- 1Department of Vascular and Endovascular Surgery, First Affiliated Hospital of Zhengzhou University, China
- 2Key Vascular Physiology and Applied Research Laboratory of Zhengzhou City, China
Objectives: This study compared results of non-surgical treatment (compression and ultrasound guided thrombin injection (UGTI)) and surgery to treat iatrogenic femoral artery pseudoaneurysms.
Methods: PubMed and Embase databases were searched up to October 2021. Primary outcome measure was success rate, and other outcomes examined were complication rate, reintervention rate. Two authors independently reviewed and extracted data. Data were presented as the odds ratios (ORs) with 95% confidence intervals (CIs). The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to appraise the quality of the body of evidence.
Results: Eight studies were included. A total of 623 patients with pseudoaneurysm undergoing treatment were included, of which 163 subjects underwent surgery, 397 subjects underwent compression, and 63 subjects underwent UGTI. The success rate was significantly lower in the non-surgery group (OR 0.24, 95% CI, 0.08–0.69, I2 = 0%). The complication rate was significantly lower in the non-surgery group (OR 0.10, 95% CI, 0.03 –0.29, I2 = 0%). Patients in the non-surgery group tended to have a lower, but statistically insignificant, reintervention rate (OR 0.11, 95% CI, 0.01–1.06, I2 = 35%). Further, the GRADE assessment showed that these results (success rate, complication rate, and reintervention rate) were of very low quality.
Conclusions: Available evidence shows that it is reasonable to regard non-surgical treatment as the primary treatment for iatrogenic femoral artery pseudoaneurysms, and surgery as a remedy after failure of non-surgical treatment in some cases.
Introduction
Currently, in the diagnostic and therapeutic procedures of coronary and peripheral circulation, percutaneous arterial puncture is very common. With development of minimally invasive treatment technology, endovascular techniques have become the first line treatment option for many diseases (1, 2). The femoral artery is the most common site of access, so iatrogenic pseudoaneurysm is common in the femoral artery (3, 4). Pseudoaneurysm is formed when the puncture site is not fully sealed and leading to arterial rupture into the surrounding tissues (5, 6). It is associated with the characteristic manifestations of pulsatile masses, palpable tremors, and audible to-and-fro murmur (4). And it is one of the most common postoperative complications (7, 8), which is associated with the length of operation, the diameter of the catheter, antiplatelet agents, anticoagulation, older age, obesity, ineffective periprocedural compression, hypertension, peripheral arterial disease, hemodialysis and the puncture site (4, 8).
Surgical repair has been the traditional therapy (9). Non-surgical techniques were commonly used to treat pseudoaneurysm including compression and ultrasound-guided thrombin injections (UGTI). The main purpose of treatment is to prevent rupture and relieve the compression symptoms of veins, nerves, and skin (10, 11).
For asymptomatic patients with small pseudoaneurysms (<2 cm), be alert and wait for spontaneous closure is appropriate (8). For large (≥2 cm) and/ or symptomatic pseudoaneurysms, the risks of rupture and bleeding are higher if left untreated (10, 12). And it may cause other complications such as deep vein thrombosis(DVT), neuropathy, and skin necrosis (8, 10, 12). Although endovascular therapy (covered stents and coil embolization) and ultrasound-guided glue injection are currently used in the treatment of pseudoaneurysm, their efficacy and safety have only been demonstrated in a small population, and large studies are needed to confirm this (13, 14). Surgical treatment was the main treatment for iatrogenic femoral artery pseudoaneurysms. In the decade of the 1990s, the transition from surgical treatment to ultrasound-guided therapy initially using noninvasive compression was gradually completed. Recently, UGTI has been widely used as a new minimally invasive technique (15).
This systematic review and meta-analysis aimed to analyze the clinical outcomes of different techniques (surgery and non-surgery) for the treatment of iatrogenic femoral artery pseudoaneurysm and report outcomes including success rate, incidence of complication, and reintervention rate.
Method
This systematic review and meta-analysis was conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) Statement (16, 17) and designed according to the latest methodological guidance (18).
Eligibility Criteria
The current analysis included original research studies that reported outcomes of non-surgery (compression or UGTI) and surgery for treatment of iatrogenic femoral artery pseudoaneurysms. Studies considered for inclusion met the following criteria: Each study had to report on the outcomes of the treatment modalities; femoral artery pseudoaneurysms were objectively diagnosed. Change from one to the other technique, in case of failure, within each study was allowed and was not used as an exclusion criterion. Studies on traumatic pseudoaneurysms and reports examining only one technique were excluded, as were studies whose data was incomplete and case reports. Studies reporting other techniques of femoral artery pseudoaneurysms treatment like para-aneurysmal saline injection, endovascular coils, and ultrasound-guided glue injection, etc., also were discarded.
