- 1Department of Head and Neck Surgery, Fujian Medical University Cancer Hospital, Fujian Cancer Hospital, Fuzhou, China
- 2Department of Head and Neck Surgery, Hunan Cancer Hospital, Changsha, China
Over the past decades, remote-access thyroid surgery has been widely developed in the treatment of thyroid carcinoma, which can help patients to avoid cosmetically displeasing scarring. In this research, we collected and review our experience with endoscopic thyroidectomy with neck dissection via trans-thoracoareolar approach combined with trans-oral approach over a 3-year period. They were all diagnosed with thyroid carcinoma, and two of them had a complication of Hashimoto's thyroiditis. No patients were dissatisfied with the postoperative cosmetic results. One patient had numbness in the lower lip, but the symptom disappeared 1 month later. No infection, hemorrhage, or air embolism occurred. Pain and numbness in the endoscopic thyroid surgery group were slighter than in those who had open surgery. The present study aims to compare the feasibility and safety of trans-thoracoareolar approach combined with trans-oral approach to conventional open surgery.
Introduction
Over the past decades, remote-access thyroid surgery has been widely developed in the treatment of thyroid carcinoma, which can help patients to avoid cosmetically displeasing scarring. Among them, the Trans-thoracoareolar approach has become the first choice by many surgeons, given the excellent cosmetic results with effective lesions oncologically resected when performing total endoscopic surgery for thyroid carcinoma (1, 2). For surgeons with proficient endoscopic operation techniques, under the premise of mastering the open combined radical resection of thyroid cancer, it is completely possible to perform endoscopic combined radical resection of thyroid cancer.
Due to the interference of the sternum stem and the clavicle, the thyroidectomy with neck dissection (TND) via trans-thoracoareolar approach cannot completely remove the grade IV and VI lymph nodes, which may lead to postoperative recurrence. For the similar reason, the lymph nodes in level II and upper level III cannot be removed completely under TND via trans-oral approach.
In this research, we collected and review our experience with endoscopic TND via trans-thoracoareolar approach combined with trans-oral approach over a 3-year period. The present study aims to compare the feasibility and safety of trans-thoracoareolar approach combined with trans-oral approach to conventional open surgery.
Materials and methods
Patients' criteria
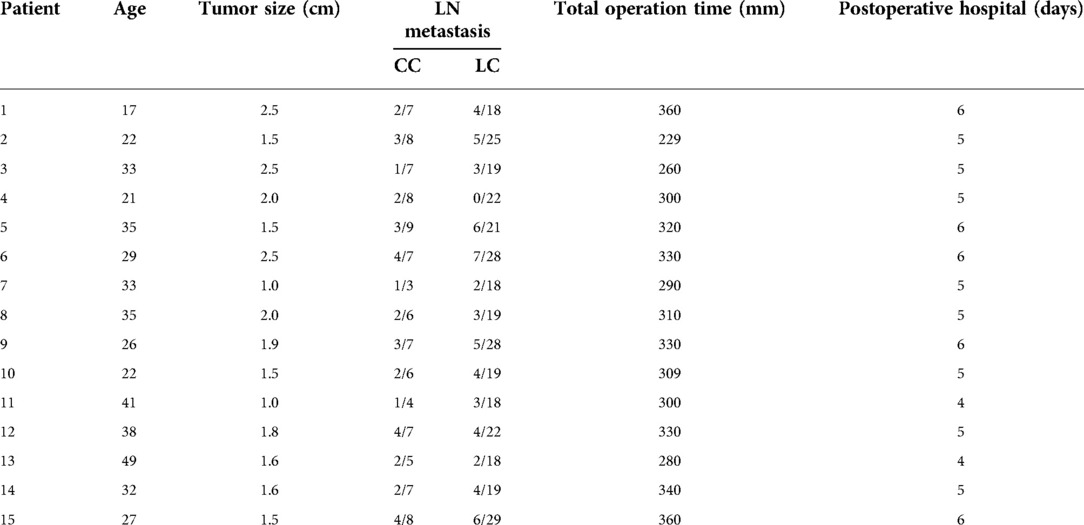
Between June 2015 and December 2020, 40 female patients with ages ranging from 17 to 49 years were included in this study (Table 1).
