
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 07 June 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.913456
This article is part of the Research Topic Endoscopic Spine Surgery: New concepts and advancements View all 23 articles
Background: Unilateral biportal endoscopy (UBE) is a newly developed technique for spine surgery. Owing to the convenience of nerve decompression and compatibility with open surgical instruments under endoscopic guidance, this technique has seen widespread global use. In this study, we first used modified UBE with suture anchor fixation for cervical laminoplasty in a 65-year-old female patient with good clinical outcomes.
Methods: We used bilateral biportal endoscopy (BBE) for cervical laminoplasty with suture anchor fixation in a patient with cervical stenosis. Under endoscopic guidance, a bilateral approach was used to make the gutter and lift the lamina door. After the lamina doors were opened, sutures were tied tightly using facia cannula and knot pusher. After confirming the solidarity of the open-door status, the drainage tube was inserted and the incisions were closed. The patient’s pre- and postoperative radiological and clinical results were evaluated.
Results: Postoperative Japanese Orthopaedic Association (JOA) and Neck Disability Index (NDI) scores were improved clinically, and cervical canal was decompressed radiologically.
Conclusions: BBE laminoplasty combined with suture anchor fixation showed a favorable clinical and radiological result and appears to be a safe and effective technique for cervical stenosis.
With the advent of an aging society, an increasing number of patients with cervical stenosis require decompression surgery (1). Traditional open surgery has many disadvantages (2) hence, minimally invasive approaches to surgery have emerged, which lead to less injury, faster recovery, and fewer complications (3). Unilateral laminectomy with bilateral decompression in a narrow cervical canal with percutaneous endoscopy and microscopy is risky and has a steep learning curve (4–6). Unilateral biportal endoscopy (UBE) is a minimally invasive spinal surgery developed in recent years, which has been widely used for degenerative diseases of the lumbar spine with remarkable efficacy (7–11). UBE for cervical decompression has also been reported, but there have been only a few published studies (12, 13). In a technical report, we applied a modified UBE technique for cervical laminoplasty with the aid of suture anchor fixation, and obtained satisfactory clinical results.
The study approval was obtained from our institutional review board (NO. 2019KY006). Informed consent was obtained from the patient for the publication of the report. A 65-year-old woman was suffering from gait disfunction and numbness in both the upper extremities for 5 years, and her condition deteriorated within 1 month. A physical examination revealed tendon hyperreflexia and the presence of a Babinski sign in the lower extremities with positive Hoffman sign and hypoesthesia in the upper extremities (more severe on the right side). The patient’s history included controlled hypertension and hyperlipidemia. Magnetic resonance imaging (MRI) revealed central cervical stenosis at the C4-C5-C6 levels, and the spinal cord was compressed due to ligamentum flavum (LF) hypertrophy and disc herniation at the C4-C5-C6 levels (Figure 1). The diagnosis of cervical myelopathy was confirmed. The patient expressed strong opposition to conventional open surgeries, such as anterior fusion and posterior open-door laminoplasty because of a history of cardiovascular diseases and agreed to biportal endoscopic cervical laminoplasty. The Japanese Orthopaedic Association (JOA) score was 9 and Neck Disability Index (NDI) score was 23 when she visited the outpatient department.
