
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 18 May 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.904928
This article is part of the Research Topic Co-use of medicines in surgery View all 114 articles
 Xianchao Zhou
Xianchao Zhou Xiang Shen*
Xiang Shen*
Objective: To compare the clinical effect of hip arthroplasty and closed reduction intramedullary nailing of proximal femur in the treatment of elderly hip fracture patients.
Methods: There are 90 elderly hip fracture patients being recruited in the present study. Fifty patients in Group A received closed reduction intramedullary nailing of proximal femur, and 40 patients in Group B received hip arthroplasty. All patients were followed up for 12 months after surgery, clinical outcomes included surgical indicators, visual analog scale (VAS) score, Harris score, quality of life, mental status, and complications.
Results: The surgery time, bleeding volume, infusion volume of patients in Group A are all significantly lower than those in Group B (p < 0.05), while the weight-bearing activity time and first workout time of Group A are all significantly higher than those in Group B (p < 0.05). The VAS score in patients of Group A at 1 week postoperative is significantly lower than that in patients of Group B (p < 0.05). The Harris score in patients of Group A at 3, 6, and 12 months postoperative are all significantly higher than those in patients of Group B (p < 0.05), and the excellent and good rate of hip function recovery at 12 months postoperative in patient of Group A is significantly lower than that in patients of Group B (80% vs. 95%, p < 0.05). Furthermore, The score of SF-36 standardized physical component, SF-36 standardized mental component and Barthel in patients of Group A at 6 months postoperative are significantly lower than those in patients of Group B (p < 0.05), and the score of mini-mental state examination is significantly higher (p < 0.05), while there are not significantly different at 12 months postoperative (p > 0.05). The incidence of postoperative complications in Group A was significantly lower than that in Group B (10% vs. 27.5%, p < 0.05).
Conclusion: Elderly hip fracture patients treated with closed reduction intramedullary nailing of proximal femur has less surgical trauma and lower complication rates, but slower postoperative recovery compared with hip arthroplasty.
Hip fractures are the most common type of fractures in orthopedics, including intertrochanteric fractures, femoral–tibial fractures, and subtrochanteric fractures, with the highest incidence in elderly patients which is due to osteopenia or osteoporosis (1, 2) Hip fractures not only increase mortality and reduce the quality of life in older patients, but also cause patients to be unable to return to their pre-injury living environment, require higher levels of care, and so on (3, 4). Treatment protocols for hip fractures include both non-surgical and operative treatments, but non-surgical treatments have significant disadvantages including fracture malunion, nonunion, and complications from prolonged bed rest (5–7). Therefore, surgery is recommended for all elderly patients with hip fractures who tolerate surgery. Protocols for surgical treatment of hip fractures include dynamic hip screw, dynamic condylar screw, proximal femoral nail, proximal femoral nail antirotation, hip arthroplasty, etc (8).
Currently, proximal femur nail and hip arthroplasty are widely used in the treatment of hip fractures due to their suitability for various types of hip fractures, simple surgery, low blood loss, and low trauma (9, 10). However, many clinical studies have compared the efficacy of proximal femur nail and hip arthroplasty in the treatment of hip fractures, but the results have been inconsistent or even opposite (11, 12). In the present study, we designed to study the clinical effect of hip arthroplasty and closed reduction intramedullary nailing of proximal femur in the treatment of elderly hip fracture patients.
There were 90 elderly hip fracture patients from January to December 2020 being recruited in the present study. Diagnostic reference for hip fractures “Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists” (13). According to the different surgical treatment methods, they were divided into Group A and Group B. Fifty patients in Group A received closed reduction intramedullary nailing of proximal femur, and 40 patients in Group B received hip arthroplasty. All patients recruited in this study were informed about the details of this study and signed informed consent. In addition, all patients enrolled in this study must meet the following criteria: Inclusion criteria: (1) over 60 years old; (2) hip fracture diagnosed by imaging; (3) surgery performed within 1 week of fracture; and (4) compliance with surgical criteria and signed informed consent. Exclusion criteria: (1) multiple fractures, or surgery performed over 1 week of fracture; (2) deep vein thrombosis, infection, cardiovascular and cerebrovascular disease, malignant tumor; (3) mental disability, intellectual disability, or communication difficulties; (4) Refracture after surgery; (5) failure to complete 12-month follow-up after surgery; (6) failure to cooperate with training; and (7) abnormal functions of organs such as liver and kidney.