Inclusion criteria were as follows: single or multiple tumors located in the gland without invasion of the capsule, diameter <3.0 cm; patients diagnosed with thyroid carcinoma by ultrasonic, CT, or fine needle aspiration preoperatively; and lateral neck lymph node metastasis revealed by imaging or fine needle aspiration without confluent tumors or invasion of the internal jugular vein. (1) Endoscopic surgery was performed on 20 patients via trans-thoracoareolar approach combined with trans-oral approach. Seventeen of them were diagnosed with a single tumor, nine in the left and eight in the right. Three of them were diagnosed with multiple tumors. The maximum diameter did not surpass 2.5 cm. The largest lymph node diameter is 1.5 cm without fusion or invasion of the internal jugular vein. (2) For the conventional open groups, 16 of them were diagnosed with a single tumor, 10 in the right and six in the left. Four of them were diagnosed with multiple tumors. The condition of the lymph nodes is similar to that of the endoscopy group.
Exclusion criteria were as follows: tumor located in the upper pole of the posterior aspect of thyroid, close to recurrent laryngeal nerve; invasion of the capsule and surrounding tissues such as recurrent laryngeal nerve, trachea, esophageal, or belt-shaped muscle; lymph node metastasis with confluent tumors or invasion of the internal jugular vein; and patients a history of thoracic or neck surgery.
We defined transient hypocalcemia and transient recurrent laryngeal nerve injury based on the recovery from symptoms and normalization of laboratory data within 6 months.
All the patients had taken levothyroxine for thyroid stimulating hormone suppression after the operation and were regularly followed up with serum thyroglobulin (Tg) and neck ultrasonography at intervals of 3 months or 6 months.
The mean follow-up period was 26.4 months (range, 9–42 months). No evidence of residual or recurrent disease was found at follow-up. The cosmetic results of this procedure were excellent.
Operative techniques
The transnasal endotracheal intubation was adopted for general anesthesia. Antibiotics were used once 30 min before operation. Patients were in a supine position with head hypsokinesis, and their necks were straightened with cushioning being placed under the shoulder so that the necks were in a slight hyperextension position.
The working space was established via trans-thoracoareolar approach. The operator stood between the thighs of patients. The “inflation fluid” was prepared with adrenaline and saline (the dilution ratio is 1:500). Two incisions were made at 11 o'clock and 4 o'clock of the left areola, respectively, the length of the former is 0.5 cm, and the length of the later is 1 cm. Another 0.5 cm long incision was made at 11 o'clock of the right areola, dissection would not be ceased until the deep fascia was exposed. The “inflation fluid” was subcutaneously injected into the neck area where the flap was separated from via the incision previously made, about 100–200 mL of “inflation fluid” was injected with a special needle connected with a 50 mL syringe. Blunt dissection between superficial and deep fascia was accomplished with visual Trocar, the operation tunnel or space would not be established until reaching the clavicles. Excess liquid was squeezed out later. A 10 mm Trocar was inserted via the incision at 4 o'clock of the left areola, and then a 30° laparoscope was inserted through the Trocar. CO2 was insufflated with the pressure maintained at about 6–8 mmHg. After that, two 5 mm Trocars were inserted via the incision at 11 o'clock of the left and right areolas, respectively, an operating forceps and an ultrasonic scalpel were inserted through the two Trocars accordingly.
