- 1Himchan UHS Spine and Joint Centre, Neurosurgery, University Hospital Sharjah, University City 1, Sharjah, United Arab Emirates
- 2Joint and Arthritis Research, Orthopaedic Surgery, Himchan Hospital, Seoul, Korea
- 3Department of Pharmaceutical Medicine and Regulatory Sciences, College of Medicine and Pharmacy, Yonsei University, Seoul, Korea
- 4Himchan UHS Spine and Joint Centre, Orthopedic Surgery, University Hospital Sharjah, Sharjah, University City 1, Sharjah, United Arab Emirates
- 5Himchan UHS Spine and Joint Centre, Physiotherapy, University Hospital Sharjah, University City 1, Sharjah, United Arab Emirates
The coronavirus disease (COVID-19) pandemic has influenced hospital visiting patterns. Although vaccination has decreased infection rates and disease severity, hospital visiting patterns and associated treatment changes related to orthopedics remain unexplored in the Middle East. Therefore, this study aimed to examine the impact of the COVID-19 pandemic and vaccination on individual departments dealing with musculoskeletal disorders in the United Arab Emirates. Relationships between publicly available national data on the number of COVID-19 polymerase chain reaction tests and confirmed and recovered cases during May 2020–July 2021 and hospital data on the number of outpatients, inpatients, operations, and physiotherapy consultations were analyzed. In January 2021, the relationship between vaccination rate and orthopedic unit utilization was evaluated after vaccination campaign initiation. Multifactorial analysis revealed that an increased number of COVID-19-related deaths correlated with a decreased number of joint operations. Negative linear relationships were observed among confirmed and death cases with inpatient treatment and joint operation as well as recovered cases with inpatient treatment. Recovered cases with inpatient treatment and joint operation showed a positive linear relationship. Inpatient spine treatment showed a positive relationship with vaccination rates. The COVID-19 pandemic influenced orthopedic treatment in the Middle East, and vaccination campaigns facilitated inpatient spine treatment.
Introduction
The coronavirus disease (COVID-19) pandemic has affected individuals’ social behaviors, including the frequency of hospital visits. There has been a significant decrease in the number of hospital treatments delivered across specialties (except those managing COVID-19 cases), especially in the emergency and outpatient departments (1, 2). Although this trend has been observed for all in-hospital treatments, nonvital departments have been less affected than vital departments (3). Orthopedic treatments, especially those related to the spine, have been shown to improve patient quality of life. Furthermore, failure of timely treatment can be detrimental and decrease survival rates (4). After the large-scale implementation of vaccination and emergent approval for vaccination by the World Health Organization, it is expected that individuals’ social lives will normalize, and the pattern of hospital visits will improve before the pandemic ends. However, the pandemic and vaccination impacts on the orthopedic field in Middle Eastern countries have not yet been reported. This study aimed to evaluate the effects of the COVID-19 pandemic and the vaccination campaign in the United Arab Emirates (UAE) on the different types of orthopedic treatments being delivered.
Materials and Methods
This was an observational study related to the effects of the COVID-19 pandemic (May 2020 to July 2021) at a single center specializing in spine and joint treatments at a tertiary hospital (Himchan Spine and Joint Center, University Hospital Sharjah) in the UAE. This study was approved by the Institutional Review Board of University Hospital Sharjah (approval no: UHS-HERC-077-15112021). The vaccination campaign analysis was initiated after approval of the Ministry of Health of the UAE (January to July 2021). The hospital data related to the type of treatment delivered (outpatient, inpatient, operation, and physiotherapy) were managed using a computerized system and organized by the administration team (S. Park and H. Jin). The term “operation” in this study corresponded to a major operation in the operating theater and did not include percutaneous injection procedures in the outpatient clinic. All physician therapists and nurses always wore N-95 masks during outpatient treatment and surgery. Faceguards were used throughout treatment from May to October 2020; however, after that period, a mask was worn before and after every procedure, and handwashing was done. In the spine department, the main treatment methods were diagnosis, injection in the outpatient clinic, laminectomy and fusion surgery. Degenerative disease, trauma injection and conservative treatment were done in the outpatient section of the joint department, and surgery was mainly for fracture, arthroscopy, and joint replacement. Open data related to COVID-19 tests confirmed and recovered cases, deaths, and vaccination rates in the UAE are used by the National Emergency Crisis and Disaster Management Authority (NCEMA) to inform the general public. The open data have been used to acquire information on the polymerase chain reaction (PCR) tests conducted and determine the monthly count of the numbers of confirmed, recovered, and death cases. All data strictly followed the open data policy in NCEMA, and personal data were not used in this study. Data regarding in-hospital visits included outpatient visits, inpatient admissions, and operation counts in each department of the spine, joint, and physiotherapy center. From May to July 2020, the hospital used 1–2 wards for corona treatment, admission beds were decreased, and non-urgent operations were recommended to be delayed. Our infection control committee strictly controlled the preventive methods for Covid-19 infection. Body temperature and a questionnaire for related symptoms were evaluated in the outpatient clinic and physiotherapy. Visitors were not allowed without being accompanied by one guardian. N-95 Mask use and hand hygiene were mandatory for our staff. Vaccination campaigns started in the UAE in January 2021. Three vaccines are currently available: BBIBP-Corv (Sinopharm, Beijing CNBG, Beijing, China), Pfizer-BioNTech (Pfizer, Inc., Philadelphia, PA, USA), and Sputnik V COVID-19 vaccine (Gam-COVID-Vac, Gamaleya Research Institute of Epidemiology and Microbiology, Moscow, Russia).
Statistical analyses were performed using the R software for Windows (version 3.6.0, Vienna, Austria). The factors affecting the patient count at hospitals were analyzed using multiple regression analysis. Correlation analysis between two variables was performed using linear analysis with Pearson’s correlation coefficient (Pearson’s r). Statistical significance was set at p-values <0.05.