We collected the demographic of patients including age, gender, height, and weight, and recorded the surgery information including American Society of Anesthesiologists (ASA) grade, the surgery time, bleeding volume, infusion volume, and we also recorded hospital stay time, weight-bearing activity time, and first workout time. Moreover, we used visual analog scale (VAS) score to evaluate the pain of patients at 1 h, 24 h, 48 h, and 1 week postoperative.
All patients completed a 12-month follow-up after surgery, and the follow-up protocol was as follows: All patients returned to the hospital for imaging examinations and hip function assessments at 3, 6, and 12 months after surgery. And we used the Harris score to evaluate the hip function of patients before treatment and at 3, 6, and 12 months postoperative. According to the Harris score, the hip function recovery of elderly hip fractures patients was rated as excellent (Harris score ≥90), good (80≤ Harris score <90), medium (70≤ Harris score <80), and poor (Harris score <70) (14, 15). At 6 and 12 months postoperative, we used the health survey summary (MOS) item short form health survey (SF-36) and Barthel index to evaluate the life quality of patients, and used mini-mental state examination (MMSE) evaluate the mental state of patients.
Data in this study were analyzed by SPSS20.0 (National Institute of Health in the USA). We used Student’s t-test to compare the differences in measurement data between the two groups, and used the χ2 test to compare differences in count data. p < 0.05 indicated significant difference.
As shown in Table 1, the demographic of patients in Group A including age, gender, height, and weight are all no significantly different with patients in Group B (p > 0.05). At the same time, there is also no significant difference in ASA grade and the time of hospital stay between Group A and Group B (p > 0.05). However, the surgery time, bleeding volume, and infusion volume of patients in Group A are all significantly lower than those in Group B (p < 0.05), while the weight-bearing activity time and first workout time of patients in Group A are all significantly higher than those in Group B (p < 0.05) (Table 1).
There is no significant difference in VAS score at 1, 24, and 48 h postoperative between Group A and Group B (p > 0.05), while the VAS score in patients of Group A at 1-week postoperative is significantly lower than that in patients of Group B (p < 0.05) (Table 2).
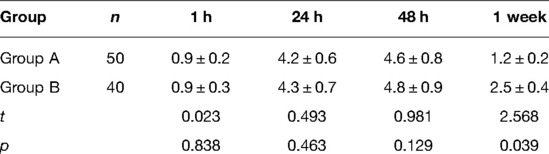
Table 2. Comparison of VAS scores at different time after operation between two groups of patients (score, ).
There is no significant difference in Harris score between Group A and Group B preoperative (p > 0.05), while the Harris score in patients of Group A at 3, 6, and 12 months postoperative are all significantly higher than those in patients of Group B (p < 0.05) (Table 3). Furthermore, according to the Harris score at 12 months postoperative, the number of patients in Group A whose hip function was rated as excellent, good, medium, and poor are 15, 25, 8, and 2, respectively. And Group B are 23, 15, 2, and 0, respectively. Importantly, the excellent and good rate of hip function recovery at 12 months postoperative in patient of Group A is significantly lower than that in patients of Group B (80.0% vs. 95.0%, p < 0.05) (Table 4).