Search Strategy
Database search was updated last on October, 2021 in the PubMed and Embase. No restriction on language or publication period was required. Search terms included “femoral artery pseudoaneurysm”, “iatrogenic femoral artery pseudoaneurysm”, “ultrasound guided thrombin injection”, “UGTI”, “ultrasound guided compression”, “UGC”, “compression” and “surgery”. Moreover, we enriched our search by manually reviewing the reference lists of all retrieved articles for additional published or unpublished trials.
Study Selection
Three review authors screened the titles and abstracts of each search result for potentially relevant studies independently. Then the selected articles were read in full to review studies eligibility and quality. Disagreements were resolved by consensus if necessary. All studies were required to directly report the results of each procedure.
Data Extraction and Management
Two review authors independently extracted data from each included study using standard forms. Data for all relevant outcomes were extracted from retrieved studies. We collected the following data: number, sex and age of enrolled patients, types of studies, number of patients with pseudoaneurysm in each treatment, and type of intervention. The primary endpoint of the analysis was success rate of treatment modalities. Successful treatment was defined as thrombosis of the flow lumen. Surgical failure was defined as postoperative death of the patient. Secondary endpoints included complication rate, reintervention rate.
Assessment of Methodological Quality
The quality of each study was assessed based on well-established criteria (Newcastle-Ottawa scale) for non-randomised studies regarding selection (0–4 points), comparability (0–2 points) and identification of the exposure of study participants (0–3 points) independently. We evaluated quality base on it with discrepancies resolved by a third author. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to evaluate the quality of evidence (19). One of four grades of very low, low, moderate, and high represented the results of the GRADE approach.
Statistical Analysis and Data Synthesis
All analyses were conducted using Review Manager (RevMan, version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012). The Mantele-Haenszel method was used to combine summarized data from each report. According to the data collected, we generated odds ratios (ORs) and 95% confidence intervals (CIs) for success rate, complication rate and reintervention rate. The software produced forest plots, and provided inconsistency (I2) statistics to evaluate the heterogeneity of the included studies. For inconsistency variable a value of 0% indicates no heterogeneity, whereas increasing values suggest increasing heterogeneity. To exclude possible bias because of the quality of the included studies, a random effects model to make comparisons was preferred over a fixed effects model. Publication bias was assessed by generating funnel plots.
Result
Literature Search
The database search returned 533 results. And there were two additional articles that were identified through the manual search of references of primary articles. After screening the title and abstract, 439 studies were excluded. The excluded reports included case reports, review articles, and studies examining alternative methods to treat pseudoaneurysms (para-aneurysmal saline injection, endovascular coils, and ultrasound-guided glue injection), which were not the focus of this analysis. Then, by reading the full texts, 88 studies were excluded because they reported on single-arm treatment (compression or UGTI). Eight studies that finally met the inclusion criteria were selected. The flow chart of the selection procedure is shown in Figure 1.
Study Characteristics and Quality
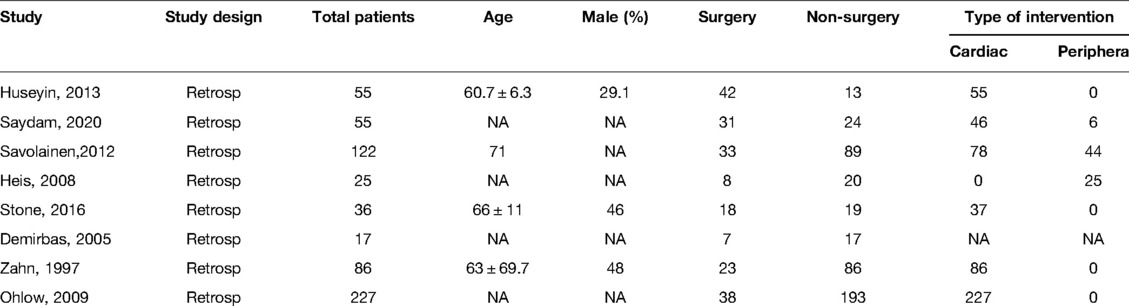
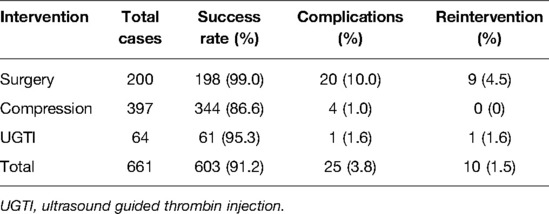
Eight retrospective studies were identified and included in this report (20–27). Tables 1, 2 showed the baseline characteristics of the patients included in our analysis. The number of patients ranged from 17 to 227. These studies were published between 1997 and 2020. A total of 623 patients with pseudoaneurysm undergoing treatment were included, of which 163 subjects underwent surgery, 397 subjects underwent compression (344 ultrasound guided compression, 39 compression bandage, 14 manual compression), and 63 subjects underwent UGTI. Moreover, 35 subjects in the former group switched to surgery after unsuccessful compression, 1 subject in the former group switched to surgery after unsuccessful UGTI, 1 subject in the former group switched to surgery after unsuccessful observation, for a total of 163 + 35 + 1 + 1 = 200 subjects undergoing surgery. In addition, one subject in the former group switched to UGTI after unsuccessful compression, for a total of 63 + 1 = 64 subjects undergoing UGTI. It can be seen that most pseudoaneurysms occurred after femoral cannulation for cardiac procedures.