Results
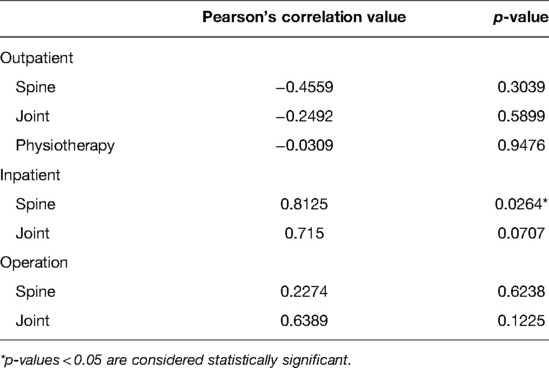
The national data on COVID-19 cases and hospital utilization are summarized in Table 1.
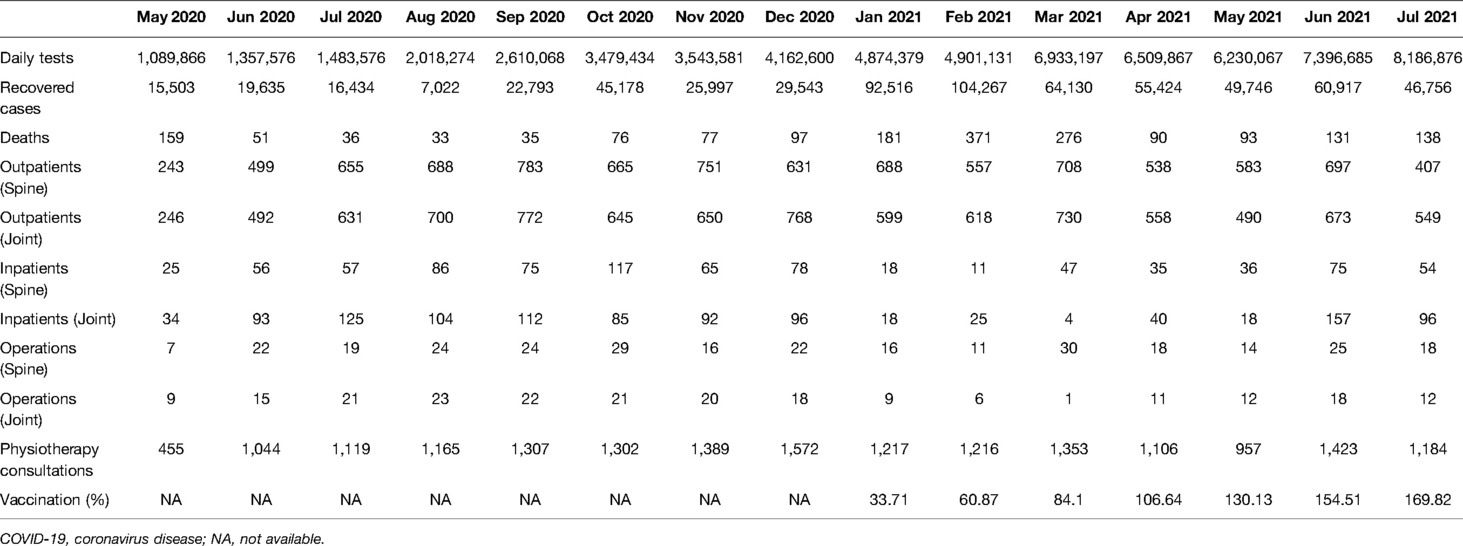
Table 1. Patient number (outpatient and inpatient), operation count, and physiotherapy consultation during the COVID-19 pandemic in the United Arab Emirates.
COVID-19 PCR Test, Confirmed Cases, and Orthopedic Treatment
The number of PCR tests conducted showed an increasing trend until July 2021, with a monthly count reaching approximately 8 million cases (Figure 1A). The number of confirmed cases peaked in January 2021 at approximately 80,000 cases/month and decreased spontaneously to 40,000 cases /month in July 2021. Recovered cases peaked at 1,000,000/month in February 2021 and showed a decreasing trend similar to that of the confirmed cases (Figure 1B). After the number of confirmed COVID-19 cases increased in January 2021, outpatient counts in the joint and physiotherapy departments decreased spontaneously until July 2021 (Figure 1C). The spine department showed a continuous outpatient count of approximately 600 cases per month compared with other departments. Patient counts fluctuated more in the joint department than in that of the spine after the peak duration (from January 2020 to March 2021), i.e., the number of reported inpatient cases increased dramatically to 140 cases per month (Figure 1D). Furthermore, joint operations varied more than spine operations; they decreased until February 2021 and peaked in March 2021. Spine operations showed stable counts, except in March 2021 (Figure 1E). The vaccination rate in the UAE, after the campaign initiation in December 2020, increased monthly and approached an accumulated rate of 169.8% in July 2021 (Figure 1F).
