- 1Hunan Provincial People’s Hospital (The First-Affiliated Hospital of Hunan Normal University), Changsha, China
- 2Department of Nursing, School of Medicine, Hunan Normal University, Changsha, China
Objectives: This study aimed to investigate the correlation between self-care ability, psychological status, and quality of life in patients with hepatolithiasis complicated with diabetes mellitus with T-tube.
Methods: The purpose of this study was to select a total of 240 patients with hepatolithiasis complicated with diabetes with T-tube from June to September 2019 in a Third-class Grade A hospital in Changsha, Hunan Province. Self-designed general information questionnaire, self-care ability implementation scale (ESCA), self-rating anxiety scale (SAS), self-rating depression scale (SDS), and quality of life scale (SF-36) were used to conduct a questionnaire survey. The correlation among self-care ability, psychological status, and quality of life of patients with hepatolithiasis complicated with diabetes mellitus with T-tube was analyzed.
Results: The total score of self-care ability of 240 patients with hepatolithiasis combined with diabetes with T-tube was positively correlated with the total score of quality of life (p < 0.05). The standard scores of anxiety and depression were negatively correlated with the total score of quality of life (p < 0.05). The total score of self-care ability was negatively correlated with the standard score of anxiety and depression (p < 0.05).
Conclusion: Improving the self-care ability of patients with hepatolithiasis complicated with diabetes with T-tube and improving their anxiety and depression can improve their quality of life, which provides reference for further study.
Introduction
Hepatolithiasis, which is defined as the stones formed in each branch bile duct above the confluence of the left and right hepatic ducts, has a high prevalence in Asia (1–3). In western countries, hepatolithiasis has a much lower incidence (4, 5). However, the incidence of hepatolithiasis is increasing in Western countries due to the increase in immigration from high prevalent areas (5–7). Surgical management has long been a primary treatment of hepatolithiasis, and a T-tube is usually retained after operation (8). However, the T-tube placement time is usually 2–3 months, and it can be as long as 3–6 months for complicated cases. Improper nursing will easily lead to complications such as tract infection and T-tube shedding (8).
Diabetes mellitus refers to the presence of hyperglycemia, which is a kind of prevalent chronic lifelong metabolic disease all over the world (9, 10). Various complications caused by long-term metabolic problems and continuous hyperglycemia can gradually damage the patient's tissues and organs, which results in a high mortality rate (11–13). With the change in people's lifestyle and diet structure, the incidence of hepatolithiasis with diabetes is increasing, which seriously affects the quality of life of patients with hepatolithiasis and diabetes with T-tube. Therefore, it is necessary to conduct nursing interventions and take some measures to improve their quality of life.
Previous studies reported a relationship between anxiety and depression, quality of life, and self-care ability of patients with heart failure (14, 15), colorectal cancer (16), or other diseases (17, 18). However, few literature works mention the relationship of these three factors in patients with hepatolithiasis complicated with diabetes mellitus with T tube. The purpose of our study is to research the correlation between self-care ability, psychological status, and quality of life of patients with hepatolithiasis complicated with diabetes mellitus and T-tube to provide a reference for further research.
Objectives and Methods
Research Objects
A total of 240 patients with hepatolithiasis complicated with diabetes with T-tube from June to September 2019 in a Third-class Grade A hospital in Changsha, Hunan Province were selected as the research objects.
Inclusion and Exclusion Criteria
Inclusion criteria are as follows:
(1) age: ≥18 years and ≤65 years;
(2) medical diagnosis of hepatolithiasis and diabetes mellitus, recovered and discharged with T-tube after surgical treatment; and
(3) informed consent and voluntary participants.
Exclusion criteria are as follows:
(1) those with serious complications or critical illness who can not take care of themselves;
(2) people with a history of mental illness; and
(3) those who have language communication barriers and can not communicate normally.
Research methods
The main research tools that were used in this study are as follows: a general information questionnaire, self-care ability implementation scale (ESCA), self-rating anxiety scale (SAS), self-rating depression scale (SDS), and quality of life scale (SF-36).