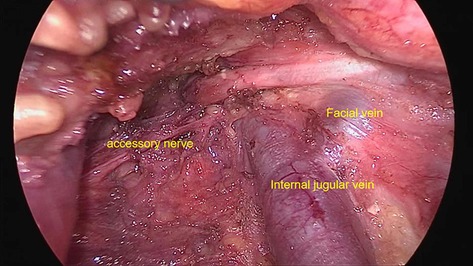
Under the monitoring of a laparoscope, dissection was made between subcutaneous tissue and deeper tissue in the chest and neck. When reaching the neck area, dissociation was made between the platysma and deep loose connective tissue. Dissociation would not be stopped until reaching the hyoid and the lateral margin of sternocleidomastoids. Using an ultrasonic scalpel, the incision was made in linea alba cervicalis and the surgical capsule of thyroid sequentially. Dissociation was made between the two layers of capsule of thyroid, and then the thyroid was exposed. To perform unilateral lobectomy or to perform bilateral thyroidectomy, the decision was made according to preoperative ultrasonic, CT results, and operation findings. After that, dissection was continued. When reaching the inferior margin of submandibular glands, dissection was made 2 cm outwards of the lateral margin of sternocleidomastoids. Using an ultrasonic scalpel, the incision was made between the sternal head and clavicular head of the sternocleidomastoid, and then traction was made with an endoscopic retractor. Omohyoid was cut off subsequently. When the vascular sheath was cut with a scissor and exposed, dissociation was made among arteria carotis communis, vena jugularis interna, and nervi vagus. The lateral neck lymph nodes were removed from the bottom up along vena jugularis interna, removing would not be ceased until the lymph nodes in level II were completely removed (Figure 1). The C2, C3, C4, and accessory nerves were preserved, meanwhile, the thoracic duct and right lymphatic duct were protected.
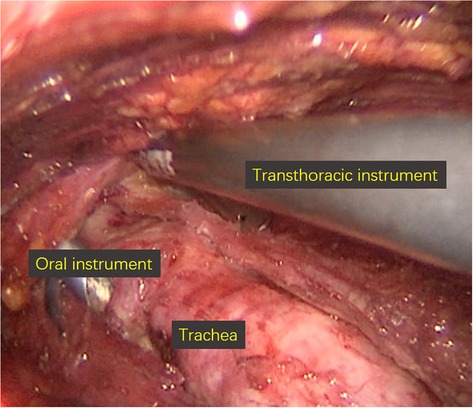
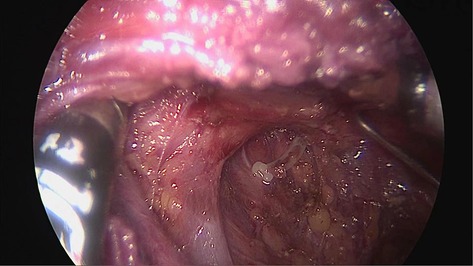
The other working space was established via trans-oral approach (Figure 2). A 1 cm long incision was made at the midpoint of sulcus vestibularis, and two 0.5 cm long incisions were made in front of the left and right first premolars in sulcus vestibularis. Trocars were inserted via the three incisions previously made. Since the working space in the neck was established before, it is easy to enter the field. The lymph nodes in level VI and level VII were removed, and the residual lymph nodes in level IV which were neglected during the removal via trans-thoracoareolar approach were eventually cleared away (Figure 3). At the end of the operation, the specimen was put into specimen bags and extracted, the operation cavity was washed with distilled water, and drainage tubes were placed.
Tips and key points
For male patients, the chest incision is suggested to be made in the second intercostal space, if so, the wound will be minimized, and the operation will be facilitated. For female patients, if the chest incision was hidden into the aureola, the scars will be invisible postoperatively. The lymph nodes in level IIB should be removed conventionally, and the removal should not be ceased until the surface of splenius capitis is exposed.
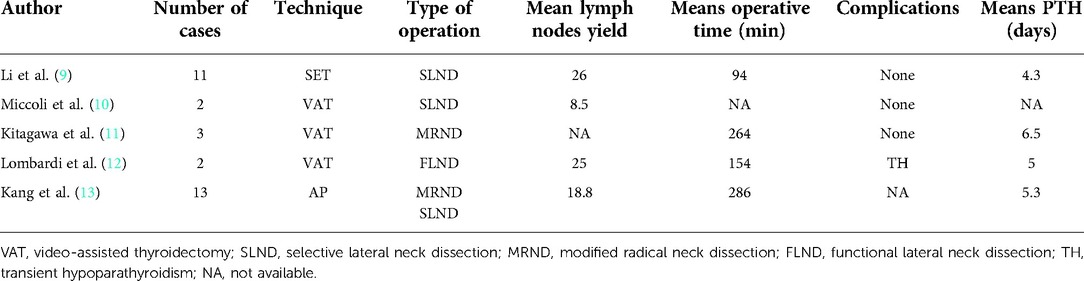
As for the scope of operation, the flap needs to be separated from the inferior margin of glandula submandibularis upwards, to the superior margin of clavicle downwards, to the medial margin of the contralateral sternocleidomastoid inwards, and the posterior margin of sternocleidomastoid outwards. When reaching the posterior margin of sternocleidomastoid, dissection should be made 2 cm outwards again. Some authors proposed that the marginal mandibular branches of the facial nerve may descend 2 cm inferior to the inferior margin of glandula submandibularis if the skin in the patient's neck is very loose (8). But in fact, the marginal mandibular branches of the facial nerve descend for the loose skin, it distributes in the deep surface of platysma and locates in the region where it is 1.2 cm superior or 0.8 cm inferior to the inferior margin of mandibular. We had never seen the marginal mandibular branches of the facial nerve descend further than 2 cm intraoperatively, so the separation mentioned above would not be threatening (Table 2).