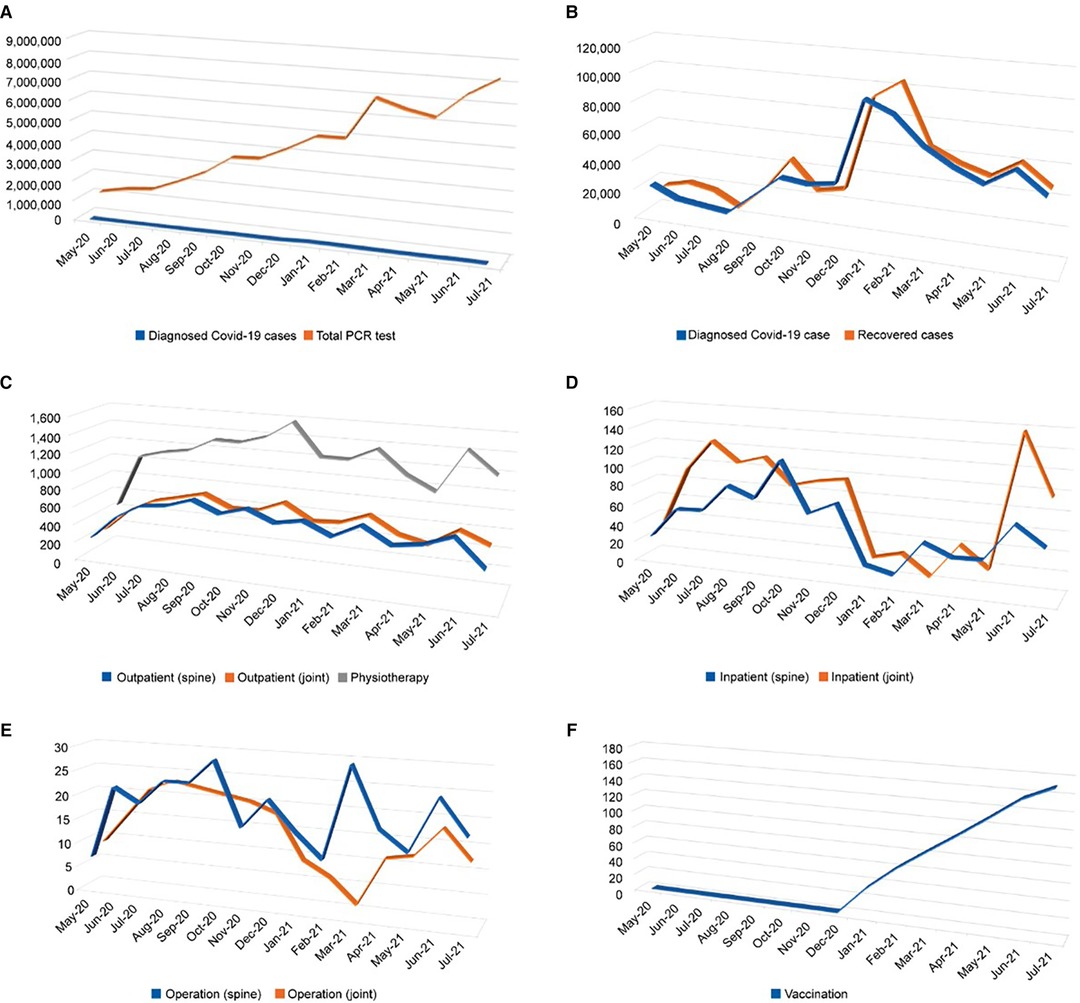
Figure 1. Graphs of national data of coronavirus disease 2019 (COVID-19) and hospital visiting patterns. (A) Diagnosed cases and number of polymerase chain reaction (PCR) tests; (B) Diagnosed and recovered cases; (C) Outpatient count in each department; (D) Inpatient count in each department; (E) Operation count in each department; (F) Vaccination rate.
Multiple Regression Analysis Considering COVID-19 and the Use of Orthopedic Treatments
The influences of various parameters related to COVID-19 on orthopedic department utilization are summarized in Table 2. Outpatient counts across departments, including those related to the spine, joints, and physiotherapy, were not affected. Regarding inpatient treatment, diagnosis in the joint department (p = 0.2341) and death count in both the departments (spine: p = 0.2689; joint: p = 0.2409) had negative relationships with the increase in COVID-19 cases, but these differences were not significant. The operation count in the joint department was only affected by the death count in all multiple regression analyses (p = 0.0112).
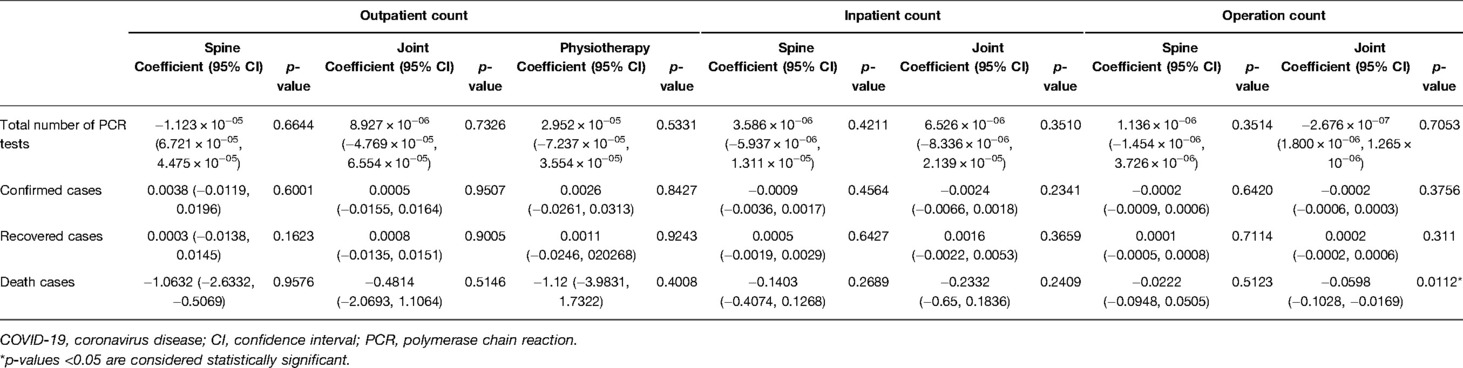
Table 2. Multiple regression analysis regarding COVID-19 in our orthopedic clinic in the United Arab Emirates.
Linear Relationships Between PCR Tests and Use of Orthopedic Treatments
The relationships between COVID-19 and orthopedic department utilization are summarized in Table 3.
