13). Per examination, the patient was allowed to familiarize herself by walking for at least 5 min at a self-selected comfortable speed. Subsequently, spatio-temporal parameters of gait together with kinematic and kinetic data were recorded during a 30-s interval, representing at least 52 steps. Mean and standard deviation were calculated and for spatio-temporal parameters repeated measures, ANOVA (SPSS statistical package 25, SPSS Inc. Chicago, Illinois, USA) was employed to assess longitudinal changes. Similarly, the mean of kinetic and kinematic data were plotted for longitudinal comparison.
Restoration of walking abilities and autonomous mobility was characterized by the K-level, by the SIGAM grade (14, 15), the Amputee Mobility Predictor with the use of a prosthesis (AMPPRO) test (16), scoring of the Fall Risk Index (17), and the patient-reported Locomotor Capabilities Index (LCI-5) (18). Magnetic resonance imaging (1.5T Magnetom Avanto Fit, Siemens Healthineers, Germany) 9 months after the index procedure served as a tool to assess the muscle volumes of both thighs relative to the findings prior to surgery. In particular, the length of the region investigated corresponds to the length of the stump with the bottom edge of the tuber ischiadicum as an upper border. Transversal T1-weighted fat/water-separated sequences were recorded and a 3D slicer was employed for quantification (19).
Results
Outcome
The surgical procedures and postoperative recovery were uneventful and already at the time of the index procedure opioids could be tapered to zero. The artificial leg was coupled to the bone-anchored prosthetic stem the second day after the creation of the stoma, and since then, the patient followed a supervised balance and gait training to restore walking abilities.
Magnetic resonance imaging confirmed severe atrophy of the thigh before the index procedure with muscle volumes of 1,781 cm3 on the affected side and 2,750 cm3 on the non-affected side in the corresponding thigh section. While 9 months after surgery the muscle volume of the affected thigh was almost the same as before, a 23% increase on the contralateral side was noted (Figure 2).
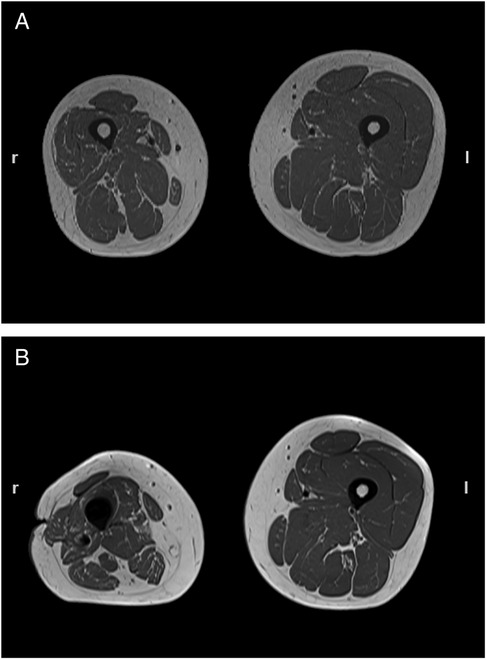
Figure 2. Transverse MRI of both thighs taken prior to transfemoral amputation (A) and 9 months after (B). Muscle volumes of the right (affected) thigh were 1,781 and 1,668 cm3, while those at the corresponding contralateral side were 2,750 and 3,378 cm3, respectively.
Clinical gait analysis
Standardized clinical gait analysis confirmed severe limping and seriously impaired walking abilities at the time of the first presentation (Figure 3). Beyond a rather short stride length and an overall low walking speed kinetic and kinematic features deviated markedly from normal. This holds especially true for the non-affected side and might be taken as an indicator of the increased risk for degenerative joint disease and subsequent aggravation of here already poor mobility. Already 6 months after switching to TOPS, the spatio-temporal characteristics of gait were significantly improved and these changes persisted during the follow-up period. In particular, walking speed was almost doubled (0.50 ± 0.00 m/s at baseline vs. 0.96 ± 0.00 m/s at the time of the last follow-up examination; p < 0.001). The cadence (steps per minute) increased from 38.6 ± 0.37 at baseline up to 50.9 ± 0.48 (p < 0.001) and the stride time dropped (1.55 ± 0.01 s at baseline vs. 1.18 ± 0.01 s; p < 0.001), while the stride length increased from 0.77 ± 0.03 m to 1.13 ± 0.01 m (p < 0.001) and the stride width remained rather constant (data not shown). Contrasting to an almost immediate normalization of the spatio-temporal features of gait (Figure 3A) and the diminished differences between the affected and non-affected leg, the continuous adaptation of the kinetic and kinematic parameters to the new situation was seen (Figures 3B,C). In particular, kinematic and kinetic data from the non-affected hip and knee joints steadily reverted to the physiological pattern.
