
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 19 May 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.905413
This article is part of the Research Topic Co-use of medicines in surgery View all 114 articles
 Qinghong Luo1
Qinghong Luo1 Shuquan Zheng2*
Shuquan Zheng2*
Objective: To observe the effects of high-quality whole-course care on the psychological status and postoperative pharyngeal complications in patients undergoing surgery for secondary hyperparathyroidism (SHPT) to chronic rrenal failure (CRF).
Methods: The clinical data of 62 patients who underwent surgical treatment for CRF-SHPT from April 2018 to October 2021 in our department were retrospectively analyzed. According to the different nursing methods after admission, they were divided into two groups, of which 33 patients who received high-quality whole-course care were the high-quality group, and 29 patients who received routine nursing were the regular group. Compliance, occurrence of pharyngeal complications, improvement of preoperative and postoperative psychological status [Assessed by self-rating anxiety scale (SAS) and self-rating depression scale (SDS)], nursing satisfaction scores, and serum hormone levels [intact parathyroid hormone (iPTH), calcium (Ca), Phosphorus (P)] were compared between the two groups.
Results: The differences between the general conditions and clinical characteristics of the two groups were not significant (p > 0.05). After care, the number of cases with good compliance in the high-quality group was higher than that in the regular group, and the number of cases with non-compliance was lower than that in the regular group (p < 0.05); the difference in the number of cases with partial compliance after care between the two groups was not significant (p > 0.05). There was no significant difference in the incidence of pharyngeal complications such as sore throat, nausea and vomiting, dry throat and hoarseness between the two groups (p > 0.05); however, the 24-h postoperative sore throat and dry throat scores in the high-quality group were significantly lower than those in the regular group (p < 0.05). Patients in the high-quality group had higher nursing attitude, nursing skills, nursing safety, nursing quality, and overall nursing satisfaction scores than the regular group (p < 0.05). Compared with the pre-care period, SAS and SDS scores decreased in both groups after care, and SAS and SDS scores decreased more in the high-quality group than in the regular group (p < 0.05). Serum iPTH, Ca, and P levels decreased in both groups at 1 week after surgery, and iPTH, Ca, and P levels decreased more in the high-quality group than in the regular group (p < 0.05).
Conclusion: Through the high-quality whole-course care, full informed participation and active cooperation of CRF-SHPT patients, close medical and nursing collaboration, attention to detail and overall level of treatment can effectively improve patient compliance, psychological status and postoperative serum indicators, promote patient recovery and improve nursing satisfaction.
Secondary hyperparathyroidism (SHPT) is a series of symptoms caused by excessive production and secretion of parathyroid hormone by the parathyroid glands due to chronic renal insufficiency, renal tubular acidosis, vitamin D deficiency, Fanconi syndrome, digestive system reactions, pregnancy and lactation (1, 2). Among the various factors that trigger this disease, SHPT due to chronic renal failure (CRF) is the most common and is an important factor affecting the quality of survival of patients with CRF (3). Medical drug therapy and hemodialysis are currently the main treatment methods for CRF-SHPT patients, but about 50% of them still cannot relieve the clinical symptoms of SHPT after medical drugs or hemodialysis, and can gradually progress to refractory or progressive disease, at which point the patient will require surgical treatment (4, 5). However, these patients undoubtedly increase the risk of surgery due to long-term hemodialysis and combined multisystemic pathologies, such as impaired coagulation mechanisms, hypoproteinemia, and renal anemia (6). In addition, the operation itself is a stressful event for the patient, which often brings greater psychological pressure to the patient. and the patient is prone to negative emotions such as anxiety and depression, which in turn have a negative impact on the patient’s postoperative regression (7), so it is necessary to strengthen all aspects of patient care after admission. High-quality whole-course care (8, 9) is a nursing service for the entire surgical treatment process, implemented according to the characteristics of preoperative, intraoperative and postoperative work, so that the patient is in an optimal state at the physical, psychological and spiritual levels.
Due to the complexity of CRF-SHPT patients, numerous perioperative complications and difficult management, the authors have conducted a study on the effect of High-quality care of CRF-SHPT patients throughout the whole process since 2018, and achieved better results in the perioperative management of CRF-SHPT patients.