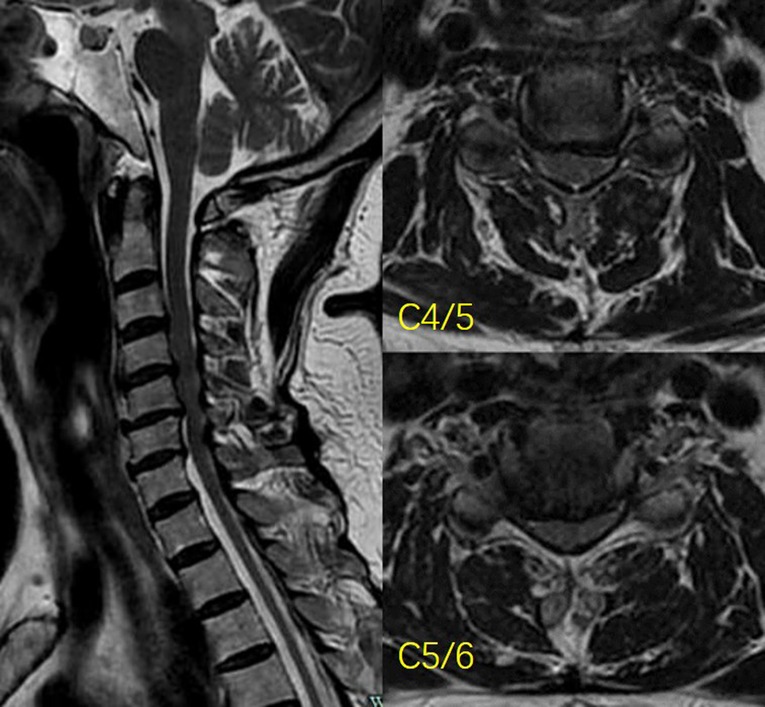
Figure 1. Preoperative MR images show central canal stenosis at the C4-C6. The spinal cord was compressed by herniated discs and a hypertrophied ligamentum flavum.
Under general anesthesia, the patient was placed prone on a spine table with the head secured in a horseshoe headrest. The cervical spine was mildly flexed and fixed by a tape (Figure 2A).
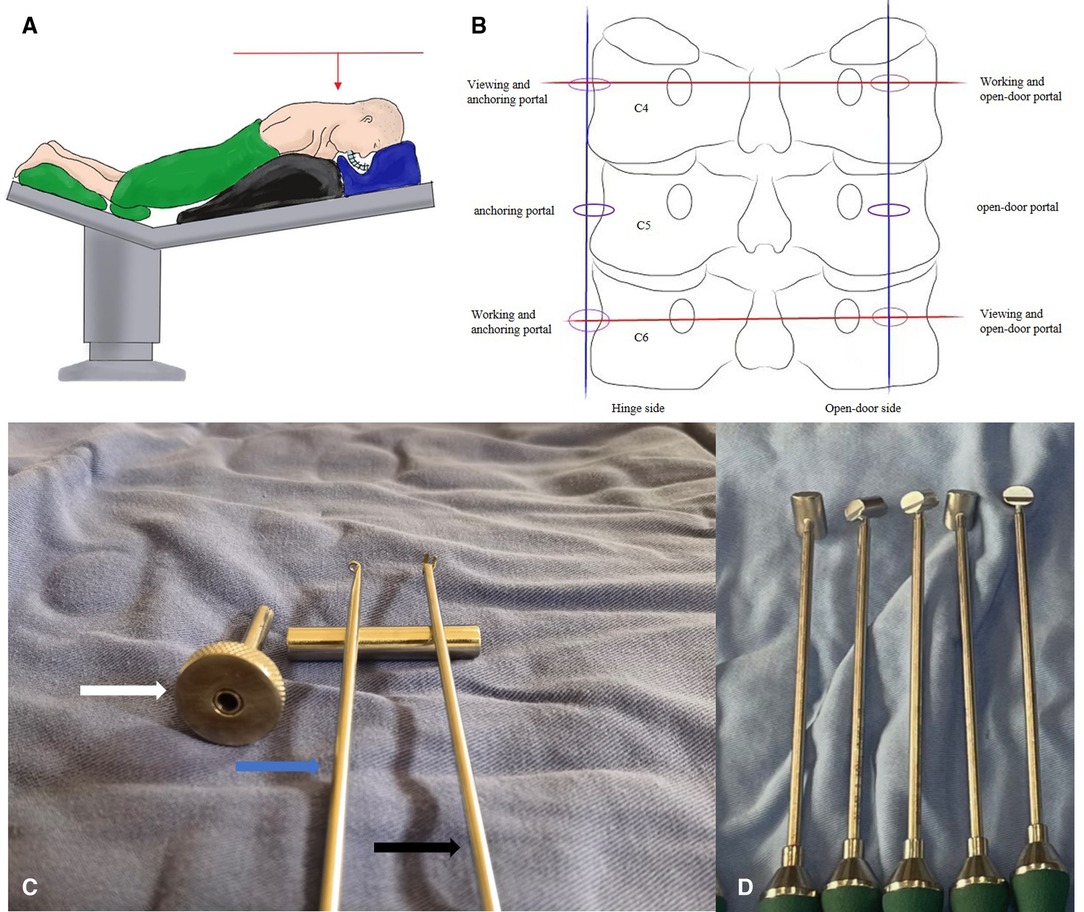
Figure 2. (A) A overall view of operating table. The table was adjusted to make sure that the intervertebral space was perpendicular to the ground. (B) Schematic representation of the location of the portals; (C) Newly designed knotting system for endoscopic laminoplasty. Facia cannula (white arrow), working length 6 cm and inner diameter 0.5 cm; endoscopic knot pusher (blue arrow) and shears (black arrow), diameter 0.3 cm; (D) Trials (range, 8 mm–12 mm) for the measurement of LOS.