Survey Tools
General Information Questionnaire
The general information questionnaire includes the age, gender, family income, education level, marital status, occupation, main caregivers, and disease-related information of the subjects.
Self-Care Ability Implementation Scale
This scale was compiled by American scholars Kearney and Fleischer (19), and Cronbach's α coefficient was 0.86–0.92 (20). There are 43 items that include four dimensions: self-concept, self-care responsibility, self-care skills, and health knowledge level. Each item of the scale scored from 0 to 4, with a total score of 172. The higher the score, the stronger the self-care ability. The level of self-care ability is evaluated by a scoring index. The scoring index >66% is in a high grade, 33%–66% is in a medium grade, and <33% is in a low grade.
Self-Rating Anxiety Scale
This scale was developed by Zung (21), and Cronbach's α coefficient was 0.807. There are 20 items in total, which are described by a standard score. Standard score = total rough score × 1.25. The score index <50 is normal, 50–59 is mild anxiety, 60–69 is moderate anxiety, and >69 is severe anxiety. The higher the standard score, the more severe the symptoms.
Self-Rating Depression Scale
SDS was compiled by Zung (22), and Cronbach’s α coefficient was 0.854. There are 20 items in total, which are described by a standard score. The higher the standard score, the more severe the symptoms are. The cut-off value of the SDS standard score is 53, of which <53 is normal, 53–62 is mild depression, 63–72 is moderate depression, and >73 is severe depression.
Quality of Life Scale (SF-36)