When the separation of the flap is accomplished, the dissection of sternocleidomastoid should be started sequentially. The traction of the anterior margin of sternocleidomastoid should be made outwards with an endoscopic retractor, and then dissection should be continued outwards. For the restriction of retractor, the lower part of sternocleidomastoid cannot be dissected sufficiently, you can only touch the vena jugularis interna. The space sternal head and clavicular head of sternocleidomastoid should be expanded, and these heads should be retracted laterally with retractors. The sternocleidomastoid should be completely dissociated. Omohoid should be dissociated, but not cut, because it can not only provide traction for other tissue in its affinity but also help the surgeon to determine the scope of operation as a landmark. The neck dissection should be performed from upside to downside, and from the middle to the two sides.
The accessory nerve should be correctly identified. First, dissociation should be made along the lateral margin of the posterior belly of digastrics, when reaching the lateral side of vena jugularis interna, the outlet where accessory nerve exits from the skull will be exposed. Second, Dissociation should be made along the sternocleidomastoid, when reaching the lateral side of vena jugularis interna, the intlet where the accessory nerve enters into the sternocleidomastoid will be exposed. Dissection should be continued upwards and the accessory nerve should be completely exposed. Third, if it is needed to perform neck dissection in level V, when the great auricular nerve is dissociated and dissection is made 1 cm upwards, the intlet where the accessory nerve enters into the sternocleidomastoid will be exposed.
The rupture of the internal jugular vein and thoracic duct should be correctly handled. First, we encountered one case of rupture of the internal jugular vein in this study. Do not attempt to make occlusion with the vessel clamp, or the rupture will be expanded. Suction should be made sufficiently, thus the surgical field can be clearly observed. The “8” pattern of stitching should be accomplished with 4-0 suture one-handed, and then suction should be ceased. Knot tying should be accomplished using both hands under a laparoscope. Otherwise, when you encounter the rupture of the thoracic duct, dissociation should be made carefully and occlusion should be made with a vessel clamp via trans-oral approach. Occlusion should not be made via trans-thoracoareolar approach, for there is an obstruction caused by the clavicle. It is safe and convenient to operate via trans-oral approach.
Postoperative management
After surgery, antibiotics were applied for 2 days, and benzalkonium bromide mouthwash was given to rinse the mouth after each meal. Liquid diet was allowed on the first day after surgery, and then semi-liquid diet was allowed on the second day after surgery. There is no need to deal with pain or numbness in the incisions, these symptoms will disappear in 1 month usually. Normally, swelling is not severe, so no measures should be taken to deal with it.
Discussion
With the development of endoscopic thyroid surgery technology and the patients' desire for cosmetic results, the indications of endoscopic thyroid surgery have expanded from benign thyroid nodule to thyroid carcinoma with lymph node metastasis. Although there is a lack of large-sample randomized controlled studies, recent follow-ups showed that no difference was found in thyroglobulin level and recurrence rate between patients with endoscopic surgery and open surgery (3–6). Therefore, the technique of endoscopic surgery should be applied not only in thyroid carcinoma with lymph node metastasis in the central cervical area but also in lymph node metastasis in the lateral cervical area, in which neck dissection under endoscope leads to authentic cosmetic and minimally invasive results. In the past years, endoscopic thyroid surgery was thought to be extremely invasive for the large scope of operation. However, patients who underwent neck dissection in the lateral cervical area with long L-shaped incisions suffered tremendous physiological and mental pain. On this account, neck dissection in the lateral cervical area under endoscope is an ideal method, because it is mentally minimally invasive. Cases of total endoscopic neck dissection in the lateral cervical area have been reported by Wang et al. (7), which demonstrates that endoscopic surgery not only leads to better cosmetic results but also clearer re-movement in level IIB because of the magnification effect of the endoscope. What's more, due to the small scope of separation brought by the endoscope, the trauma is less than that of open surgery.