The clinical data of 62 patients who underwent surgical treatment for CRF-SHPT in our department from April 2018 to October 2021 were retrospectively analyzed. Patients were admitted to the hospital and were treated surgically, according to the different nursing methods after admission, they were divided into two groups, of which 33 patients who received high-quality whole-course care were the high-quality group, and 29 patients who received routine nursing were the regular group.
General clinical data including gender, age, weight, age on dialysis, and other general demographic information were collected from the subjects. All subjects were tested for serum calcium, phosphorus, and whole segment parathyroid hormone (iPTH) before surgery and 1 week after surgery.
① Patients with indications for surgery (10), such as (i) joint and bone pain and/or skeletal deformities, significant symptoms of muscle weakness, myalgia and skin pruritus; (ii) persistent blood iPTH > 800 ng/L with hypercalcemia or hyperphosphatemia; (iii) Color Doppler ultrasound showed at least 1 or more enlarged parathyroid glands >1 cm in diameter with abundant blood flow; (iv) Failure of internal medicine treatment.
② No severe skeletal deformity and osteoporosis, severe coagulation dysfunction, or combined with serious systemic diseases such as heart, lung, and brain dysfunction.
③ ASA classification of grade I to III.
④ Aged 20–65 years.
① Patients with recent history of upper respiratory tract infection, cough, or throat discomfort.
② Previous history of pharyngeal surgery.
③ Primary parathyroid disease.
④ Psychiatric disorders, etc., and the presence of physical disabilities.
⑤ The patient or the patient’s family gave informed consent to this treatment plan.
Preoperatively, the nursing staff closely observed the patient’s blood pressure, heart rate, pulse and other vital signs.
Nursing staff should actively cooperate with the physician, closely observe the patient’s temperature, pulse and other relevant changes, and promptly notify the physician for treatment if any situation arises. In terms of diet, the patient should be advised to pay attention to diet and daily living habits, and take medication regularly.
The patient was placed in a flat position and nursing staff closely monitored the patient’s skin and pulse; if abnormalities occurred, they were recorded and the physician was notified in a timely manner; when anti-infective drugs were administered, the patient’s condition was closely monitored and the physician was notified in a timely manner if abnormalities occurred.
The members of the quality treatment responsibility group all received detailed training on quality treatment and knowledge related to CRF-SHPT surgery, and developed scientific and reasonable quality treatment measures.
The treatment problems were determined with regard to the etiology and surgical characteristics of CRF-SHPT, the causes of major perioperative complications, prevention and treatment points, and the specific conditions of patients.
① Psychological counseling was carried out: As patients suffered from long-term disease as well as lifelong dialysis and expensive medical costs, they were generally in a state of tension and depression before surgery; coupled with a lack of confidence in the upcoming surgery and fear of surgical risks and prognosis, they were more prone to varying degrees of fear and anxiety, so psychological counselling should be carried out. ② Hypercalcemia management: Monitored the patient’s serum Ca, P level, when the patient has nausea and vomiting symptoms, should be alert to the occurrence of critical signs. When the patient’s blood Ca was greater than 3.2 mmol/L, he (she) should be promptly given a low-calcium diet and drink more water, drinking >1,500 mL/d. Daily intake and output were recorded to maintain the balance of output, and blood potassium was monitored to prevent hypokalemia due to massive urination; when the patient’s blood calcium was >3.75 mmol/L, the patient should be resuscitated as hypercalcemic, regardless of the manifestation of hypercalcemic crisis. ③ Preoperative preparation: the last preoperative dialysis was performed with heparin-free or low-molecular heparin dialysis to reduce intraoperative and postoperative bleeding. Trained patients to adapt to shoulder elevation and neck hyperextension position to ensure smooth operation, and patients were instructed to pay attention to safety when moving around, not to fall, prevent falling from bed and avoid fracture.
Helped the anesthesiologist to do a good job of anesthesia, and when the anesthesia was successful, we had to position the patient to a safe and comfortable angle, and take 2 mL venous blood specimens for the patient before, 5 minutes and 10 minutes after surgery, and send them to the laboratory for PTH testing. The changes in the patient’s blood oxygen saturation, pulse, blood pressure, heart rate and other indicators were closely observed during the operation. The infusion rate should be strictly controlled, and once the patient is found to have hand and foot convulsion symptoms, 10–20 mL of calcium gluconate (concentration of 10%) should be slowly pushed intravenously in a timely manner.