Two horizontal lines were drawn along the C4 and C6 pedicles, a vertical line in the midline of the right lateral mass, while the other one was along the lateral margin of the left lateral mass in the anteroposterior view. The intersection points on the left-hand side served as a viewing portal, whereas the intersection points on the right-hand side served as a working portal. Two more incisions were made at the midpoints of the intersections on both sides. The three incisions on the left were used as the anchoring portal while the contralateral incisions were used as the open-door portal (Figure 2B).
We used suture anchors with a length of 10 mm and diameter of 2.8 mm. A high-speed burr (Guizhou Zirui Technology, China), specially designed arthroscopic facilities (Figure 2C), a tool-kit of radiofrequency (RF) systems (Jiangsu BONSS Medical Technology, China), and open spine surgical instruments, including pituitary forceps, curettes, and Kerrison rongeurs, were used.
The first stage of the procedure was performed on the left side of the patient. A RF was used to expose the lamina, spinous process, and lateral mass of C4-C5-C6. A 4-mm diamond burr was used to remove the dorsal cortex and cancellous bone at the junction of the lamina and lateral mass of C4-C5-C6 (Figure 3A), and the bony gutter on the hinge side was completed. Subsequently, a 2-mm diamond burr was employed to make entry points on the center of the lateral mass and spinous processes of C4-C5-C6 (Figure 3B); suture anchors were inserted in succession (Figure 3C).
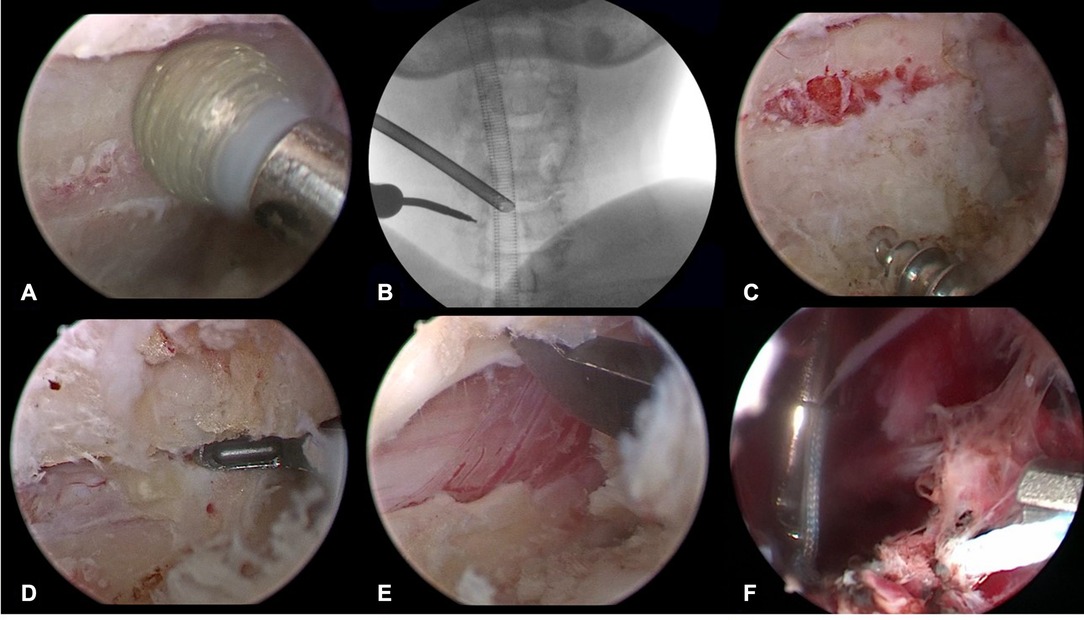
Figure 3. The drilled gutter was first completed using 4-mm diamond burr on the hinge side (A) Insertion hole for the suture anchor was also prepared using 2-mm diamond burr on the hinge side and confirmed under fluoroscopy (B) Suture anchor was screwed in the lateral mass (C) The remained ventral cortical bone on the open-door side was resected using 1-mm Kerrison rongeur (D) The lamina door was raised by a 2-mm Kerrison rongeur (E) The sutures was knotted tightly to maintain the lamina door in open position (F).