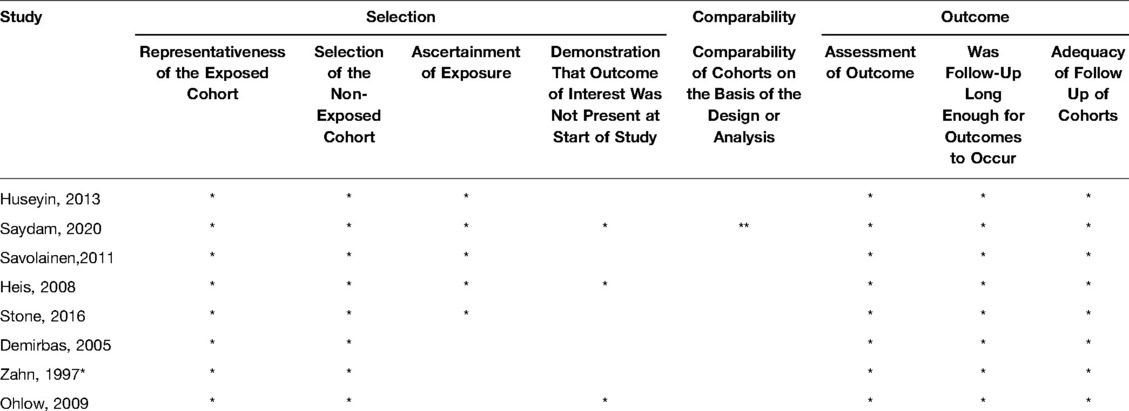
The median Newcastle-Ottawa scale score was 7 stars (range 5–9). In general, low quality articles had increased risk in their data analysis and confounding (Table 3).
Data Synthesis
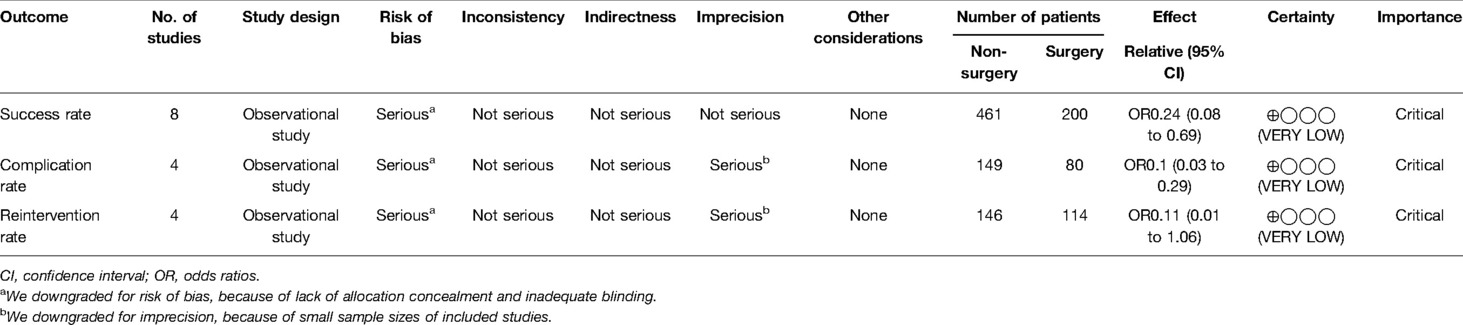
Data regarding efficacy of strategies to treat iatrogenic femoral artery pseudoaneurysms could be extracted from all 8 included studies. In total 200 patients underwent surgery and 461 non-surgical treatments (Table 4). The success rate was significantly lower in the non-surgery group (OR 0.24, 95% CI, 0.08–0.69, I2 = 0%) (Figure 2). With respect to safety, there were low complication rates for both groups. Data was available for 200 patients undergoing surgery, and corresponding complication rates were 10.0% (20/200). There were 461 patients in the non-surgical group, with a total complication rate of 1.1% (5/461), of which the complication rate in the compression group was 1.0% (4/397) and the complication rate in the UGTI group was 1.6% (1/64). Among patients in the surgery group, there were six cases of surgical site infection, six cases require wound drainage (cause unknown), three cases of major hemorrhage, two cases of maceratin, one case of DVT, one case of sepsis, and one case of arteriovenous fistula. Among patients in the compression group there was one case of DVT, one case of arterial occlusion, one case of local infection, and one case of major hemorrhage. Among patients in the UGTI group there was one case of thrombin emboli. The complication rate was significantly lower in the non-surgery group (OR 0.10, 95% CI, 0.03–0.29, I2 = 0%) (Figure 3). Patients in the non-surgery group tended to have a lower, but statistically insignificant, reintervention rate (OR 0.11, 95% CI, 0.01–1.06, I2 = 35%) (Figure 4). Four of the patients who underwent reintervention after surgery had hematomas and five had wound infections. Subgroup analysis result showed that the failure rate of compression and UGTI group was not significantly different (OR 0.60, 95% CI, 0.12–2.97, I2 = 0%) (Figure 5).