① Strict observation of vital signs: For postoperative patients, vital signs should be strictly observed, especially if there was a tendency of bleeding during dialysis or hypertension with heart failure, notify the doctor immediately and gave symptomatic treatment. Kept a tracheotomy kit at the patient’s bedside for 24 h after surgery, and resuscitated the patient in time if he/she was found to have respiratory distress or tendency to suffocate. ② Control of infection: Due to the large amount of toxins that accumulate in the body of CRF-SHPT patients and cannot be eliminated on their own, the water-electrolyte disorders in the body were highly susceptible to infectious diseases such as skin mucosal infections and stomatitis. Some studies concluded that active oral care and skin care were the keys to preventing pressure sores and infections, while ventilating, disinfecting and reducing visits to the ward. Monitor blood count, blood sugar and kidney function at all times so that problems could be notified to the doctor in time for appropriate treatment. ③ Health education was provided to patients and their families to guide them to choose a nutritious diet and to enhance the intake of iron-containing foods. It was important to avoid consuming iron-containing foods while quoted tea and coffee to avoid affecting the absorption of iron in the body, but you could increase vitamin C-rich vegetables and fruits at the same time with iron-containing foods to promote their absorption.
The classification of compliance of surgical patients was divided into 3 levels: ① Good compliance: Perioperative patients fully accepted the treatment plan formulated by the physician, complete the complete treatment process, and fully cooperate with all care measures. ② Partial compliance: Perioperative patients accepted the treatment plan developed by their physicians and partially cooperated with the nursing measures. ③ Non-compliance: Perioperative patients did not understand the reactions and side effects that occur and do not cooperate with medical care..
The occurrence, severity and incidence of sore throat, dry throat, nausea and vomiting, and hoarseness at 24 h after surgery were recorded in the two groups. ① Postoperative sore throat: the degree was evaluated by numerical rating system (NRS) (11): 0 being no pain, and 10 being the most painful. ② Dry throat score: A score of 0 indicated that the patient felt no difference from before surgery and had no symptoms of dry throat. 1 indicated mild discomfort, the patient felt different from before surgery and had symptoms of dry throat, but it was not obvious that there was no feeling of stuffiness and/or constriction and no foreign body sensation in the pharynx. A score of 2 indicated moderate discomfort, mainly dryness of the throat with a feeling of stuffiness and/or constriction, with minimal self-consciousness, no or no foreign body sensation in the throat, occasional throat clearing, no habitual throat clearing, and a score of 3 indicated severe discomfort, with a constant habitual throat clearing to ensure the comfort of the throat, a feeling of stuffiness and/or constriction, and a feeling of reduced mucus secretion in the throat and an obvious foreign body sensation in the throat.
A questionnaire designed in-house was used to determine the satisfaction level of nursing care for both groups. The questionnaire was scored on a percentage scale, and the nursing satisfaction score consisted of 20 items in four dimensions: nursing attitude, nursing skills, nursing safety and nursing quality. Assessments were conducted separately before and after care and were rated by the same assessor.
Self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used to determine the severity of patients’ anxiety and depression negative emotions were positively correlated with the scores (12). A final SAS score of <50 indicates no anxiety, with higher scores indicating more severe anxiety. A final SDS score of <53 indicates no depression, with higher scores indicating more severe depression. Assessments were conducted separately before and after care and were rated by the same assessor.
The serum iPTH, Ca and P levels of the patients were compared preoperatively and at the 1st postoperative week. Serum iPTH was measured by enzyme-linked immunosorbent assay (The relevant kits were purchased from Shanghai mlbio Co.), and serum Ca and P were measured by fully automated biochemical analyzer(Shandong Boke Biological Industry Co.).
SPSS 20.0 was used for data analysis, and the independent sample t-test or Kruskal-Wallis and Mann-Whitney method tests were used for measurement data, and Fisher’S exact probability method was used for count data. P < 0.05 was considered a statistically significant difference.