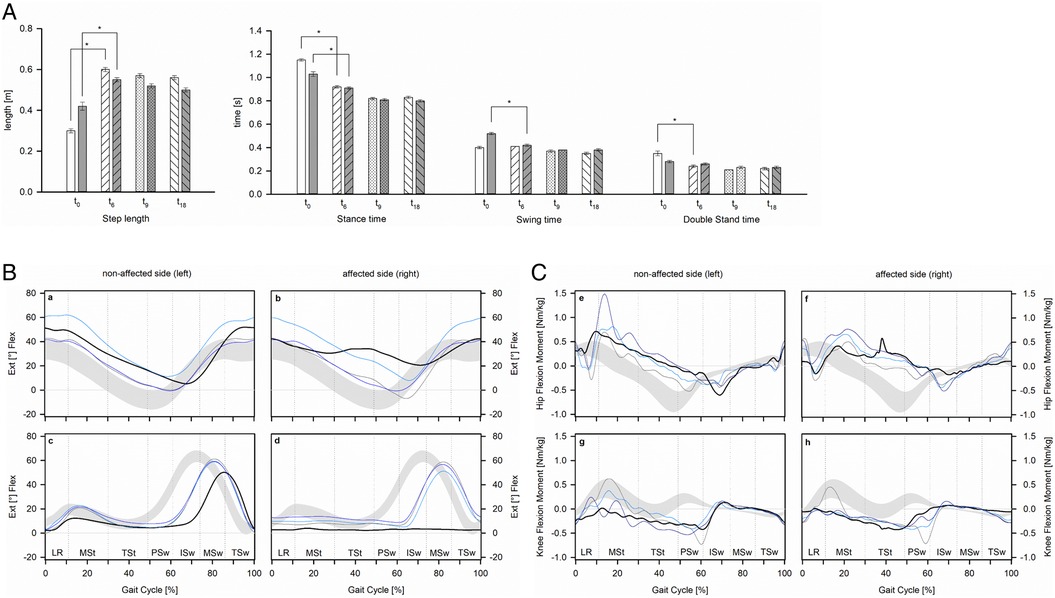
Figure 3. Spatio-temporal parameters of gait (A), kinematics (B), and kinetics (C) of hip and knee joints prior to transfemoral amputation and during the follow-up period. (A) Open and filled bars represent the non-affected and affected side prior to surgery (t0) as well as 6 (t6), 9 (t9), and 18 (t18) months after. (B) Kinematics of the hip (a,b) and knee joints (c,d) together with the normal range [gray area (24)] are presented prior to transfemoral amputation (black) as well as 6 (light blue), 9 (gray), and 18 (dark blue) months after switching to transcutaneous osseointegrated prosthesis system (TOPS). (C) Kinetics of the hip (e,f) and knee joints (g,h) together with the normal range [gray area (24)] are presented prior to transfemoral amputation (black) as well as 6 (light blue), 9 (gray), and 18 (dark blue) months after switching to TOPS. Vertical lines indicate the phases of the gait cycle, that is, LR, loading response; MSt, mid stance; TSt, terminal stance; PSw, pre-swing; ISw, initial swing; Msw, mid-swing; TSw, terminal swing (25).
The patient achieved K-level type 3 and a SIGAM mobility grade F corresponding to a near normal gait ability within 18 months postoperatively (14, 15). Likewise, the patient achieved 41, 44, and 44 points out of 47 points with the AMPPRO, 26, 28, and 27 points out of 28 points with the Tinetti test, and 47, 54, and 54 points out of 56 points with the LCI-5 at the follow-up examinations 6, 9, and 18 months after the index procedure.
Discussion
This case is two-fold unique in that we decided on a TOPS rather than the classical socket prosthesis and performed the first step of the TOPS procedure at the time of transfemoral amputation. Although there were serious concerns for infections due to the transcutaneous metal implant, these are mostly superficial and restricted to the stoma rather than ending with explantation of the prosthesis. Similarly, revision due to failure of the implant is rarely seen (7, 8, 10, 20–23).
At the time of her first presentation, she was seriously disabled with very limited autonomous mobility and chronic pain. Furthermore, she had been rather busy gaining knowledge on the pros and cons of the socket-mounted and bone-anchored prosthesis as measures to restore autonomous mobility after transfemoral amputation. Given the rather long history of the disease, she was not willing to try a socket prosthesis first, as she was seeking for a solution to her issues rather than for replacement of the existing problems with new ones. Thus, we followed her dedicated wish and paralleled the treatment and rehabilitation course with additional examinations. In particular, standardized clinical gait analysis prior to surgery confirmed severe limping with abnormal kinetics and kinematics for both legs. In other words, the risk for degenerative joint disease on the non-affected side and subsequent aggravation of here already poor mobility is foreseeable unless the dysfunctionality of the affected leg is solved. Already 6 months after switching to TOPS, a steep improvement in her walking abilities with diminished differences between the spatio-temporal features related to the affected and non-affected leg was noted, and these changes persisted during the follow-up period. The continuous normalization of kinematic and kinetic data especially on the non-affected side has to be considered as an important prerequisite to prevent the progression of degenerative joint disease. The restoration of bilateral symmetry by mutual approximation to the standard gait pattern during the 18 months of follow-up period mirrors her constant efforts to train and improve her walking abilities.