Recently, some authors performed endoscopic neck dissection in the lateral cervical area via trans-thoracoareolar approach. However, due to the existence of the anatomical blind area, especially the affinity of the clavicle and level II, it is hard to remove the affected lymph nodes, which may lead to unmanageable hemorrhage or lymphatic fistulas and residue of lymph nodes. These problems will be solved with endoscopic operation via trans-oral approach. As for the total trans-oral approach, the lymph nodes removed were only limited to level VI. In addition, it is difficult to learn to operate by this method, which will cost a long learning curve. But if the working space is established via trans-thoracoareolar approach in advance, it may be easier to operate via trans-oral approach. Moreover, it is very difficult to remove the lymph nodes in levels II, III, and IV via trans-oral approach. But it is easier to operate via trans-oral approach if the dissociation is made sufficiently via trans-thoracoareolar approach in advance. In our study, we found that if the dissociation of the posterior margin of the sternocleidomastoid achieves 2 cm, the lymph nodes in level V is not difficult to remove. The combination of these two approaches has advantages in removing the lymph nodes in the lateral neck area, which will benefit surgeons with little experience in oral operations. Thus, the difficulty of learning for endoscopic thyroid operation is greatly reduced.
In our study, when we were removing the lymph nodes in level IV via trans-oral approach, residual lymph nodes left by operation via trans-thoracoareolar approach were discovered in five patients, and lymph node metastasis was found in three of these five. The other four patients were also diagnosed with lymph node metastasis in the progress of removing the lymph nodes in level IV via trans-oral approach. Thus, there is a possibility of residue in removing lymph nodes via total trans-thoracoareolar approach. Rupture of thoracic duct was found in one patient when we were removing the lymph nodes via trans-oral approach. Fortunately, we made occlusion with vessel clamp via trans-oral approach later, and no lymphatic fistulas occurred after surgery (Figure 3). Both the total trans-thoracoareolar approach and total trans-oral approach have their own disadvantages. The total trans-thoracoareolar approach is not always efficient with complete dissection of the lymph nodes, which is affected by the skill of surgeons and the tumor-nodemetastasis stage. However, the combination of trans-thoracoareolar approach and trans-oral approach could achieve this goal easily. Moreover, compared with open surgery, the combination of these two approaches not only achieves significant cosmetic effects but also causes less tissue damage and has shorter hospital stays. It is important to be clear that not every patient is amenable to the endoscopic approach, given that the radical cure of cancer is always in the first place. Thus, we should carefully control indications and contraindications for the endoscopic thyroidectomy. Hence we propose to combine these two approaches to improve the endoscopic surgery and curative effect.
In conclusion, to have endoscopic surgery for thyroid carcinoma via the combined approach, the candidate should meet the requirements below: (1) Age <45 years old. If a patient is eager for cosmetic results, this requirement can be relaxed. (2) The diameter of thyroid mass should not be larger than 3 cm. No affection in the adjacent tissue. (3) No widespread lymph node metastasis, confluent tumors, or invasion of the great vessels in the neck. (4) Eagerness for cosmetic results.