General clinical data of the subjects were collected, including general demographic data and clinical characteristics such as gender, age, height, years on dialysis, and ASA classification, and iPTH, Ca, and P were tested before care. The results of the analysis showed that there was no significant difference between patients in the regular and high-quality group s in terms of gender, age, years on dialysis, weight, preoperative iPTH, Ca, and P levels, and the ratio of ASA classification, intractable pruritus, bone pain, insomnia, muscle weakness, and restless leg syndrome (p > 0.05) (Table 1).
The results of the pre-care measurement showed that there was no significant difference in the distribution of the three levels of good, partial and non-adherence between the regular group and the high-quality group (p > 0.05). After care, the number of cases of good compliance was higher, and the number of cases of non-compliance was lower in the high-quality group when compared to the regular group (p < 0.05); the difference in the number of cases of partial compliance between the two groups after care was not significant (p > 0.05) (Table 2).
We observed and counted the occurrence of pharyngeal complications such as sore throat, nausea and vomiting, dry throat, and hoarseness in the regular group and the high-quality group at 24 h postoperatively, and scored the degree of sore throat and dry throat. The results of the analysis showed that there was no significant difference in the incidence of pharyngeal complications such as sore throat, nausea and vomiting, dry throat and hoarseness between the two groups (p > 0.05); however, the scores of sore throat and dry throat in the high-quality group were significantly lower than the regular group 24 h after surgery (p < 0.05) (Table 3 and Figure 1).
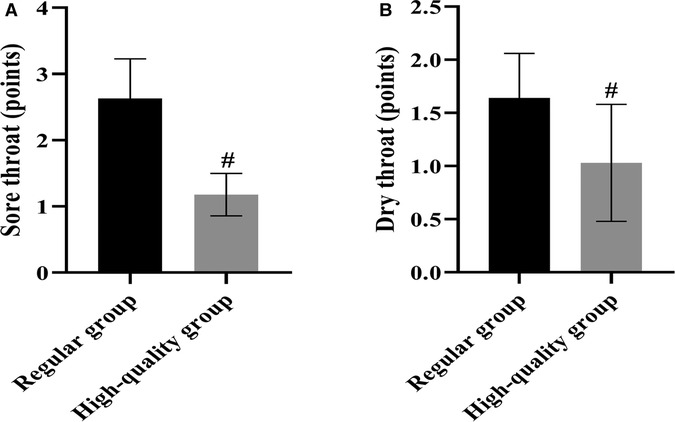
Figure 1. Comparison of the severity of postoperative pharyngeal complications between the two groups (Mean, SD). Note: (A) shows the sore throat score and (B) shows the dry throat score. # shows the difference with the Regular group, p < 0.05.
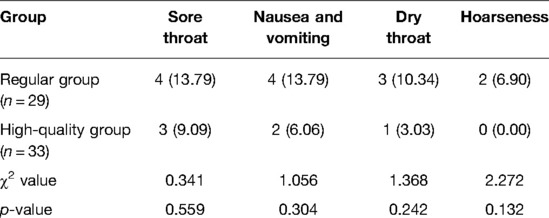
Table 3. Comparison of the occurrence of postoperative pharyngeal complications between the two groups (n,%).
The degree of patient satisfaction with nursing care in both groups was determined after nursing care using our in-house designed questionnaire. The results of the analysis showed that the patients in the high-quality group had higher ratings of nursing attitude, nursing skills, nursing safety, nursing quality, and overall nursing satisfaction than the regular group (p < 0.05) (Figure 2).