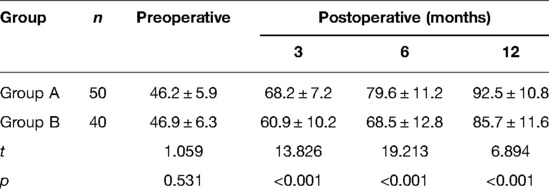
Table 3. Comparison of Harris score between two groups of patients at different time after operation (score, ).
The score of SF-36 (PCS), SF-36 (MCS), and Barthel in patients of Group A at 6 months postoperative are significantly lower than those in patients of Group B, while the score of MMSE in patients of Group A at 6 months postoperative is significantly lower than that patients of Group B (p < 0.05) (Table 5). At 12 months postoperative, there are no significance in the score of SF-36 (PCS), SF-36 (MCS), Barthel, and MMSE between Group A and Group B (p > 0.05) (Table 6).
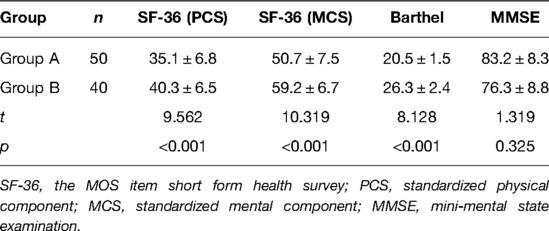
Table 5. Comparison of life quality and mental state at 6 months postoperative between two group (score, ).
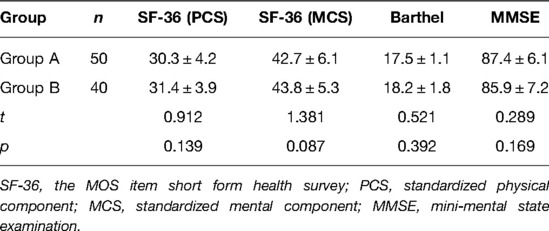
Table 6. Comparison of life quality and mental state at 12 months postoperative between two group (score, ).
All patients were followed up for 12 months after surgery, there were 1 infection, 3 deep vein thrombosis (DVT), and 1 bedsore in Group A, while 1 infection, 2 built-in loose, 2 DVT, 2 bedsores, and 4 cardiovascular disease occurred in Group B. Namely, the incidence of postoperative complications in Group A was significantly lower than that in Group B (10% vs. 27.5%, p < 0.05) (Table 7).
Hip fracture is the most common fracture in the elderly, accounting for about 3%–4% of the whole-body fracture, which not only seriously affects the daily life of patients, but also increases the risk of death of patients (1, 2). At present, non-surgical conservative treatment, internal fixation surgery, and artificial hip replacement are clinically used for the treatment of patients with different types of hip fractures. Among them, non-surgical conservative treatment is only recommended for patients who cannot tolerate surgical treatment due to its long treatment cycle, poor treatment effect, and long-term bed rest. Surgery is currently the preferred treatment protocol recommended for hip fracture patients (5–7). Internal fixation and artificial hip arthroplasty are the main surgical methods for hip fracture surgical treatment, and the advantages are not only reduced trauma and shortened bed time, but also significantly reduced the incidence of complications, promoted functional recovery of the hip joint and improved the life quality of hip fracture patients (9, 10).
In this study, elderly hip fracture patients received hip arthroplasty or closed reduction proximal femur nail treatment, and we found that compared with hip arthroplasty, closed reduction proximal femur nail treatment had less surgery time, bleeding volume, infusion volume, but higher weight-bearing activity time and first workout time, which suggested closed reduction proximal femur nail treatment is less traumatic for elderly fracture patients, while hip arthroplasty treatment patients recover faster after surgery. In addition, we also found that the postoperative long-term hip function recovery of hip arthroplasty patients was better than closed reduction proximal femur nail treatment, but there was no significant difference in postoperative long-term quality of life and mental state between the two groups.