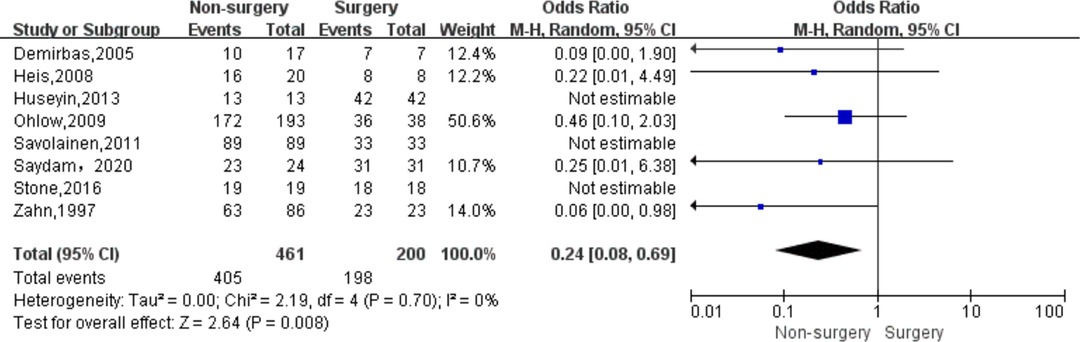
Figure 2. Forest plot showing the pooled odds ratio for pseudoaneurysm treatment success rate after surgery and non-surgical treatment.
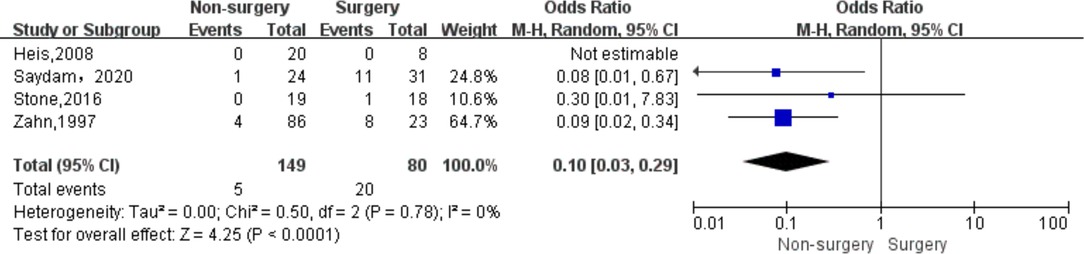
Figure 3. Forest plot showing the pooled odds ratio for pseudoaneurysm treatment complication rate after surgery and non-surgical treatment. CI, confidence interval; IV, inverse variance.
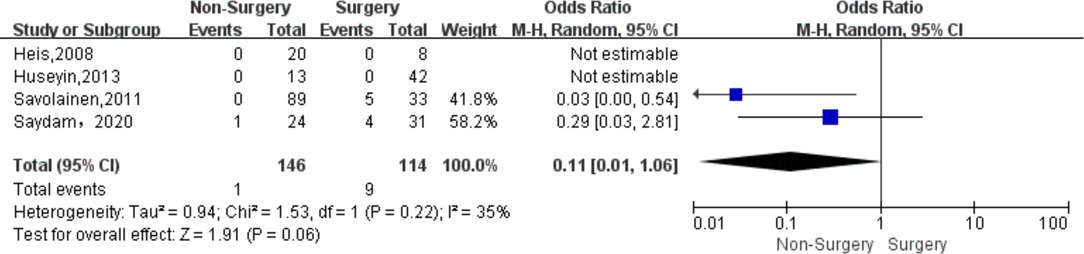
Figure 4. Forest plot showing the pooled odds ratio for pseudoaneurysm treatment reintervention rate after surgery and non-surgical treatment. CI, confidence interval; IV, inverse variance.