The endoscopy and instruments were moved to the right to begin the second stage of the procedure. After C4-C5-C6 lamina and intersections of C34 and C67 were exposed, the same longitudinal gutter was created at the margin between the lamina and the lateral mass of C4-C5-C6 using a 4-mm diamond burr. The remaining ventral cortex was removed by a 1 mm Kerrison rongeur with a thin blade (Figure 3D). The LF between C34 and C67 was cut transversely to facilitate the process of floating laminae.
At the beginning of the third stage, the tip of spinous process of C4-C5-C6 was carefully cut. The arthroscopy was passed over the top of the lamina via the interspinous ligament, reaching the contralateral side to observe the knotting process. A retriever was used to take the previously introduced sutures for each segment out of the same soft tissue portal; then, the facia cannula was inserted along the sutures in the anchoring portal. The assistant bent the hinge in a greenstick fashion and held the lamina door in place (Figure 3E). The sutures were tied firmly to prevent reclosure of the lifted laminae (Figures 3F, 4).
A drainage tube was inserted on the open-door side, and the incisions were closed using a standard method (Supplementary Video S1). The surgery was performed without complications. The estimated blood loss during the operation was 200 mL, and the operation time was 190 min. Cefuroxime (1.5 g, twice a day, intravenous) was administered for 24 h, and the pain was managed with flurbiprofen (100 mg, twice a day, intravenous) postoperatively.
A postoperative semirigid cervical collar was prescribed for 3 months. The patient gave consent to the regular anti-osteoporosis treatment which could effectively improve bone mineral density and prevent anchors from loosening and displacement.
Postoperative computed tomography scan revealed adequate enlargement of cervical canal of C4-C5-C6 and the cord was fully decompressed on MRI (Figure 5). The JOA and NDI scores were 11 and 20 on day 3 after surgery, and improved to 14 and 16 at the 6 months follow-up, respectively.
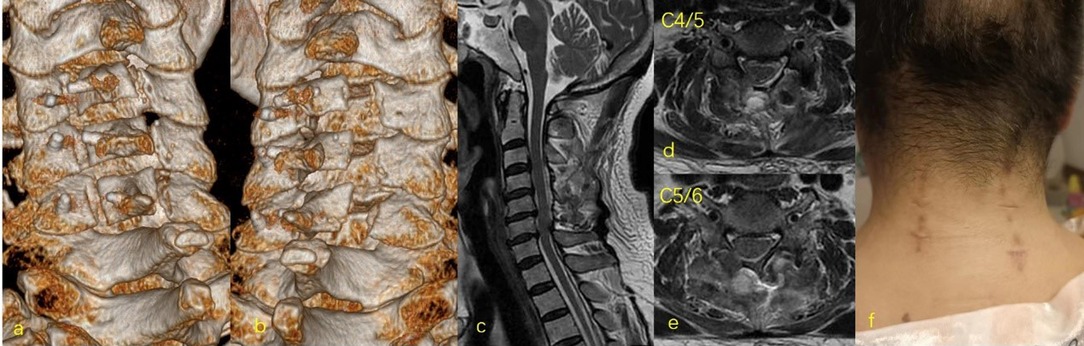
Figure 5. Postoperative 3D CT of C4-C6 showed widening of the spinal canal after BBE laminoplasty using suture anchor fixation (A,B) Postoperative MRI showed full decompression of spinal cord with an adequate subarachnoid space (C–E). Six wounds were created for the cervical laminoplasty at three levels (F).