Artificial hip arthroplasty is the most commonly used surgical treatment in clinical practice, and its advantages are that the postoperative joint mobility is good, the stability is high, and the patient can get out of bed early without waiting for the fracture site to heal (16, 17). Bone cement-type and bio-type artificial hip joints are two groups of prostheses commonly used in the clinic, and they have different characteristics when used in the treatment of elderly patients with hip fractures (18, 19). Bone cement artificial hip joint can improve early stability, help get out of bed early, and promote recovery, but different degrees of acute hypotension, hypoxemia, arrhythmia, cardiac arrest, and cardiopulmonary dysfunction may occur (20, 21). The initial stability of the biological artificial hip joint is not ideal, and long-term bed rest is required after the operation (21). Therefore, the effect of short-term follow-up after the operation is not as good as that of the cemented artificial hip joint, but the risk of postoperative unsafe events is relatively low. In the present study, since the subjects included in this study were all elderly patients with hip fracture, osteoporosis, and severe bone loss were common, so a cemented artificial hip joint was selected during the operation to improve the early stability. Proximal femoral nail fixation is a minimally invasive intramedullary fixation procedure based on biomechanical principles using an anti-rotation helical blade to fix the femoral neck. Because the helical blade is very close to the bone, it can prevent fracture rotation and varus deformity, and enhance fracture stability (22–25). As a minimally invasive operation, small surgical incision, small trauma, short operation time, and avoiding periosteum and soft tissue dissection are the inherent advantages of proximal femoral nailing (26, 27).
Postoperative complications are the main risk factors affecting the recovery of elderly patients with hip fracture (28, 29). Bone cement poisoning, including cardiovascular disease, pulmonary dysfunction, and hypotension, is the main postoperative complication of hip arthroplasty (20, 21). In this study, there were 11 postoperative complications in elderly hip fracture patients treated with hip arthroplasty, among which the highest incidence of cardiovascular disease (four cases). Compared with hip replacement, the postoperative complication rate of elderly hip fracture patients treated with proximal femoral nail fixation is lower, only 10%. This is mainly due to the low trauma to patients treated with proximal femoral nail fixation. However, it should be noted that although the postoperative complication rate of patients treated with proximal femoral nail fixation was significantly lower than that treated with hip arthroplasty, patients treated with hip arthroplasty had faster recovery of hip function. This is mainly due to the timely intervention of postoperative complications to reduce their impact on patients’ postoperative recovery.
Hip arthroplasty and proximal femoral nail fixation have different advantages for elderly patients with hip fractures. The advantages of proximal femoral nail fixation are ease of operation, less trauma, less operative time, and postoperative complication rates, while the advantages of hip arthroplasty are faster postoperative recovery. Therefore, for different elderly hip fracture patients, different surgical treatment methods should be selected according to their actual status.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by This study was approved by the ethics committee of our hospital. All subjects gave informed consent and signed the informed consent form. The patients/participants provided their written informed consent to participate in this study.