Conclusion
Although the decision for unilateral transfemoral amputation is hard to achieve and requires careful counseling, there is no doubt that this procedure has the power to improve quality of life and autonomous mobility rather than worsening the situation. The outcome of our patient is well in line with this notion. Furthermore, a reasonable number of patients claim recurrent problems at the interface between stump and standard socket prosthesis, ranging from intradaily fluctuations of the stump volume to ulcera caused by relative movements of the socket (or liner) and the stump. Such issues may lead to fitting and re-fitting of the socket over and over and this we probably spared our patient. Nevertheless, long-term follow-up is necessary to detect future complications of TOPS.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Written informed consent for publication of her clinical details and images was submitted for review to the editor of this journal.
Author contributions
KK and KR collected the data and performed gait analysis. TB was responsible for MRT imaging and analysis. HHA and TM performed the surgery. KK, KR, DCF, and TM drafted the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We greatly appreciate the time and enthusiasm of our patient to undergo repetitive clinical gait analysis and to fill in several questionnaires on her perception of the outcome.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Palazzolo A, Rosso F, Bonasia DE, Saccia F, Rossi R, Knee Committee S. Uncommon complications after anterior cruciate ligament reconstruction. Joints. (2018) 6(3):188–203. doi: 10.1055/s-0038-1675799
2. Hungerer S, Kiechle M, von Ruden C, Militz M, Beitzel K, Morgenstern M. Knee arthrodesis versus above-the-knee amputation after septic failure of revision total knee arthroplasty: comparison of functional outcome and complication rates. BMC Musculoskelet Disord. (2017) 18(1):443. doi: 10.1186/s12891-017-1806-8
3. Trouillez T, Faure PA, Martinot P, Migaud H, Senneville E, Pasquier G, et al. Above-the-knee amputation versus knee arthrodesis for revision of infected total knee arthroplasty: recurrent infection rates and functional outcomes of 43 patients at a mean follow-up of 6.7 years. Orthop Traumatol Surg Res. (2021) 107(4):102914. doi: 10.1016/j.otsr.2021.102914
4. Munin MC, Espejo-De Guzman MC, Boninger ML, Fitzgerald SG, Penrod LE, Singh J. Predictive factors for successful early prosthetic ambulation among lower-limb amputees. J Rehabil Res Dev. (2001) 38(4):379–84. PMID: 11563490
5. Butler K, Bowen C, Hughes AM, Torah R, Ayala I, Tudor J, et al. A systematic review of the key factors affecting tissue viability and rehabilitation outcomes of the residual limb in lower extremity traumatic amputees. J Tissue Viability. (2014) 23(3):81–93. doi: 10.1016/j.jtv.2014.08.002
6. Dudek NL, Marks MB, Marshall SC, Chardon JP. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. (2005) 86(4):659–63. doi: 10.1016/j.apmr.2004.09.003
7. Juhnke DL, Beck JP, Jeyapalina S, Aschoff HH. Fifteen years of experience with integral-leg-prosthesis: cohort study of artificial limb attachment system. J Rehabil Res Dev. (2015) 52(4):407–20. doi: 10.1682/JRRD.2014.11.0280
8. Reif TJ, Khabyeh-Hasbani N, Jaime KM, Sheridan GA, Otterburn DM, Rozbruch SR. Early experience with femoral and tibial bone-anchored osseointegration prostheses. JBJS Open Access. (2021) 6(3):e21.00072. doi: 10.2106/JBJS.OA.21.00072
9. Leijendekkers RA, van Hinte G, Frolke JP, van de Meent H, Nijhuis-van der Sanden MW, Staal JB. Comparison of bone-anchored prostheses and socket prostheses for patients with a lower extremity amputation: a systematic review. Disabil Rehabil. (2017) 39(11):1045–58. doi: 10.1080/09638288.2016.1186752
10. Aschoff HH, Kennon RE, Keggi JM, Rubin LE. Transcutaneous, distal femoral, intramedullary attachment for above-the-knee prostheses: an endo-exo device. J Bone Joint Surg Am. (2010) 92(Suppl 2):180–6. doi: 10.2106/JBJS.J.00806