To the best of our knowledge, this is the first study to apply the UBE and suture anchor techniques for cervical laminoplasty. An endoscopic open-door laminoplasty with minimal muscle invasion was performed. The patient’s clinical symptoms improved significantly.
Cervical spondylotic myelopathy caused by posterior compression often requires posterior surgery. Open laminectomy and laminoplasty necessitate extensive paraspinal muscle release and retraction, which may result in axial pain and kyphotic deformity during follow-ups (14). In percutaneous endoscopic and microscopic surgery, contralateral decompression can be completed only when the base of spinous process is excessively removed, which leads to more intraspinal work and a higher risk. The operation and observation in a single portal manifested several difficulties (4, 6).
The UBE technique has been widely used in the treatment of lumbar degenerative diseases, with less iatrogenic injury and faster recovery (15, 16). The application of UBE in cervical spine was mainly in foraminoplasty (12, 17); There is only one report on spinal canal decompression and the technical requirements are relatively high (13). We have designed a contralateral “Zhang’s portal” to facilitate cervical canal decompression (18), therefore, we have rich experience in bilateral biportal operations. Kurokaw (19) demonstrated the validity of suture anchors in cervical laminoplasty in a cadaveric study, and we successfully performed suture anchor fixation on the contralateral side using the UBE technique. Compared with open surgery, continuous irrigation not only ensures a clear operative field, but also lowers the risk of infection (7, 20). The working portal is independent of the viewing portal, and thus the operative efficacy is dramatically improved. Moreover, under the arthroscope, the field of vision is enlarged 30 times, and the observation of dural pulsation, tiny blood vessels, and ligaments is very clear, which is conducive for hemostasis and decompression.
Before the operation, we considered placing the plate on the open-door side, however, it was very difficult to operate under the arthroscope. Without specially designed instruments, it was also difficult to find the tiny internal fixation materials once they were lost in the soft tissue. Besides, the cervical canal was opened and the spinal cord exposed, which was vulnerable to internal fixation. Suture anchor repair is technically mature under arthroscopy (21). Our team has a lot of experience in arthroscopic surgery and suture management, so we chose the suture anchor fixation on the hinge side under UBE guidance. The indications of this procedure were the same as those of traditional open cervical laminoplasty, while the contraindications included severe osteophytes around the lateral mass and abnormally distributed vessels which make safe anchor placement difficult, and prior cervical surgery with posterior approach.
There are some tips that surgeons should not overlook. The lateral mass should be fully exposed on the hinge side, but not on the open-door side. Exposure beyond the lateral margin of the lateral mass will significantly increase bleeding. Guttering should be done before anchoring; otherwise, the sutures can easily get tangled. When creating the open side, the ventral cortex of the laminae and LF were removed carefully using a 1 mm Kerrison rongeur, a nerve hook was used to separate the adhesions, and a low frequency probe was used to decrease the bleeding from epidural veins. No force was applied during the open-door procedure. The lamina open-door angle should not exceed 45° (22). After opening the lamina, trials (Figure 2D) for miniplate were used to make sure that the laminoplasty opening size (LOS) was large enough for decompression (23). Before knotting, the retriever was used to retrieve the sutures to the same soft tissue portal, and then the fascia cannula was inserted along the sutures to help avoid soft tissue incarceration. Under the arthroscopic supervision, knot in the fascia cannula should be fastened to prevent lamina reclosure.