The quality of life scale (SF-36) adopts the Chinese version of the reliability and validity scale tested by Li’s team (23), and Cronbach's α coefficient is 0.763. SF-36 has 36 items in total that include eight health dimensions and a self-assessment of health changes. These health dimensions are role-physical (RP), mental health (MH), vitality (VT), bodily pain (BP), social functioning (SF), physiological functioning (PF), general health (GH), and role-emotional (RE). Eight dimensions are divided into the mental health field and the physical health field. The total score of quality of life is the sum of scores in eight dimensions. The higher the score, the better the patient’s quality of life.
Statistical Methods
Statistical analysis was performed on all experimental data using SPSS 20.0 software. The data on frequency, percentage, and Spearman rank correlation were analyzed.
Results and Discussion
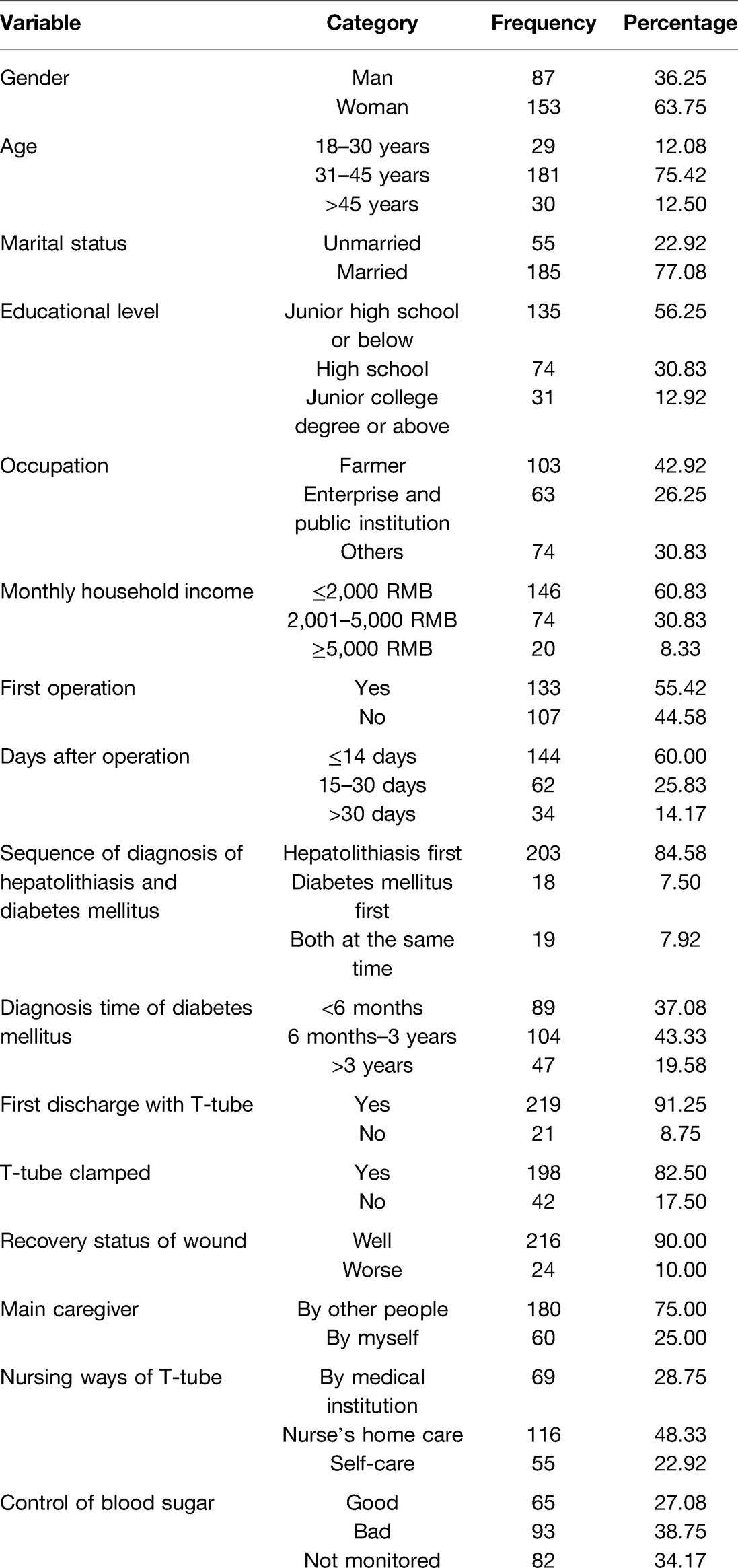
In this study, a total of 248 questionnaires were sent out, of which 240 were valid. The effective recovery rate was 96.7%. There are 87 males and 153 females (Table 1).
As shown in Table 2, the total score of self-care ability was negatively correlated with the standard score of anxiety and depression (r = −0.424, −0.400, p < 0.05). Additionally, the score of each dimension has negative significance with psychological status. Therefore, the stronger the self-care ability of patients with hepatolithiasis and diabetes with T tube, the better their psychological status, and vice versa. This is consistent with the research results of scholars such as Patrick (24). The reason may be that patients with good self-care ability know the importance of self-care, which can stimulate their self-responsibility to actively learn relevant health knowledge and nursing skills from passive acceptance to active participation. Patients know more about diseases and nursing knowledge so that they can treat diseases correctly and maintain a good psychological state to enhance patients’ confidence in overcoming diseases.