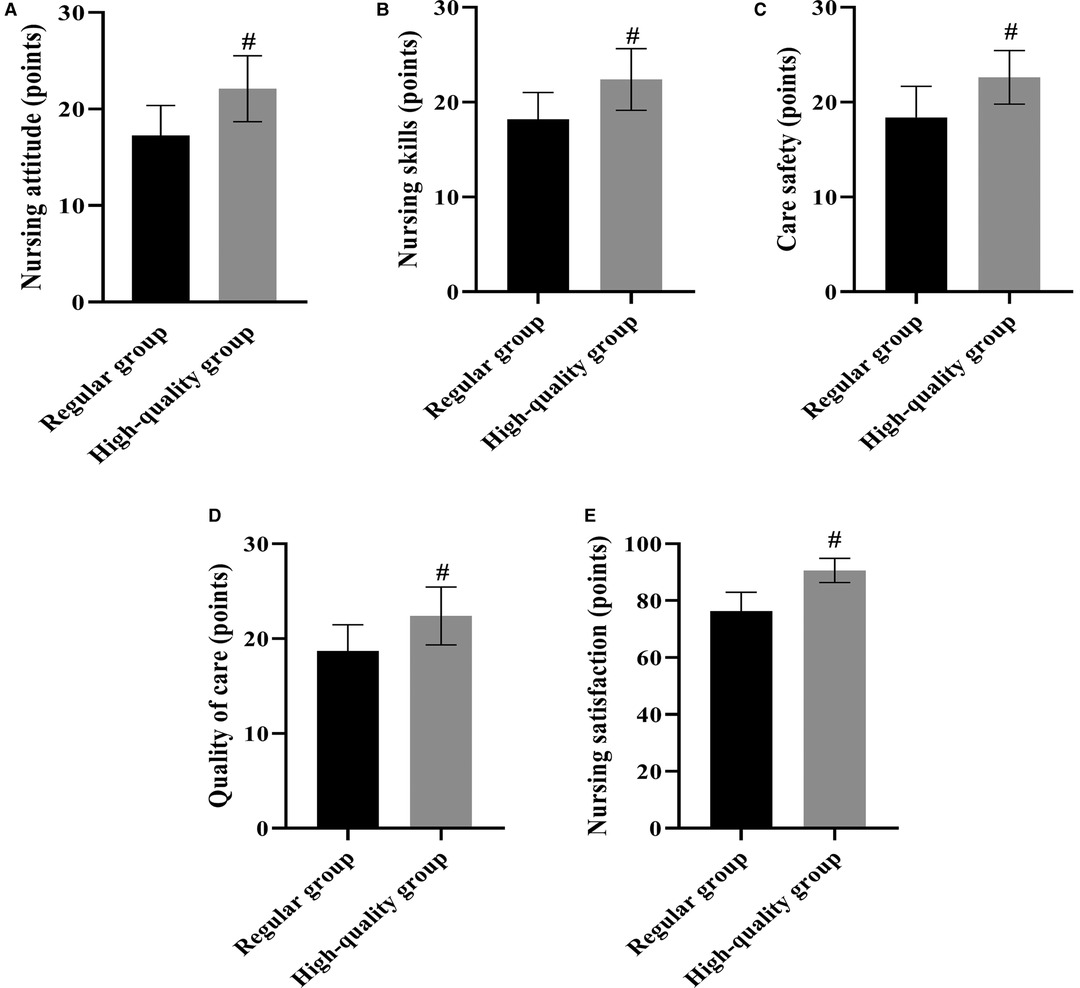
Figure 2. Comparison of various scores of nursing satisfaction after care in the two groups (Mean, SD). Note: (A) shows nursing attitude scores, (B) shows nursing skill scores, (C) shows nursing safety scores, (D) shows quality of care scores, and E shows total nursing satisfaction scores. # shows the difference with the Regular group, p < 0.05.
The SAS and SDS scales were used to assess the patients’ anxiety and depression before and after care. The results of the analysis showed that the difference between the SAS and SDS scores of the regular group and the high-quality group before care was not significant (p > 0.05). After care, the SAS and SDS scores of both groups decreased, and the SAS and SDS scores of the high-quality group decreased more than the regular group (p < 0.05) (Figure 3).
Figure 3. Comparison of psychological status scores between the two groups before and after care. (Mean, SD), Note: (A) shows SAS scores, (B) shows SDS scores. * shows the difference with the same group before care, p < 0.05; # shows the difference with the Regular group, p < 0.05.
Serum iPTH, Ca, and P levels were measured pre-op and 1 week post-op, respectively. The results of the analysis showed that the differences between the pre-op serum iPTH, Ca and P levels of the regular group and the high-quality group were not significant (P > 0.05). Serum iPTH, Ca, and P levels in both groups decreased at 1 week post-op, and the iPTH, Ca, and P scores in the high-quality group decreased more than those in the regular group (p < 0.05) (Figure 4).