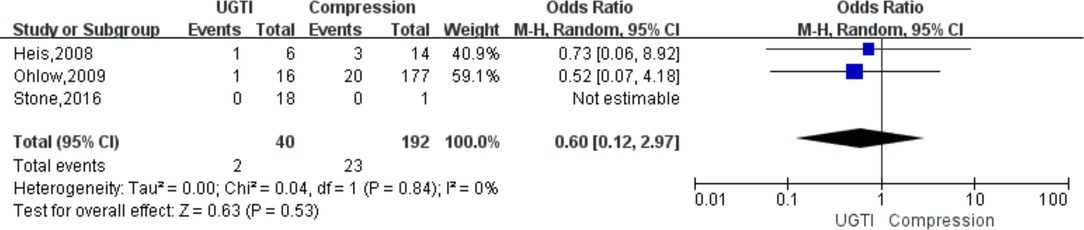
Figure 5. Forest plot showing the pooled odds ratio for failure rate of subgroup analysis about compression and UGTI group.
GRADE of Evidence
Based on the results of the GRADE approach, the quality of evidence of outcome measures (success rate, complication rate, and reintervention rate) were rated as very low (Table 5). The large risk of bias was caused by lack of allocation concealment and inadequate blinding. The reason for downgrading for imprecision was the small sample sizes of included studies.
Sensitivity Analysis
Sensitivity analysis was performed to explore the effect of individual studies. The result of success rate produced marked change (OR 0.30, 95% CI, 0.10–0.95, I2 = 0%) by excluding the study by Zahn. When analyzing complication rate, sensitivity analysis, results showed no significant change after exclusion of each study.
Discussion
In this study, we have found significantly higher in the success rate in surgical treatment for iatrogenic femoral artery pseudoaneurysm, but complication rate was significantly higher in the surgery group.
Until the 1990s, surgery was the gold standard treatment for treating iatrogenic femoral artery pseudoaneurysms. Then, UGC (ultrasound guided compression) and UGTI were used to treat pseudoaneurysms (28, 29). Gradually, endovascular treatment (covered stents and coil embolization), para-aneurysmal saline injection, and ultrasound-guided glue injection appeared (13, 30–32). However, each procedure has advantages and disadvantages. In our study, we compared non-surgical and surgical treatments. In the non-surgical treatment group, we only included patients who received compression and UGTI, because no studies comparing other non-surgical treatments with surgical treatment were found.
In our study, the success rate of UGTI was 95.3% and the success rate of compression was 86.6%. And subgroup analysis result showed no significant difference in failure rate. In a meta-analysis comparing UGC and UGTI in 992 patients, it suggested the success rate of UGTI was 97.4% and the success rate of UGC was 69.3% (33). The result about UGTI is similar to our finding. However, there is a major difference in the results of compression. There may be several reasons. In our study, the compression group included patients undergoing manual compression, compression bandage and UGC, while only patients who received UGC were included in the above meta-analysis. The use of anticoagulant and antiplatelet drugs, age, features of pseudoaneurysm and body mass index (BMI) of the enrolled patients were different, and these factors may have a certain impact on the success rate (4, 8). Then, the relatively higher success rate of our study may because of the relatively few patients. Finally, we defined therapeutic success as the final thrombosis of the pseudoaneurysm regardless of whether the compression or UGTI succeed at first time. In some studies, patients had to undergo two or even three attempts of compression before they succeeded (21).
The result we got was that the success rate of non-surgery was significantly lower than that of surgical treatment. It should be noted that a total of 37 patients received surgical treatment after the failure of conservative treatment, including one case of UGTI, one case of observation and 35 cases of compression. There was one surgical failure in these patients. In total, two patients in the surgery group were judged failures due to death, one case was in hemorrhagic shock due to acute rupture of a pseudoaneurysm, and one case was due to multiorgan dysfunction syndrome. The sensitivity analysis about success rate showed marked change by excluding the study by Zahn, which might be related to the fact that it was an earlier study and only it included patients treated by different compression methods (compression bandage and UGC) (27).
For the comparison of two non-surgical treatment methods, a meta-analysis involving 996 patients pointed out that UGTI is better than UGC (33). This study pointed out that UGTI resulted in a higher success rate in the treatment of pseudoaneurysms, and might be associated with lower complication rate and treatment cost.
There were many complications of surgery and compression, while in the UGTI group, according to our results, only one complication was thrombin emboli (25). At present, one study has shown that thrombin emboli risk may be negatively correlated with sac area and neck length, and negatively correlated with neck width (34). However, another study suggested that pseudoaneurysm neck dimensions was not associated with treatment efficacy (35). Skin infection is another potential complication of UGTI identified by Weinmann et al. (36) The fatal complication of UGTI is an anaphylactic reaction to thrombin, which is related to the use of bovine thrombin and repeated exposure to thrombin (37).