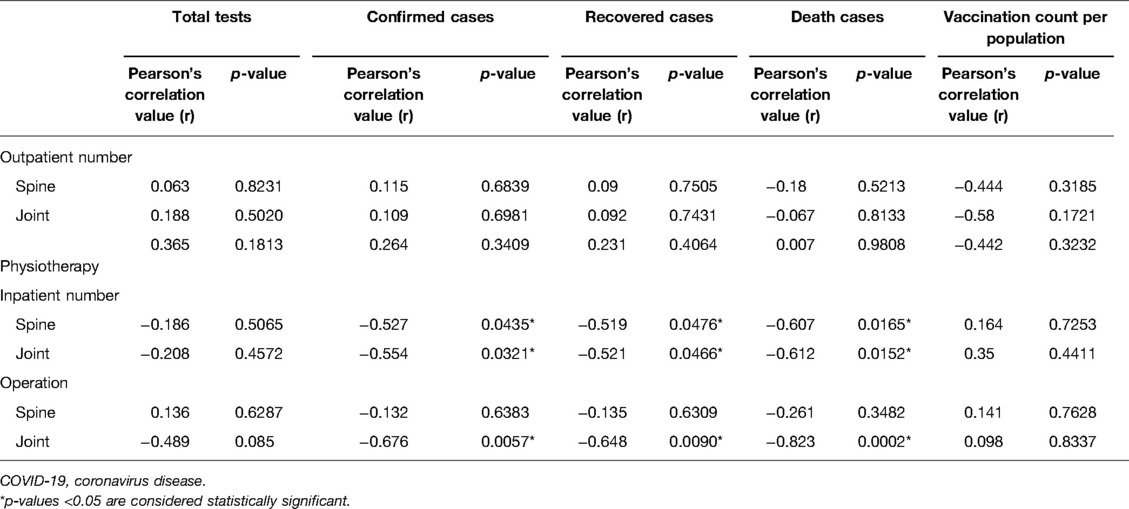
Table 3. Pearson’s correlation of COVID-19 counts and orthopedic clinics in the United Arab Emirates.
As PCR testing increased, outpatient treatment increased (spine: r = 0.063, joint: r = 0.188, Figures 2A, B) and inpatient treatment decreased (spine: r = −0.186, joint: r = −0.208, Figures 2C, D). In addition, operations in the spine department increased slightly (r = 0.136, Figure 2E), but those in the joint department decreased (r = −0.489, Figure 2F). Physiotherapy patient counts increased (r = 0.264, Figure 2G); however, these increases and decreases were not significant.
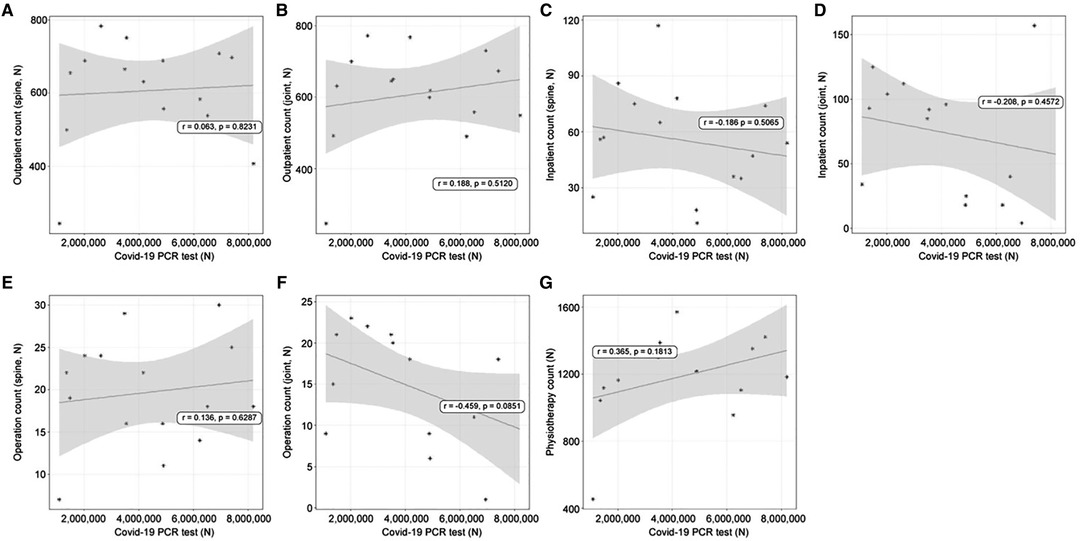
Figure 2. The linear relationships between coronavirus disease 2019 (COVID-19) polymerase chain reaction (PCR) test count and orthopedic hospital visiting patterns. (A) Spine department outpatient count; (B) Joint department outpatient count; (C) Spine department inpatient count; (D) Joint department inpatient count; (E) Spine operation patient count; (F) Joint operation patient count; (G) Physiotherapy patient count.
Linear Relationships Between Confirmed Cases and the Use of Orthopedic Treatments
With increasing diagnoses, outpatient treatment increased, but not significantly, in both the spine (r = 0.115, p = 0.6839, Figure 3A) and joint departments (r = 0.109, p = 0.6981, Figure 3B). However, inpatient treatment decreased in both the departments; the joint department showed a more significant decline (spine: r = −0.527, p = 0.0423, Figure 2C; Joint; r = −0.554, p = 0.0321, Figure 3D). Concerning operations, those of the spine (r = −0.132, p = 0.6383, Figure 2E) and joints (r = −0.459, p = 0.0851) decreased, but the differences were not significant. Physiotherapy patient counts showed an insignificant relationship (r = 0.264, p = 0.3409, Figure 3G).
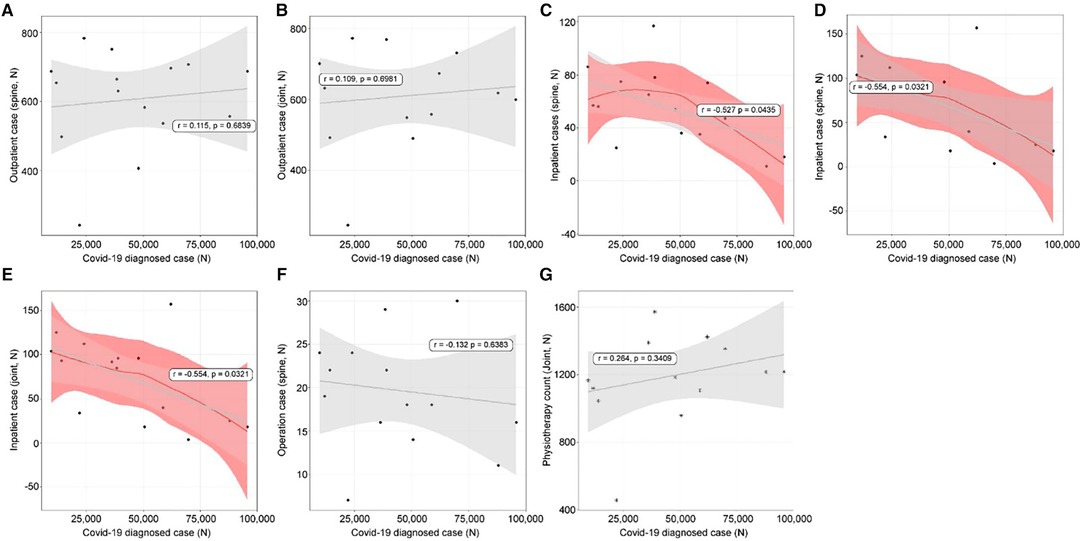
Figure 3. The linear relationships between coronavirus disease 2019 (COVID-19) diagnosis and orthopedic hospital visiting patterns. (A) Spine outpatient count; (B) Joint outpatient count; (C) Spine inpatient count; (D) Joint inpatient count; (E) Spine operation patient count; (F) Joint operation patient count; (G) Physiotherapy patient count.