However, the described technique has some limitations. The operation should be performed by experienced surgeons and assistants. Large sample studies in multicenters should be conducted to determine further clinical outcomes. With the development of surgical instruments and techniques, plate and screw fixation on the hinge side may be a better choice.
In conclusion, we described a bilateral biportal laminoplasty for the treatment of cervical stenosis. With the innovation of endoscopic instruments and techniques, this modified technique will play a role in cervical disorders.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by institutional review board of Hangzhou TCM hospital. The patients/participants provided their written informed consent to participate in this study.
Conceptualization, CZ and HP; methodology, WZ; validation, WZ and HP; investigation, WC; resources, DW; writing-original draft preparation, CZ; writing-review and editing, WZ; supervision, HP; project administration, JW. All authors contributed to the article and approved the submitted version.
This work was supported by Grants from the National Key R&D program of China (2019YFC0121400). The funds will provide support in terms of article processing charge.
Thanks are due to Li Zhu for assistance with the operation and to Hang Zhu for valuable discussion.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.913456/full#supplementary-material.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction. J Orthop Sports Phys Ther. (2009) 39:172–8. doi: 10.2519/jospt.2009.2938
2. Asher AL, Devin CJ, Kerezoudis P, Chotai S, Nian H, Harrell FE Jr, et al. Comparison of outcomes following anterior vs posterior fusion surgery for patients with degenerative cervical myelopathy: an analysis from quality outcomes database. Neurosurgery. (2019) 84:919–26. doi: 10.1093/neuros/nyy144
3. Yuan H, Zhang XF, Zhang L M, Yan YQ, Liu YK, Lewandrowski KU. Comparative study of curative effect of spinal endoscopic surgery and anterior cervical decompression for cervical spondylotic myelopathy. J Spine Surg. (2020) 6(S1):S186–96. doi: 10.21037/jss.2019.11.15
4. Carr DA, Abecassis IJ, Hofstetter CP. Full endoscopic unilateral laminotomy for bilateral decompression of the cervical spine: surgical technique and early experience. J Spine Surg. (2020) 6(2):447–56. doi: 10.21037/jss.2020.01.03
5. Li C, Tang X, Chen S, Meng Y, Zhang W. Clinical application of large channel endoscopic decompression in posterior cervical spine disorders. BMC Musculoskelet Disord. (2019) 20(1):548. doi: 10.1186/s12891-019-2920-6
6. Minamide A, Yoshida M, Yamada H, Nakagawa Y, Maio K, Kawai M, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J. (2010) 19(3):487–93. doi: 10.1007/s00586-009-1233-0
7. Eun SS, Eum JH, Lee SH, Sabal LA. Biportal endoscopic lumbar decompression for lumbar disk herniation and spinal canal stenosis: a technical note. J Neurol Surg A Cent Eur Neurosurg. (2017) 78(4):390–6. doi: 10.1055/s-0036-1592157
8. Choi CM, Chung JT, Lee SJ, Choi DJ. How i do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir. (2016) 158(3):459–63. doi: 10.1007/s00701-015-2670-7
9. Ahn JS, Lee HJ, Choi DJ, Lee KY, Hwang SJ. Extraforaminal approach of biportal endoscopic spinal surgery: a new endoscopic technique for transforaminal decompression and discectomy. J Neurosurg Spine. (2018) 28(5):492–8. doi: 10.3171/2017.8.SPINE17771
10. Kim JE, Choi DJ. Unilateral biportal endoscopic decompression by 30° endoscopy in lumbar spinal stenosis: technical note and preliminary report. J Orthop. (2018) 15(2):366–71. doi: 10.1016/j.jor.2018.01.039