Currently, UGTI is often the first-line treatment for iatrogenic post-catheterization pseudoaneurysms. But there are also treatments that use various glues instead of thrombin, such as N-butyl cyanoacrylate (NBCA) (38), N-butyl cyanoacrylate-methacryloxy sulfolane (NBCA-MS) (39), fibrin glue (40), and tissue glue (TG) (41). The use of these glues has been proven to be safe and effective, and they have the potential to become an alternative to thrombin (14).
This meta-analysis also has some limitations. Firstly, the quality of the studies we included was not high, which contributed to the very low quality of our evidence. Second, the final results were combined using a random-effects model, and the weight of each article was proportional to the number of cases reported, so the source of variation should be considered within the study. There may also be some deviations in some cases, because the circumstances of each study are different, the basic characteristics of the patients and the characteristics of pseudoaneurysms are different. In addition, the current study was not registered, so there might be a small bias, but we still strictly follow the steps of systematic review. Last, in the current protocol, crossover from compression or UGTI to surgery is allowed, which may have some impact on the outcome.
Conclusion
The success rate of surgery of iatrogenic femoral artery pseudoaneurysm is higher than that of non-surgical treatment, but the complication risk is higher, and the reintervention rate also tends to be higher. Therefore, it is reasonable to regard non-surgical treatment for pseudoaneurysm as main treatment if the situation is not critical, and surgical treatment as a remedy after failure. Moreover, the quality of the success rate, complication rate, and reintervention rate assessments was very low. Further research is required because of the low overall quality of the included studies.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
HW, LZ designed experiments, performed data analysis, wrote, and revised the manuscript; CZ, BX, CL, YL compiled data; HB obtained funding. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Natural Science Foundation of China to Hualong Bai (Grant No: 81870369), Health Science and Technology Innovation Fund for Distinguished Young Scholars of Henan Province, (YXKC2021040), and Key projects of medical science and technology in Henan Province to Hualong Bai (Grant NO: SBGJ202002035).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics–2006 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. (2006) 113(6):e85–e151. doi: 10.1161/circulationaha.105.171600
2. Sachs T, Schermerhorn M, Pomposelli F, Cotterill P, O'Malley J, Landon B. Resident and fellow experiences after the introduction of endovascular aneurysm repair for abdominal aortic aneurysm. J Vasc Surg. (2011) 54(3):881–8. doi: 10.1016/j.jvs.2011.03.008
3. DeRubertis BG, Faries PL, McKinsey JF, Chaer RA, Pierce M, Karwowski J, et al. Shifting paradigms in the treatment of lower extremity vascular disease: a report of 1000 percutaneous interventions. Ann Surg. (2007) 246(3):415–22; discussion 22–4. doi: 10.1097/SLA.0b013e31814699a2
4. Kronzon I. Diagnosis and treatment of iatrogenic femoral artery pseudoaneurysm: a review. J Am Soc Echocardiogr. (1997) 10(3):236–45. doi: 10.1016/s0894-7317(97)70061-0
5. Kresowik TF, Khoury MD, Miller BV, Winniford MD, Shamma AR, Sharp WJ, et al. A prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplasty. J Vasc Surg. (1991) 13(2):328–33; discussion 33–5. PMID: 1990173
6. Houlind K, Jepsen JM, Saicu C, Vammen S, Christensen JK, Ravn H. Current management of inguinal false aneurysms. J Cardiovasc Surg. (2017) 58(2):278–83. doi: 10.23736/s0021-9509.16.09836-0
7. Hessel SJ, Adams DF, Abrams HL. Complications of angiography. Radiology. (1981) 138(2):273–81. doi: 10.1148/radiology.138.2.7455105
8. Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation. (2007) 115(20):2666–74. doi: 10.1161/circulationaha.106.681973
9. Franco CD, Goldsmith J, Veith FJ, Calligaro KD, Gupta SK, Wengerter KR. Management of arterial injuries produced by percutaneous femoral procedures. Surgery. (1993) 113(4):419–25. PMID: 8456398