Linear Relationships Between Recovered Cases and Use of Orthopedic Treatments
Recovered cases and the use of orthopedic treatments were not strongly related. Outpatient treatments (spine: r = 0.09, p = 0.7505, Figure 4A; joint: r = 0.092, p = 0.7431, Figure 4B) had insignificant decreases. Inpatient treatments (spine: r = −0.519, p = 0.0476, Figure 4C; joint: r = −0.521, p = 0.0466, Figure 4D) had significant decreases. Spine operation patient counts showed no relationship (r = −0.135, p = 0.6309, Figure 4E); however, those of the joints (r = −0.648, p = 0.0090, Figure 4F) showed a negative relationship. Physiotherapy patient counts showed an insignificant relationship (r = 0.231, p = 0.4064, Figure 4G).
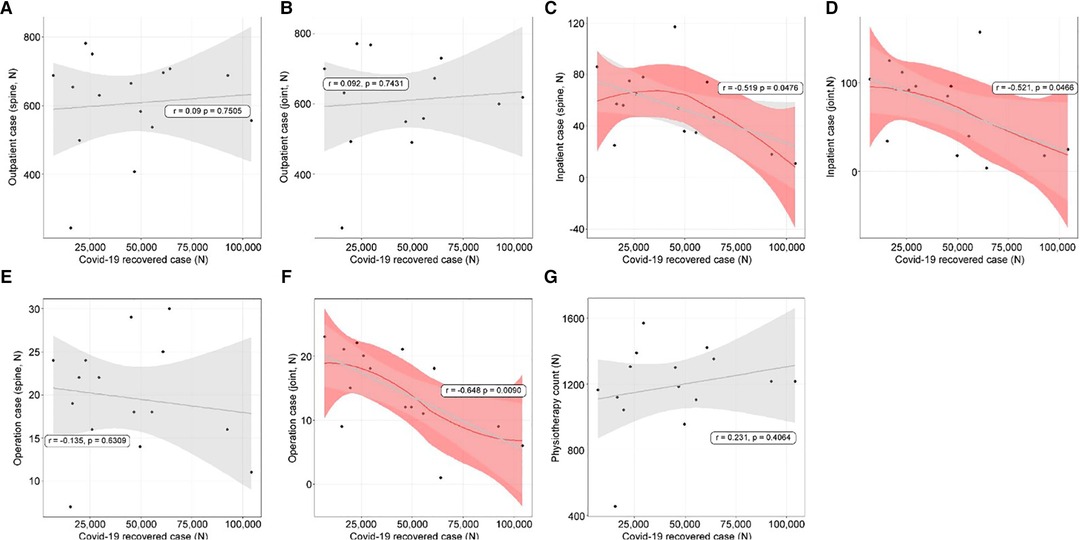
Figure 4. The linear relationships between cases that recovered from coronavirus disease 2019 (COVID-19) and orthopedic hospital visiting patterns. (A) Spine outpatient count; (B) Joint outpatient count; (C) Spine inpatient count; (D) Joint inpatient count; (E) Spine operation patient count; (F) Joint operation patient count; (G) Physiotherapy patient count.
Linear Relationships Between Death Cases and Use of Orthopedic Treatments
Death cases and the need for orthopedic treatments affect inpatient treatments and joint operations. Outpatient treatments (spine: r = −0.18, p = 0.5213, Figure 5A; joint: r = −0.067, p = 0.8133, Figure 5b) had insignificant decreases. Inpatient treatments (spine: r = −0.607, p = 0.0165, Figure 5C; joint: r = −0.612, p = 0.0152, Figure 5D) had significant decreases. Spine operation patient counts (r = −0.261, p = 0.3482, Figure 5E) showed no relationship; however, joint operation patient counts (r = −0.823, p = 0.0002, Figure 5F) showed a negative relationship. Physiotherapy patient counts showed an insignificant relationship (r = 0.007, p = 0.9808, Figure 5G).