Conclusion
All of the patients had undergone successful surgery. They were all diagnosed with thyroid carcinoma, and two of them had a complication of Hashimoto's thyroiditis. No patients were dissatisfied with the postoperative cosmetic results. One patient had numbness in the lower lip, but the symptom disappeared 1 month later. No infection, hemorrhage, or air embolism occurred. Pain and numbness in the endoscopic thyroid surgery group were slighter than in those who had open surgery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics committee of Fuzhou provincial cancer hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YS contributed to all of the literature review in this work. XL and LZ participated in the process of finalizing the final manuscript. HZ revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Natural Science Foundation of Fujian Province (2021J01447).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Miccoli P, Materazzi G, Berti P. Minimally invasie thyroidectomy in the treatment of well differentiated thyroid cancers: indications and limits. Curr Opin Otolaryngol Head Neck Surg. (2010) 18(2):114–8. doi: 10.1097/MOO.0b013e3283378239
2. Vasileiadis I, Boutzios G, Karalaki M, Misiakos E, Karatzas T. Papillary thyroid carcinoma of the isthmus: total thyroidectomy or isthmusectomy? Am J Surg. (2018) 216(1):135–9. doi: 10.1016/j.amjsurg.2017.09.008
3. Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, et al. Endoscopic thyroidectomy for thyroid malignancies: comparision with conventional open thyroidectomy. World J Surg. (2007) 31:2302–6. doi: 10.1007/s00268-007-9117-0
4. Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, et al. Comparative study of endoscopic thyroid microcarcinaoma (PTMC) patients. J Surg Oncol. (2009) 100:477–80. doi: 10.1002/jso.21367
5. Li Z, Wang P, Wang Y, Xu S, Cao L, Que R, et al. Endoscopic lateral neck dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg Endosc. (2011) 25(3):809–96. doi: 10.1007/s00464-010-1292-7
6. Miccoli P, Elisei R, Materazzi G, Capezzone M, Galleri D, Pacini F, et al. Minimlly invasive videoassited thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery. (2002) 132:1070–4. doi: 10.1067/msy.2002.128694
7. Neiderman NNC, Baris H, Duek I, Warshavsky A, Ringel B, Izkhakov E, et al. Lateral neck dissection for well-differentiated thyroid carcinoma: is prophylactic level V neck dissection necessary? A retrospective cohort study. Ear Nose Throat J. (2021):1455613211003805. doi: 10.1177/01455613211003805. [Epub ahead of print]33915059
8. Park JY, Koo BS. Individualized optimal surgical extent of the lateral neck in papillary thyroid cancer with lateral cervical metastasis. Eur Arch Otorhinolaryngol. (2014) 271(6):1355–60. doi: 10.1007/s00405-013-2630-x
9. Li Z, Wang P, Wang Y, Xu S, Cao L, Que R, et al. Endoscopic lateral neck dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg Endosc. (2011) 25:890–6. doi: 10.1007/s00464-010-1292-7
10. Miccoli P, Materazzi G, Berti P. Minimally invasive videoassisted lateral lymphadenectomy: a proposal. Surg Endosc. (2008) 22:1131–4. doi: 10.1007/s00464-007-9564-6
11. Kitagawa W, Shimizu K, Akasu H, Tanaka S. Endoscopic neck surgery with lymph node dissection for papillary carcinoma of the thyroid using a totally gasless anterior neck skin lifting method. J Am Coll Surg. (2003) 196:990–4. doi: 10.1016/S1072-7515(03)00130-3
12. Lombardi CP, Raffaelli M, Princi P, De Crea C, Bellantone R. Minimally invasive video-assisted functional lateral neck dissection for metastatic papillary thyroid carcinoma. Am J Surg. (2007) 193:114–8. doi: 10.1016/j.amjsurg.2006.02.024
Keywords: trans-oral endoscopic thyroid surgery, trans-thoracoareolar approach, conventional open surgery, comparison, outcomes
Citation: Shi Y, Zhang L, Liu C, Wang Y, Zhang H and Lin X (2022) Comparison of surgical outcomes between patients undergoing trans-oral endoscopic thyroid surgery combined with trans-thoracoareolar approach and conventional open surgery. Front. Surg. 9:916874. doi: 10.3389/fsurg.2022.916874
Received: 10 April 2022; Accepted: 5 August 2022;
Published: 8 September 2022.
Edited by:
Weihong Jiang, Central South University, China© 2022 Shi, Zhang, Liu, Wang, Zhang and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hailin Zhang emhhaGFsaUAxNjMuY29t Xiuan Lin bHhhZmp0aEAxMjYuY29t
Specialty Section: This article was submitted to Otorhinolaryngology-Head and Neck Surgery, a section of the journal Frontiers in Surgery
 Youyuan Shi
Youyuan Shi Lu Zhang1
Lu Zhang1