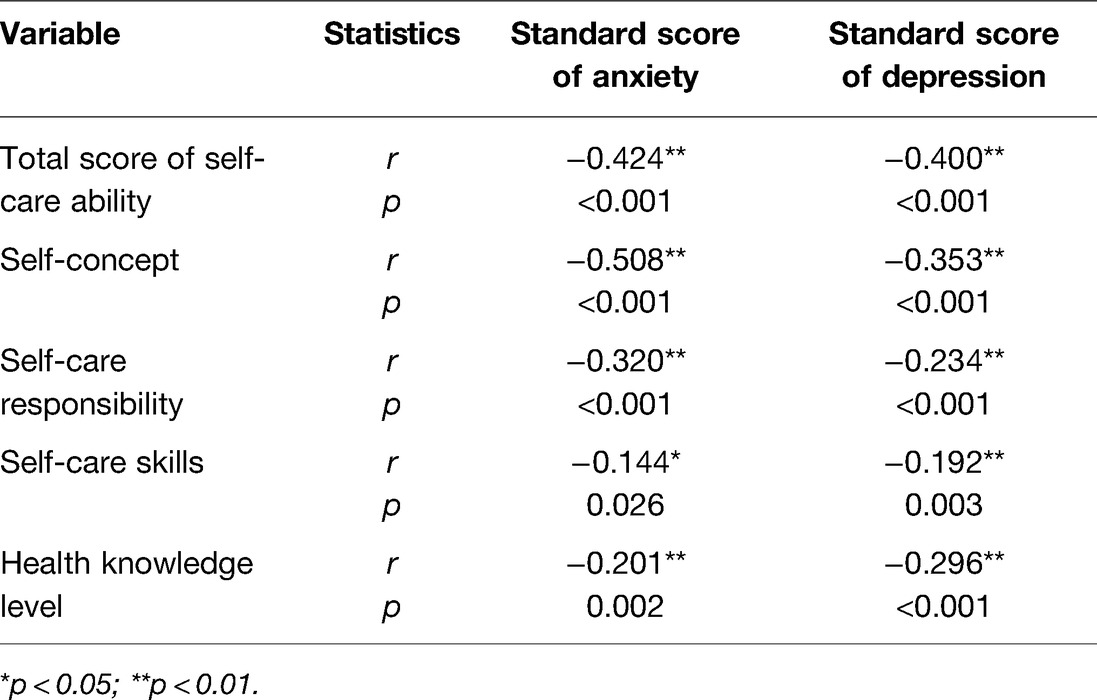
Table 2. Correlation between self-care ability and psychological status of discharged patients with hepatolithiasis and diabetes mellitus with T-tube (n = 240).
The results of Table 3 showed that the total score of the SF-36 scale was positively correlated with the total score of self-concept, self-care responsibility, self-care skills, and health knowledge level (r = 0.263, p < 0.05). It is consistent with the results of Patrick (24) and Kessing (25). From the table, we found that the higher quality of life of patients with hepatolithiasis complicated with diabetes mellitus and T-tube was closely related to their stronger self-care ability. The main reasons are that patients having strong self-concept and awareness of self-recognition can cooperate with the medical treatment positively so as to improve their body function and their quality of life. Therefore, nursing staff should improve patients’ weaknesses in personalize training and health education in continuing home care to improve their quality of life.
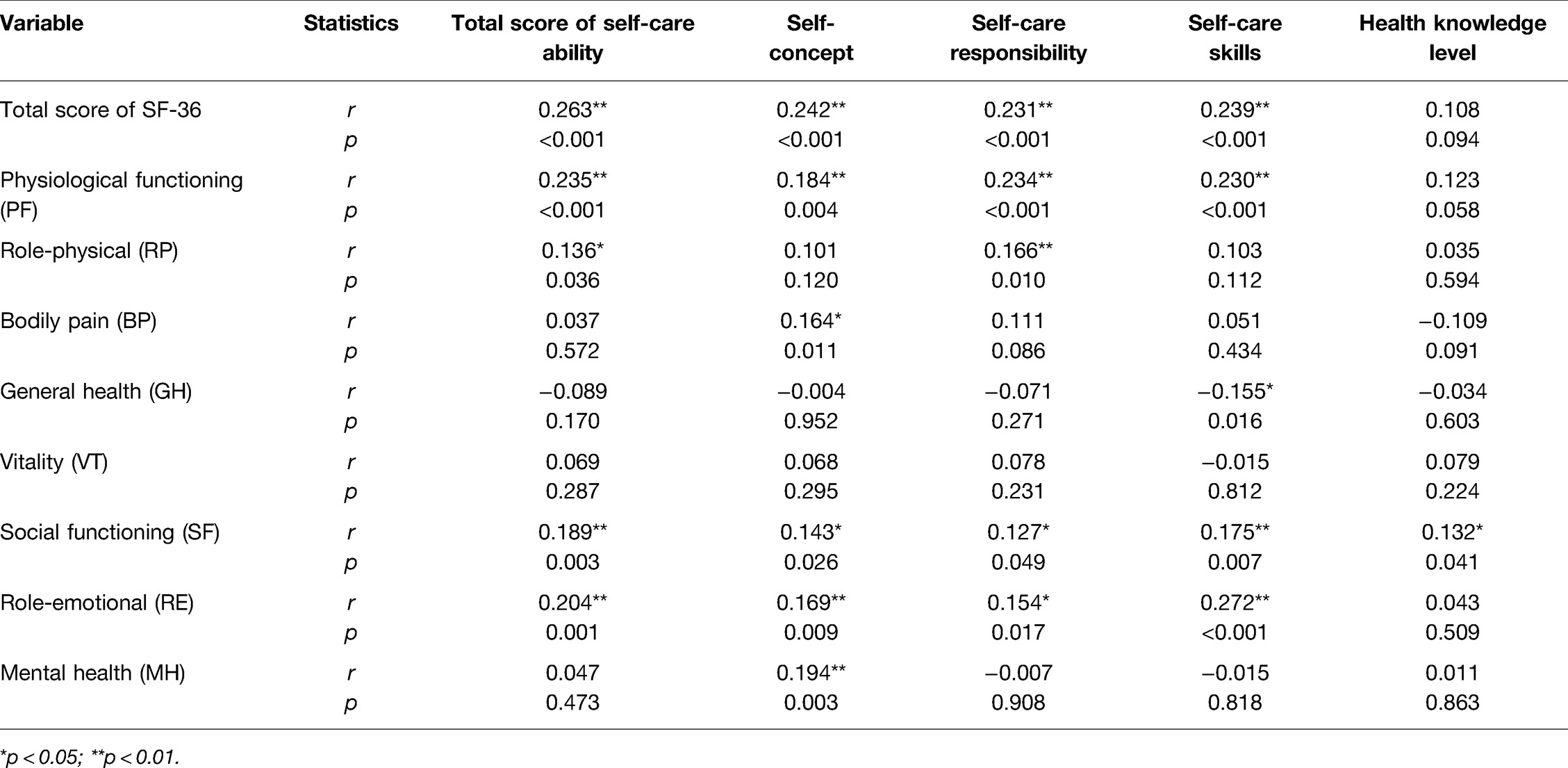
Table 3. Correlation between self-care ability and quality of life in discharged patients with hepatolithiasis and diabetes mellitus with T-tube (n = 240).
As shown in Table 4, the total score of the SF-36 scale was negatively correlated with the standard score of anxiety and depression (r = −0.285, −0.266, p < 0.05). Therefore, the better the psychological status of discharged patients with hepatolithiasis and diabetes mellitus with T-tube, the higher the patients’ quality of life, and vice versa. The results were consistent with the research results of Patrick (24) and Park (26). Although hepatolithiasis is a benign disease, it has a high recurrence rate with some complications (27). Diabetes mellitus is a typical physical and mental disease with a long course and many complications (28). Patients with hepatolithiasis complicated with diabetes mellitus and T-tube are prone to psychological problems and stress due to their awareness of the difficulty in curing their diseases completely and the inconvenience of these diseases to their daily life and social work, which will lead to abnormal emotional control and result in a significant negative impact on their quality of life. Therefore, in the management and treatment of patients with hepatolithiasis complicated with diabetes, we should not only pay attention to the improvement of patients’ physiological functions but also intervene in the factors that affect their psychology and life behavior.