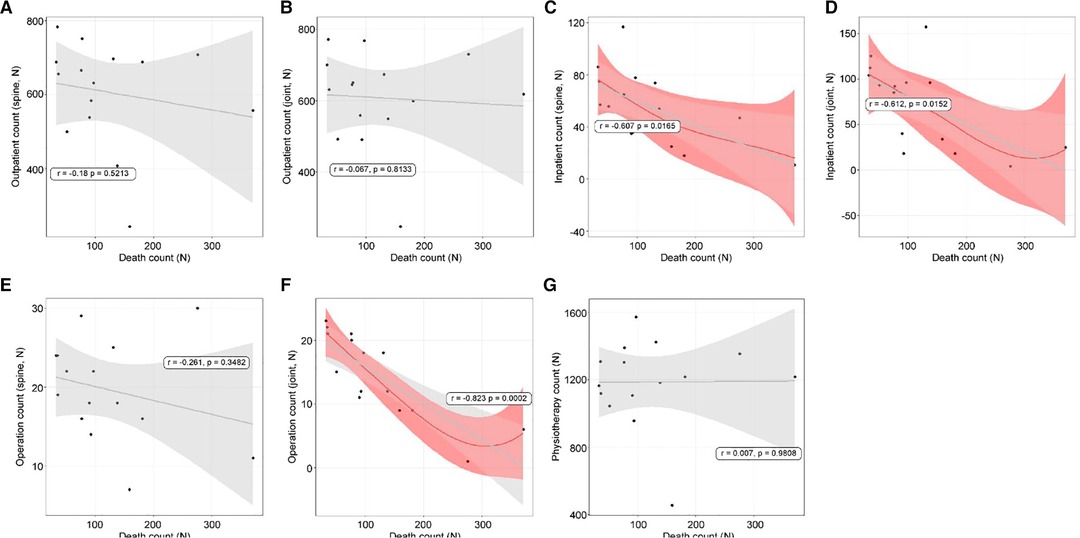
Figure 5. The linear relationships between death counts and orthopedic hospital visiting patterns. (A) Spine outpatient count; (B) Joint outpatient count; (C) Spine inpatient count; (D) Joint inpatient count; (E) Spine operation patient count; (F) Joint operation patient count; (G) Physiotherapy patient count.
Linear Relationships Between Vaccination Rate and Use of Orthopedic Treatments
The linear relationships between the vaccination rate and use of orthopedic treatments are summarized in Table 4. Outpatient treatments (spine: r = −0.456, p = 0.3039, Figure 6A; joint: r = −0.249, p = 0.5899, Figure 6B) had insignificant decreases. Inpatient spine treatments showed a linear increase (r = 0.812, p = 0.264, Figure 6C). Inpatient joint treatments increased, but this was not significant (r = 0.715, p = 0.0707, Figure 6D). The number of operations conducted in the spine department (r = 0.227, p = 0.6238, Figure 6E) and joint department (r = 0.639, p = 0.1225, Figure 6F) did not show any relationships. Physiotherapy patient counts showed an insignificant relationship (r = 0.031, p = 0.9476, Figure 6G).
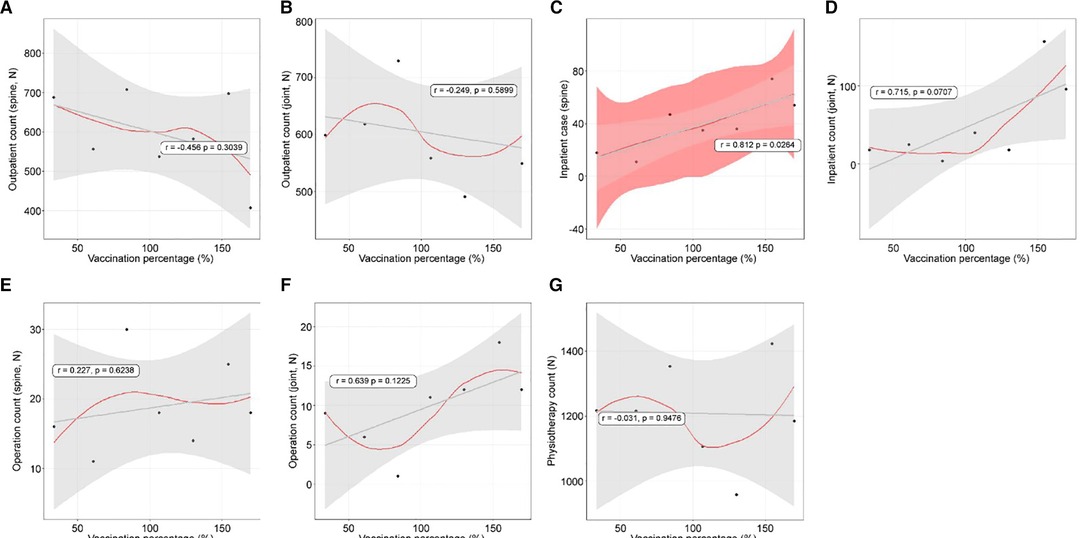
Figure 6. The linear relationships between vaccination rate and orthopedic hospital visiting patterns. (A) Spine outpatient count; (B) Joint outpatient count; (C) Spine inpatient count; (D) Joint inpatient count; (E) Spine operation patient count; (F) Joint operation patient count; (G) Physiotherapy patient count.
Discussion
This study demonstrated that our hypotheses that the COVID-19 pandemic would decrease the number of outpatients, inpatients, and operations and that these numbers would normalize with vaccination coverage were partially correct. Regarding the multifactor relationship, the number of joint operations decreased; however, upon evaluation of single-factor relationships, linear correlations were observed between COVID-19 diagnosis and both inpatient count and number of operations in the joint department. The recovered cases with inpatient treatment and death cases with both inpatient treatment and operations in the joint department showed a relationship. With the increasing vaccination rate, the number of spine operations increased, but that of joint operations did not.
Confirmed and recovered cases showed the same tendency; therefore, these factors can be evaluated together (5). Many factors influence hospital visits for outpatient treatment: “pandemic fever,” or the fear of visiting the hospital, was the main reason highlighted in a previous study (6). Government-imposed lockdowns may be another factor (7). Additionally, the popularity of telemedicine has considerably decreased outpatient treatments (8). Interestingly, the spine, joint, and physiotherapy departments showed no significant decrease in the number of outpatients in this study; this can be explained by the treatments delivered at the orthopedic clinic. Conditions in this field primarily include fractures, sprains, and herniated intervertebral discs that require direct intervention. For example, splint placement, all types of injection administrations, and physiotherapy require physical contact and specialized equipment. In addition, chronic pain management in elderly patients warrants regular visits and physiotherapy as needed. However, inpatient treatment showed a linear decrease in the number of confirmed and recovered COVID-19 cases owing to the lack of available beds. In the UAE, the peak of confirmed COVID-19 cases was during January and February 2021, and many beds were occupied by respiratory disease patients, mainly those with COVID-19. Bed unavailability is unavoidable; however, it should be considered that orthopedic patients requiring inpatient treatment may have to pay the price. Operation count can be affected during a pandemic due to a lack of blood for transfusions and bed unavailability (9). We found that joint operations decreased significantly compared to spine operations, likely because the timing of surgery is more crucial in spine operations (10). In addition, considering the urgency of the situation, spine surgery can be prioritized in a limited bed situation (11).