10. Toursarkissian B, Allen BT, Petrinec D, Thompson RW, Rubin BG, Reilly JM, et al. Spontaneous closure of selected iatrogenic pseudoaneurysms and arteriovenous fistulae. J Vasc Surg. (1997) 25(5):803–8; discussion 8–9. doi: 10.1016/s0741-5214(97)70209-x
11. Graham AN, Wilson CM, Hood JM, Barros D’Sa AA. Risk of rupture of postangiographic femoral false aneurysm. Br J Surg. (1992) 79(10):1022–5. doi: 10.1002/bjs.1800791012
12. Kent KC, McArdle CR, Kennedy B, Baim DS, Anninos E, Skillman JJ. A prospective study of the clinical outcome of femoral pseudoaneurysms and arteriovenous fistulas induced by arterial puncture. J Vasc Surg. (1993) 17(1):125–31; discussion 31–3. doi: 10.1067/mva.1993.41707
13. Kobeiter H, Lapeyre M, Becquemin JP, Mathieu D, Melliere D, Desgranges P. Percutaneous coil embolization of postcatheterization arterial femoral pseudoaneurysms. J Vasc Surg. (2002) 36(1):127–31. doi: 10.1067/mva.2002.124372
14. Kurzawski J, Janion-Sadowska A, Sadowski M. A novel minimally invasive method of successful tissue glue injection in patients with iatrogenic pseudoaneurysm. Br J Radiol. (2018) 91(1087):20170538. doi: 10.1259/bjr.20170538
15. Pezzullo JA, Cronan JJ. Postcatheterization pseudoaneurysms: new developments in the diagnosis and treatment with ultrasound. Ultrasound Q. (2001) 17(4):227–34. doi: 10.1097/00013644-200112000-00004
16. Antoniou GA, Antoniou SA, Mani K. Enhancing the reporting of systematic reviews and meta-analyses in vascular surgery: PRISMA 2020. Eur J Vasc Endovasc Surg. (2021) 62(4):664–6. doi: 10.1016/j.ejvs.2021.06.010
17. Page MA-O, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10(1):89. doi: 10.1186/s13643-021-01626-4
18. Riley RD, Hayden JA, Steyerberg EW, Moons KG, Abrams K, Kyzas PA, et al. Prognosis research strategy (progress) 2: prognostic factor research. PLoS Med. (2013) 10(2):e1001380. doi: 10.1371/journal.pmed.1001380
19. Antoniou SA, Antoniou GA. The GRADE approach to appraising the evidence or how to increase the credibility of your research. Am J Surg. (2020) 220(2):290–3. doi: 10.1016/j.amjsurg.2020.01.021
20. Demirbas O, Batyraliev T, Eksi Z, Pershukov I. Femoral pseudoaneurysm due to diagnostic or interventional angiographic procedures. Angiology. (2005) 56(5):553–6. doi: 10.1177/000331970505600505
21. Heis HA, Bani-Hani KE, Elheis MA, Yaghan RJ, Bani-Hani BK. Postcatheterization femoral artery pseudoaneurysms: therapeutic options. a case-controlled study. Int J Surg. (2008) 6(3):214–9. doi: 10.1016/j.ijsu.2008.03.006
22. Huseyin S, Yuksel V, Sivri N, Gur O, Gurkan S, Canbaz S, et al. Surgical management of iatrogenic femoral artery pseudoaneurysms: a 10-year experience. Hippokratia. (2013) 17(4):332–6. PMID: 25031512
23. Ohlow MA, Secknus MA, von Korn H, Neumeister A, Wagner A, Yu J, et al. Incidence and outcome of femoral vascular complications among 18,165 patients undergoing cardiac catheterisation. Int J Cardiol. (2009) 135(1):66–71. doi: 10.1016/j.ijcard.2008.03.035
24. Savolainen H, Baumgartner I, Schmidli J, Heller G, Do DD, Willenberg T. Femoral pseudoaneurysms requiring surgical treatment. Trauma Monthly. (2012) 16(4):194–7. doi: 10.5812/kowsar.22517464.3186
25. Saydam O, Serefli D, Engin AY, Atay M. Ultrasound-guided thrombin injection for treatment of iatrogenic femoral artery pseudoaneurysms compared with open surgery: first experiences from a single institution. Ann Surg Treat Res. (2020) 98(5):270–6. doi: 10.4174/astr.2020.98.5.270
26. Stone PA, Thompson SN, Hanson B, Masinter D. Management of iatrogenic pseudoaneurysms in patients undergoing coronary artery bypass grafting. J Vasc Endovasc Surg. (2016) 50(4):217–20. doi: 10.1177/1538574416637448
27. Zahn R, Thoma S, Fromm E, Lotter R, Zander M, Seidl K, et al. Pseudoaneurysm after cardiac catheterization: therapeutic interventions and their sequelae: experience in 86 patients. Cathet Cardiovasc Diagn. (1997) 40(1):9–15. doi: 10.1002/(sici)1097-0304(199701)40:1 < 9::aid-ccd3 > 3.0.co;2-g