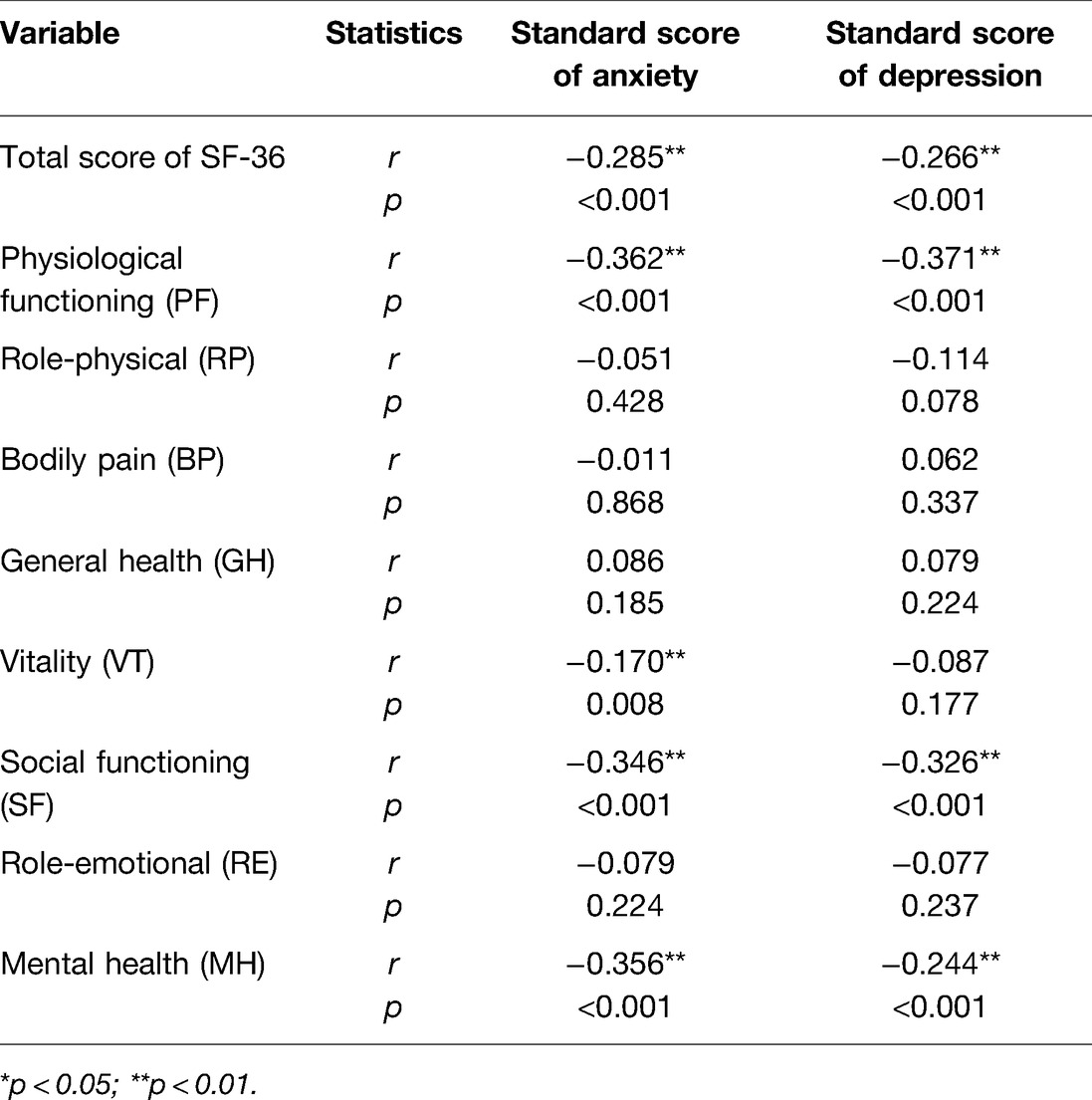
Table 4. Correlation between psychological status and quality of life in discharged patients with hepatolithiasis and diabetes mellitus with T-tube (n = 240).
Conclusion
Our study focused on exploring the correlation between self-care ability, psychological status, and quality of life in discharged patients with hepatolithiasis complicated with diabetes mellitus and T-tube. Data showed that (1) patients’ self-care ability was negatively associated with their psychological status (p < 0.05), (2) self-care ability of 240 patients with hepatolithiasis combined with diabetes and T-tube was positively correlated with their quality of life (p < 0.05), and (3) psychological status has a negative difference with the quality of life (p < 0.05). From the results, it can be seen that stronger self-care ability and lower anxiety and depression level were closely related to the higher quality of life.