The number of PCR-confirmed COVID-19 active cases is controversial, and this may be a reason for the temporary increase in the number of confirmed cases (12). In the UAE, an increase in the number of confirmed cases was reported in January 2021, which gradually decreased within a year (13). The field of orthopedics also recovered early with the detection of asymptomatic infections. Although the number of PCR tests has increased and the diagnosis and death rates have decreased, orthopedic treatments remained unaffected. Reportedly, COVID-19 death rates can affect one’s psychological health (14, 15); this could be a reason for the decreased number of joint operations due to staying or admission to the hospital. Limited bed availability with increased numbers of COVID-19 inpatients could be another reason for this decrease. The bed availability rate decreased for other patients due to longer hospitalization periods (16) and difficulty in treatment (17) of patients with COVID-19. One study reported higher mortality and associated complications in COVID-19-positive patients following hip fracture treatment (18). It also reported that the same orthopedic treatment is more challenging in a COVID-19-positive patient than in a non-COVID-19 patient.
Owing to the pandemic, the utilization of hospital services has changed. Outpatient consultations at the departments of internal medicine and familial medicine decreased by 14% and those at the dental clinic by 7% in East Asian countries (19). Hospital visits decreased due to government-imposed movement restrictions depending on the country (20). Pediatric departments also reported a decreased inflow of patients, though only the overall decline has been confirmed owing to differences in hospital policies globally (21). In the UAE, there were no restrictions on visiting and practicing in hospitals during the pandemic, yet our inpatient treatment was affected, and the number of joint operations decreased. We also experienced a lack of inpatient beds due to the increasing number of patients in the internal medicine department. In addition, medical supplies from other departments were diverted to care for patients with COVID-19. We believe that these factors contributed to a decrease in inpatient treatment. We believe a decrease in joint operations compared to spine operations was observed due to the severity of spinal cord injuries and neurological emergencies. Despite the surgery being the same, hospital admission was decreased, and non-urgent surgery was delayed. The number of spine operations normalized earlier than that of joint operations following sufficient vaccination coverage for the same reasons.
The efficacy of COVID-19 vaccination remains controversial; other strains (delta and gamma) are decreasing the efficacy (22). However, vaccination imparts direct protection to elderly patients and patients with comorbidities (23). To achieve herd immunity, most of the population should be vaccinated (24). The vaccination rate can vary across regions and cultures (25). According to our results, with >160% vaccination coverage, patients who underwent spine operations have recovered despite the ongoing pandemic. Although this result is not overestimated, it cannot be the result of vaccination alone. Social distancing and mask use have already shown their benefits (26). All preventive measures have a role in the era of COVID-19 (27). The adoption of these practices could help in normalizing hospital treatments. Our outpatient treatments did not decrease during the pandemic; only inpatient treatments decreased due to other departments’ situations. The number of confirmed cases and deaths has drastically decreased following the strict implementation of face masks and vaccination. Nonetheless, psychological recovery is the main factor for the normalization of hospital visiting patterns. Based on our results, the joint department is more effective during the corona pandemic than the spine department, and the vaccination rate affects the normalization of clinic treatment. During a pandemic, prevention methods including wearing a mask, hand hygiene and social distancing, vaccination and prediction of patient pattern change should be observed.
This study has some limitations. Each vaccine has different efficacies; however, these were not evaluated. Our results would be more reliable if each vaccine’s efficacy were analyzed. Our results cannot be generalized to other medical fields. The orthopedic department deals mainly with outpatients and involves many interventions. Other areas with different therapeutic characteristics may have different results. Further studies are required to compare the results in each field. Even within the same clinic, various diagnoses and different treatments are required. The current study focused on general trend changes in orthopedic clinics; however, future studies will be valuable to evaluate each disease separately.
In conclusion, in the UAE, orthopedic treatment was influenced by the COVID-19 pandemic, including patient diagnosis, recovery, and death. With the increasing vaccination rate, the treatment pattern has seemed to normalize.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by UHS-HERC-077-15112021. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conceptualization, S.K.K; methodology, S. Park.; software, D.-W. C.; validation, H.S.K., H.Y. J and S.H.Y.; formal analysis, N.J. K.; investigation, E.J.H.; resources, J.Y.H.; data curation, G.E.K.; writing—original draft preparation, S.K.K.; writing—review and editing, S.-K.K.; visualization, S.-K.K.; supervision, S.-J.P.; project administration, S.K.K. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE 3rd, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. (2020) 180:1328–33. doi: 10.1001/jamainternmed.2020.3288
2. Wosik J, Clowse MEB, Overton R, Adagarla B, Economou-Zavlanos N, Cavalier J, et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am Heart J. (2021) 231:1–5. doi: 10.1016/j.ahj.2020.10.074
3. Quaquarini E, Saltalamacchia G, Presti D, Caldana G, Tibollo V, Malovini A, et al. Impact of COVID-19 outbreak on cancer patient care and treatment: data from an outpatient oncology clinic in Lombardy (Italy). Cancers (Basel). (2020) 12:2941. doi: 10.3390/cancers12102941
4. Balachandar V, Mahalaxmi I, Subramaniam M, Kaavya J, Senthil Kumar N, Laldinmawii G, et al. Follow-up studies in COVID-19 recovered patients - is it mandatory? Sci Total Environ. (2020) 729:139021. doi: 10.1016/j.scitotenv.2020.139021
5. Song XJ, Xiong DL, Wang ZY, Yang D, Zhou L, Li RC. Pain management during the COVID-19 pandemic in China: lessons learned. Pain Med. (2020) 21:1319–23. doi: 10.1093/pm/pnaa143
6. Dwivedi LK, Rai B, Shukla A, Dey T, Ram U, Shekhar C, et al. Assessing the impact of complete lockdown on COVID-19 Infections in India and its burden on public health facilities. Int Inst Popul Sci Mumbai. (2020) 49(Special Issue):37–50.