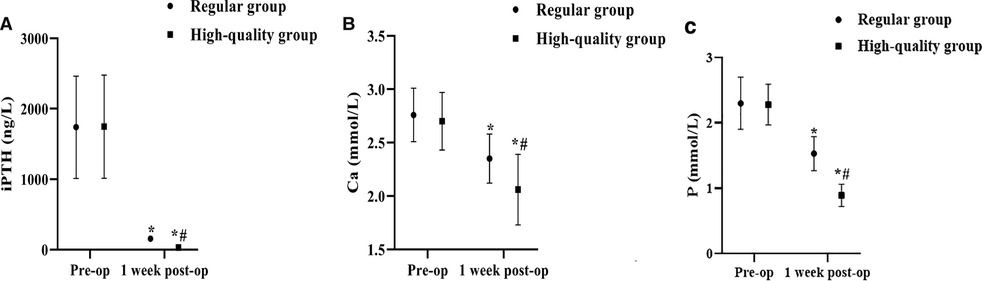
Figure 4. Comparison of iPTH, Ca, and P levels between the two groups before and 1 week after surgery. (Mean, SD). Note: (A) shows iPTH levels, (B) shows Ca levels, and (C) shows P levels. * shows the difference with the same group before care, p < 0.05; # shows the difference with the Regular group, p < 0.05.
SHPT is one of the common serious complications in CRF patients, especially in patients on long-term maintenance dialysis therapy. In CRF, the stimulation of the parathyroid glands by the imbalance of acid-base balance and various electrolyte metabolism disorders, as well as the presence of calcium and phosphorus metabolism disorders and active vitamin D deficiency in the middle and late stages of renal failure promote the secretion of PTH and induce the development of SHPT (13, 14). Studies have shown (15) that hypersecretion of PTH and hyperplasia and hypertrophy of parathyroid glands are characteristic of hyperparathyroidism. Patients with CRF-SHPT tend to present with hypercalcemia, osteoporosis, bone pain, skeletal deformities and pathological fractures, and most patients come to the clinic when they develop persistent bone pain (16). In China, because there are fewer kidney sources available for kidney transplantation and more patients with chronic renal impairment to chronic renal failure due to various reasons, patients with chronic renal failure are treated with hemodialysis or peritoneal dialysis with drug treatment for complications in order to maintain the quality of life of these patients and prolong their life span (17, 18). Over the past 20 years, SHPT has been well controlled due to the development of dialysis technology and early intervention with drugs, but some patients with refractory SHPT still require surgical treatment. However, the condition of these patients is complex, with many complications, and the surgical treatment of general anesthesia with tracheal intubation is an invasive operation, which can easily cause local nerve compression, airway mucosal injury, and vocal cord injury; the damage to the pharyngeal mucosa caused by tracheal intubation can lead to an imbalance in the ratio of the attached local flora, and some bacteria can move down with the catheter, which can increase the risk of infection, and then form harmful irritation and increase the risk of pharyngeal complications such as sore throat and dry throat (19, 20). Therefore, more effort needs to be invested before and after the procedure in CRF-SHPT patients to enable them to safely survive the perioperative period.
In this study, by observing the effect of implementing full quality care for patients undergoing CRF-SHPT surgery, we found that patient compliance, satisfaction with care, and improvement in SAS and SDS scores after care were better in the high-quality group than in the regular group. Although there was no significant difference in the incidence of pharyngeal complications between the two groups at 24 h postoperatively, the sore throat and dry throat degree scores were lower in the high-quality group than in the regular group. This suggests that the whole process of quality care can effectively improve the compliance of patients undergoing CRF-SHPT surgery, reduce patients’ bad mood, make patients accept the surgery in a good state of mind, and better cooperate with the treatment and nursing work; it can also reduce the degree of sore throat and dry throat of patients 24 h after surgery to accelerate their postoperative recovery, and improve the recognition and satisfaction of nursing work. In addition, the serum iPTH, Ca, and P levels of patients in the high-quality group were lower than those in the regular group at 1 week postoperatively, suggesting that conventional care enables faster correction of calcium and phosphorus disorders in patients undergoing CRF-SHPT. High-quality whole-course care takes quality care as the main nursing concept and enhances the efficiency of nursing work with a patient-centered service concept in the nursing process. By establishing a professional full quality nursing team, the nursing staff’s level of care has been enhanced to provide a comfortable treatment environment for patients undergoing CRF-SHPT, which is conducive to enhancing the comfort level of the patient’s organism, thereby increasing patient compliance with treatment (21, 22). Preoperative quality treatment was carried out mainly for patients’ psychological stress, hypercalcemia and surgical adaptation exercises, and medical and nursing education measures were further strengthened to give patients a more comprehensive understanding of the purpose, steps and procedures, and effects of the upcoming surgery, to fully prepare them psychologically, to eliminate their nervousness and concerns, and to reasonably avoid surgical risks (23, 24). Care through intraoperative sign monitoring, position selection, encouragement support and temperature maintenance can ensure a smooth operation. By planning a proper diet and actively taking good oral care and skin care after surgery, patients can reduce the discomfort level of sore throat, dry throat and other throat complications.