11. Kim JE, Choi DJ. Bi-portal Arthroscopic Spinal Surgery (BASS) with 30° arthroscopy for far lateral approach of L5-S1 – technical note. J Orthop. (2018) 15(2):354–8. doi: 10.1016/j.jor.2018.01.034
12. Park JH, Jun SG, Jung JT, Lee SJ. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics. (2017) 40(5):1. doi: 10.3928/01477447-20170531-02
13. Kim J, Heo DH, Lee DC, Chung HT. Biportal endoscopic unilateral laminotomy with bilateral decompression for the treatment of cervical spondylotic myelopathy. Acta Neurochir. (2021) 163(9):2537–43. doi: 10.1007/s00701-021-04921-0
14. Minamide A, Yoshida M, Simpson AK, Yamada H, Hashizume H, Nakagawa Y, et al. Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study. J Neurosurg Spine. (2017) 27(4):1–7. doi: 10.3171/2017.2.SPINE16939
15. Merter A, Karaeminogullari O, Shibayama M. Comparison of radiation exposure among 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. (2020) 139:e572–9. doi: 10.1016/j.wneu.2020.04.079
16. Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev. (2019) 42(3):753–61. doi: 10.1007/s10143-019-01114-3
17. Song KS, Lee CW. The biportal endoscopic posterior cervical inclinatory foraminotomy for cervical radiculopathy: technical report and preliminary results. Neurospine. (2020) 17(Suppl 1):S145–53. doi: 10.14245/ns.2040228.114
18. Zhu C, Cheng W, Wang D, Pan H, Zhang W. A helpful third portal for unilateral biportal endoscopic decompression in patients with cervical spondylotic myelopathy: a technical note. World Neurosurg. (2022) 161:75–81. doi: 10.1016/j.wneu.2022.02.021
19. Kurokawa Y, Yokoyama Y, Kuroda K, Koruprolu S, Paller D, Nakano A, et al. Biomechanical evaluation of the suture anchors used in open-door laminoplasty: a cadaveric study. Spine. (2014) 39(21):E1248–55. doi: 10.1097/BRS.0000000000000522
20. Soliman HM. Irrigation endoscopic discectomy: a novel percutaneous approach for lumbar disc prolapse. Eur Spine J. (2013) 22(5):1037–44. doi: 10.1007/s00586-013-2701-0
21. Ergün S, Akgün U, Barber FA, Karahan M. The clinical and biomechanical performance of all-suture anchors: a systematic review. Arthrosc Sports Med Rehabil. (2020) 2(3):e263–75. doi: 10.1016/j.asmr.2020.02.007
22. Shrestha D, Miao J, Zhang J, Qiang BJ. Effect of titanium niniplate fixation on hinge fracture and hinge fracture displacement following cervical open-door laminoplasty. Int J Spine Surg. (2020) 14(4):7061. doi: 10.14444/7061
23. Gu Z, Zhang A, Shen Y, Li F, Sun X, Ding W. Relationship between the laminoplasty opening size and the laminoplasty opening angle, increased sagittal canal diameter and the prediction of spinal canal expansion following open-door cervical laminoplasty. Eur Spine J. (2015) 24(8):1613–20. doi: 10.1007/s00586-015-3779-3
Keywords: bilateral biportal endoscopy, cervical laminoplasty, suture anchor, endoscopic spine surgery, cervical stenosis
Citation: Zhu C, Wang J, Cheng W, Wang D, Pan H and Zhang W (2022) Case Report: Bilateral Biportal Endoscopic Open-Door Laminoplasty With the Use of Suture Anchors: A Technical Report and Literature Review. Front. Surg. 9:913456. doi: 10.3389/fsurg.2022.913456
Received: 5 April 2022; Accepted: 18 May 2022;
Published: 7 June 2022.
Edited by:
Zhen-Zhou Li, Fourth Medical Center of PLA General Hospital, ChinaReviewed by:
Pang Hung Wu, Ng Teng Fong General Hospital, SingaporeCopyright © 2022 Zhu, Wang, Cheng, Wang, Pan and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Zhang; dm9sY2FubzgwNjBAMTYzLmNvbQ==
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.