In this work, we demonstrated that promoting the self-care ability of patients with hepatolithiasis complicated with diabetes and T-tube and improving their psychological status can improve their quality of life. Our findings highlight the necessity of psychological interventions and guidance of self-recognition of patients, which provide a reference for further study on the improvement of quality of life for this population.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by The Ethical Review Committee of Hunan Provincial People’s Hospital (The First-Affiliated Hospital of Hunan Normal University). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CH and YW contributed to the conception and design of the study and wrote the first draft of the manuscript. YC contributed to manuscript revision, reading, and project management. ZS, HZ, ZT, HC, and BZ contribute to data collection and analysis. All authors contributed to the article and approved the submitted version.
Funding
The work is supported by Hunan Provincial People’s Hospital (The First-Affiliated Hospital of Hunan Normal University).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lorio E, Patel P, Rosenkranz L, Patel S, Sayana H. Management of hepatolithiasis: review of the literature. Curr Gastroenterol Rep. (2020) 22(6):30. doi: 10.1007/s11894-020-00765-3
2. Xiao Z, Huang Z, Gao J, Wang J, Lei J, Zhou F, et al. The imbalance of biliary microflora in hepatolithiasis. Microb Pathog. (2021) 157:104966. doi: 10.1016/j.micpath.2021.104966
3. Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol. (2015) 21(48):13418–31. doi: 10.3748/wjg.v21.i48.13418
4. Kayhan B, Akdogan M, Parlak E, Ozarslan E, Sahin B, et al. Hepatolithiasis: a Turkey experience. Turk J Gastroenterol. (2007) 18(1):28–32. https://www.turkjgastroenterol.org/en/hepatolithiasis-a-turkey-experience-162143117450492
5. Li C, Wen T. Surgical management of hepatolithiasis: a minireview. Intractable Rare Dis Res. (2017) 6(2):102–5. doi: 10.5582/irdr.2017.01027
6. Mori T, Sugiyama M, Atomi Y. Gallstone disease: management of intrahepatic stones. Best Pract Res Clin Gastroenterol. (2006) 20(6):1117–37. doi: 10.1016/j.bpg.2006.05.010
7. Al-Sukhni W, Gallinger S, Pratzer A, Wei A, Ho CS, Kortan P, et al. Recurrent pyogenic cholangitis with hepatolithiasis - the role of surgical therapy in North America. J Gastrointest Surg. (2008) 12(3):496–503. doi: 10.1007/s11605-007-0398-2
8. Ambreen M, Shaikh AR, Jamal A, Qureshi JN, Dalwani AG, Memon MM, et al. Primary closure versus T-tube drainage after open choledochotomy. Asian J Surg. (2009) 32(1):21–5. doi: 10.1016/S1015-9584(09)60004-X
9. Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand Spec Suppl. (2022) 37(1):61–6. doi: 10.7748/ns.2021.e11709
10. Lu M, Pilla SJ, Oh SH. Diabetes mellitus: dietary management. Reference Module in Food Science. (2021). https://www.sciencedirect.com/science/article/pii/B9780128218488000214
11. Chowdhury T, Shaho S, Moolla A. Complications of diabetes: progress, but significant challenges ahead. Ann Transl Med. (2014) 2(12):120. doi: 10.3978/j.issn.2305-5839.2014.08.12
12. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract Suppl. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
13. Saeedi P, Salpea P, Karuranga S, Petersohn I, Malanda B, Gregg EW, et al. Mortality attributable to diabetes in 20-79 years old adults, 2019 estimates: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. (2020) 162:108086. doi: 10.1016/j.diabres.2020.108086
14. Patrick M, Miller B, Will B, Bena JF, Morrison SL, Siegmund LA, et al. Anxiety and depression moderate the relationship between quality of life and self-care in patients with heart failure. Geriatr Nurs. (2022) 44:54–9. doi: 10.1016/j.gerinurse.2021.12.020