In conclusion, this study confirms that through the whole process of quality case, fully informed participation and active cooperation of CRF-SHPT patients, close medical and nursing collaboration, attention to detail and overall level of treatment can effectively improve patient compliance, psychological status and postoperative serum indicators, promote patient recovery and increase nursing satisfaction.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by This trial was approved by the local ethics committee. The patients/participants provided their written informed consent to participate in this study.
QL is the mainly responsible for the writing, data analysis. SZ is responsible for the guidance of the entire research. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. van der Plas WY, Noltes ME, van Ginhoven TM, Kruijff S. Secondary and tertiary hyperparathyroidism: a narrative review. Scand J Surg. (2020) 109:271–8. doi: 10.1177/1457496919866015
2. Boruah R, Monavari AA, Conlon T, Murphy N, Stroiescu A, Ryan S, et al. Secondary hyperparathyroidism in children with mucolipidosis type II (I-cell disease): irish experience. J Clin Med. (2022) 11:1366. doi: 10.3390/jcm11051366
3. Chandran M, Wong J. Secondary and tertiary hyperparathyroidism in chronic kidney disease: an endocrine and renal perspective. Indian J Endocrinol Metab. (2019) 23:391–9. doi: 10.4103/ijem.IJEM_292_19
4. Sari R, Yabanoglu H, Hargura AS, Kus M, Arer IM. Outcomes of total parathyroidectomy with autotransplantation versus subtotal parathyroidectomy techniques for secondary hyperparathyroidism in chronic renal failure. J Coll Physicians Surg Pak. (2020) 30:18–22. doi: 10.29271/jcpsp.2020.01.18
5. Jannot M, Normand M, Chabroux-Seffert A, Azzouz L, Afiani A, Jurine J, et al. Evolution of secondary hyperparathyroidism in patients following return to hemodialysis after kidney transplant failure. Nephrol Ther. (2020) 16:118–23. doi: 10.1016/j.nephro.2019.07.328
6. Joseph C, Shah S, Geer J, Juarez-Calderon M, Srivaths PR, Swartz SJ. Cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients below age 5 years. Clin Nephrol. (2019) 92:279–86. doi: 10.5414/CN109871
7. Fronk E, Billick SB. Pre-operative anxiety in pediatric surgery patients: multiple case study aalysis with literature review. Psychiatr Q. (2020) 91:1439–51. doi: 10.1007/s11126-020-09780-z
8. Ventura M, Belleudi V, Sciattella P, Di Domenicantonio R, Di Martino M, Agabiti N, et al. High quality process of care increases one-year survival after acute myocardial infarction (AMI): a cohort study in Italy. PLoS One. (2019) 14:e0212398. doi: 10.1371/journal.pone.0212398
9. Li XQ. Effects of high-quality nursing care on psychological outcomes in patients with chronic heart failure. Medicine (Baltimore). (2019) 98:e17351. doi: 10.1097/MD.0000000000017351
10. de Holanda NCP, Baad VMA, Bezerra LR, de Lima SKM, Filho JM, de Holanda Limeira CC, et al. Secondary hyperparathyroidism, bone density, and bone turnover after bariatric surgery: differences between roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. (2021) 31:5367–75. doi: 10.1007/s11695-021-05739-6
11. Baravieira PB, Brasolotto AG, Montagnoli AN, Silvério KC, Yamasaki R, Behlau M. Auditory-perceptual evaluation of rough and breathy voices: correspondence between analogical visual and numerical scale. Codas. (2016) 28:163–7. English, Portuguese. doi: 10.1590/2317-1782/20162015098