11. Reetz D, Atallah R, Mohamed J, van de Meent H, Frolke JPM, Leijendekkers R. Safety and performance of bone-anchored prostheses in persons with a transfemoral amputation: a 5-year follow-up study. J Bone Joint Surg Am. (2020) 102(15):1329–35. doi: 10.2106/JBJS.19.01169
12. Hoellwarth JS, Tetsworth K, Rozbruch SR, Handal MB, Coughlan A, Al Muderis M. Osseointegration for amputees: current implants, techniques, and future directions. JBJS Rev. (2020) 8(3):e0043. doi: 10.2106/JBJS.RVW.19.00043
13. Feldhege F, Richter K, Bruhn S, Fischer DC, Mittlmeier T. MATLAB-based tools for automated processing of motion tracking data provided by the GRAIL. Gait Posture. (2021) 90:422–6. doi: 10.1016/j.gaitpost.2021.09.179
14. Hofstad CJ, Bongers KTJ, Didden M, van Ee RF, Keijsers NLW. Maximal walking distance in persons with a lower limb amputation. Sensors. (2020) 20(23):6770. doi: 10.3390/s20236770
15. Ryall NH, Eyres SB, Neumann VC, Bhakta BB, Tennant A. The SIGAM mobility grades: a new population-specific measure for lower limb amputees. Disabil Rehabil. (2003) 25(15):833–44. doi: 10.1080/0963828021000056460
16. Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, et al. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee's ability to ambulate. Arch Phys Med Rehabil. (2002) 83(5):613–27. doi: 10.1053/ampr.2002.32309
17. Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. (1986) 80(3):429–34. doi: 10.1016/0002-9343(86)90717-5
18. Franchignoni F, Orlandini D, Ferriero G, Moscato TA. Reliability, validity, and responsiveness of the locomotor capabilities index in adults with lower-limb amputation undergoing prosthetic training. Arch Phys Med Rehabil. (2004) 85(5):743–8. doi: 10.1016/j.apmr.2003.06.010
19. Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, et al. 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. (2012) 30(9):1323–41. doi: 10.1016/j.mri.2012.05.001
20. Hagberg K, Branemark R. One hundred patients treated with osseointegrated transfemoral amputation prostheses–rehabilitation perspective. J Rehabil Res Dev. (2009) 46(3):331–44. doi: 10.1682/JRRD.2008.06.0080
21. Al Muderis M, Khemka A, Lord SJ, Van de Meent H, Frolke JP. Safety of osseointegrated implants for transfemoral amputees: a two-center prospective cohort study. J Bone Joint Surg Am. (2016) 98(11):900–9. doi: 10.2106/JBJS.15.00808
22. Hagberg K, Ghassemi Jahani SA, Kulbacka-Ortiz K, Thomsen P, Malchau H, Reinholdt C. A 15-year follow-up of transfemoral amputees with bone-anchored transcutaneous prostheses. Bone Joint J. (2020):102-B(1):55–63. doi: 10.1302/0301-620X.102B1.BJJ-2019-0611.R1
23. Marano AA, Modiri O, Rozbruch SR, Otterburn DM. Soft tissue contouring at the time of osseointegrated implant reconstruction for lower extremity amputation. Ann Plast Surg. (2020) 85(S1 Suppl 1):S33–6. doi: 10.1097/SAP.0000000000002329
Keywords: ACL reconstruction, surgical complication, knee joint arthrodesis, transfemoral amputation, transcutaneous osseointegrated prosthesis system, gait analysis
Citation: Krause K, Richter K, Beyer T, Aschoff HH, Fischer D and Mittlmeier T (2022) Elective transfemoral amputation and simultaneous implantation of a transcutaneous osseointegrated prosthesis stem as salvage treatment after knee joint arthrodesis with poor function: A case report. Front. Surg. 9:918303. doi: 10.3389/fsurg.2022.918303
Received: 12 April 2022; Accepted: 22 July 2022;
Published: 30 August 2022.
Edited by:
Paphon Sa-ngasoongsong, Ramathibodi Hospital, Mahidol University, ThailandReviewed by:
Kerstin Hagberg, Sahlgrenska University Hospital, SwedenSamuel Oliver Poore, University of Wisconsin-Madison, United States
© 2022 Krause, Richter, Beyer, Aschoff, Fischer and Mittlmeier. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Mittlmeier dGhvbWFzLm1pdHRsbWVpZXJAbWVkLnVuaS1yb3N0b2NrLmRl
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Katharina Krause
Katharina Krause Katherina Richter1,2
Katherina Richter1,2 Dagmar-Christiane Fischer
Dagmar-Christiane Fischer Thomas Mittlmeier
Thomas Mittlmeier