15. Patron E, Benvenuti SM, Lopriore V, Roest AM, Thombs BD, Grace SL, Stewart DE, Abbey SE, de Jonge P, et al. Somatic-affective, but not cognitive-depressive symptoms are associated with reduced health-related quality of life in patients with congestive heart failure. Psychosomatics. (2017) 58(3):281–91. doi: 10.1016/j.psym.2017.01.001
16. Zhou L, Sun H. The effect of reminiscence therapy-involved care on anxiety, depression, life quality and survival in colorectal cancer patients. Clin Res Hepatol Gastroenterol. (2021) 45(3):101546. doi: 10.1016/j.clinre.2020.09.007
17. Cho S, Cho O-H. Depression and quality of life in older adults with pneumoconiosis: the mediating role of death anxiety. Geriatr Nurs. (2022) 44:215–20. doi: 10.1016/j.gerinurse.2022.02.018
18. Park J-M, Bae S-M. Impact of depressive, anxiety, and PTSD symptoms in disaster victims on quality of life: the moderating effect of perceived community resilience. Int J Disaster Risk Reduct. (2022) 69:102749. doi: 10.1016/j.ijdrr.2021.102749
19. Kearny B, Fleischer B. Development of all instrument measure exercise of self-care agency. Res Nurs Health. (1979) 2(1):25–34. doi: 10.1002/nur.4770020105
20. Wang H-H, Laffrey SC. Preliminary development and testing of instruments to measure self-care agency and social support of women in Taiwan. Kaohsiung J Med Sci. (2000) 16(9):459–467. https://pubmed.ncbi.nlm.nih.gov/11271731/11271731
21. Zung WWK. Prevalence of clinically significant anxiety in a fancily practice setting. Am J Psychiatry. (1986) 143(11):1471–2. doi: 10.1176/ajp.143.11.1471
22. Zung WWK. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12(1):63–70. doi: 10.1001/archpsyc.1965.01720310065008
23. Li L, Wang HM, Shen Y. Chinese SF-36 health survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health. (2003) 57(4):259–63. doi: 10.1136/jech.57.4.259
24. Patrick M, Miller B, Will B, Bena JF, Morrison SL, Siegmund, LA, et al. Anxiety and depression moderate the relationship between quality of life and self-care in patients with heart failure. Geriatr Nurs. (2022) 44:54–9. doi: 10.1016/j.gerinurse.2021.12.020
25. Kessing D, Denollet J, Widdershoven J, Kupper N, et al. Self-care and health-related quality of life in chronic heart failure: a longitudinal analysis. Eur J Cardiovasc Nurs. (2017) 16(7):605–13. doi: 10.1177/1474515117702021
26. Park J-M, Bae S-M. Impact of depressive, anxiety, and PTSD symptoms in disaster victims on quality of life: the moderating effect of perceived community resilience. Int J Disaster Risk Reduct. (2022) 69:102749. doi: 10.1016/j.ijdrr.2021.102749
27. Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol. (2015) 21:13418. doi: 10.3748/wjg.v21.i48.13418
Keywords: Hepatolithiasis complicated with diabetes mellitus, T-tube, self-care ability, psychological status, quality of life
Citation: Huang C, Wang Y, Cai Y, Shen Z, Zhang H, Tan Z, Chen H and Zhou B (2022) Correlation Among Self-Care Ability, Psychological Status, and Quality of Life in Discharged Patients with Hepatolithiasis Complicated with Diabetes Mellitus and T-Tube. Front. Surg. 9:907900. doi: 10.3389/fsurg.2022.907900
Received: 30 March 2022; Accepted: 19 April 2022;
Published: 16 May 2022.
Edited by:
Weiguo Li, Harbin Institute of Technology, ChinaReviewed by:
Yunrun Liu, Hong Kong Baptist University, ChinaHongwen Wu, Liuzhou Workers Hospital, China
Copyright © 2022 Huang, Wang, Cai, Shen, Zhang, Tan, Chen and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yimin Cai eWltaW4uY2FpQG91dGxvb2suY29t
†These authors have contributed equally to this work and share first authorship.
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Chunqiu Huang1†
Chunqiu Huang1† Yimin Cai
Yimin Cai