28. Fellmeth BD, Roberts AC, Bookstein JJ, Freischlag JA, Forsythe JR, Buckner NK, et al. Postangiographic femoral artery injuries: nonsurgical repair with us-guided compression. Radiology. (1991) 178(3):671–5. doi: 10.1148/radiology.178.3.1994400
29. Cope C, Zeit R. Coagulation of aneurysms by direct percutaneous thrombin injection. AJR Am J Roentgenol. (1986) 147(2):383–7. doi: 10.2214/ajr.147.2.383
30. Thalhammer C, Kirchherr AS, Uhlich F, Waigand J, Gross CM. Postcatheterization pseudoaneurysms and arteriovenous fistulas: repair with percutaneous implantation of endovascular covered stents. Radiology. (2000) 214(1):127–31. doi: 10.1148/radiology.214.1.r00ja04127
31. Gehling G, Ludwig J, Schmidt A, Daniel WG, Werner D. Percutaneous occlusion of femoral artery pseudoaneurysm by para-aneurysmal saline injection. Catheter Cardiovasc Interv. (2003) 58(4):500–4. doi: 10.1002/ccd.10485
32. Loose HW, Haslam PJ. The management of peripheral arterial aneurysms using percutaneous injection of fibrin adhesive. Br J Radiol. (1998) 71(852):1255–9. doi: 10.1259/bjr.71.852.10318997
33. Kontopodis N, Tsetis D, Tavlas E, Dedes A, Ioannou CV. Ultrasound guided compression versus ultrasound guided thrombin injection for the treatment of post-catheterization femoral pseudoaneurysms: systematic review and meta-analysis of comparative studies. Eur J Vasc Endovasc Surg. (2016) 51(6):815–23. doi: 10.1016/j.ejvs.2016.02.012
34. Hashemi Fard O. Iatrogenic femoral artery pseudoaneurysm (review of treatment options). ARYA Atheroscler. (2010) 6(2):74–7. PMID: 22577418
35. Yang EY, Tabbara MM, Sanchez PG, Abi-Chaker AM, Patel J, Bornak A, et al. Comparison of ultrasound-guided thrombin injection of iatrogenic pseudoaneurysms based on neck dimension. Ann Vasc Surg. (2018) 47:121–7. doi: 10.1016/j.avsg.2017.07.029
36. Weinmann EE, Chayen D, Kobzantzev ZV, Zaretsky M, Bass A. Treatment of postcatheterisation false aneurysms: ultrasound-guided compression vs ultrasound-guided thrombin injection. Eur J Vasc Endovasc Surg. (2002) 23(1):68–72. doi: 10.1053/ejvs.2001.1530
37. Jalaeian H, Misselt A. Anaphylactic reaction to bovine thrombin in ultrasound-guided treatment of femoral pseudoaneurysm. J Vasc Interv Radiol. (2015) 26(6):915–6. doi: 10.1016/j.jvir.2015.02.020
38. Aytekin C, Firat A, Yildirim E, Kirbas I, Boyvat F. Ultrasound-guided glue injection as alternative treatment of femoral pseudoaneurysms. Cardiovasc Intervent Radiol. (2004) 27(6):612–5. doi: 10.1007/s00270-004-0197-z
39. Griviau L, Chevallier O, Marcelin C, Nakai M, Pescatori L, Galland C, et al. Percutaneous ultrasound-guided balloon-assisted embolization of iatrogenic femoral artery pseudoaneurysms with glubran(®)2 cyanoacrylate glue: safety, efficacy and outcomes. Quant Imaging Med Surg. (2018) 8(8):796–803. doi: 10.21037/qims.2018.09.12
40. Gummerer M, Kummann M, Gratl A, Haller D, Frech A, Klocker J, et al. Ultrasound-guided fibrin glue injection for treatment of iatrogenic femoral pseudoaneurysms. Vasc Endovasc Surg. (2020) 54(6):497–503. doi: 10.1177/1538574420934631
Keywords: surgery, ultrasound guided thrombin injection, ultrasound guided compression, iatrogenic femoral artery pseudoaneurysm, UGTI
Citation: Wu H, Zhang L, Zhang C, Xie B, Lou C, Liu Y and Bai H (2022) Non-Surgical treatment Versus Surgery for Iatrogenic Femoral Artery Pseudoaneurysms: Systematic Review and Meta-Analysis. Front. Surg. 9:905701. doi: 10.3389/fsurg.2022.905701
Received: 27 March 2022; Accepted: 19 May 2022;
Published: 8 June 2022.
Edited by:
Konstantinos A. Filis National and Kapodistrian University of Athens, GreeceReviewed by:
Andreas M. Lazaris, National and Kapodistrian University of Athens, AthensNikolaos Kontopodis, University Hospital of Heraklion, Greece
Copyright © 2022 Wu, Zhang, Zhang, Xie, Lou, Liu and Bai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hualong Bai YmFpaHVhbG9uZ2RvY3RvckAxMjYuY29t; ZmNjYmFpaGxAenp1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Specialty section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
 Haoliang Wu
Haoliang Wu Liwei Zhang
Liwei Zhang Cong Zhang1
Cong Zhang1 Boao Xie
Boao Xie Yuanfeng Liu
Yuanfeng Liu Hualong Bai
Hualong Bai