XZ is mainly responsible for the writing, data analysis, and research design of the article. The corresponding author is XS, and he is responsible for ensuring that the descriptions are accurate and agreed by all authors. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Asada M, Horii M, Ikoma K, Goto T, Okubo N, Kuriyama N, et al. Hip fractures among the elderly in Kyoto, Japan: a 10-year study. Arch Osteoporos. (2021) 16:30. doi: 10.1007/s11657-021-00888-8
2. Li L, Bennett-Brown K, Morgan C, Dattani R. Hip fractures. Br J Hosp Med. (2020) 81:1–10. doi: 10.12968/hmed.2020.0215
3. Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging. (2018) 13:143–50. doi: 10.2147/CIA.S150067
4. Wang Z, Chen M, Luo X, Xiong X, Ma F. Effectiveness of optimised care chain for hip fractures in elderly Chinese. Int J Health Plann Manage. (2021) 36:1445–64. doi: 10.1002/hpm.3261
5. Kim SJ, Park HS, Lee DW. Outcome of nonoperative treatment for hip fractures in elderly patients: a systematic review of recent literature. J Orthop Surg. (2020) 28:2309499020936848. doi: 10.1177/2309499020936848
6. Wijnen HH, Schmitz PP, Es-Safraouy H, Roovers LA, Taekema DG, Van Susante JLC. Nonoperative management of hip fractures in very frail elderly patients may lead to a predictable short survival as part of advance care planning. Acta Orthop. (2021) 92:728–32. doi: 10.1080/17453674.2021.1959155
7. Loggers SAI, Van Lieshout EMM, Joosse P, Verhofstad MHJ, Willems HC. Prognosis of nonoperative treatment in elderly patients with a hip fracture: a systematic review and meta-analysis. Injury. (2020) 51:2407–13. doi: 10.1016/j.injury.2020.08.027
8. Saul D, Riekenberg J, Ammon JC, Hoffmann DB, Sehmisch S. Hip fractures: therapy, timing, and complication spectrum. Orthop Surg. (2019) 11:994–1002. doi: 10.1111/os.12524
9. Adeel K, Nadeem RD, Akhtar M, Sah RK, Mohy-Ud-Din I. Comparison of proximal femoral nail (PFN) and dynamic hip screw (DHS) for the treatment of AO type A2 and A3 pertrochanteric fractures of femur. J Pak Med Assoc. (2020) 70:815–9. doi: 10.5455/JPMA.295426
10. Godoy-Monzon D, Diaz Dilernia F, Piccaluga F, Cid Casteulani A, Turus L, Buttaro M. Conversion total hip arthroplasty with a proximally modular, distal fixation reconstruction prosthesis following cephalomedullar nail failure. Hip Int. (2020) 30:26–33. doi: 10.1177/1120700020937952
11. Suh YS, Nho JH, Kim SM, Hong S, Choi HS, Park JS. Clinical and radiologic outcomes among bipolar hemiarthroplasty, compression hip screw and proximal femur nail antirotation in treating comminuted intertrochanteric fractures. Hip Pelvis. (2015) 27:30–5. doi: 10.5371/hp.2015.27.1.30
12. Ucpunar H, Camurcu Y, Çöbden A, Sofu H, Kis M, Demirel H. Comparative evaluation of postoperative health status and functional outcome in patients treated with either proximal femoral nail or hemiarthroplasty for unstable intertrochanteric fracture. J Orthop Surg. (2019) 27:2309499019864426. doi: 10.1177/2309499019864426
13. Griffiths R, Babu S, Dixon P, Freeman N, Hurford D, Kelleher E, et al. Guideline for the management of hip fractures 2020: guideline by the association of anaesthetists. Anaesthesia. (2021) 76:225–37. doi: 10.1111/anae.15291
14. Li F, Zhu L, Geng Y, Wang G. Effect of hip replacement surgery on clinical efficacy, VAS score and Harris hip score in patients with femoral head necrosis. Am J Transl Res. (2021) 13:3851–5. doi: 10.3892/ajtr.2021.6214
15. Jolly A, Bansal R, More AR, Pagadala MB. Comparison of complications and functional results of unstable intertrochanteric fractures of femur treated with proximal femur nails and cemented hemiarthroplasty. J Clin Orthop Trauma. (2019) 10:296–301. doi: 10.1016/j.jcot.2017.09.015