7. Fraissé M, Logre E, Pajot O, Mentec H, Plantefève G, Contou D. Thrombotic and hemorrhagic events in critically ill COVID-19 patients: a French monocenter retrospective study. Crit Care. (2020) 24:275. doi: 10.1186/s13054-020-03025-y
8. van Middendorp JJ, Hosman AJF, Doi SAR. The effects of the timing of spinal surgery after traumatic spinal cord injury: a systematic review and meta-analysis. J Neurotrauma. (2013) 30:1781–94. doi: 10.1089/neu.2013.2932
9. Bernstein M. Editorial. Neurosurgical priority setting during a pandemic: COVID-19. J Neurosurg. (2020) 133:1–2. doi: 10.3171/2020.4.JNS201031
10. Binnicker MJ. Challenges and controversies to testing for COVID-19. J Clin Microbiol. (2020) 58:e01695-20. doi: 10.1128/JCM.01695-20
11. Hellewell J, Russell TW, et al., SAFER Investigators and Field Study Team, Crick COVID-19 Consortium, CMMID COVID-19 working group, Estimating the effectiveness of routine asymptomatic PCR testing at different frequencies for the detection of SARS-CoV-2 infections. BMC Med. (2021) 19:1–10. doi: 10.1186/s12916-021-01982-x
12. Dawson DL, Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Contextual Behav Sci. (2020) 17:126–34. doi: 10.1016/j.jcbs.2020.07.010
13. McBride O, Murphy J, Shevlin M, Gibson-Miller J, Hartman TK, Hyland P, et al. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. Int J Methods Psychiatr Res. (2021) 30:e1861. doi: 10.1002/mpr.1861
14. Butt AA, Kartha AB, Masoodi NA, Azad AM, Asaad NA, Alhomsi MU, et al. Hospital admission rates, length of stay, and in-hospital mortality for common acute care conditions in COVID-19 vs. pre-COVID-19 era. Public Health. (2020) 189:6–11. doi: 10.1016/j.puhe.2020.09.010
15. Brill SE, Jarvis HC, Ozcan E, Burns TLP, Warraich RA, Amani LJ, et al. COVID-19: a retrospective cohort study with focus on the over-80s and hospital-onset disease. BMC Med. (2020) 18:194. doi: 10.1186/s12916-020-01665-z
16. Arafa M, Nesar S, Abu-Jabeh H, Jayme MOR, Kalairajah Y. COVID-19 pandemic and hip fractures: impact and lessons learned. Bone Jt Open. (2020) 1:530–40. doi: 10.1302/2633-1462.19.BJO-2020-0116.R1
17. Chang WH. The influences of the COVID-19 pandemic on medical service behaviors. Taiwan J Obstet Gynecol. (2020) 59:821–7. doi: 10.1016/j.tjog.2020.09.007
18. Pinggera D, Kerschbaumer J, Grassner L, Demetz M, Hartmann S, Thomé C. Effect of the COVID-19 pandemic on patient presentation and perception to a neurosurgical outpatient clinic. World Neurosurg. (2021) 149:e274–80. doi: 10.1016/j.wneu.2021.02.037
19. Virani AK, Puls HT, Mitsos R, Longstaff H, Goldman RD, Lantos JD. Benefits and risks of visitor restrictions for hospitalized children during the COVID pandemic. Pediatrics. (2020) 146:e2020000786. doi: 10.1542/peds.2020-000786
20. Cevik M, Grubaugh ND, Iwasaki A, Openshaw P. COVID-19 vaccines: keeping pace with SARS-CoV-2 variants. Cell. (2021) 184:5077–81. doi: 10.1016/j.cell.2021.09.010
21. Sultana J, Mazzaglia G, Luxi N, Cancellieri A, Capuano A, Ferrajolo C, et al. Potential effects of vaccinations on the prevention of COVID-19: rationale, clinical evidence, risks, and public health considerations. Expert Rev Vaccines. (2020) 19:919–36. doi: 10.1080/14760584.2020.1825951
22. Randolph HE, Barreiro LB. Herd immunity: understanding COVID-19. Immunity. (2020) 52:737–41. doi: 10.1016/j.immuni.2020.04.012
23. Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines (Basel). (2020) 8:582. doi: 10.3390/vaccines8040582
24. Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood). (2020) 39:1237–46. doi: 10.1377/hlthaff.2020.00608
25. Galanti M, Pei S, Yamana TK, Angulo FJ, Charos A, Swerdlow DL, et al. Social distancing remains key during vaccinations. Science. (2021) 371:473–4. doi: 10.1126/science.abg2326
26. Pradhan D, Biswasroy P, Kumar Naik PK, Ghosh G, Rath G. A review of current interventions for COVID-19 prevention. Arch Med Res. (2020) 51:363–74. doi: 10.1016/j.arcmed.2020.04.020
Keywords: COVID-19, coronavirus, pandemic, vaccination, orthopedics
Citation: Kim S, Park S, Cho D, Kwak H, Jin H, Eum S, Heo E, Kim G, Ji H and Park S (2022) Impact of the Coronavirus Disease Pandemic and Related Vaccination in an Orthopedic Clinic in the United Arab Emirates: An Observational Study. Front. Surg. 9:906797. doi: 10.3389/fsurg.2022.906797
Received: 29 March 2022; Accepted: 12 May 2022;
Published: 31 May 2022.
Edited by:
Philip Frank Stahel, Rocky Vista University, United StatesReviewed by:
Jung-Wee Park, Seoul National University Bundang Hospital, South KoreaYan Zhou, Renmin Hospital of Wuhan University, China
Copyright © 2022 Kim, Park, Cho, Kwak, Jin, Eum, Heo, Kim, ji and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seung-Kook Kim c2V1bmdrb29rLmtpbUB1aHMuYWU=
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Seung-Kook Kim
Seung-Kook Kim Seo-jung Park1,4,5
Seo-jung Park1,4,5