12. Besèr A, Sorjonen K, Wahlberg K, Peterson U, Nygren A, Asberg M. Construction and evaluation of a self rating scale for stress-induced exhaustion disorder, the Karolinska Exhaustion Disorder Scale. Scand J Psychol. (2014) 55:72–82. doi: 10.1111/sjop.12088
13. Pasnicu C, Radu PA, Garofil D, Bengulescu I, Paic V, Tigora A, et al. Clinical aspects of parathyroid hyperplasia in secondary renal hyperparathyroidism. Chirurgia (Bucur). (2019) 114:594–601. doi: 10.21614/chirurgia.114.5.594
14. Hu Y, Hua SR, Wang MY, Su Z, Cui M, Zhang X, et al. Sequential parathyroidectomy under cervical plexus anesthesia for secondary hyperparathyroidism with renal function failure. Zhonghua Wai Ke Za Zhi. (2018) 56:528–32. Chinese. doi: 10.3760/cma.j.issn.0529-5815.2018.07.009
15. Palumbo VD, Palumbo VD, Damiano G, Messina M, Fazzotta S, Lo Monte G, et al. Tertiary hyperparathyroidism: a review. Clin Ter. (2021) 172:241–6. doi: 10.7417/CT.2021.2322
16. Palmer SC, Mavridis D, Johnson DW, Tonelli M, Ruospo M, Strippoli GFM. Comparative effectiveness of calcimimetic agents for secondary hyperparathyroidism in adults: a systematic review and network meta-analysis. Am J Kidney Dis. (2020) 76:321–30. doi: 10.1053/j.ajkd.2020.02.439
17. Gong X, Zou L, Wu H, Shan Y, Liu G, Zheng S, et al. Altered brain structural and cognitive impairment in end-stage renal disease patients with secondary hyperparathyroidism. Acta Radiol. (2020) 61:796–803. doi: 10.1177/0284185119878360
18. Sun Y, Tian B, Sheng Z, Wan P, Xu T, Yao L. Efficacy and safety of cinacalcet compared with other treatments for secondary hyperparathyroidism in patients with chronic kidney disease or end-stage renal disease: a meta-analysis. BMC Nephrol. (2020) 21:316. doi: 10.1186/s12882-019-1639-9
19. Wu Y, Liu Y, Huang T, Jiang Y, Wang H, He Z. Application of nanocarbon negative imaging technology in surgery for secondary hyperparathyroidism. Gland Surg. (2021) 10:2455–61. doi: 10.21037/gs-21-385
20. Steinl GK, Kuo JH. Surgical management of secondary hyperparathyroidism. Kidney Int Rep. (2020) 6:254–64. doi: 10.1016/j.ekir.2020.11.023
21. Truant TLO, Varcoe C, Gotay CC, Thorne S. Toward equitably high-quality cancer survivorship care. Can Oncol Nurs J. (2019) 29:156–62. doi: 10.5737/23688076293156162
22. Litao H, Yuxuan R, Yongxia S. Infiltration and extravasation of intravenous infusions in children-value of high-quality care on outcome. J Pak Med Assoc. (2021) 71:1181–3. doi: 10.47391/JPMA.02-194
23. Walpole SC, Smith K, McElvaney J, Taylor J, Doe S, Tedd H. An investigation into hospital prescribers’ knowledge and confidence to provide high-quality, sustainable respiratory care. Future Healthc J. (2021) 8:e272–6. doi: 10.7861/fhj.2020-0251
Keywords: chronic renal failure, secondary hyperparathyroidism, high-quality whole-course care, psychological status, surgery, pharyngeal complications
Citation: Luo Q and Zheng S (2022) Effect of High-Quality Whole-Course Care on Psychological Status and Postoperative Pharyngeal Complications in Patients Undergoing Surgery for Hyperparathyroidism Secondary to Chronic Rrenal Failure. Front. Surg. 9:905413. doi: 10.3389/fsurg.2022.905413
Received: 27 March 2022; Accepted: 19 April 2022;
Published: 19 May 2022.
Edited by:
Songwen Tan, Central South University, ChinaReviewed by:
Fang Wei, Second Xiangya Hospital, Central South University, ChinaCopyright © 2022 Luo and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuquan Zheng MTUxNzc0NjQzM0BxcS5jb20=
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.