16. Marcu FM, Negrut N, Uivaraseanu B, Ciubara A, Lupu VV, Dragan F, et al. Benefits of combining physical therapy with occupational therapy in hip arthroplasty. J Pers Med. (2021) 11:1131. doi: 10.3390/jpm11111131
17. Magan AA, Kayani B, Chang JS, Roussot M, Moriarty P, Haddad FS. Artificial intelligence and surgical innovation: lower limb arthroplasty. Br J Hosp Med. (2020) 81:1–7. doi: 10.12968/hmed.2020.0309
18. Cui Q, Liu YS, Li DF, Zhang P, Guo J, Liu C, et al. Cemented hip hemiarthroplasty clinical observations on unstable intertrochanteric fracture in elderlies. Eur J Trauma Emerg Surg. (2016) 42:651–6. doi: 10.1007/s00068-015-0566-0
19. Pezzotti G, Yamamoto K. Artificial hip joints: the biomaterials challenge. J Mech Behav Biomed Mater. (2014) 31:3–20. doi: 10.1016/j.jmbbm.2013.06.001
20. Cai Z, Piao C, Sun M, Zhou H, Gao Z, Xiang L. Bone cement leaking into iliac vein during artificial femoral head replacement: A case report. Medicine (Baltimore). (2019) 98:e17547. doi: 10.1097/MD.0000000000017547
21. Santori N, Falez F, Potestio D, Santori FS. Fourteen-year experience with short cemented stems in total hip replacement. Int Orthop. (2019) 43:55–61. doi: 10.1007/s00264-018-4205-3
22. Heckmann ND, Chen XT, Ballatori AM, Ton A, Shahrestani S, Chung BC, et al. Cemented vs cementless femoral fixation for total hip arthroplasty after displaced femoral neck fracture: a nationwide analysis of short-term complications and readmission rates. J Arthroplasty. (2021) 36:3667–75.e4. doi: 10.1016/j.arth.2021.06.029
23. Chang HM, Lu WY, Kuan FC, Su WR, Chen PY, Su PF, et al. Wound drainage after proximal femoral nail antirotation (PFNA) fixation may negatively affect the patients with intertrochanteric fractures: a prospective randomized controlled trial. Injury. (2021) 52:575–81. doi: 10.1016/j.injury.2020.10.033
24. Baral P, Chaudhary P, Shah AB, Banjade D, Jha SC. Outcome of proximal femoral nail antirotation II fixation of peritrochanteric fracture of femur. J Nepal Health Res Counc. (2020) 18:301–6. doi: 10.33314/jnhrc.v18i2.2956
25. Nherera L, Trueman P, Horner A, Watson T, Johnstone AJ. Comparison of a twin interlocking derotation and compression screw cephalomedullary nail (InterTAN) with a single screw derotation cephalomedullary nail (proximal femoral nail antirotation): a systematic review and meta-analysis for intertrochanteric fractures. J Orthop Surg Res. (2018) 13:46. doi: 10.1186/s13018-018-0749-6
26. Liu W, Liu J, Ji G. Comparison of clinical outcomes with proximal femoral nail anti-rotation versus InterTAN nail for intertrochanteric femoral fractures: a meta-analysis. J Orthop Surg Res. (2020) 15:500. doi: 10.1186/s13018-020-02031-8
27. Guo J, Dong W, Jin L, Yin Y, Zhang R, Hou Z, et al. Treatment of basicervical femoral neck fractures with proximal femoral nail antirotation. J Int Med Res. (2019) 47:4333–43. doi: 10.1177/0300060519862957
28. Wang X, Zhao BJ, Su Y. Can we predict postoperative complications in elderly Chinese patients with hip fractures using the surgical risk calculator? Clin Interv Aging. (2017) 22:1515–20. doi: 10.2147/CIA.S142748
Keywords: hip fracture, hip arthroplasty, closed reduction, intramedullary nailing, proximal femur nail
Citation: Zhou X and Shen X (2022) A Comparative Study of Hip Arthroplasty and Closed Reduction Proximal Femur Nail in the Treatment of Elderly Patients with Hip Fractures. Front. Surg. 9:904928. doi: 10.3389/fsurg.2022.904928
Received: 26 March 2022; Accepted: 20 April 2022;
Published: 18 May 2022.
Edited by:
Songwen Tan, Central South University, ChinaReviewed by:
Yang Liu, The First Medical Center of Chinese PLA General Hospital, ChinaCopyright © 2022 Zhou and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiang Shen c3g4NDcyOTMzMUAxNjMuY29t
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.